Abstract
Background:
No meta-analysis exists elucidate the impact of prior hip arthroscopy on the outcomes of subsequent hip arthroplasty. The purpose of this study was to systematically review the current evidence in the literature to ascertain if prior hip arthroscopy leads to inferior outcomes after hip arthroplasty.
Methods:
PUBMED, Scopus, EMBASE, and Cochrane Library databases were searched on May 20, 2019. Only English publications were included. The primary outcomes were postoperative complication, revision, and reoperation. Secondary outcomes included Harris Hip Score (HHS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), operative time, and estimated blood loss.
Results:
Eleven studies with a total of 1227 patients were included. The pooled data revealed that patients with prior hip arthroscopy were associated with higher risks for any postoperative complication (P < .00001), dislocation (P = .03), revision (P = .03), and reoperation (P = .02) following subsequent hip arthroplasty. However, there were no significant differences in infection rate (P = .22), HHS (P = .09), WOMAC (P = .19), operative time (P = .52), and estimated blood loss (P = .17) between the groups.
Conclusions:
Patients with prior hip arthroscopy are at increased risks for any postoperative complication, dislocation, revision, and reoperation following subsequent hip arthroplasty. However, prior hip arthroscopy does not appear to have an impact on the functional outcomes and intraoperative outcomes.
Keywords: complication, functional outcome, hip arthroplasty, prior hip arthroscopy, revision
1. Introduction
Hip arthroscopy has become a well-accepted practice for the diagnosis and treatment of certain prearthritic and early arthritic hip problems.[1] It has proven to be safe and effective in treating femoroacetabular impingement and labral tears, and indications continue to expand to other intra-articular and extra-articular pathologies.[2–4] The incidence of hip arthroscopy has increased dramatically over the past decade, with growth of 365% between 2004 and 2009[5] and 250% between 2007 and 2011 in the United States.[6] In the United Kingdom, there was a 727% increase in the number of hip arthroscopic procedures between 2002 and 2013.[7] Unfortunately, a significant proportion of patients, as high as 36% at 10 years, will ultimately require conversion to hip arthroplasty.[8–10] Given the increasing incidence of hip arthroscopy, more patients who have had prior hip arthroscopy will require conversion to hip arthroplasty. Therefore, the imminent demand for good postoperative outcomes reinforces the importance of determining the link between prior arthroscopy and future hip arthroplasty.
Currently, there remains a paucity of literature about the impact of prior hip arthroscopy on subsequent hip arthroplasty. Looking at total knee arthroplasty, there is some evidence that prior knee arthroscopy has some negative effect on the clinical outcome after total knee arthroplasty.[11–13] However, in the hip literature, most of studies have suggested that prior hip arthroscopy does not appear to have an impact on the complications, revisions, and patient-reported outcomes of a subsequent hip arthroplasty.[14–17] Only a few studies reported lower functional outcomes[18] or increased complications[19] after conversion hip arthroplasty. However, these studies are few and have small cohort sizes. Given the paucity of data available and its limited strength, the effect of prior hip arthroscopy on hip arthroplasty outcomes remains unclear.
To the best of our knowledge, no meta-analysis exists elucidate the impact of prior hip arthroscopy on the outcomes of subsequent hip arthroplasty. Therefore, the purpose of this study is to systematically review the current evidence in the literature to ascertain whether previous hip arthroscopy would lead to inferior outcomes in patients undergoing subsequent hip arthroplasty. Our hypothesis was that patients with prior hip arthroscopy were not associated with lower functional outcomes, high complication and revision rates after hip arthroplasty.
2. Materials and methods
2.1. Search strategy
The systematic literature review was structured to adhere to PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-analyses), which include requirements deemed essential for the transparent reporting of results.[20] The following search terms were used in PUBMED, Scopus, EMBASE, and Cochrane Library databases on August 20, 2019, as the search algorithm: (total hip arthroplasty) OR (hip resurfacing arthroplasty) AND (arthroscopy) OR (arthroscopic) AND (prior) OR (previous). No time limit was given to publication date. References within included articles were reviewed to include articles that were not included within our literature search. Ethical approval was not necessary because the present meta-analysis was performed based on previous published studies.
