Abstract
Background
The potential impact of the COVID-19 pandemic on population mental health is of increasing global concern. We examine changes in adult mental health in the UK population before and during the lockdown.
Methods
In this secondary analysis of a national, longitudinal cohort study, households that took part in Waves 8 or 9 of the UK Household Longitudinal Study (UKHLS) panel, including all members aged 16 or older in April, 2020, were invited to complete the COVID-19 web survey on April 23–30, 2020. Participants who were unable to make an informed decision as a result of incapacity, or who had unknown postal addresses or addresses abroad were excluded. Mental health was assessed using the 12-item General Health Questionnaire (GHQ-12). Repeated cross-sectional analyses were done to examine temporal trends. Fixed-effects regression models were fitted to identify within-person change compared with preceding trends.
Findings
Waves 6–9 of the UKHLS had 53 351 participants. Eligible participants for the COVID-19 web survey were from households that took part in Waves 8 or 9, and 17 452 (41·2%) of 42 330 eligible people participated in the web survey. Population prevalence of clinically significant levels of mental distress rose from 18·9% (95% CI 17·8–20·0) in 2018–19 to 27·3% (26·3–28·2) in April, 2020, one month into UK lockdown. Mean GHQ-12 score also increased over this time, from 11·5 (95% CI 11·3–11·6) in 2018–19, to 12·6 (12·5–12·8) in April, 2020. This was 0·48 (95% CI 0·07–0·90) points higher than expected when accounting for previous upward trends between 2014 and 2018. Comparing GHQ-12 scores within individuals, adjusting for time trends and significant predictors of change, increases were greatest in 18–24-year-olds (2·69 points, 95% CI 1·89–3·48), 25–34-year-olds (1·57, 0·96–2·18), women (0·92, 0·50–1·35), and people living with young children (1·45, 0·79–2·12). People employed before the pandemic also averaged a notable increase in GHQ-12 score (0·63, 95% CI 0·20–1·06).
Interpretation
By late April, 2020, mental health in the UK had deteriorated compared with pre-COVID-19 trends. Policies emphasising the needs of women, young people, and those with preschool aged children are likely to play an important part in preventing future mental illness.
Funding
None.
Introduction
COVID-19, caused by severe acute respiratory syndrome coronavirus 2, and measures taken to curb its spread, have profoundly affected every aspect of day-to-day life around the world. The UK Government's lockdown, implemented on March 23, 2020, stipulated severe restrictions on social contact, on the ability for many people to work, and greatly reduced access to services. Early indications suggest a serious impact on employment and livelihoods, income, and personal debt.1 Coupled with a substantial amount of worry about future insecurity,2 there are increasing concerns about the mental health sequelae of the pandemic in the UK.3 Policymakers, commissioners, and service providers need reliable information about mental health changes associated with the pandemic so that decisions are underpinned by knowledge of the scale of changes in population mental health, and who is most vulnerable to symptoms of mental distress.4
Evidence from around the world on change in population mental health potentially attributable to the COVID-19 pandemic has been limited by use of convenience samples, modified or unvalidated mental health measures, and a lack of comparable, pre-COVID-19 baseline data against which to measure change; either within individuals or across the population as a whole.5 One study found increased rates of psychological distress among US adults in April, 2020, compared with those in 2018, and that the increase was greatest in young people aged 18–24 years and women.6
Well described demographic effects on mental health such as sex, age, and socioeconomic resources, in addition to pre-pandemic life circumstances, are likely to remain important determinants of people's mental health during the pandemic.7 However, changes in mental health during the public health emergency might not be evenly distributed across the population.8 Effects pertinent to lockdown include acute financial strain (low income, unemployment), household dynamics (domestic violence, living alone or with young children not attending nursery or school),9 and having an underlying mental or physical health condition; specific effects include being a keyworker exposed to potential infection.10 For some people with high levels of socioeconomic security, the suspension of commuting, changes to education and work activities, and increased time with family potentially could have reduced stress and increased mental health and wellbeing. For others, anxieties about infection risk could be particularly high.11 WHO has emphasised concerns for older adults, especially those in isolation, and those with cognitive decline or dementia, who could become more anxious, angry, stressed, agitated, or withdrawn during the outbreak or while in quarantine.4
Research in context.
Evidence before this study
We searched PubMed and Google Scholar with the terms “mental*” or “psychiatr*” and “prevalence” and “COVID*” or “coronavirus” for articles in English published between Jan 1 and May 30, 2020. Nearly all studies identified used a non-probability sample design, focused on specific population subgroups (such as health professionals), relied on unvalidated mental health measures, or had no comparable pre-pandemic baseline data. One study was identified, which found increased rates of psychological distress among US adults, with increases greatest among young people and women.
Added value of this study
This is the first dataset to allow the change in UK mental distress attributable to the COVID-19 pandemic to be discerned, adjusting for previous long-term trends and demographic, socioeconomic, and health-related factors. The substantial increase in mental distress in the UK population has not affected all groups equally. Established health inequalities persist, with prevalence of mental distress higher in people with pre-existing health conditions, those living in low-income homes, and people of Asian ethnicity. Other sources of inequalities have widened, with pronounced increases in younger (but not older) age groups, and in women (but not men). New inequalities in mental distress have emerged, with those living with young children and those in employment at the start of the pandemic being at risk of larger increases in mental distress.
Implications of all the available evidence
Although COVID-19 presents the greatest physical health risk to older people, the mental health of the young might be disproportionately affected by transmission mitigation strategies and the pandemic response of governments. Similarly, a greater increase in mental distress among women widens established mental health inequalities and emphasises the importance of providers maintaining access to domestic violence and sexual and reproductive health services. Additionally, prioritising the availability of childcare is an urgent requirement. Mental distress in men might manifest differently, and this requires further investigation. These results reflect the UK situation after one month in lockdown. As furloughs turn into redundancies and mortgage holidays expire, the socioeconomic fallout on mental health inequalities might widen and increase and must be monitored closely, along with implementation of early mitigation strategies.
We did a secondary analysis of data from a national, longitudinal cohort study to test the hypothesis that psychological distress in people in the UK increased one month into the COVID-19 emergency to a greater extent than expected given previous annual trends since 2014. We hypothesised that the following groups would experience greater than expected deterioration in their mental health: younger and older people, women, ethnic minorities, those living without a partner, those living with children, keyworkers, those living in the poorest homes or who are unemployed, people in urban areas or regions first affected by COVID-19, and those with pre-existing health conditions.
