Abstract
The recent outbreak of the coronavirus disease (COVID-19) is causing a shortage of personal protective equipment (PPE) in different countries around the world. Because the coronavirus can transmit through droplets and aerosols, facemasks and N95 respirators that require complex certification, are urgently needed. Given the situation, the U.S. Centers for Disease Control and Prevention (CDC) recommends that “in settings where facemasks are not available, healthcare personnel might use homemade masks (e.g., bandana, scarf) for the care of patients with COVID-19 as a last resort.” Although aerosols and droplets can be removed through the fibers of fabrics through a series of filtration mechanisms, their filtration performances have not been evaluated in detail. Moreover, there are a series of non-medical materials available on the market, such as household air filters, coffee filters, and different types of fabrics, which may be useful when facemasks and respirators are not available. In this study, we comprehensively evaluated the overall and size-dependent filtration performances of non-medical materials. The experiments were conducted under different face velocities to study its influence on size-dependent filtration performances. The flow resistance across these filter materials is measured as an indicator of the breathability of the materials. The results illustrate that multiple layers of household air filters are able to achieve similar filtration efficiencies compared to the N95 material without causing a significant increase in flow resistance. Considering that these air filters may shed micrometer fibers during the cutting and folding processes, it is recommended that these filters should be inserted in multiple layers of fabrics when manufacturing facemasks or respirators.
Keywords: Homemade facemasks, Respirators, Filter materials, Household air filter, Filtration efficiency, Aerosols
Highlights
-
•
Agencies suggest the manufacturing of homemade face masks during COVID-19.
-
•
This work examined a wide range of non-medical materials for their filtration performance.
-
•
We studied the influences of face velocity, number of filter material layers, and the size-dependent filtration efficiency.
-
•
Several layers of household air filters can achieve similar filtration performance compared to N95 materials.
-
•
The information will be crucial for healthcare personnel and the general public in manufacturing homemade face masks.
1. Introduction
Due to the 2019 coronavirus disease (COVID-19) outbreak, the global demand for personal protective equipment (PPE) has surged and created a severe shortage across the world (CDC, 2020). It is especially the case for facemasks and respirators, as they can minimize the inhalation or spread of droplets and aerosols. Respirators are devices designed to reduce the exposure to airborne contaminants, and therefore require a tight seal. Facemasks, however, do not have a tight seal between the face and the facemask, but wearing facemasks can reduce the spread of aerosols and droplets from the wearer. Facemasks and respirators are crucial for protecting healthcare personnel (HCP) and immune-compromised people from the virus (Adhikari et al., 2020; Bowdle and Munoz-Price, 2020; Milton et al., 2013). Given the situation, the Centers for Disease Control and Prevention (CDC) recommends a few strategies for optimizing the supply of facemasks. Specifically, under the circumstance when no facemasks cleared by the U.S. Food and Drug Administration (FDA) are available, the mitigating options include using high-efficiency particulate air (HEPA) filters to generate particle-free air, or manufacturing homemade masks as a last resort (CDC, 2020). The homemade masks can be made of non-medical materials, including “bandana and scarf,” which are mentioned in the strategies. The CDC further noted that “however, homemade masks are not considered PPE, since their capability to protect HCP is unknown.” These non-medical materials can also be integrated into existing respirators as filter materials. 3D printing has the potential to produce respirators with high repeatability and quality control and may be used to alleviate the shortage of PPE in remote communities (as shown in Fig. S1). The 3D-printed respirator requires a filter material to be inserted at its front to remove droplets and aerosols from the ambient air. At the same time, the 3D-printed respirator is regarded as an alternative for N95 respirator, which needs to follow fit test guidelines (OSHA, 2003). Given the shortage of certified medical filter supplies, the filter materials also need to be selected from non-medical sources that are easily accessible through the market.
As a core component of the facemask and respirator, the filter materials need to achieve a high efficiency in particle removal and a low flow resistance to ensure breathability. Candidate non-medical materials may include household air filters, coffee filters, activated carbon filters, and various types of fabrics, such as bandana, scarf, and bedsheets. However, few existing studies have comprehensively assessed the effectiveness of these non-medical materials in particle filtration, creating uncertainties in the choice of filter materials. The dataset on the filtration performance of non-medical materials is also urgently needed, so that mitigation strategies can be used when medical supplies are unavailable.
The performance of the filter material is characterized by its filtration efficiency, i.e., the percentage of particles filtered by the material (Hinds, 1999), and its flow resistance across the filter material, which decides breathability. We can use Darcy's equation under turbulent regime and Hagen–Poiseuille equation under the laminar regime to calculate the pressure drop across a filter for fluid flow through porous media, where it linearly increases with the thickness of the filter material and the superficial filtering velocity (Cooper and Alley, 2010). Airborne particles are removed by filtration through mechanisms of impaction, interception, diffusion, and electrostatic interaction (Hinds, 1999). Impaction and interception are effective for removing particles with larger sizes (>1 μm), while diffusion is most effective for removing particles with smaller sizes (<100 nm) (Friedlander, 2000). This feature results in an “escape window” where particles with hundreds of nanometers can penetrate through the filter, resulting in lower efficiencies. Existing literature also uses the term “most penetrating particle size (MPPS)” to describe the reduced filtration efficiency in this size range (Podgorski et al., 2006). According to the classification of filter materials, medical masks and household air filters use electrostatic interactions to filter particles in addition to the general mechanisms of impaction, interception, and Brownian diffusion. These materials have the potential to remove particles more efficiently while maintaining a relatively low flow resistance. Household fabrics belong to fabric filters, which mainly rely on low permeabilities of the materials to collect aerosols via general mechanisms of impaction, interception, and Brownian diffusion, and may result in a high flow resistance. Therefore, it is hypothesized that the performance of fabrics will not be comparable to the electret filter materials used in commercial medical filters and household air filters.
The overall filtration efficiency of a filter is calculated by dividing the concentration of particles collected via filter media by that of total particles. Therefore, the overall efficiency may depend on the size distribution of the introduced aerosols and does not differentiate the performance of the filter for particles with different sizes. However, as the virus may be carried by aerosols with different sizes, the size-dependent filtration efficiency of the filter materials needs to be carefully examined. For example, the widely used “N95” respirator is required to provide a filtration efficiency of at least 95% for 0.3 m particles when subjected to careful testing (FDA, 2019). To demonstrate the capabilities of non-medical filter materials in removing ambient aerosols and potentially virus particles, we need to examine both the size-dependent and overall filtration efficiencies.
