Abstract
Physicians, nurses, and other health care providers initiated the #GetMePPE movement on Twitter to spread awareness of the shortage of personal protective equipment (PPE) during the coronavirus disease (COVID-19) pandemic. Dwindling supplies, such as face masks, gowns and goggles, and inadequate production to meet increasing demand have placed health care workers and patients at risk. The momentum of the #GetMePPE Twitter hashtag resulted in the creation of a petition to urge public officials to address the PPE shortage through increased funding and production. Simultaneously, the GetUsPPE.org website was launched through the collaboration of physicians and software engineers to develop a digital platform for the donation, request, and distribution of multi-modal sources of PPE. GetUsPPE.org and #GetMePPE were merged in an attempt to combine public engagement and advocacy on social media with the coordination of PPE donation and distribution. Within 10 days, over 1800 hospitals and PPE suppliers were registered in a database that enabled the rapid coordination and distribution of scarce and in-demand materials. One month after its launch, the organization had distributed hundreds of thousands of PPE items and had built a database of over 6000 PPE requesters. The call for action on social media and the rapid development of this digital tool created a productive channel for the public to contribute to the health care response to COVID-19 in meaningful ways. #GetMePPE and GetUsPPE.org were able to mobilize individuals and organizations outside of the health care system to address the unmet needs of the medical community. The success of GetUsPPE.org demonstrates the potential of digital tools as a platform for larger health care institutions to rapidly address urgent issues in health care. In this paper, we outline this process and discuss key factors determining success.
Keywords: digital health, getusppe, getmeppe, COVID-19, personal protective equipment, protection, Twitter, pandemic, health care worker
Introduction
On March 17, 2020, the Twitter hashtag #GetMePPE went viral [1-3] as thousands of nurses, physicians, and other health care providers posted pictures of themselves with personal protective equipment (PPE). The pictures were accompanied by attestations of dwindling—or in some cases completely absent—stocks of face masks, N95 respirators, and other supplies, even as providers began to evaluate and treat patients with coronavirus disease (COVID-19). The hashtag drew an outpouring of public support and media attention [4] amplifying the PPE shortage (Figure 1); a website, GetMePPE.org, obtained over 62,000 signatures for its online petition for increased government support of, and funding for, PPE [5].
Figure 1.
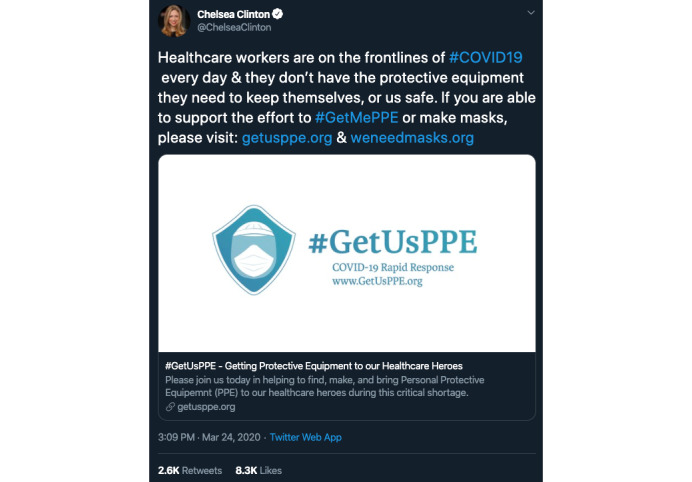
Example tweet from an individual who increased the viewership of #GetMePPE [4].
Simultaneously, a separate group launched GetUsPPE.org [6] with the goal of connecting people who needed PPE with individuals or organizations who had some available. The two groups came together on March 21, with the GetUsPPE.org webpage taking on the #GetMePPE petition as well as the coordination of PPE donation delivery. Only 10 days later, the site had over 120,000 views, the petition had over 10,000 signatures, and over 1800 hospitals and PPE suppliers had entered their information into the continuously updated database. Currently, one month after the merger, a web application with automated attribution and a last-mile system has facilitated the delivery of hundreds of thousands of items of PPE in three trial cities (getusppe.org/data), and partnerships have been formed with the American Medical Association, the American Hospital Association, and a number of specialty societies [7]. The GetUsPPE.org website was rapidly launched to collect available supply and demand requests. Textbox 1 shows a list of the types of facilities that can request PPE on the website.