Methods
Study design and participants
The UK Household Longitudinal Study (UKHLS; Understanding Society) is an ongoing panel survey of more than 40 000 households that began in 2009.12, 13 From April 23 to April 30, 2020, members of households who participated in either of the two most recent UKHLS data collections (Waves 8 or 9), who were older than age 16 years, were invited to complete the first wave of the COVID-19 web survey.14, 15 Invitations and reminders were sent via email, text message, or postal letter. The probability sample was drawn from postal addresses. In England, Wales, and Scotland, the samples were clustered and stratified; in Northern Ireland unclustered systematic random samples were drawn. Northern Ireland and areas in England, Scotland, and Wales with proportionately large migrant and ethnic minority populations were oversampled. All household members aged 16 or older in April, 2020, were invited to participate, except for those unable to make an informed decision as a result of incapacity, and those with unknown postal addresses or addresses abroad. Participants aged 16 years in April, 2020, were not eligible to complete the UKHLS at previous waves, but participated in the COVID-19 survey if they were from eligible households (ie, households with at least one respondent to Waves 8 or 9 of UKHLS). Monthly web surveys about the effect of the pandemic are being completed following the April, 2020, survey.
Understanding Society is an initiative funded by the Economic and Social Research Council and various government departments, with scientific leadership by the Institute for Social and Economic Research, University of Essex, and survey delivery by NatCen Social Research and Kantar Public. The research data are distributed by the UK Data Service. The University of Essex Ethics Committee has approved all data collection on Understanding Society main study and innovation panel waves. The study protocol was pre-registered on OSF Registries before any outcome data analysis.
Procedures and outcomes
Pre-COVID-19 measures were extracted for participants aged 16 years and older in Waves 6–9 (n=53 351) and participants were linked across waves. Previous waves were carried out annually from Jan 1, 2014, with most of the fieldwork taking place over the course of 2 years. Therefore, waves overlap in their data collection periods (eg, Wave 6: from Jan 1, 2014, to Dec 31, 2015; Wave 7: from Jan 1, 2015, to Dec 31, 2016). Data from previous waves were mainly collected via face-to-face interviews.
The 12-item General Health Questionnaire (GHQ-12) is a validated measure of non-specific mental distress in the past 2 weeks, which performs well in longitudinal samples.16 It was administered by self-completion in Waves 6–9 and as part of the COVID-19 web survey and covers symptoms such as difficulties with sleep, concentration, problems in decision making, strain, and feeling overwhelmed.
We examined two GHQ-12 measures in the analyses: a mean symptom score (indicating a central average for the population) as the primary outcome, and a binary threshold score (indicating the proportion of the population with a clinically significant level of distress) as a secondary outcome. For the mean, GHQ-12 items were scored as: 0, not at all; 1, no more than usual; 2, rather more than usual; or 3, much more than usual; a total score was derived for each wave (0–36). The threshold measure was derived by scoring the “not at all” and “no more than usual” responses as 0 and the “rather more than usual” and “much more than usual” responses as 1, summed to produce a total (range 0–12). The cutoff for the threshold measure was a score of 4 or more, as used on the Health Survey for England Official Statistics indicator.17
Demographic variables were extracted on gender (women and men), age (16–24, 25–34, 35–44, 45–54, 55–69, ≥70 years), ethnicity (White British, White non-British, Mixed, Asian, Black, Other), and geography (Wales, Scotland, Northern Ireland, and region of England). An indicator of urbanicity, based on population density, and classified as urban or rural, was extracted.
Socioeconomic variables were extracted from Waves 6–9 and analysed as lagged variables (ie, using data collected from the previous wave) to ensure temporal ordering. Total annual household income was estimated with the use of a prompt card and scaled according to the number and ages of people living in the household using a weight of 1 for the first adult in the household; 0·5 for each additional person aged 14 years or older; and 0·3 for each person aged 0–13 years. This measure of equivalised household income for each wave's sample was divided into quintiles for analysis. Employment status was categorised as: employed, unemployed, retired, and other economically inactive (ie, those not working and not looking for work, such as students, people unable to work for health reasons or disability, and carers).
Two aspects of the household structure were derived to identify whether the participant lived with a partner (yes or no) and the age of the youngest child living in the household (none; 0–5 years; 6–15 years).
Two further covariates collected during the COVID-19 web survey were examined. First, those who reported receipt of a letter from the National Health Service or Chief Medical Officer indicating that they had been identified as someone at risk of severe illness should they contract COVID-19, because they had an underlying disease or health condition; second, participants who reported being a key worker during the COVID-19 emergency.
Statistical analysis
The statistical analyses were done in three phases. The first describes the COVID-19 web-survey sample participants and their mental health, overall and by all the covariates considered in the analysis. The second consisted of repeated cross-sectional analyses to produce temporal trends in mean GHQ-12 score and prevalence in the population for people exceeding threshold GHQ-12 scores. These analyses were done on data pertaining to all participants aged 16 years and older. Mean GHQ-12 scores and prevalence were calculated according to UK financial year of interview, grouping individuals across waves. Financial year (from April 1, to March 31) was preferred over calendar year because data collection for Wave 9 had only a small fraction of observations in 2019 and estimates within this group would therefore be imprecise. Because of the small number of observations leading to less precise estimates, we excluded years 2019–20 (n=75 responses, six participants) and 2013–14 (n=5790 responses, 558 participants). Mean scores and prevalence values were presented graphically as point estimates at the midpoint of each financial year (Oct 1) and estimates from the COVID-19 web survey were presented at the median date of data collection (April 25, 2020). Estimates were produced for the whole population, and by combinations of gender and age-group stratifications.
The third analysis examined the effect of the pandemic on changes within an individual's mental health using fixed-effects regression. These models included only those who participated in the COVID-19 survey and who had responded to at least one previous survey. Individuals aged 16 or 17 years during the COVID-19 survey were not included in the third analysis because they would have no previous measurements against which to assess change over time. An indicator variable for GHQ-12 score during the COVID-19 emergency was constructed and fitted in a model with variables for calendar date of interview, parameterised as the number of years since the day of data collection, and included as a continuous variable and its squared term. Mean scores were used for the outcome measure, rather than fitting a fixed-effects model for a binary outcome indicator. This is because the fixed-effects model approach would further reduce the sample available for analysis because it would exclude those who had concordant responses over follow-up, affecting the statistical power and generalisability of the findings. The date variables captured time trends. A positive coefficient from the fixed-effects model indicates worsening mental distress associated with the COVID-19 pandemic and accounts for any existing trends in psychological distress that were already occurring over time. Interactions between the COVID-19 period indicator and ten pre-defined subgroups were fitted to investigate heterogeneity in the effect of the pandemic. Effect estimates are also reported by subgroup and the associated p values test the null hypothesis that there is no evidence for a difference in change associated with the pandemic between different subgroups of people. All significant interactions (p<0·05; two-sided) were included in a final model to investigate which had an independent influence. The adjusted coefficients are interpretable as the change within a subgroup, accounting for changes in overlapping subgroups. The factors adjusted for in the final model were: age, gender, household income, employment status, living with a partner, age of the youngest child in the household, and presence of an underlying health condition. All covariates had less than 1% missing data except for the GHQ-12 scores, which were positioned at the end of the web-survey, and which were missing for 4·2% of respondents. Those with missing values for variables were excluded from analysis.