Due to its extensive usage in building air purification, household air filters have been comprehensively examined by manufacturers and previous researchers (Alderman et al., 2008; Fazli et al., 2019; Payet et al., 1992; Wallace, 2006; Wallace and Howard-Reed, 2002; Wallace et al., 2004). Different rating systems, such as microparticle performance rating (MPR), minimum efficiency reporting value (MERV), and filter performance rating (FPR) are created to consider the filtration performance for particles in different size ranges. The certification of these filters may be done by the manufacturer and by a professional as a part of a complete system test according to guidelines (ASHRAE, 1996). However, these air filters are not designed for homemade facemasks, and the face velocities through the filters may significantly vary when they are used as facemask materials. One issue associated with these household air filter materials is their biocompatibility, where fiber fragments may be generated after a long period of usage and inhaled by wearers. Two fabric layers can be placed front and back the filter material to avoid the spreading of these large debris, allowing the usage of these non-medical filter materials as medical filters.
Household fabrics were evaluated in a few studies, although the specifications of the fabrics were not provided in detail. Jung et al. (2014) compared the filtering efficiencies of masks and handkerchiefs commonly used by the general public to protect against particulate air pollution, and found that the average filtration efficiency per mask type ranged from 99% for quarantine masks to 2% for handkerchiefs. In a similar study, Mueller et al. (2018) discovered that the filtration efficiency for folded bandana range from 18 to 40%, while that of handkerchief is around 23% (Mueller et al., 2018). To consider this particle leakage associated with different mask-wearing configurations, studies also used a mannequin head for testing. Filtration efficiencies of 33–78% for surgical masks, 65% for cloth masks, 10–60% for household fabrics were reported (Bowen, 2010; Rengasamy and Eimer, 2011; Shakya et al., 2017). The issue associated with these studies on fabrics as homemade facemask material is that the specifications of the fabrics are not directly comparable. According to the mechanism of filtration, the fiber diameter, fiber material, and filter permeability determine the interactions between the fibers and particles. To isolate the influence of different fabric specifications on their filtration performance, we used the thread count, i.e., the number of horizontal and vertical threads per square inch, as the parameter to study the filtration performance of the fabrics.
In this study, we comprehensively measured the size-dependent and overall filtration efficiency of non-medical filter materials under a range of face velocities. The flow resistances across the filter materials as a function of the number of filter layers and face velocities were examined. The filtration performances of the non-medical materials were compared against medical counterparts such as N95, KN95 (equivalent of N95 in China, GB2626-2006), and earloop facemask materials. The derived results will help communities where certified facemasks are urgently needed and in severe shortage.
2. Methods
2.1. Experimental setup
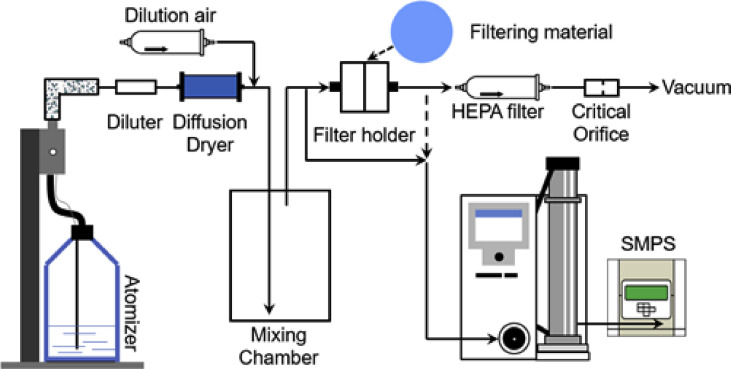
Fig. 1 shows a schematic diagram of the experimental setup. The test aerosols were generated by a constant output atomizer (Model 3076, TSI Inc.) nebulizing a NaCl-water solution with a mass concentration of 0.1%. The atomizer generated aerosols at a flow rate of 3.0 L per minute (lpm). The aerosols were first diluted by an inline diluter and then dried by a homemade diffusion dryer. Afterward, the aerosols, together with a stream of filtered make-up air, were introduced to a mixing chamber. The homogeneous aerosols were then directed into a filter holder (Air Sampling Cassette, Zefon International Inc.), where the disc-shaped filter material was firmly pressed onto mesh support and sealed at the edge. The filter material was cut to discs with a diameter of 37 mm. The flow rate through the filter material was determined by the face velocity, which, on the other hand, decided by the breathing flow rate. In general, the breathing flow rate may vary between 10 and 60 lpm depending on the age, gender, and motion status of a person (Hinds, 1999; Becquemin et al., 1991; Grinshpun et al., 2009). The testing condition employed by the National Institute for Occupational Safety and Health (NIOSH) uses a face velocity of 5.3 cm s−1 (NIOSH, 2007). However, given the variabilities of breathing flow rates, common facemask, respirators, and filter materials have been tested under a wide range of face velocities, ranging from 5.3 cm s−1 to 26 cm s−1 (Rengasamy et al., 2010; Konda et al., 2020; Li et al., 2012). In this study, we examined the filtration performance of the filter materials under face velocities of 23.2, 15.3, and 9.2 cm s−1 to consider a wide range of breathing conditions. We used higher face velocities than that used by NIOSH to allow for the consideration of exercising conditions and the conditions where the wearer may press the nose and mouth area to ensure a tight sealing between the filter material and the face. These three face velocities correspond to a flow rate of 15, 10, and 6 lpm through the 37 mm filter material. A scanning mobility particle sizer (SMPS, Model 3936, TSI Inc.) measured the mobility size distributions of aerosols upstream and downstream of the filter holder. The SMPS sampled aerosols at a flow rate of 1 lpm, so the rest of the flow (14, 9, or 5 lpm) through the filter holder was maintained by a critical orifice. As a make-up flow, filtered dilution air was introduced to the system downstream of the diffusion dryer.
Fig. 1.
A schematic diagram of the experimental setup of this study.
The SMPS system is equipped with a differential mobility analyzer (DMA, Model 3081, TSI Inc.) that classifies particles in the range between 10 and 600 nm, and a condensation particle counter (CPC, Model 3750) that measures the concentration of the mobility-classified particles. The size distribution of aerosols () is obtained by scanning the voltage that is applied to the DMA. Similar to a previous work (Li et al., 2018), the size-dependent filtration efficiency () is calculated by
| (1) |
where and are the size distributions measured at the outlet (downstream) and inlet (upstream) of the filter holder. Based on the size distributions, we can also evaluate the overall number-based filtration efficiencies. The particle size distributions are first integrated over the measured size range to calculate the total number (), where
| (2) |
The overall number-based filtration efficiencies () are calculated by
| (3) |
where and are the total number concentrations of aerosols at the outlet and inlet of the filter holder. The SMPS system also monitored the pressures upstream and downstream of the filter, which could be used to calculate the pressure drop across the filter materials. It should be noted that the number of viruses in an aerosol at the point of generation is more likely dependent on the volume of that aerosol, meaning that the filtration efficiencies at larger sizes may be of more importance (Woo et al., 2010; Damit et al., 2014; Zuo et al., 2015). However, once emitted, aerosols with different sizes may be subject to different evolution processes, such as evaporation, deposition, and decay of microorganisms, and the relationship between the number of viable viruses and aerosol size is still not well understood. Therefore, we still reported the number-based filtration efficiencies, similar to previous filtration studies (Rengasamy et al., 2010; Konda et al., 2020).