Types of health care facility designations for the Request Donations page on the GetUsPPE.org website.
Acute care hospital
Freestanding emergency room
Field hospital
Hospital overflow facility
Emergency medical services
Urgent care clinic
Nonacute care hospital
Inpatient psychiatric facility
Inpatient rehabilitation facility
Residential substance treatment facility
Nursing home or skilled nursing facility
Assisted living facility or group home
Homeless shelter
Correctional facility or detention center
Hospice
Dialysis center
Outpatient clinic (primary care or specialist)
Public health clinic or community health center
Indian or Tribal healthcare facility (any kind)
Outpatient rehabilitation facility
Dental or oral surgery clinic (providing urgent/emergency care)
Home health agency
COVID-19 test site
Ophthalmic provider
Clinical laboratory
Pharmacy
Mortuary or coroner's office
Social services organization
Other
Much like just-in-time manufacturing [8], we propose that this type of rapid website deployment will be a solution in the future when urgent health care scenarios arise.
Needs
At the time of writing, 56/60 US jurisdictions (93.3%) have reported cases of COVID-19 infection [9]; most states are experiencing sustained community spread. While analysis of US statistics is ongoing, in analyses from Wuhan, China, 26% of patients received ICU care, and the mortality rate was 4.3% [10]. PPE is critical to protect health care workers at the front lines of caring for these patients. According to US Centers for Disease Control guidelines for use of PPE in US hospitals [11], both N-95 filtering facemask respirators and powered air-purifying respirators should be accompanied by the use of a full-face shield, helmet, or headpiece. Prior experience with the Ebola virus and severe acute respiratory syndrome (SARS) affirm that PPE provides “the last physical barrier” between health care workers and infectious body fluids [12,13].
Despite this, health care providers across the United States are lacking basic PPE, including gowns and masks, as they care for sick patients with COVID-19 [14]. Evidence from past epidemics suggests that clinical workers are at much higher risk than the general population of being infected [15,16]. PPE shortages not only compromise the safety of health care workers but also put patients at risk. As health care providers fall sick, fewer of us are available to care for patients. The lack of PPE also results in higher infection rates within hospitals as staff move from patient to patient without proper protection. In the Wuhan case analysis, hospital-related COVID-19 transmission occurred in 41% of patients [10].
Application of Digital Tools
In less than 12 hours over the course of a weekend, a group of medical students, doctors, software engineers, and volunteers from around the US built and launched a web-based platform, GetUsPPE.org, to enable the public to answer the call for help. On the website, organizations requesting PPE report their name, organization type, and address, followed by their PPE needs (such as PPE types and conditions of acceptance). People or organizations interested in donating PPE provide their contact details and information about their supplies, and they indicate if they are available to deliver or ship them. We were immediately flooded with heartwarming support and offers to help, not only from a variety of existing sources of PPE but also from novel additive manufacturing facilities and homemade makers. More importantly, the site enabled us to collect signatures to push for government action, process PPE donations from a public now keenly aware of the problem, and facilitate distribution of the PPE to health care workers in need. The website now supports global affiliates, including India as a prominent partner [17].
We attribute the success of our digital platform to three key components. First, there was unity around a clear and common cause. Importantly, the effort was not limited to physicians but was extended to all staff impacted by the shortage of PPE. Through firsthand stories of paramedics facing exposure in the field, nurses treating patients who were coughing in their faces, housekeeping staff cleaning rooms without adequate protection, pharmacists assisting with intensive care unit medication dosing without masks, and concerned friends and family, it was clear that our platform was needed for health care workers of all types.
Second, as health care providers in the “trenches,” we leveraged social media to share what we were witnessing and give all stakeholders a voice. Using the #GetUsPPE hashtag, physicians shared photographs of themselves without proper PPE, video tutorials teaching each other how to create homemade PPE [18], and images of store shelves fully stocked with boxes of N95 masks [19] while hospitals had none [20]. Stories circulated quickly on Twitter and on other social media platforms, including stories of emergency physicians hospitalized after contracting COVID-19 on the job [21]. Later, the stories became more uplifting, with updates of community members coming together to support health care workers and donate PPE to hospitals and other health care organizations.