A sensitivity analysis was done to check potential seasonality effects, given that pre-COVID-19 data were collected year-round, whereas the COVID-19 web survey was carried out during late April. For this analysis, the fixed-effect analysis was re-run on data pertaining to participants who had previous responses that fell in spring or summer months.
Analyses were carried out in Stata version 14 and graphs were produced using the R package ggplot. To take account of the weighting and the clustered and stratified design, the svy suite of commands was used. Cross-sectional weights were used for cross-sectional analysis of Waves 6–9, and a weighting variable was used for the longitudinal analysis, which adjusted for unequal selection probabilities and differential non-response to the COVID-19 web survey. As of May, 2020, this weight was released as a beta-version and slight future refinements of the weighting models are possible, but unlikely to have a substantial effect on results.14
Role of the funding source
There was no funding source for this study. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
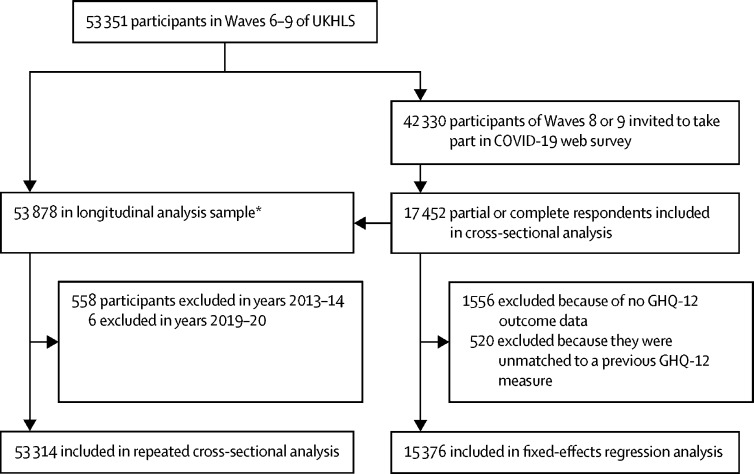
Waves 6–9 of the UKHLS had 53 351 participants, and 42 330 people from households that took part in Waves 8 or 9 were eligible for invitation to take part in the COVID-19 web survey. Web-survey interviews were completed (full and partial) by 15 835 of the 32 596 participants of Wave 9, representing a response rate of 48·6%. When also including those who took part in Wave 8 (but not Wave 9), 17 452 (41·2%) participated of the total sample of 42 330 (figure ). The COVID-19 web-survey sample comprised 17 452 participants, aged 16 years and older, weighted to be representative of the UK population (table 1 ), with the fixed-effects analyses based on those aged 18 years and older (median follow-up 5·3 years, IQR 4·6–5·8). Characteristics associated with non-response to the web-survey are provided in the appendix (p 1). Of the 17 452 participants, 1556 were excluded because of missing GHQ-12 outcome data, and 520 because they were unmatched to a previous GHQ-12 measure, with 15 376 included in the fixed-effects regression analysis.
Figure.
Flow chart showing selection into cohorts
GHQ-12=12-item General Health Questionnaire. UKHLS=UK Household Longitudinal Study. *An additional 527 participants who were age 16 years in April, 2020, or who had not previously responded to another survey wave were included in the longitudinal analysis.
Table 1.
COVID-19 web-survey sample profile and GHQ-12 responses
| Sample size | Unweighted profile | Weighted profile | Mean GHQ-12 score (95% CI) | Proportion with significant level of mental distress*(95% CI) | ||
|---|---|---|---|---|---|---|
| Total sample | 17 452 | 100% | 100% | 12·6 (12·5–12·8) | 27·3% (26·4–28·2) | |
| Gender | ||||||
| Women | 10 165 | 41·8% | 46·7% | 13·6 (13·4–13·8) | 33·3% (32·1–34·6) | |
| Men | 7287 | 58·4% | 53·3% | 11·5 (11·3–11·7) | 20·4% (19·1–21·6) | |
| Age, years | ||||||
| 16–24 | 1543 | 8·8% | 9·8% | 14·7 (14·1–15·3) | 36·7% (33·0–40·4) | |
| 25–34 | 1950 | 11·2% | 13·0% | 14·2 (13·7–14·7) | 35·0% (32·0–38·0) | |
| 35–44 | 2784 | 16·0% | 15·4% | 13·4 (13·0–13·8) | 30·6% (28·3–32·9) | |
| 45–54 | 3506 | 20·1% | 18·1% | 12·5 (12·2–12·8) | 26·3% (24·3–28·2) | |
| 55–69 | 5036 | 28·9% | 27·6% | 12·0 (11·8–12·3) | 24·7% (23·2–26·2) | |
| ≥70 | 2633 | 15·1% | 16·2% | 10·9 (10·6–11·1) | 17·6% (15·8–19·5) | |
| Ethnicity | ||||||
| White British | 14 029 | 80·4% | 86·9% | 12·5 (12·4–12·7) | 27·2% (26·3–28·2) | |
| White non-British | 779 | 4·5% | 4·2% | 13·1 (12·3–14·0) | 27·5% (23·0–32·0) | |
| Mixed | 284 | 1·6% | 1·3% | 13·7 (12·2–15·2) | 28·1% (20·2–36·0) | |
| Asian | 1281 | 7·3% | 4·4% | 13·7 (13·0–14·5) | 29·6% (25·2–34·1) | |
| Black | 392 | 2·2% | 1·8% | 12·7 (11·5–13·9) | 21·3% (14·6–28·0) | |
| Other | 87 | 0·5% | 0·5% | 13·7 (11·6–15·7) | 29·3% (13·2–45·3) | |
| Missing | 600 | 3·4% | 1·0% | .. | .. | |
| UK country or region | ||||||
| North East | 593 | 3·4% | 4·1% | 12·9 (12·2–13·7) | 28·9% (23·9–33·8) | |
| North West | 1716 | 9·8% | 11·1% | 12·1 (11·7–12·5) | 25·5% (22·8–28·1) | |
| Yorkshire | 1482 | 8·5% | 8·6% | 12·5 (12·1–13·0) | 25·8% (22·9–28·7) | |
| East Midlands | 1334 | 7·6% | 7·9% | 12·6 (12·1–13·2) | 27·2% (24·1–30·3) | |
| West Midlands | 1479 | 8·5% | 8·9% | 12·8 (12·3–13·3) | 29·5% (26·1–32·9) | |