2.2. Filter materials
In this study, four types of medical filter materials and thirteen types of non-medical filter materials were evaluated. Some materials were assessed in multiple layers to study the effect of the number of layers (or filter thickness) on filtration efficiency and flow resistance. A total number of 43 combinations of filter materials were examined under the three different face velocities (23.2, 15.3, and 9.2 cm s−1). Table 1 lists the information of the filter materials and the tests that have been performed.
Table 1.
Information on the non-medical materials and the tests conducted.
| Filter type | Brand | Model | Layers | Acronym | |
|---|---|---|---|---|---|
| N95 | 3M | 8210 | 1 | N95 | 5.76 |
| KN95 | NIDI | 3D Mask | 1 | KN95-N | 4.62 |
| KN95 | Jinjiang | GW2049 | 1 | KN95-J | 5.90 |
| Surgical (earloop) | Walgreens | N/A | 1 | Sg | 2.92 |
| Household air filter | 3M | 1900 MPR | 1–2 | H19 | 3.67 |
| Household air filter | 3M | 2500 MPR | 1–4 | H25 | 5.71 |
| Household air filter | BestAir | 3000 MPR | 1–8 | H30 | 7.20 |
| Vacuum Bag | Hoover | N/A | 1 | VB | 3.09 |
| Coffee Filter | Natural Brew | N/A | 3 | NB-3 | 0.29 |
| Coffee Filter | Brew Rite | N/A | 3 | BR-3 | 0.34 |
| Activated Carbon | API | Coarse | 1 | CC | 1.14 |
| Activated Carbon | API | Fine | 1 | FC | 1.22 |
| Bandana | Levi | Men's Cotton | 1–4 | B | 0.37 |
| Scarf | Wander Agio | Warm Long | 1–4 | S | 1.10 |
| Pillowcase | Cal Design Den | 400 TC | 1–4 | P4 | 0.34 |
| Pillowcase | Cal Design Den | 600 TC | 1–4 | P6 | 0.38 |
| Pillowcase | Cal Design Den | 1000 TC | 1–4 | P10 | 0.46 |
In this study, the N95 filter material was used as a reference for filter performance. Two KN95 filter materials and a surgical mask material were evaluated and compared against N95 material. We also examined three types of household air filters, each with a different microparticle performance rating (MPR). The rating system was developed and mainly used by 3M to quantify the air filter's ability to capture aerosols from 0.3 to 1 μm in size from the air passing through the filter. The MPR values in this study can be used as references when choosing air filters in the market. The activated carbon filter (fine ground and coarse ground) was combined with one layer of the household 2500 MPR filter. The two types of coffee filters, each combined into three layers, and one layer of the vacuum bag were used for evaluation. In the testing of the fabrics, we evaluated the filtration performance of a cotton bandana, a woolen yarn scarf, and several pillowcases. The pillowcases are manufactured by the same company, but with different thread counts (TC) to study how the quality of the fabrics affects the filtration performance. Certain materials were tested with varying layers to promote filtration efficiency. For simplicity, Table 1 also lists the acronyms of the tested materials, showing both the type of the material and the layers being tested.
The performance of the filter material is a function of the filtration efficiency and the flow resistance through the filter. Better filter materials have a higher filtration efficiency (lower penetration efficiency) and a lower pressure drop. Following the convention of Hinds (1999), the filter quality, , is calculated for each type of the filter, using the equation
| (4) |
where is the penetration efficiency of particles (), and is the pressure drop across the filter. Based on this definition, filters with better performances, i.e., higher filtration efficiency and lower pressure drop, will have higher values of .
3. Results and discussion
3.1. Comparison of different filter materials
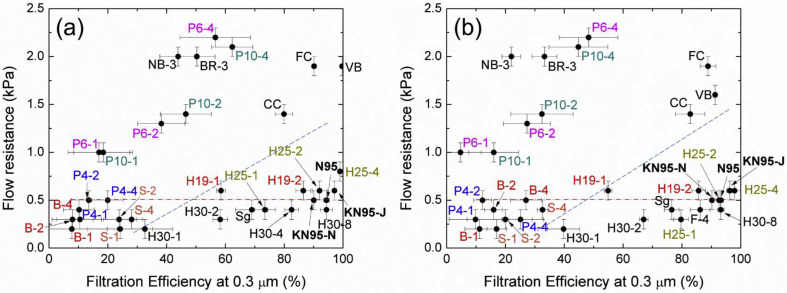
We first examined the performance of the medical and non-medical materials in their filtration efficiencies for 0.3 μm particles and their overall efficiencies. Fig. 2 a, 2c, and 2d show the efficiencies and flow resistances at face velocities of 23.2, 15.3, and 9.2 cm s−1, respectively. Filters with better performances generate data points at the bottom right corners of the figures. Fig. 2b further shows the overall filtration efficiencies and flow resistances measured at the face velocity of 23.2 cm s−1. A comparison between Fig. 2a and 2b did not demonstrate significant changes in the data point locations, meaning that different methods for calculating the filtration efficiencies will not significantly influence the performance of the filter materials. However, according to Eq. (2), the overall filtration efficiency is dependent on the size distribution of the test aerosols. The evaluation of filter performance based on overall number-based filtration efficiency may be biased for filters with higher filtration efficiencies in the size range where the test aerosols are most concentrated. Therefore, we follow the convention of using the filtration efficiency at 0.3 μm as an indicator of the filter performance.
Fig. 2.
Filtration efficiency at 0.3 μm, overall number-based filtration efficiency, and corresponding pressure drops of the tested medical and non-medical filter materials. (a) Filter pressure drop and filtration efficiency for 0.3 μm particles measured at a face velocity of 23.2 cm s−1; (b) Filter pressure drop and overall filtration efficiency measured at a face velocity of 23.2 cm s−1; (c) Filter pressure drop and filtration efficiency for 0.3 μm particles measured at a face velocity of 15.3 cm s−1; (d) Filter pressure drop and filtration efficiency for 0.3 μm particles measured at a face velocity of 9.2 cm s−1. Dashed lines mark the approximate boundary between fibrous and fabric filters.