2.2. Eligibility criteria and study selection
Study included in our meta-analysis had to meet all of the following inclusion criteria in the PICOS order:
-
1.
population: patients had primary total hip arthroplasty (THA) or hip resurfacing arthroplasty (HRA);
-
2.
intervention: patients had history of hip arthroscopy;
-
3.
comparison intervention: patients had not history of hip arthroscopy;
-
4.
outcome measures: at least one of the following outcome measures was reported: complications, revision, reoperation, functional outcome, operative time, and estimated blood loss;
-
5.
study design: English cohort study.
Articles with no assessment of outcomes mentioned above or no comparison of 2 groups were not included into meta-analysis. Duplicate reports and conference abstracts were excluded. Case reports, biochemical trials, letters, and reviews were also eliminated. Articles were exported to EndNote, and duplicates removed. Two independent authors screened the titles and abstracts of potentially relevant studies to determine their eligibility based on the criteria. Disagreements were resolved through a discussion with a third review author.
2.3. Data extraction
The method of data extraction followed the approach outlined by the Cochrane Handbook for Systematic Reviews of Interventions.[21] Two independent authors extracted the following descriptive raw information from the selected studies: study characteristics such as author, publication year, study design, follow-up period; patient demographic details such as patients’ number, average age, and gender ratio. The primary outcomes were postoperative complication, revision, and reoperation. Secondary outcomes included Harris Hip Score (HHS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), operative time, and estimated blood loss. Where disagreement in the collection of data occurred, this was resolved through discussion. If the data were missing or could not be extracted directly, we contacted the corresponding authors to ensure that the information integrated. Otherwise, we calculated them with the guideline of Cochrane Handbook for Systematic Reviews of Interventions.[21] If necessary, we would abandon the extraction of incomplete data.
2.4. Data analysis
Revman 5.3 (Nordic Cochrane Centre, Denmark) was used to complete the meta-analysis and generate forest plots. We used the Mantel–Haenzel method to calculate the pooled odds ratio (OR). OR with a 95% confidence interval (CI) and mean difference (MD) or standardized mean differences (SMD) with 95% CI were assessed for dichotomous outcomes or continuous outcomes, respectively. The heterogeneity was assessed by using the Q test and I2 statistic. An I2 value of <25% was chosen to represent low heterogeneity and an I2 value of >75% to indicate high heterogeneity. We chose between a fixed effects and random effects model based upon the heterogeneity of included studies. Significance was set at P < .05.
2.5. Quality evaluation
The literature search did not yield any randomized trials. The Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I) assessment tool was adopted to evaluate the quality of nonrandomized surgical studies.[22] The ROBINS-I tool includes following 7 domains: bias due to confounding, bias in the selection of participants, bias in measurement of interventions, bias due to departures from intended interventions, bias due to missing data, bias in measurement of outcomes, and bias in selection of the reported result. Each paper was reviewed by one reviewer and verified by a second and disagreements were resolved by discussion with a third reviewer. Subgroup analyses were planned by type of arthroplasty (THA or HRA). We also conducted the sensitivity analysis to evaluate whether any single study had the weight to skew on the overall estimate and data. Begg's funnel plot was used to assess publication bias. If publication bias exists, the Begg's funnel plot is asymmetric.
3. Results
3.1. Database search
The initial literature search resulted in 412 total studies. After removal of duplicates, 307 irrelevant articles were excluded based on title and abstract screening. Among the remaining 105 studies, 82 articles were excluded by title and abstract. After reading the full text of all remaining articles in detail, 11 studies were then further excluded for reasons such as conference abstract, reviews, and no comparison of intervention and control group. Additionally, one cohort study which evaluated the outcomes following THA in patients with prior hip salvage surgery compared with patients without prior salvage procedure was also deleted.[23] Ultimately, 11 studies from 2012 to 2019 were available for meta-analysis (Fig. 1).[14–19,24–28]
Figure 1.

PRISMA Flow diagram describing the selection process for relevant clinical trials used in this meta-analysis.
3.2. Study characteristics and quality assessments
The study baseline characteristics and patient demographic details can be seen in Table 1. All 11 studies were matched control studies. A total of 1227 patients were included for analysis, with 481 patients had hip arthroscopy prior to hip arthroplasty and 746 patients without history of hip arthroscopy.[14–19,24–28] The mean age between groups was similar. Overall, the female percentage ranged from 36.4% to 70.5%. Mean follow-up period ranged from 2 to 5.4 years. The qualities of 11 researches were assessed, and the overall quality was good. The study qualities are shown in Table 2.
Table 1.
Characteristics of the included studies.

Table 2.
Methodological assessment according to 7 domains of potential biases (ROBINS-I).