| East of England | 1689 | 9·7% | 10·2% | 12·3 (11·8–12·7) | 24·9% (21·9–27·9) | |
| London | 1849 | 10·6% | 10·9% | 13·3 (12·8–13·8) | 29·3% (26·4–32·1) | |
| South East | 2428 | 13·9% | 14·5% | 12·5 (12·1–12·9) | 26·2% (23·8–28·6) | |
| South West | 1598 | 9·2% | 9·3% | 12·5 (12·0–13·0) | 28·1% (25·2–31·0) | |
| Wales | 1018 | 5·8% | 4·6% | 13·1 (12·4–13·9) | 28·3% (24·0–32·7) | |
| Scotland | 1523 | 8·7% | 7·8% | 12·9 (12·4–13·3) | 28·6% (25·5–31·7) | |
| Northern Ireland | 742 | 4·3% | 2·3% | 12·5 (11·5–13·5) | 28·5% (23·1–34·0) | |
| Missing | 1 | 0 | 0 | |||
| Residence† | ||||||
| Urban | 12 623 | 74·6% | 75·1% | 12·8 (12·6–13·0) | 28·0% (26·9–29·1) | |
| Rural | 4291 | 25·4% | 24·9% | 12·2 (11·9–12·4) | 25·1% (23·3–26·8) | |
| Missing | 538 | 3·1% | 0 | |||
| Equivalised household income quintiles† | ||||||
| Lowest | 2220 | 12·7% | 14·3% | 13·9 (13·4–14·3) | 32·3% (29·5–35·2) | |
| 2nd | 2692 | 15·4% | 18·1% | 12·8 (12·4–13·1) | 25·7% (23·5–27·9) | |
| 3rd | 3230 | 18·5% | 19·8% | 13·0 (12·6–13·X) | 29·3% (27·1–31·5) | |
| 4th | 3995 | 22·9% | 22·1% | 12·1 (11·8–12·4) | 25·2% (23·3–27·0) | |
| Highest | 4449 | 25·5% | 23·0% | 12·0 (11·7–12·2) | 25·7% (24·0–27·4) | |
| Missing | 866 | 5·0% | 2·7% | .. | .. | |
| Employment status† | ||||||
| Employed | 10 636 | 60·9% | 61·1% | 12·5 (12·3–12·7) | 27·1% (25·9–28·2) | |
| Unemployed | 446 | 2·6% | 3·4% | 15·0 (14·0–15·9) | 33·7% (27·5–39·9) | |
| Retired | 3770 | 21·6% | 21·6% | 11·1 (10·9–11·3) | 19·3% (17·7–20·9) | |
| Other inactive | 2062 | 11·8% | 13·8% | 15·3 (14·8–15·9) | 39·1% (36·2–42·1) | |
| Missing | 538 | 3·1% | 0·1% | 12·5 (12·3–12·7) | 27·1% (25·9–28·2) | |
| Lives with partner | ||||||
| Yes | 12 316 | 70·6% | 66·0% | 12·0 (11·9–12·2) | 24·3% (23·2–25·3) | |
| No | 5136 | 29·4% | 34·0% | 13·8 (13·6–14·1) | 33·1% (31·3–34·9) | |
| Age of youngest child in household | ||||||
| No children | 12 221 | 70·0% | 72·2% | 12·3 (12·2–12·5) | 25·9% (24·8–27·0) | |
| 0–5 years | 1756 | 10·1% | 9·0% | 13·7 (13·2–14·3) | 31·9% (28·7–35·1) | |
| 6–15 years | 3475 | 19·9% | 18·8% | 13·4 (13·0–13·7) | 30·3% (28·1–32·5) | |
| Keyworker | ||||||
| Yes | 4515 | 25·9% | 74·3% | 12·7 (12·4–12·9) | 29·9% (28·2–31·7) | |
| No | 12 928 | 74·1% | 25·7% | 12·6 (12·4–12·8) | 26·4% (25·3–27·4) | |
| Missing | 9 | 0·1% | 0 | .. | .. | |
| Received National Health Service shielding letter | ||||||
| Yes | 1007 | 5·8% | 6·6% | 13·7 (13·1–14·3) | 31·9% (27·9–35·8) | |
| No | 16 439 | 94·2% | 93·4% | 12·6 (12·4–12·7) | 27·0% (26·0–27·9) | |
| Missing | 6 | 0 | .. | .. | .. | |
Sample sizes are true (unweighted). All analyses are weighted, adjusting for complex survey design and non-response. GHQ-12=12-item General Health Questionnaire.
GHQ-12 scores exceeding threshold indicative of a potentially clinically significant level of mental distress (4 or more).
Measured during previous wave.
Between April 23 and April 30, 2020, the mean GHQ-12 symptom score for the population was 12·6 (95% CI 12·5–12·8), with 27·3% (26·4–28·2) exceeding the threshold score indicative of a clinically significant level of mental distress (table 1).
Mean GHQ-12 scores were higher for women (13·6, 95% CI 13·4–13·8) than for men (11·5, 11·3–11·7); and in younger age groups (16–24 years: 14·7, 14·1–15·3) than in older ones (≥70 years: 10·9, 10·6–11·1). Asian people had a higher mean score (13·7, 95% CI 13·0–14·5) than did White British people (12·5, 12·4–12·7); variation by other ethnic groups was not significant. Mean scores were higher in London (13·3, 95% CI 12·8–13·8) and among urban populations (12·8, 12·6–13·0) than in rural populations (12·2, 11·9–12·4).
Socioeconomic patterns were notable. Mean scores were 13·9 (95% CI 13·4–14·3) among those in households in the lowest income quintile and 12·0 (11·7–12·2) in the highest income homes. People who were unemployed (15·0, 95% CI 14·0–15·9) or economically inactive (15·3, 14·8–15·9) had higher scores than did those in employment (12·5, 12·3–12·7) or who were retired (11·1, 10·9–11·3). Key workers had a similar mean score to the rest of the population, but were more likely to exceed the clinically significant threshold score.
People not cohabiting with a partner (13·8, 95% CI 13·6–14·1) and those cohabiting with young children in the household (13·7, 13·2–14·3) also had high scores; as did those who received a shielding letter from the government because of a pre-existing health condition (13·7, 13·1–14·3).