Finally, the digital platform itself is intuitive and easy for users to negotiate, and it was not difficult to develop. The website, while initially primitive, was created literally overnight with the aid of the increasingly large number of tools that facilitate building and maintaining websites for the uninitiated; after its quick launch, the site experienced rapid growth. The live launch and traffic catalyzed further development and collaboration with subject matter experts to quickly iterate multimodal technological solutions, including databases (eg, to store information regarding which hospitals are most in need of PPE), matching algorithms (eg, to match PPE donations with the closest hospital in need), and logistics capabilities (eg, to coordinate the manufacturing of PPE and delivery to hospitals).
Lessons
Our experience with #GetMePPE and GetUsPPE.org exemplifies the untapped potential of digital platforms to mobilize and enable a ready and willing public to alleviate some of the largest barriers faced by health care workers. The COVID-19 pandemic has illuminated the deficiencies of our health care supply chain, rendering traditional sources of support inadequate. Fortunately, digital literacy is increasing rapidly worldwide, and the general public is increasingly embracing digital media. However, the medical field has yet to take full advantage of this opportunity.
Social media is just one example of a digital opportunity for health care providers to help increase the quality and efficiency of health care [22]. Current use of social media by physicians is mostly one-way rather than interactive [23]. However, it is critical for health care providers and organizations to create and participate in websites. While social media is essential for raising public awareness and excitement, a website enables health care providers to action this momentum to manifest tangible benefits for themselves and their patients.
Conclusion
GetUsPPE.org is just one example of the successful use of digital tools not only to voice needs, such as those of people working on the front lines of a pandemic, but to mobilize available resources at a speed we have rarely seen before. This initiative has demonstrated the efficacy, reach, and speed of digital platforms; however, it by no means represents the potential the medical community could achieve with full support and buy-in from larger national organizations or the federal government. To date, we have taken a bottom-up, grassroots approach, operating in entrepreneurial fashion, often donating our personal time and resources. It is interesting to imagine what we could accomplish with formal support. In this time of unprecedented crisis and need, we health care professionals have a responsibility to do everything we can to offer the best possible care, including ensuring that we can continue serving our patients without sacrificing either our safety or theirs.
Abbreviations
- COVID-19
coronavirus disease
- PPE
personal protective equipment
- SARS
severe acute respiratory syndrome
Footnotes
Conflicts of Interest: All authors are volunteers for GetUsPPE, a subsidiary of AFFIRM Research. SH and MLR are directors of GetUsPPE. ALB reports receiving consulting fees from Aledade.
References
- 1.Gondi S, Beckman AL, Deveau N, Raja AS, Ranney ML, Popkin R, He S. Personal protective equipment needs in the USA during the COVID-19 pandemic. Lancet. 2020 May 23;395(10237):e90–e91. doi: 10.1016/S0140-6736(20)31038-2. http://europepmc.org/abstract/MED/32416784 .S0140-6736(20)31038-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glenza J. The Guardian. 2020. Mar 24, [2020-06-15]. Medical staff beg for masks on social media amid coronavirus crisis https://www.theguardian.com/world/2020/mar/24/coronavrirus-medical-staff-beg-for-masks-social-media .
- 3.@nytimes. 2020. Mar 19, [2020-06-06]. Doctors, nurses and others are rallying on social media with the hashtag #GetMePPE — a reference to personal protective equipment — to put pressure on elected leaders to get them more gear to guard against the coronavirus https://twitter.com/nytimes/status/1240634143266013185?lang=en .
- 4.@ChelseaClinton. 2020. Mar 24, [2020-06-15]. Healthcare workers are on the frontlines of #COVID19 every day & they don’t have the protective equipment they need to keep themselves, or us safe. If you are able to support the effort to #GetMePPE or make masks, please visit: http://getusppe.org & http://weneedmasks.org https://twitter.com/ChelseaClinton/status/1242528991485087744 .