3.3. Meta-analysis results
3.3.1. Any postoperative complication
Any postoperative complication was reported in all 11 studies.[14–19,24–28] It was present in 64 of 481 patients (13.3%) in the arthroscopy group and 39 of 746 patients (5.2%) in the control group, with statistically significant differences in favor of the control group (OR 2.59, 95% CI 1.68–4.01, I2 = 0%, P < .00001) (Fig. 2A).
Figure 2.

(A) Forest plots of the any postoperative complication between arthroscopy group and control group after hip arthroplasty; (B) Forest plots of the dislocation between arthroscopy group and control group after hip arthroplasty; (C) Forest plots of the infection between arthroscopy group and control group after hip arthroplasty.
3.3.2. Dislocation
Dislocation was reported in 8 studies.[15–17,19,25–28] It was present in 12 of 370 patients (3.2%) in the arthroscopy group and 6 of 592 patients (1.0%) in the control group, with statistically significant differences in favor of the control group (OR 2.67, 95% CI 1.10–6.51, I2 = 0%, P = .03) (Fig. 2B).
3.3.3. Infection
Infection was reported in 6 studies.[15–19,28] It was present in 8 of 287 patients (2.9%) in the arthroscopy group and 5 of 405 patients (1.2%) in the control group. The difference was not significant (OR 1.85, 95% CI 0.69–4.98, I2 = 0%, P = .22) (Fig. 2C).
3.3.4. Revision
All 11 trials[14–19,24–28] reported the revision between the groups, with 22 of 433 patients (5.1%) in the arthroscopy group and 19 of 717 patients (2.6%) in the control group, with statistically significant differences in favor of the control group (OR 2.00, 95% CI 1.07–3.71, I2 = 0%, P = .03) (Fig. 3A).
Figure 3.
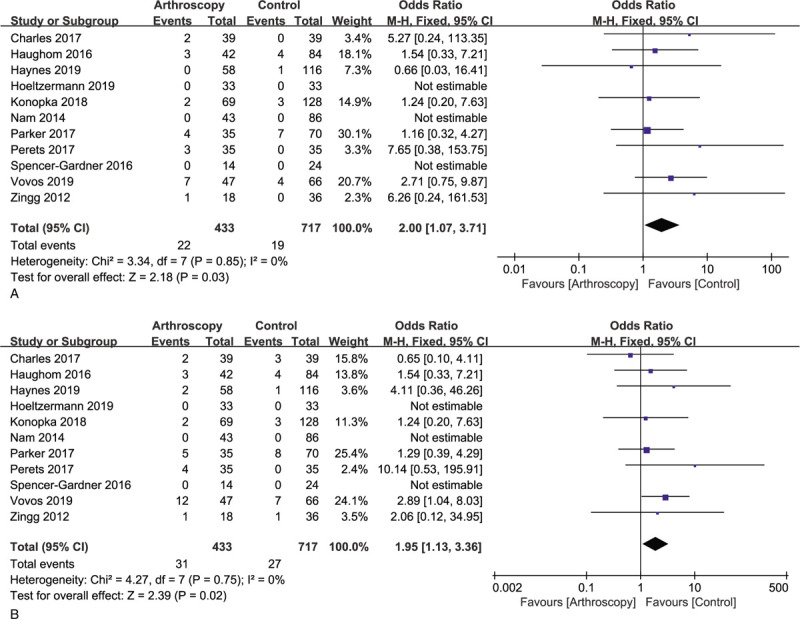
(A) Forest plots of the revision between arthroscopy group and control group after hip arthroplasty; (B) Forest plots of the reoperation between arthroscopy group and control group after hip arthroplasty.
3.3.5. Reoperation
All 11 trials[14–19,24–28] reported the reoperation between the groups, with 31 of 433 patients (7.2%) in the arthroscopy group and 27 of 717 patients (3.8%) in the control group, with statistically significant differences in favor of the control group (OR 1.95, 95% CI 1.13–3.36, I2 = 0%, P = .02) (Fig. 3B).
3.3.6. HHS
Seven trials[14–16,18,24,26] including 708 patients showed the HHS, with no statistically significant differences between the groups (MD = −0.83, 95% CI −1.81 to 0.14, I2 = 1%, P = .09) (Fig. 4A).
Figure 4.

(A) Forest plots of the HHS between arthroscopy group and control group after hip arthroplasty; (B) Forest plots of the WOMAC between arthroscopy group and control group after hip arthroplasty.