Between April 23 and April 30, 2020, the mean score for the overall population was 12·6 (95% CI 12·5–12·8); higher than the mean scores in 2018–19 (11·5, 11·3–11·6), 2017–18 (11·4, 11·3–11·4), and for earlier waves (table 2 ). The increases were significant (as shown by their non-overlapping confidence intervals) in both women and men overall and in most age groups. Increases were steepest for women aged 16–44 years, and men aged 16–24 (appendix p 4).
Table 2.
Mean GHQ-12 scores from Waves 6–9 of UKHLS, and COVID-19 web survey, by year*
| 2014–15 (n=26 979) | 2015–16 (n=44 024) | 2016–17 (n=39 984) | 2017–18 (n=33 540) | 2018–19 (n=12 312) | April, 2020 (n=17 452) | ||
|---|---|---|---|---|---|---|---|
| Overall | 10·9 (10·8–10·9) | 10·9 (10·8–10·9) | 11·1 (11·1–11·2) | 11·4 (11·3–11·4) | 11·5 (11·3–11·6) | 12·6 (12·5–12·8) | |
| Gender | |||||||
| Women | 11·4 (11·3–11·5) | 11·4 (11·3–11·5) | 11·7 (11·6–11·8) | 11·9 (11·8–12·1) | 12·0 (11·8–12·2) | 13·6 (13·4–13·8) | |
| Men | 10·3 (10·2–10·4) | 10·3 (10·2–10·4) | 10·6 (10·5–10·7) | 10·7 (10·6–10·8) | 10·8 (10·6–11·1) | 11·5 (11·3–11·7) | |
| Age, years | |||||||
| 16–24 | 10·9 (10·6–11·1) | 10·8 (10·6–11·0) | 11·1 (10·8–11·3) | 11·6 (11·3–11·8) | 12·0 (11·6–12·5) | 14·7 (14·1–15·3) | |
| 25–34 | 11·0 (10·7–11·2) | 11·0 (10·8–11·2) | 11·4 (11·2–11·6) | 11·9 (11·6–12·2) | 12·1 (11·5–12·6) | 14·2 (13·7–14·7) | |
| 35–44 | 11·2 (11·0–11·40) | 11·2 (11·0–11·4) | 11·4 (11·2–11·6) | 11·7 (11·4–11·9) | 11·7 (11·3–12·1) | 13·4 (13·0–13·8) | |
| 45–54 | 11·3 (11·1–11·5) | 11·4 (11·2–11·5) | 11·7 (11·5–11·8) | 11·9 (11·7–12·1) | 12·0 (11·6–12·4) | 12·5 (12·2–12·8) | |
| 55–69 | 10·6 (10·5–10·8) | 10·7 (10·6–10·8) | 11·0 (10·8–11·1) | 11·2 (11·0–11·3) | 11·2 (10·9–11·5) | 12·0 (11·8–12·3) | |
| ≥70 | 10·2 (10·0–10·4) | 10·2 (10·0–10·3) | 10·4 (10·3–10·6) | 10·2 (10·1–10·4) | 10·1 (9·8–10·3) | 10·9 (10·6–11·1) | |
Data are mean GHQ score (95% CI). 53 314 total participants. Sample sizes are true (unweighted). All analyses are weighted, adjusting for complex survey design and non-response. GHQ-12=12-item General Health Questionnaire. UKHLS=UK Household Longitudinal Study.
Based on financial year, from April to March.
During late April, 2020, more than a quarter (27·3%; 95% CI 26·3–28·2) of the population reported a GHQ-12 score that indicated a clinically significant level of mental distress (table 3 ). Although a steady upward trend had already been evident over recent years (from 16·7%, 95% CI 16·1–17·3 in 2014–15 to 18·9%, 17·8–20·0 in 2018–19), a marked step-change increase occurred in 2020 (appendix p 5). Particularly steep increases were evident in young people and in women; for example, 44·0% (95% CI 39·2–48·9) of women aged 16–24 reported clinically significant distress in April, 2020, compared with 32·0% (27·5–36·5) in 2017–18 (appendix p 2).
Table 3.
Proportion of participants with a clinically significant level of mental distress, by year*
| 2014–15 (n=26 979) | 2015–16 (n=44 024) | 2016–17 (n=39 984) | 2017–18 (n=33 540) | 2018–19 (n=12 312) | April, 2020 (n=17 452) | ||
|---|---|---|---|---|---|---|---|
| Overall | 16·7% (16·1–17·3) | 16·9% (16·4–17·4) | 18·2% (17·7–18·8) | 19·0% (18·4–19·6) | 18·9% (17·8–20·0) | 27·3% (26·3–28·2) | |
| Gender | |||||||
| Women | 19·4% (18·7–20·2) | 19·8% (19·1–20·5) | 21·0% (20·3–21·7) | 22·4% (21·6–23·3) | 23·0% (21·5–24·5) | 33·3% (32·0–34·6) | |
| Men | 13·7% (12·9–14·5) | 13·8% (13·1–14·4) | 15·2% (14·5–15·9) | 15·3% (14·5–16·1) | 14·5% (13·0–16·0) | 20·4% (19·1–21·7) | |
| Age, years | |||||||
| 16–24 | 19·8% (18·0–21·6) | 19·6% (18·2–21·0) | 19·7% (18·2–21·3) | 23·5% (21·7–25·3) | 24·5% (21·3–27·8) | 36·7% (32·9–40·5) | |
| 25–34 | 18·1% (16·4–19·8) | 18·3% (16·8–19·7) | 20·5% (18·9–22·2) | 21·7% (19·7–23·6) | 21·6% (18·1–25·1) | 35·0% (31·9–38·2) | |
| 35–44 | 18·3% (16·8–19·8) | 18·1% (16·9–19·4) | 19·2% (17·9–20·5) | 19·9% (18·3–21·5) | 21·0% (18·4–23·7) | 30·6% (28·2–33·0) | |
| 45–54 | 18·3% (17·0–19·6) | 18·8% (17·7–19·9) | 20·0% (18·8–21·2) | 20·5% (19·1–21·9) | 21·5% (18·9–24·0) | 26·3% (24·3–28·2) | |
| 55–69 | 14·8% (13·8–15·8) | 15·2% (14·3–16·1) | 16·5% (15·6–17·5) | 17·7% (16·6–18·8) | 17·0% (15·1–18·8) | 24·7% (23·2–26·3) | |
| ≥70 | 12·9% (11·7–14·1) | 12·8% (11·8–13·8) | 14·6% (13·5–15·7) | 12·9% (11·8–14·0) | 10·8% (9·1–12·4) | 17·6% (15·7–19·5) | |
Data are proportion of participants with a clinically significant level of mental distress (95% CI). 53 314 total participants. Sample sizes are true (unweighted). All analyses are weighted, adjusting for complex survey design and non-response.
Based on financial year, from April to March.