At a face velocity of 23.3 cm s−1, N95 material has filtration efficiencies of 94.4% for 0.3 μm particles and 93.3% for the test aerosols overall, while the pressure drop is 0.5 kPa KN95 materials have similar performances compared to the N95 material, but the surgical mask material provides a filtration efficiency of 73.4% for 0.3 μm particles. Using N95 material as a reference, we can identify several non-medical materials that have similar performance. For example, four layers of air filter (2500 MPR), two layers of air filter (1900 MPR), and eight layers of air filters (3000 MPR) provide filtration efficiencies of 99.0%, 92.0%, and 94.4% for 0.3 μm particles at pressure drops of 0.6, 0.5, and 0.4 kPa. Finer activated carbon filter and vacuum bag produce filtration efficiencies of 90.2% and 93.0% for 0.3 μm particles, similar to that of N95, but the pressure drop is significantly larger (2.0 and 1.6 kPa). Coffee filters provide moderate filtration efficiencies of around 50% for 0.3 μm particles, but the pressure drop is significantly higher than most of the other materials.
Compared to the more efficient commercialized medical and household air filters, all of the tested fabrics showed much lower filtration efficiencies, with below 60%. A scarf or bandana is not able to remove aerosols efficiently, even after multiple layers were stacked. For example, four layers of a scarf or a bandana only provide filtration efficiencies of 28.1% or 7.1% for 0.3 μm particles. These filtration efficiencies are not acceptable for removing airborne particles. It should be noted that different fabrics may have different specifications, such as fiber diameter, thickness, permeability, and fiber material, resulting in different filtration performance. In this study, we use the thread count as the parameter to relate the fabric property to the filtration performance. Our results suggest that fabrics with denser weaving patterns are able to provide a higher filtration efficiency. For example, four layers of 1000, 600, and 400-thread count pillowcases generate filtration efficiencies of 55.0%, 44.6%, and 19.9%, respectively. We should also note that particles can also be removed by fabrics through electrostatic interaction with fabric fibers. Therefore, fabrics made of polyester, glass, and silk materials may remove aerosols more efficiently than cotton fabrics (Perumalraj, 2016). The measurement also shows that the filtration efficiency and flow resistance increase with the number of layers used for testing. However, the slope of the correlations between the flow resistance and the number of layers in the filter is different for materials, which is a result of different filter permeabilities.
At reduced face velocities of 15.3 cm s−1 (Fig. S2a) and 9.2 cm s−1 (Fig. S2b), the flow resistance across the filters reduced significantly, and this trend is in agreement with Darcy's equation or Hagen–Poiseuille equation. Meanwhile, there is a general trend that the filtration efficiencies at 0.3 μm increase with decreasing face velocity, which may result from the longer residence time of particles in the filter. However, as shown in Section 3.3, there is not a simple correlation between face velocity and filtration efficiency, because the removal of particles under different face velocities is strongly size-dependent.
Fig. 2 and S2 shows that fibrous and fabric filters separate into two regimes in the flow resistance-filtration efficiency plot. This separation is labeled with blue dashed lines in the figure, where data to the left of the blue dashed line correspond to fabric filters, and data to the right correspond to fibrous filters. The red dot-dashed lines mark the flow resistance of the N95 materials. According to ATSM standard F2100-11 (ASTM, 2020), the flow resistance is required to be below 5 mm H2O/cm2 for medical facemasks at a testing flow rate of 8 lpm, corresponding to a total pressure drop of 107 Pa. Fig. S2(b) (6 lpm) shows that most of the tested materials satisfy this standard. Using Eq. (4), we calculated the filter quality of the test materials, and the results are listed in Table 1. Note that our calculation shows that for filter materials with multiple layers, the filter quality gradually increases with the number of layers used in the material. In general, the filter quality should be independent on the number of layers, since filter quality is designed to eliminate the effect of thickness for filters made by the same material. However, the influence of packing should also be considered when multiple layers are stacked. Our observation is likely caused by the change of filter fiber orientations in different layers or improvement of packing structure (Hinds, 1999; Zhang et al., 2010; Yun et al., 2010). Studies also show that the loading of particles on existing layers may also affect the filter quality (Przekop and Gradoń, 2008). Therefore, Table 1 lists the highest filter quality values only. Fibrous filters generally have better filter quality, due to the removal of aerosols through the additional electrostatic interactions. Fabrics with a higher thread count generally have a better filter quality. Using the filter quality as a metric, we can observe that household air filters are potential candidates for homemade mask materials. Among the fabric filter materials, the vacuum bag showed good filter quality. However, the large flow resistance associated with the flow through the vacuum bag limits its application in homemade masks due to the significantly enhanced flow resistance and reduced breathability. Coffee filters showed the least filter quality among these materials.
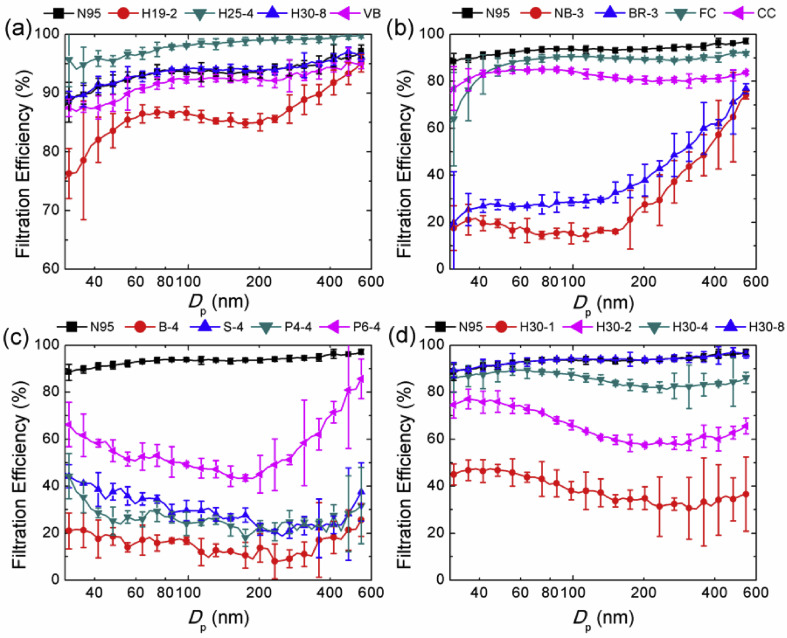
3.2. Size-dependent filtration efficiency
The size-dependent filtration efficiency is essential to the filtration performance, and previous studies used this metric to evaluate the performance of common filter materials (Stafford and Ettinger, 1972; Hanley et al., 1994; Rengasamy et al., 2008; He et al., 2015; Fazli et al., 2019). Fig. 3 shows the size-dependent filtration efficiencies of the selected non-medical materials and comparison against the N95 material. These filters yield satisfactory filtration efficiencies for droplets and larger particles. Almost all the test materials show an “escape window” between 100 and 400 nm. Because common respiratory virus (e.g., flu virus and coronavirus), which rarely exist as individual virions in the air but typically attached to airborne particles, has a size between 20 and 400 nm (Almeida and Tyrrell, 1967; Lakdawala et al., 2011; Shangguan et al., 1998; Zhu et al., 2020), it is possible that the virus-containing aerosols can penetrate through this “escape window” and further transmit through the human respiratory system.