3.3.7. WOMAC
Only 4 studies[15,24,25,28] including 564 patients showed the WOMAC. According to the analysis, there were no statistically significant differences between the groups (SMD = −0.12, 95% CI −0.29 to 0.06, I2 = 0%, P = .19) (Fig. 4B).
3.3.8. Operative time
Five trials[14,15,17,19,28] including 562 patients showed the operative time. According to the analysis, there were no statistically significant differences between the groups (MD = −4.48, 95% CI −18.11 to 9.14, I2 = 88%, P = .52) (Fig. 5A). Sensitivity analysis showed that the statistical result could not be materially altered by eliminating any study
Figure 5.

(A) Forest plots of the operative time between arthroscopy group and control group after hip arthroplasty; (B) Forest plots of the estimated blood loss between arthroscopy group and control group after hip arthroplasty.
3.3.9. Estimated blood loss
Only 4 studies[17,19,27,28] including 360 patients showed the estimated blood loss. According to the analysis, there were no statistically significant differences between the groups (MD = 48.32, 95% CI −20.37 to 117.01, I2 = 0%, P = .17) (Fig. 5B).
3.4. Publication bias
There were significant publication biases with asymmetrical Begg's funnel plots (Fig. 6A–C). However, after trimming by imputing the missing studies, adding them to the analysis, and then recomputing the effect size (Duval and Rweedie's trim and fill method), the OR did not change significantly.
Figure 6.

(A) Funnel plot of publication bias for the any postoperative complication between arthroscopy group and control group after hip arthroplasty; (B) Funnel plot of publication bias for the revision between arthroscopy group and control group after hip arthroplasty; (C). Funnel plot of publication bias for the reoperation between arthroscopy group and control group after hip arthroplasty.
4. Discussion
In recent years, the use of hip arthroscopy for treatment of various hip conditions has grown rapidly.[1] Despite reports of favorable outcomes after hip arthroscopy, a subset of patients inevitably experience progression of hip disease that necessitates subsequent arthroplasty. In light of this, the evaluation of hip arthroplasty outcomes after arthroscopic hip surgery is emerging as an important area of research. Knowledge of the impact of hip arthroscopy on the outcomes of a subsequent hip arthroplasty, however, is currently limited. To the best of our knowledge, this is the first meta-analysis to investigate the impact of prior hip arthroscopy on the outcomes of subsequent hip arthroplasty. The purpose of this study was to systematically review the current evidence in the literature to ascertain if prior hip arthroscopy leads to inferior outcomes after hip arthroplasty. We hypothesized that there would be no difference in clinical outcomes between the groups. Contrary to our hypothesis, we found that patients with prior hip arthroscopy were associated with higher risks for any postoperative complication (P < .00001), dislocation (P = .03), revision (P = .03), and reoperation (P = .02) following subsequent hip arthroplasty. However, there were no significant differences in infection rate (P = .22), HHS (P = .09), WOMAC (P = .19), operative time (P = .52), and estimated blood loss (P = .17) between the groups. The findings of our study will have implications for the arthroplasty patient, arthroplasty surgeon, and healthcare system.
While the body of present literature is incomplete, some proposed concerns about arthroscopic hip surgery prior to hip arthroplasty include complications in the exposure as a result of scar tissue, increased infection risk owing to prior surgery, and the potential of encountering hardware that may make subsequent hip arthroplasty more difficult.[15] Our finding among conversion hip arthroplasty patients partly corroborates this fear. This study identified that conversion hip arthroplasty patients with prior hip arthroscopy were at higher risk for any postoperative complication, hip dislocation, revision, and reoperation at mean of 3.6 years follow-up, but had similar rate of infection, compared to those who did not have hip arthroscopy. However, given the relatively small cohort size, none of included studies revealed higher risks of dislocation, revision, and reoperation in the arthroscopy group. Already, experience with total knee arthroplasty after either open or arthroscopic knee surgery has shown that prior surgery increases complications and failure rates.[11–13] As with any invasive hip surgery, arthroscopic hip surgery traumatizes the connective tissue envelop around the hip joint and can lead to derangement of tissue planes, scar formation, and heterotopic ossification (HO), which might affect wound healing and increased complications. It is therefore not surprising to see increased complications associated with arthroscopy.