Table 4 presents the results of the fixed-effects regression analyses. The adjusted model controls for variables that were significantly associated with change in GHQ score in unadjusted analyses (p<0·05): age, gender, household income, employment status, living with a partner, age of the youngest child in the household, and presence of an underlying health condition. Overall, GHQ-12 scores were 0·48 points (95% CI 0·07 to 0·90) greater than would have been expected had trends observed in the years before the COVID-19 pandemic continued. There was clear evidence, after adjustment, for heterogeneous effects by age and gender (both effect modifiers, p<0·0001). The mean score in 18–24-year-olds was 2·69 points (95% CI 1·89 to 3·48) higher than would have been expected from the trends observed before the pandemic, and in 25–34-year-olds was 1·57 points (0·96 to 2·18) higher. Adjusted estimates indicated that women experienced an increase of 0·92 points (95% CI 0·50 to 1·35) whereas there was no evidence of higher than expected scores for men (0·06, −0·37 to 0·48). Living with children in the house significantly modified the effect (p=0·0003): those with children younger than 5 years had a 1·45 (0·79 to 2·12) point increase in GHQ-12 score after adjustment for other factors. After adjustment, there was evidence of a difference in effect according to employment status (p=0·0037), such that being either in employment (0·63, 95% CI 0·20 to 1·06), or retirement (0·73, 0·24 to 1·21) before the pandemic were associated with greater than expected increases in scores, whereas being unemployed (−0·48, −1·55 to −1·60) or otherwise inactive (−0.19, −0.80 to 0.43) were not.
Table 4.
Fixed-effects regression analysis showing the within-person change in GHQ-12 score associated with the pandemic, compared with preceding trends
|
Unadjusted |
Adjusted* |
||||
|---|---|---|---|---|---|
| Change in GHQ-12 score (95% CI) | p value† | Change in GHQ-12 score (95% CI) | p value† | ||
| Total | 0·48 (0·07 to 0·90) | .. | .. | .. | |
| Gender | |||||
| Women | 0·88 (0·45 to 1·31) | <0·0001 | 0·92 (0·50 to 1·35) | <0·0001 | |
| Men | 0·03 (−0·40 to 0·45) | .. | 0·06 (−0·37 to 0·48) | .. | |
| Age, years | |||||
| 18–24 | 2·21 (1·51 to 2·91) | <0·0001 | 2·69 (1·89 to 3·48) | <0·0001 | |
| 25–34 | 1·61 (1·01 to 2·21) | .. | 1·57 (0·96 to 2·18) | .. | |
| 35–44 | 0·78 (0·25 to 1·31) | .. | 0·53 (−0·03 to 1·10) | .. | |
| 45–54 | 0·04 (−0·44 to 0·52) | .. | 0·08 (−0·41 to 0·58) | .. | |
| 55–69 | −0·21 (−0·66 to 0·23) | .. | −0·02 (−0·47 to 0·43) | .. | |
| ≥70 | 0·05 (−0·39 to 0·49) | .. | 0·17 (−0·33 to 0·68) | .. | |
| Ethnicity | |||||
| White British | 0·47 (0·06 to 0·89) | 0·35 | .. | .. | |
| Non-white British | 0·71 (0·10 to 1·33) | .. | .. | .. | |
| Urbanicity | |||||
| Urban | 0·52 (0·10 to 0·95) | 0·29 | .. | .. | |
| Rural | 0·37 (−0·07 to 0·82) | .. | .. | .. | |
| Equivalised household income quintiles‡ | |||||
| Lowest | 0·63 (0·07 to 1·20) | 0·025 | 0·68 (0·12 to 1·25) | 0·0008 | |
| 2nd | 0·37 (−0·14 to 0·87) | .. | 0·29 (−0·21 to 0·79) | .. | |
| 3rd | 0·56 (0·08 to 1·04) | .. | 0·45 (−0·03 to 0·93) | .. | |
| 4th | 0·28 (−0·19 to 0·74) | .. | 0·26 (−0·20 to 0·73) | .. | |
| Highest | 0·80 (0·36 to 1·25) | .. | 0·90 (0·45 to 1·35) | .. | |
| Employment status‡ | |||||
| Employed | 0·63 (0·21 to 1·06) | <0·0001 | 0·63 (0·20 to 1·06) | 0·0037 | |
| Unemployed | −0·07 (−1·12 to 0·9) | .. | −0·48 (−1·55 to 0·60) | .. | |
| Retired | 0·07 (−0·36 to 0·51) | .. | 0·73 (0·24 to 1·21) | .. | |
| Other inactive | 0·68 (0·10 to 1·26) | .. | −0·19 (−0·80 to 0·43) | .. | |
| Lives with a partner | |||||
| Yes | 0·33 (−0·09 to 0·75) | 0·0021 | 0·60 (0·13 to 1·06) | 0·48 | |
| No | 0·78 (0·32 to 1·25) | .. | 0·48 (0·06 to 0·90) | .. | |
| Age of youngest child in household | |||||
| No children | 0·27 (−0·15 to 0·69) | <0·0001 | 0·33 (−0·09 to 0·75) | 0·0003 | |
| 0–5 years | 1·73 (1·11 to 2·35) | .. | 1·45 (0·79 to 2·12) | .. | |
| 6–15 years | 0·74 (0·24 to 1·25) | .. | 0·81 (0·28 to 1·34) | .. | |
| Keyworker | |||||
| Yes | 0·46 (0·00 to 0·92) | 0·80 | .. | .. | |
| No | 0·50 (0·08 to 0·91) | .. | .. | .. | |
| Underlying health conditions | |||||
| Yes | −0·03 (−0·72 to 0·66) | 0·050 | 0·40 (−0·30 to 1·09) | 0·66 | |
| No | 0·53 (0·12 to 0·95) | .. | 0·53 (0·12 to 0·94) | .. | |
Sample sizes are true (unweighted). All analyses are weighted, adjusting for complex survey design and non-response. GHQ-12=12-item General Health Questionnaire. 15 376 participants included in fixed-effects regression analysis.
Adjusted for all other predictors of change that had p<0·05 in the unadjusted analysis.
p value for test of heterogeneity of effect across subgroups.
Lagged variables (measured during previous wave).
There was some variation in score increase by household income (p=0·0008), although no clear trend was discernible. Other characteristics tested (ethnicity, urbanicity, living with a partner, having an underlying health condition, and being a key worker) did not independently predict differences in effect. In the sensitivity analysis done on 9294 participants, which restricted previous data to spring or summer months (from April 1 to August 31) the overall change associated with the COVID-19 emergency increased to 1·13 (95% CI 0·39–1·86).