Fig. 3.
(a-c) Size-dependent filtration efficiencies of non-medical materials and comparison against N95 material. (d) The influence of air filter (3000 MPR) layer number on the size-dependent filtration efficiency. Measurements were made under a face velocity of 23.2 cm s−1.
Household air filters typically have better filtration performances, as shown in Fig. 3a. At a face velocity of 23.2 cm s−1, the filtration efficiencies are above 70% at all sizes. Eight layers of air filter (F-8) have almost the identical size-dependent filtration efficiency as that of N95, while its pressure drop (0.4 kPa) is lower than that of N95 (0.5 kPa). Four layers of the household air filter (H-4, 2500 MPR) has superior filtration efficiency than N95 material at all different sizes, but its pressure drop (0.6 kPa) is slightly higher than N95. Vacuum bag (VB) also has a similar filtration efficiency compared to N95, but its pressure drop, 1.6 kPa, is much higher. It can be observed that household air filters show reduced filtration efficiencies for particles below 80 nm, which was also observed in a previous study (Fazli et al., 2019). It is likely because of the low charge fraction and insufficient induced dipole effects for these ultrafine particles. These household air filters generally have high permeability, so when the electrostatic effect is not adequate, the removal of ultrafine particles by these materials is not as efficient as materials with lower permeability. Coffee filters and activated carbon filters have lower size-dependent filtration efficiencies compared to that of N95 (Fig. 3b). The coffee filters (NB and BR) show significantly high flow resistance under the face velocity of 23.2 cm s−1. The activated carbon filters have relatively high filtration efficiencies for submicron aerosols, and finer activated carbon particles (FC) provide a better filtration performance.
As for the fabrics (Fig. 3c), the size-dependent filtration efficiencies are significantly lower than that of N95, again demonstrating the insufficiency of using fabrics as homemade masks. The bandana, scarf, and 400 thread count pillowcase have size-dependent filtration efficiency values below 40%. However, if the fabrics are the only resources of non-medical materials for homemade facemasks, we should choose more densely woven fabrics that have higher thread counts (see P6-4 vs P4-4), or use multiple layers of fabrics.
Fig. 3d shows the size-dependent filtration efficiency of the household air filter (3000 MPR, H30) with different numbers of layers. Comparing Fig. 3d with Fig. 3c, it can be seen that a single layer of air filter is already much more efficient in removing aerosols than most of the fabrics. Therefore, given the high filtration efficiency of multi-layer air filter and low pressure drops of both the air filter and fabrics, a layer-by-layer stacking combination of fabrics and household air filter may achieve both high filtration performance (i.e. filtration efficiency and breathability) and good biocompatibility, where the debris from the air filter can be collected by the fabrics. Fig. 3 also shows that a filter that has a higher filtration efficiency at 0.3 μm performs consistently better at all sizes within the test range. This is likely because the filter with better performance has larger filter thickness and lower permeability, which is beneficial for removing both smaller particles by Brownian diffusion and larger particles by impaction and interception.
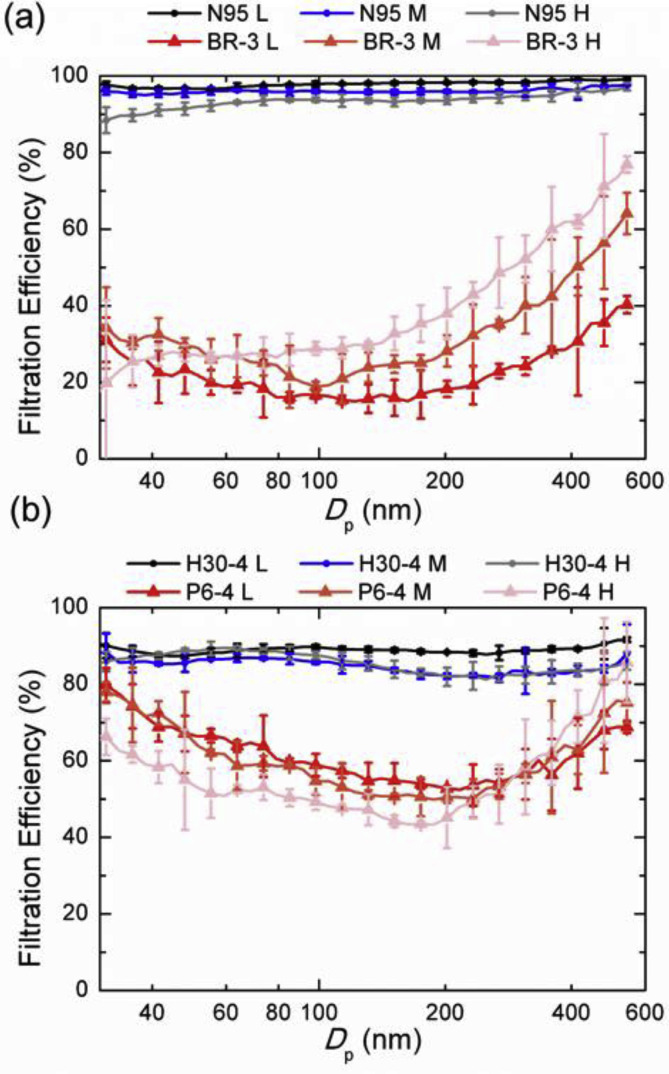
3.3. Influence of face velocity
In this study, we tested the filter materials under three different face velocities (23.2, 15.3, and 9.2 cm s−1) (Fig. 4 ). At an inhaling flow rate of 60 lpm, the face velocities correspond to filtering areas of 111, 67, and 43 cm2, respectively. Fibrous and fabric filters showed different patterns in their dependence on face velocity. For fibrous filters, such as N95 and household air filters (3000 MPR), the filtration efficiency decreases with increasing face velocity. This decrease in filtration efficiency appeared at all tested sizes. However, for fabric filters, such as BR coffee filter and folded pillowcase (600 thread count, 4 layers), the enhanced face velocity led to decreased filtration efficiency for particles with smaller sizes (e.g., below 100 nm) and increased filtration efficiency for particles with larger sizes (e.g., above 200 nm).