- 5.GetUsPPE. [2020-06-15]. GetMePPE Petition https://getusppe.org/getmeppe/
- 6.GetUsPPE. [2020-06-15]. https://getusppe.org/
- 7.GetUsPPE. [2020-06-15]. Partners https://getusppe.org/partners .
- 8.Tack P, Victor J, Gemmel P, Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016 Oct 21;15(1):115. doi: 10.1186/s12938-016-0236-4.10.1186/s12938-016-0236-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Centers for Disease Control and Prevention. [2020-06-05]. CDC COVID Data Tracker https://www.cdc.gov/covid-data-tracker/
- 10.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 Feb 07;:1061–1069. doi: 10.1001/jama.2020.1585. http://europepmc.org/abstract/MED/32031570 .2761044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Centers for Disease Control and Prevention. 2019. [2020-04-06]. Strategies to Optimize the Supply of PPE and Equipment https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/
- 12.Fischer WA, Weber D, Wohl DA. Personal Protective Equipment: Protecting Health Care Providers in an Ebola Outbreak. Clin Ther. 2015 Nov 01;37(11):2402–2410. doi: 10.1016/j.clinthera.2015.07.007. http://europepmc.org/abstract/MED/26452427 .S0149-2918(15)00935-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weber DJ, Rutala WA, Schaffner W. Lessons learned: Protection of healthcare workers from infectious disease risks. Crit Care Med. 2010 Aug;38:S306–S314. doi: 10.1097/ccm.0b013e3181e69ebd. [DOI] [PubMed] [Google Scholar]
- 14.Ranney ML, Griffeth V, Jha AK. Critical Supply Shortages - The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic. N Engl J Med. 2020 Apr 30;382(18):e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 15.Chan-Yeung M. Severe acute respiratory syndrome (SARS) and healthcare workers. Int J Occup Environ Health. 2004;10(4):421–7. doi: 10.1179/oeh.2004.10.4.421. [DOI] [PubMed] [Google Scholar]
- 16.Beckman AL, Gondi S, Forman HP. Health Affairs. 2020. Mar 18, [2020-03-18]. How To Stand Behind Frontline Health Care Workers Fighting Coronavirus https://www.healthaffairs.org/do/10.1377/hblog20200316.393860/full/
- 17.GetUsPPE. [2020-06-06]. GetUsPPE India https://in.getusppe.org/
- 18.@mystifide. 2020. Mar 23, [2020-03-30]. It is terrible to say this, but if it comes to using sewn masks, might as well make one with extra filters. #covid4MDs #GetUsPPE https://twitter.com/mystifyde/status/1242130913254760448?s=20 .
- 19.@drdanchoi. 2020. Mar 21, [2020-03-30]. Wow @Target please set an example and redirect your ENTIRE national stock of N95 masks to hospitals for them to purchase Or if you want to generate some great PR, donate them! https://twitter.com/drdanchoi/status/1241562744807133185?s=20 .
- 20.@choo_ek. 2020. Mar 20, [2020-03-30]. From a friend in the emergency department at a major academic hospital. #GetMePPE #GetUsPPE https://twitter.com/choo_ek/status/1240909433032421376?s=20 .
- 21.American College of Emergency Physicians. 2020. Mar 14, [2020-03-30]. Two Emergency Physicians in Critical Condition https://www.acep.org/corona/covid-19-articles/a-statement-from-acep-president-william-jaquis-md-facep .
- 22.McGowan BS, Wasko M, Vartabedian BS, Miller RS, Freiherr DD, Abdolrasulnia M. Understanding the factors that influence the adoption and meaningful use of social media by physicians to share medical information. J Med Internet Res. 2012 Sep 24;14(5):e117. doi: 10.2196/jmir.2138. https://www.jmir.org/2012/5/e117/ v14i5e117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campbell L, Evans Y, Pumper M, Moreno MA. Social media use by physicians: a qualitative study of the new frontier of medicine. BMC Med Inform Decis Mak. 2016 Jul 15;16:91. doi: 10.1186/s12911-016-0327-y. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-016-0327-y .10.1186/s12911-016-0327-y [DOI] [PMC free article] [PubMed] [Google Scholar]