Discussion
This study is among the first national probability sample studies to track temporal changes in population mental health from before the COVID-19 pandemic and into the subsequent lockdown period. Consistent with our hypothesis, we found an overall increase in mental distress in people aged 16 years and older in the UK compared with in the previous year: mean population GHQ-12 score increased from 11·5 (95% CI 11·3–11·6) in 2018–19 to 12·6 (12·5–12·8) in April, 2020. This increase in population mental distress was not simply a continuation of previous upward trends: we estimate that the average score was 0·48 points higher than would have been expected had trajectories from 2014–19 continued.
This higher than projected increase in mental distress did not affect all groups equally, with people in some demographic subgroups showing little (or no) additional mental distress after lockdown, while other subgroups showed marked increases. The factors that we hypothesised would be most strongly linked with mental health deterioration were those associated with pre-existing health inequalities, such as gender, age, and low income, and factors specific to the unique circumstances of societal lockdown such as household dynamics, being a keyworker, and having a pre-existing health condition. Our findings suggest that being young, a woman, and living with children, especially preschool age children, have had a particularly strong influence on the extent to which mental distress increased under the conditions of the pandemic. Although rates of mental distress were higher in people who, before lockdown, were unemployed or in other economically inactive roles such as being a full-time student, the increase in mental distress relative to previous trends was greater among those who were employed before the pandemic. Some in this group will have lost their jobs, seen their income plummet, been furloughed, attempted to shift to homeworking, or been required to work in ways that exposed them to COVID-19 infection. As of late April, 2020, we found no clear pattern of variation in change by income group. However, consistent with established patterns, mental distress was more common among people living in low-income households.
Contrary to our hypothesis, we did not find a significant additional independent increase in an individual's change in mental distress because of the COVID-19 pandemic according to other pre-existing characteristics. These characteristics included being an ethnic minority, living without a partner, being a keyworker, being unemployed, living in an urban area, or having a pre-existing health condition that would put a person at greater risk from infection with COVID-19. For these categories, established pre-pandemic inequalities in mental health were maintained, but they had not significantly increased by the end of the first month of the lockdown period. However, we are of the opinion that had this analysis been done further into the lockdown period or afterward, perhaps after 6 months, socioeconomic inequalities would widen because of the probable recession resulting from COVID-19.
To our knowledge, this is one of the first national general population probability sample studies to emerge using a reliable measure of mental health with pre-pandemic baseline data enabling the long-term tracking of population mental health before and during COVID-19. The participant characteristics in the modelling were mostly measured before the pandemic, and the mental health outcome was measured during the pandemic. Our analyses identified which characteristics were associated with a subsequent decline in mental health under pandemic conditions. However, although the UKHLS is a high-quality probability sample cohort study, response to the COVID-19 wave questionnaire was less than 50%, and varied by age, gender, ethnic group, health status, and other characteristics (appendix p 1). Non-response was adjusted for via application of survey weights, but attrition remains a potential source of bias.
The GHQ-12 is a screening tool and, although it correlates strongly with presence of mental illness as well as future clinical diagnosis of a psychiatric disorder, and a high score threshold was applied (four or more) for the analysis of prevalence, it is not a clinical assessment. This limitation means that, for example, the notable proportion (44%, 95% CI 39·2–48·9) of women aged 16–24 years who reported clinically significant scores during April, 2020, should be interpreted with caution and does not mean that nearly half of young women in the population require treatment for a mental illness. The GHQ-12 underestimates both socioeconomic and ethnic disparities.18 Furthermore, mental distress in men could be more likely to manifest in ways not captured by the GHQ-12, including alcohol misuse.
Although the sample was large, it was underpowered to detect change for some groups. Specifically, a major limitation was the lack of scope to examine significant change by different ethnic groups, and for men and women separately within ethnic groups, particularly when considering the high prevalence of mental distress evident in the descriptive analysis. We found some evidence in mean scores of widening inequalities for both ethnic minorities and those in lowest income quintiles. However, within-person adjusted analyses did not find significant effects for these characteristics.
Between Wave 9 and the COVID-19 survey, necessary changes were introduced in the mode of the questionnaire administration that could have affected reporting: in Wave 9 the GHQ-12 was self-completed with the interviewer present as part of a face-to-face interview, whereas the COVID-19 questionnaire was completed online. Future data collection by telephone with those unable or unwilling to complete the survey online will be forthcoming, but these data were not yet available for this analysis, which could have introduced bias. Finally, no contemporaneous control group was available so we cannot rule out secular changes, aside from those predicted from previous data, which would have occurred anyway. Therefore, we cannot unequivocally rule out other ecological drivers of change in mental health that might have influenced our results. However, given the acute nature and degree of change, we are of the opinion that the changes that we have in population mental health are probably largely attributable to the virus and events associated with the pandemic.
The initial increase in mental distress in the UK population one month after lockdown might represent a so-called spike in emotional response that stabilises or falls as people adjust; an idea already described in several non-probability surveys.19, 20, 21 Opposite trends might also develop as differences in people's reactions to crisis become apparent.
Certain groups experienced higher mental distress than did others, indicating persistence of ethnic and socioeconomic health inequalities. Some experienced higher than expected increases in mental distress, which widened pre-existing age and gender inequalities. However, some inequalities decreased—for example, those in employment pre-pandemic experienced a marked deterioration in their mental health. Although we did not see larger than expected increases in mental distress associated with poverty, our findings do suggest that overall pre-existing inequalities in mental health have widened.
This study identifies groups in the population that had a high prevalence of psychological distress before the pandemic. As the economic consequences of lockdown develop, when furloughs turn to redundancies, mortgage holidays expire, and recession takes effect, we believe it is reasonable to expect not only sustained distress and clinically significant deterioration in mental health for some people, but emergence of well described long-term effects of economic recession on mental health including increasing suicide rates22 and hospital admissions23 for mental illness.24
Women, young people, and those with preschool aged children are experiencing the greatest increase in mental distress. This supports results of previous reports of high prevalence of common mental disorder and self-harm in girls and women aged 16–24 years;7, 25, 26, 27 while Marmot28 made a pressing case for tackling health inequalities for women in poverty. The COVID-19 pandemic has produced many new challenges for health research, policy, and service provision.3 The problems for mental health from COVID-19 and governmental responses to the pandemic are not necessarily new; instead, pre-existing mental health inequalities could become more entrenched and tackling them might be even more challenging. The pandemic has brought people's differing life circumstances into stark contrast: access to outside and inside space, household crowding, lack of school provision and childcare, food insecurity, domestic violence, addiction, access to internet and maintenance of social connectivity, as well as economic reserves are all relevant to mental health.9, 10, 29, 30 An appropriate, proportionate response to mitigate and manage additional needs requires more high-quality information to be included in public health messaging about mental health during the pandemic, alongside adequately resourced services.4, 31
Data sharing
The data used are publicly available via UK Data Service repository (study numbers 6614 and 8644), and do not require ethical assessment for academic research purposes.