Fig. 4.
Influence of face velocity on the size-dependent filtration performances of the filter materials: (a) N95 and Brew rite coffee filters (3 layers) and (b) household air filter (3000 MPR, 4 layers) and 600 thread count pillowcases (4 layers). L, M, and H correspond to face velocities of 9.2, 15.3, and 23.2 cm s−1.
These different dependence of filtration performances on face velocity are likely a result of the balance between the residence time of particles in the filter and particle filtration mechanisms. Most of the fibrous filter materials are made of electrets, which retain electrostatic charges to enhance the collection of particles through electrostatic force and induced dipole effects. It should be noted that these fibrous filters often have a relatively smaller flow resistance, meaning that the residence time of particles in the filter is mainly determined by the face velocities. Under this situation, a reduced residence time of particles will lead to less particle collection. As for fabric filters, the significantly enhanced flow resistance is a result of the low permeability of the filter materials. This low permeability leads to a considerably increased velocity of particles through the pores of the materials, leading to further reduction of particle residence time. However, the removal of larger particles likely benefited from this enhanced velocity, promoting the impaction and interception of particles on the filter fibers. As for particles with smaller sizes, the filtration efficiency will further decrease because the particle residence time is not long enough for particle collection via Brownian motion, which agrees the previous studies (Stafford and Ettinger, 1972; Rengasamy et al., 2010; Leung et al., 2010).
Therefore, the materials of the filter will largely determine the filtration efficiencies. A larger flow resistance does not necessarily lead to a higher filtration efficiency. Fibrous filters are able to achieve both a lower flow resistance that facilitates the flow through the materials, and a high collection efficiency of particles through the Brownian motion, interception, impaction, and electrostatic interaction. The increase of the flow resistance through these fibrous filters, resulting from the enhanced face velocities, will lead to a reduced residence time of particles in the filter and a reduction of filtration efficiency. Whereas for fabric filters, the increase of flow resistance will lead to an enhanced filtration efficiency of larger particles due to the enhanced impaction and interception, while the filtration efficiency of smaller particles will decrease.
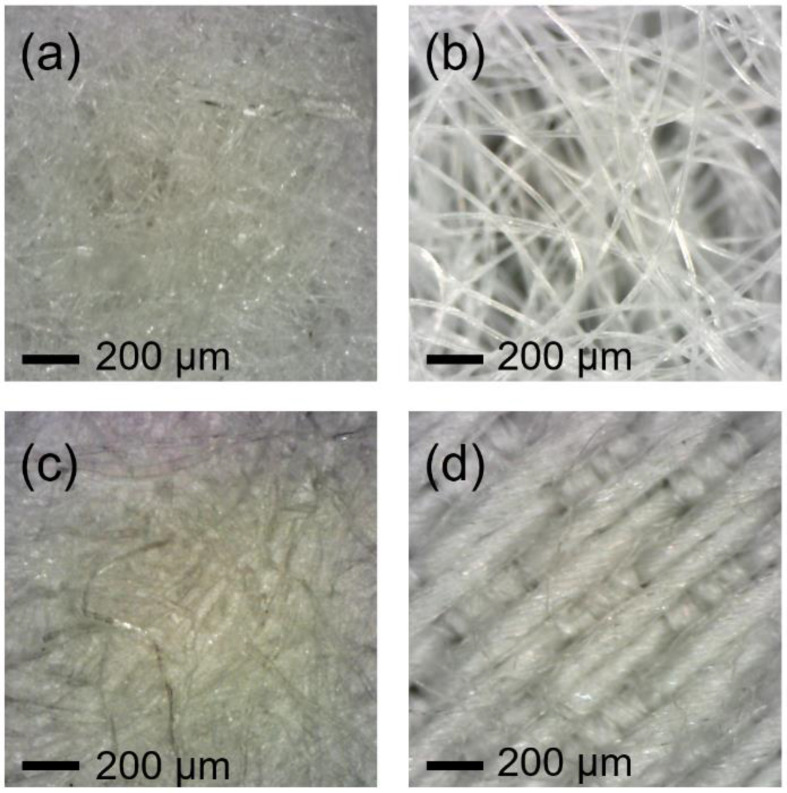
We further examined the microscopic structures of the tested filter materials examined in Fig. 4, and the images are shown in Fig. 5 . It confirms that fibrous filters typically have higher permeability and thinner fiber. Fabric filter materials, on the other hand, are less permeable and composed of wider fibers. Similar features were also observed in an earlier study on cloth masks (Neupane et al., 2019). The lower permeability of the fabric filters leads to drastic changes in the particle velocity in the filter and different size-dependent filtration features under different face velocities. Additional microscopic images of the fabric materials and the corresponding filtration performance are displayed in Fig. S3.
Fig. 5.
Microscope images of filter materials: (a) N95; (b) household air filter (3000 MPR); (c) Brew Rite coffee filter; and (d) 600 thread count pillowcase.
3.4. Non-medical materials for homemade masks
Our study shows that fabrics, such as scarfs, bandanas, and pillowcases, are insufficient to remove aerosols in the size range (30–600 nm) where SARS-CoV-2 may be attached onto (Liu et al., 2020). However, we should note that droplets are a significant mode of transmission for SARS-CoV-2 (WHO, 2020), and many fabrics are helpful in capturing larger respiratory droplets by inertial impaction. Although folding the fabrics can enhance the filtration efficiencies, the values are still not comparable to those of commercialized household air filters and medical materials. Furthermore, the significantly increased flow resistance after folding or stacking will lead to difficulty in breathing and the leakage of airflow from the sides of the homemade masks.
Household air filters can remove aerosols efficiently at a relatively low flow resistance. The issues associated with using these filter materials is that they may shed fibers during the cutting and bending of the materials. These fibers, typically in size range of 0.5–2 μm, can be inhaled if the materials are in direct contact with the wearer, and may further cause respiratory diseases (Shannon et al., 2005). However, our study shows that folded fabric materials can be relatively efficient in collecting particles above 0.5 μm through impaction and interception (Fig. 4b). Therefore, a “sandwich” structure of the fabric and fibrous filters, with fibrous filters inserted inside the layers of fabric materials, may serve as an approach for the general public to manufacture homemade masks when medical supplies are urgently needed but in severe shortage.
We should also note that the certification of facemasks and respirators requires additional evaluation processes. For example, surgical masks should address additional health risks (FDA, 2018), such as inadequate fluid resistance, inadequate barrier for bacteria, flammability, and inadequate respiratory barrier for bacteria. Respirators should also satisfy requirements in bacterial filtration, flammability (Rengasamy et al., 2018), and biocompatibility (FDA, 2020). In this study, we evaluated the flow resistance and particle filtration only. The remaining aspects will be examined in our future studies.