Although patient-reported outcome scores were similar between groups in most of the studies, the other studies revealed inferior functional outcomes in the arthroscopy group. Perets et al[18] found that the arthroscopy group had significantly lower HHS, Forgotten Joint Score-12, and satisfaction compared to control group at 3.3 years follow-up. Konopka et al[25] also indicated that patients who underwent THA with history of arthroscopy had lower Hip disability and Osteoarthritis Outcome Score, WOMAC, and Short Form-12 physical component scores at 5.3 years follow-up. However, our data suggest that prior hip arthroscopy has no effect on HHS and WOMAC following a subsequent THA or HRA procedure. Arthroscopic hip surgery could potentially lead to increased scar tissue formation and HO. Although the association between HO and outcome scores has not been consistent, the influence of severe HO on terminal range of motion is well established.[29,30] However, there was insufficient data to perform meta-analyses of other functional outcomes such as range of motion, University of California at Los Angeles score, and Oxford Hip Score. Therefore, more high-quality studies are still needed to discuss these issues in the future.
A secondary surgery on the same site can be of increased difficulty due to formation of scar tissue and changes in tissue relations. However, our pooled data suggest that intraoperative measures including operative time (I2 = 88%, P = .52) and estimated blood loss (I2 = 0%, P = .17) are similar between the 2 groups. High heterogeneity in operative time results from conflicting results of the two included studies. Vovos et al[19] found that arthroscopy group resulted in increased operative time compared to control group, whereas Zingg et al[28] found that the operative time was significantly longer in the control group. The remaining 3 studies[14,15,17] revealed similar operative time between groups. The inconsistent results of these studies may be due to the differences in study design and sample size. However, estimated blood loss was also considered a reasonable indicator of operative time. The similarity of the blood loss may indirectly reflect similar operative time between the groups.
The present study does have recognized limitations despite the use of a systematic process. First, all of the included studies were retrospective in nature, which can introduce potential biases with meta-analysis. However, all including studies are matched-controlled, which may minimize possible inhomogeneity. Second, only 11 studies assessing a total of 1227 patients were included in our meta-analysis; if more studies had been included, the statistical efficacy of our analysis would increase. Third, the mean follow-up time for all studies was relatively short (3.6 years), thus, the data presented in this review cannot be used to draw conclusions about long-term outcomes of hip arthroplasty in this patient population, trials with longer and similar follow-up are still needed. Fourth, there was insufficient data to perform subgroup analyses by type of arthroplasty, we were unable to determine whether the type of hip arthroscopic procedure had an effect on patient clinical outcomes. Fifth, only English publications were included in our meta-analysis; thus, publication bias is unavoidable. Finally, some minor factors such as differences in technique, assessment techniques, the mean interval between hip arthroscopy and subsequent arthroplasty may affect the quality of results. To some extent, these factors were inevitable.
5. Conclusion
Patients with prior hip arthroscopy are at increased risks for any postoperative complication, dislocation, revision, and reoperation following subsequent hip arthroplasty. However, prior hip arthroscopy does not appear to have an impact on the functional outcomes and intraoperative outcomes.
Author contributions
Conceptualization: Dongmei Dou.
Data curation: Dongmei Dou.
Writing – review & editing: Jiankuo Guo.
Footnotes
Abbreviations: CI = confidence interval, HHS = Harris Hip Score, HRA = hip resurfacing arthroplasty, MD = mean difference, OR = odds ratio, ROBINS-I = The Risk of Bias in Non-Randomized Studies of Interventions, SMD = standardised mean differences, THA = total hip arthroplasty, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
How to cite this article: Guo J, Dou D. Influence of prior hip arthroscopy on outcomes after hip arthroplasty: A meta-analysis of matched control studies. Medicine. 2020;99:29(e21246).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the present study are publicly available.