Acknowledgments
Acknowledgments
We are grateful to the excellent work and commitment to open science of the UK Household Longitudinal Study (UKHLS) survey team, as well as to the participants who continue to cooperate, some for several decades. The UKHLS (also known as Understanding Society) is funded by the Economic and Social Research Council and the Health Foundation. Fieldwork for the survey is carried out by Ipsos MORI and Kantar. Understanding Society is an initiative funded by the Economic and Social Research Council and various government departments, with scientific leadership by the Institute for Social and Economic Research, University of Essex. The research data are distributed by the UK Data Service.
Contributors
KMA and SMcM devised the study concept. MP wrote the initial analysis plan with input from all authors. MP carried out data analysis and produced figures. KMA, MP, and SMcM wrote the first draft of the manuscript and all authors contributed to editing and commenting on the final version.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Joyce R, Xu X. The Institute for Fiscal Studies; London: 2020. Sector shutdowns during the coronavirus crisis: which workers are most exposed? IFS Briefing Note. [Google Scholar]
- 2.Office for National Statistics Coronavirus and the social impacts on Great Britain. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandthesocialimpactsongreatbritain/7may2020
- 3.Holmes EA, O'Connor RC, Perry VH. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO Mental health and psychosocial considerations during COVID-19 outbreak. 2020. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_22020
- 5.Pierce M, McManus S, Jessop C. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7:567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020 doi: 10.1001/jama.2020.9740. https://doi.org.10.1001/jama.2020.9740 published online June 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McManus S, Bebbington PE, Jenkins R. Data resource profile: Adult Psychiatric Morbidity Survey (APMS) Int J Epidemiol. 2020;49:361. doi: 10.1093/ije/dyz224. 62e. [DOI] [PubMed] [Google Scholar]
- 8.Benzeval M, Burton J, Crossley T. The Institute for Fiscal Studies; Colchester: 2020. The idiosyncratic impact of an aggregate shock: the distributional consequences of COVID-19. [Google Scholar]
- 9.Andrew A, Cattan S, Dias MC. Institute of Fiscal Studies; London: 2020. How are mothers and fathers balancing work and family under lockdown? [Google Scholar]
- 10.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368 doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 11.Townsend E, Nielsen E, Allister R, Cassidy SA. Key ethical questions for research during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:381–383. doi: 10.1016/S2215-0366(20)30150-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.University of Essex. Institute for Social and Economic Research. NatCen Social Research. Kantar Public . 12th edn. UK Data Service; Essex: 2019. Understanding Society: Waves 1–9, 2009–2018 and Harmonised BHPS: Waves 1–18, 1991–2009. [Google Scholar]
- 13.Jäckle A, Gaia A, Al Baghal T, Burton J, Lynn P. University of Essex; Colchester: 2017. Understanding society—The UK Household Longitudinal Study, innovation panel, Waves 1–9, user manual. [Google Scholar]
- 14.Institute for Social and Economic Research . University of Essex; Colchester: 2020. Understanding Society COVID-19 user guide version 1·0. [Google Scholar]
- 15.University of Essex. Institute for Social and Economic Research . 1st edn. UK Data Service; Essex: 2020. Understanding Society: COVID-19 Study, 2020. [Google Scholar]
- 16.Pevalin DJ. Multiple applications of the GHQ-12 in a general population sample: an investigation of long-term retest effects. Soc Psychiatry Psychiatr Epidemiol. 2000;35:508–512. doi: 10.1007/s001270050272. [DOI] [PubMed] [Google Scholar]
- 17.Neave A. Office of National Statistics; London: 2017. Health Survey for England, 2016—NHS Digital. [Google Scholar]
- 18.Bowe A. The cultural fairness of the 12-item General Health Questionnaire among diverse adolescents. Psychol Assess. 2017;29:87–97. doi: 10.1037/pas0000323. [DOI] [PubMed] [Google Scholar]
- 19.Fancourt D, Steptoe A, Bu F. Trajectories of depression and anxiety during enforced isolation due to COVID-19: longitudinal analyses of 59 318 adults in the UK with and without diagnosed mental illness. medRxiv. 2020 doi: 10.1101/2020.06.03.20120923. published online June 4. (preprint). [DOI] [Google Scholar]
- 20.McBride O, Murphy J, Shevlin M. An overview of the context, design and conduct of the first two waves of the COVID-19 Psychological Research Consortium (C19PRC) Study. PsyArXiv. 2020 doi: 10.31234/osf.io/z3q5p. published online June 11, 2020. (preprint). [DOI] [Google Scholar]
- 21.YouGov Britain's mood, measured weekly. 2020. https://yougov.co.uk/topics/science/trackers/britains-mood-measured-weekly
- 22.Barr B, Taylor-Robinson D, Scott-Samuel A, McKee M, Stuckler D. Suicides associated with the 2008–10 economic recession in England: time trend analysis. BMJ Br Med J. 2012;345 doi: 10.1136/bmj.e5142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gunnell D, Appleby L, Arensman E. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang S-S, Stuckler D, Yip P, Gunnell D. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ Br Med J. 2013;347 doi: 10.1136/bmj.f5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bebbington PE, McManus S. Revisiting the one in four: the prevalence of psychiatric disorder in the population of England 2000–2014. Br J Psychiatry. 2020;216:55–57. doi: 10.1192/bjp.2019.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McManus S, Gunnell D, Cooper C. Prevalence of non-suicidal self-harm and service contact in England, 2000–14: repeated cross-sectional surveys of the general population. Lancet Psychiatry. 2019;6:573–581. doi: 10.1016/S2215-0366(19)30188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sadler K, Vizard T, Ford T. Mental health of children and young people in England, 2017. 2018. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2017/2017 [DOI] [PubMed]
- 28.Marmot M. The Institute of Health Equity; London: 2020. Health Equity in England: the Marmot review 10 years on. [DOI] [PubMed] [Google Scholar]
- 29.Cable N, Sacker A. Validating overcrowding measures using the UK Household Longitudinal Study. SSM - Popul Heal. 2019;8 doi: 10.1016/j.ssmph.2019.100439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abel KM, Heuvelman H, Rai D. Intelligence in offspring born to women exposed to intimate partner violence: a population-based cohort study. Wellcome Open Res. 2019;4:107. doi: 10.12688/wellcomeopenres.15270.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;4:317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used are publicly available via UK Data Service repository (study numbers 6614 and 8644), and do not require ethical assessment for academic research purposes.