4. Conclusions
In this study, we examined the performance of a wide range of non-medical materials as candidates for medical filters. By evaluating four types of medical materials and thirteen types of non-medical materials (43 combinations of filter configurations), each under three different face velocities, we found that fibrous filters, such as household air filters, can achieve a filtration efficiency and flow resistance similar to that of N95 mask materials. Fabrics, such as a scarf, bandana, and pillowcases with different thread counts, are relatively inefficient for collecting aerosols while inducing a large pressure drop, which may lead to difficulty in breathing. Moreover, we observed a positive relationship between the thread count of the fabrics and the filtration efficiencies. The difference between the fibrous and fabric materials is that fibrous materials could further remove aerosols with electrostatic mechanisms. This additional mechanism allows an adequate removal of aerosols at a relatively large permeability of the filter materials. Based on the results, we recommend manufacturing homemade facemasks with a combination of fibrous and fabric materials to guarantee the sufficient removal of aerosols and avoid the inhaling of fiber fragments generated during the cutting and folding of the fibrous filters. If fibrous materials are unavailable, fabric materials need to be folded with multiple layers to enhance filtration efficiency. However, the wearer needs to ensure the sealing between the mask and face, as the flow resistance associated with these folded fabrics are relatively high.
Acknowledgments
The authors acknowledge the helpful discussions with Christopher Ramsay, Jennifer Nixon, Eric Schnider, Andrew Gerth, Thomas Hoing, Keyton Rovka, and others in the Missouri S&T face shield and facemask manufacturing team. The authors also want to thank Dr. Brian Kreite at Phelps Health and Bond Clinic for helpful suggestions. This work is partly supported by the US National Science Foundation (NSF) 2027571.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijheh.2020.113582.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Adhikari S.P., Meng S., Wu Y.-J., Mao Y.-P., Ye R.-X., Wang Q.-Z., Sun C., Sylvia S., Rozelle S., Raat H. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect. Dis. Poverty. 2020;9:1–12. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderman S.L., Parsons M.S., Hogancamp K.U., Waggoner C.A. Evaluation of the effect of media velocity on filter efficiency and most penetrating particle size of nuclear grade high-efficiency particulate air filters. J. Occup. Environ. Hyg. 2008;5:713–720. doi: 10.1080/15459620802383934. [DOI] [PubMed] [Google Scholar]
- Almeida J.D., Tyrrell D. The morphology of three previously uncharacterized human respiratory viruses that grow in organ culture. J. Gen. Virol. 1967;1:175–178. doi: 10.1099/0022-1317-1-2-175. [DOI] [PubMed] [Google Scholar]
- ASHRAE . 1996. HVAC Systems and Equipment. Chapter 29. [Google Scholar]
- ASTM . 2020. ASTM International: ASTM F2100 - 19 Standard Specification forPerformance of Materials Used in Medical Face Masks. [Google Scholar]
- Becquemin M., Swift D., Bouchikhi A., Roy M., Teillac A. Particle deposition and resistance in the noses of adults and children. Eur. Respir. J. 1991;4:694–702. [PubMed] [Google Scholar]
- Bowdle A., Munoz-Price L. Preventing infection of patients and healthcare workers should be the new normal in the era of novel coronavirus epidemics. Anesthesiology. 2020 doi: 10.1097/ALN.0000000000003295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen L.E. Does that facemask really protect you? Appl. Biosaf. 2010;15:67–71. [Google Scholar]
- CDC . 2020. Strategies for Optimizing the Supply of Facemasks. [Google Scholar]
- Cooper C.D., Alley F.C. Waveland press; 2010. Air Pollution Control: A Design Approach. [Google Scholar]
- Damit B., Bischoff B.L., Phelps T.J., Wu C.-Y., Cheng M.-D. Filtration of bioaerosols using a granular metallic filter with micrometer-sized collectors. J. Environ. Eng. 2014;140 [Google Scholar]
- Fazli T., Zeng Y., Stephens B. Fine and ultrafine particle removal efficiency of new residential HVAC filters. Indoor Air. 2019;29:656–669. doi: 10.1111/ina.12566. [DOI] [PubMed] [Google Scholar]
- FDA . Guidance for Industry and FDA Staff; 2018. Surgical Masks-Premarket Notification [510-(k)] Submissions. [Google Scholar]
- FDA . US Government Printing Office, Office of the Federal Register; Washington, DC: 2019. General and Plastic Surgery Devices. 21 CFR Part 878.4040. Code of Federal Regulations. [Google Scholar]
- FDA . 2020. N95 Respirators and Surgical Masks (Facemasks)https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-and-surgical-masks-face-masks [Google Scholar]
- Friedlander S.K. Oxford University Press; New York: 2000. Smoke, Dust, and Haze. [Google Scholar]
- Grinshpun S.A., Haruta H., Eninger R.M., Reponen T., McKay R.T., Lee S.-A. Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: two pathways for particle penetration. J. Occup. Environ. Hyg. 2009;6:593–603. doi: 10.1080/15459620903120086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley J.T., Ensor D.S., Smith D.D., Sparks L.E. FractionalAerosolFiltration efficiency of in-duct ventilation air cleaners. Indoor Air. 1994;4:169–178. [Google Scholar]
- He M., Dhaniyala S., Wagner M. Aerosol Filtration with Mobility-Classified Particles: role of multiply charged particles in skewing penetration measurements. Aerosol Sci. Technol. 2015;49:705–716. [Google Scholar]
- Hinds W. Wiley-Interscience; New York: 1999. Particle Technology. [Google Scholar]
- Jung H., Kim J., Lee S., Lee J., Kim J., Tsai P., Yoon C. Comparison of filtration efficiency and pressure drop in anti-yellow sand masks, quarantine masks, medical masks, general masks, and handkerchiefs. Aerosol Air Qual. Res. 2014;14:991–1002. [Google Scholar]
- Konda A., Prakash A., Moss G.A., Schmoldt M., Grant G.D., Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020 doi: 10.1021/acsnano.0c03252. [DOI] [PubMed] [Google Scholar]
- Lakdawala S.S., Lamirande E.W., Suguitan A.L., Jr., Wang W., Santos C.P., Vogel L., Matsuoka Y., Lindsley W.G., Jin H., Subbarao K. Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog. 2011;7 doi: 10.1371/journal.ppat.1002443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung W.W., Hung C., Yuen P. Effect of face velocity, nanofiber packing density and thickness on filtration performance of filters with nanofibers coated on a substrate. Separ. Purif. Technol. 2010;71:30–37. [Google Scholar]
- Li L., Zuo Z., Japuntich D.A., Pui D.Y. Evaluation of filter media for particle number, surface area and mass penetrations. Ann. Occup. Hyg. 2012;56:581–594. doi: 10.1093/annhyg/mes034. [DOI] [PubMed] [Google Scholar]
- Li J., Leavey A., Wang Y., O'Neil C., Wallace M.A., Burnham C.-A.D., Boon A.C., Babcock H., Biswas P. Comparing the performance of 3 bioaerosol samplers for influenza virus. J. Aerosol Sci. 2018;115:133–145. doi: 10.1016/j.jaerosci.2017.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ning Z., Chen Yu. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020 doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9 doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller W., Horwell C.J., Apsley A., Steinle S., McPherson S., Cherrie J.W., Galea K.S. The effectiveness of respiratory protection worn by communities to protect from volcanic ash inhalation. Part I: filtration efficiency tests. Int. J. Hyg Environ. Health. 2018;221:967–976. doi: 10.1016/j.ijheh.2018.03.012. [DOI] [PubMed] [Google Scholar]
- Neupane B.B., Mainali S., Sharma A., Giri B. Optical microscopic study of surface morphology and filtering efficiency of facemasks. PeerJ. 2019;7 doi: 10.7717/peerj.7142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIOSH . DHHS, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, National Personal Protective Technology Laboratory; Pittsburgh, PA: 2007. Procedure No. TEB-APR-STP-0059, Revision 2.0. Determination of Particulate Filter Efficiency Level for N95 Series Filters against Solid Particulates for Non-powered, Air Purifying Respirators Standard Testing Procedure (STP) TEB-APR-STP-0059.pdf. Accessed 9 December 2009. [Google Scholar]
- OSHA . Department of Health; 2003. OSHA Revised Respiratory Protection Standards 29 CFR 1910.134. [Google Scholar]
- Payet S., Boulaud D., Madelaine G., Renoux A. Penetration and pressure drop of a HEPA filter during loading with submicron liquid particles. J. Aerosol Sci. 1992;23:723–735. [Google Scholar]
- Perumalraj R. Characterization of electrostatic discharge properties of woven fabrics. J. Textil. Sci. Eng. 2016;6:6. [Google Scholar]
- Podgorski A., Bałazy A., Gradoń L. Application of nanofibers to improve the filtration efficiency of the most penetrating aerosol particles in fibrous filters. Chem. Eng. Sci. 2006;61:6804–6815. [Google Scholar]
- Przekop R., Gradoń L. Deposition and filtration of nanoparticles in the composites of nano-and microsized fibers. Aerosol Sci. Technol. 2008;42:483–493. [Google Scholar]
- Rengasamy S., Eimer B.C. Total inward leakage of nanoparticles through filtering facepiece respirators. Ann. Occup. Hyg. 2011;55:253–263. doi: 10.1093/annhyg/meq096. [DOI] [PubMed] [Google Scholar]
- Rengasamy S., King W.P., Eimer B.C., Shaffer R.E. Filtration performance of NIOSH-approved N95 and P100 filtering facepiece respirators against 4 to 30 nanometer-size nanoparticles. J. Occup. Environ. Hyg. 2008;5:556–564. doi: 10.1080/15459620802275387. [DOI] [PubMed] [Google Scholar]
- Rengasamy S., Eimer B., Shaffer R.E. Simple respiratory protection—evaluation of the filtration performance of cloth masks and common fabric materials against 20–1000 nm size particles. Ann. Occup. Hyg. 2010;54:789–798. doi: 10.1093/annhyg/meq044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rengasamy S., Niezgoda G., Shaffer R. Flammability of respirators and other head and facial personal protective equipment. J. Int. Soc. Respir. Prot. 2018;35:1. [PMC free article] [PubMed] [Google Scholar]
- Shakya K.M., Noyes A., Kallin R., Peltier R.E. Evaluating the efficacy of cloth facemasks in reducing particulate matter exposure. J. Expo. Sci. Environ. Epidemiol. 2017;27:352–357. doi: 10.1038/jes.2016.42. [DOI] [PubMed] [Google Scholar]
- Shangguan T., Siegel D.P., Lear J.D., Axelsen P.H., Alford D., Bentz J. Morphological changes and fusogenic activity of influenza virus hemagglutinin. Biophys. J. 1998;74:54–62. doi: 10.1016/S0006-3495(98)77766-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon H., Muir A., Haines T., Verma D. Mortality and cancer incidence in Ontario glass fiber workers. Occup. Med. 2005;55:528–534. doi: 10.1093/occmed/kqi124. [DOI] [PubMed] [Google Scholar]
- Stafford R.G., Ettinger H.J. Filter efficiency as a function of particle size and velocity. Atmos. Environ. 1972;6:353–362. [Google Scholar]
- Wallace L. Indoor sources of ultrafine and accumulation mode particles: size distributions, size-resolved concentrations, and source strengths. Aerosol Sci. Technol. 2006;40:348–360. [Google Scholar]
- Wallace L., Howard-Reed C. Continuous monitoring of ultrafine, fine, and coarse particles in a residence for 18 months in 1999-2000. J. Air Waste Manag. Assoc. 2002;52:828–844. doi: 10.1080/10473289.2002.10470823. [DOI] [PubMed] [Google Scholar]
- Wallace L.A., Emmerich S.J., Howard-Reed C. Effect of central fans and in-duct filters on deposition rates of ultrafine and fine particles in an occupied townhouse. Atmos. Environ. 2004;38:405–413. [Google Scholar]
- WHO Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. 2020. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations
- Woo M.-H., Hsu Y.-M., Wu C.-Y., Heimbuch B., Wander J. Method for contamination of filtering facepiece respirators by deposition of MS2 viral aerosols. J. Aerosol Sci. 2010;41:944–952. doi: 10.1016/j.jaerosci.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yun K.M., Suryamas A.B., Iskandar F., Bao L., Niinuma H., Okuyama K. Morphology optimization of polymer nanofiber for applications in aerosol particle filtration. Separ. Purif. Technol. 2010;75:340–345. [Google Scholar]
- Zhang Q., Welch J., Park H., Wu C.-Y., Sigmund W., Marijnissen J.C. Improvement in nanofiber filtration by multiple thin layers of nanofiber mats. J. Aerosol Sci. 2010;41:230–236. [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuo Z., Kuehn T.H., Pui D.Y. Respirator testing using virus aerosol: comparison between viability penetration and physical penetration. Ann. Occup. Hyg. 2015;59:812–816. doi: 10.1093/annhyg/mev019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.