References
- [1].Bozic KJ, Chan V, Valone FH, et al. Trends in hip arthroscopy utilization in the United States. J Arthroplasty 2013;28: 8 Suppl: 140–3. [DOI] [PubMed] [Google Scholar]
- [2].Botser IB, Smith TW, Jr, Nasser R, et al. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy 2011;27:270–8. [DOI] [PubMed] [Google Scholar]
- [3].McCormick F, Nwachukwu BU, Alpaugh K, et al. Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy 2012;28:1359–64. [DOI] [PubMed] [Google Scholar]
- [4].Skendzel JG, Philippon MJ, Briggs KK, et al. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med 2014;42:1127–33. [DOI] [PubMed] [Google Scholar]
- [5].Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy 2013;29:661–5. [DOI] [PubMed] [Google Scholar]
- [6].Sing DC, Feeley BT, Tay B, et al. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy 2015;31:2307–13. [DOI] [PubMed] [Google Scholar]
- [7].Palmer AJ, Malak TT, Broomfield J, et al. Past and projected temporal trends in arthroscopic hip surgery in England between 2002 and 2013. BMJ Open Sport Exerc Med 2016;2:e000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Menge TJ, Briggs KK, Dornan GJ, et al. Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement: labral debridement compared with labral repair. J Bone Joint Surg Am 2017;99:997–1004. [DOI] [PubMed] [Google Scholar]
- [9].Horner NS, Ekhtiari S, Simunovic N, et al. Hip arthroscopy in patients age 40 or older: a systematic review. Arthroscopy 2017;33:464–75. [DOI] [PubMed] [Google Scholar]
- [10].McCarthy JC, Jarrett BT, Ojeifo O, et al. What factors influence long-term survivorship after hip arthroscopy? Clin Orthop Relat Res 2011;469:362–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Barton SB, McLauchlan GJ, Canty SJ. The incidence and impact of arthroscopy in the year prior to total knee arthroplasty. Knee 2017;24:396–401. [DOI] [PubMed] [Google Scholar]
- [12].Werner BC, Burrus MT, Novicoff WM, et al. Total knee arthroplasty within six months after knee arthroscopy is associated with increased postoperative complications. J Arthroplasty 2015;30:1313–6. [DOI] [PubMed] [Google Scholar]
- [13].Piedade SR, Pinaroli A, Servien E, et al. Is previous knee arthroscopy related to worse results in primary total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 2009;17:328–33. [DOI] [PubMed] [Google Scholar]
- [14].Hoeltzermann M, Sobau C, Miehlke W, et al. Prior arthroscopic treatment for femoro-acetabular impingement does not compromise hip arthroplasty outcomes: a matched-controlled study with minimum two-year follow-up. Int Orthop 2019;43:1591–6. [DOI] [PubMed] [Google Scholar]
- [15].Haynes JA, Xiong A, Nepple JJ, et al. Does previous hip arthroscopy affect the clinical outcomes of total hip arthroplasty? Orthop J Sports Med 2019;7:2325967119829736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Haughom BD, Plummer DR, Hellman MD, et al. Does hip arthroscopy affect the outcomes of a subsequent total hip arthroplasty? J Arthroplasty 2016;31:1516–8. [DOI] [PubMed] [Google Scholar]
- [17].Charles R, LaTulip S, Goulet JA, et al. Previous arthroscopic repair of femoro-acetabular impingement does not affect outcomes of total hip arthroplasty. Int Orthop 2017;41:1125–9. [DOI] [PubMed] [Google Scholar]
- [18].Perets I, Mansor Y, Mu BH, et al. Prior arthroscopy leads to inferior outcomes in total hip arthroplasty: a match-controlled study. J Arthroplasty 2017;32:3665–8. [DOI] [PubMed] [Google Scholar]
- [19].Vovos TJ, Lazarides AL, Ryan SP, et al. Prior hip arthroscopy increases risk for perioperative total hip arthroplasty complications: a matched-controlled study. J Arthroplasty 2019;34:1707–10. [DOI] [PubMed] [Google Scholar]
- [20].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Wiley-Blackwell; 2017. [Google Scholar]
- [22].Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].George J, Miller EM, Higuera CA, et al. Influence of prior hip salvage surgery on outcomes after total hip arthroplasty in young patients. J Arthroplasty 2018;33:1108–12. [DOI] [PubMed] [Google Scholar]
- [24].Nam D, Maher P, Nath T, et al. Does a prior hip arthroscopy affect clinical outcomes in metal-on-metal hip resurfacing arthroplasty? Am J Orthop (Belle Mead NJ) 2014;43:E255–60. [PubMed] [Google Scholar]
- [25].Konopka JF, Buly RL, Kelly BT, et al. The effect of prior hip arthroscopy on patient-reported outcomes after total hip arthroplasty: an institutional registry-based, matched cohort study. J Arthroplasty 2018;33:1806–12. [DOI] [PubMed] [Google Scholar]
- [26].Parker SJM, Grammatopoulos G, Davies OLI, et al. Outcomes of hip arthroplasty after failed hip arthroscopy: a case-control study. J Arthroplasty 2017;32:3082–7. [DOI] [PubMed] [Google Scholar]
- [27].Spencer-Gardner LS, Camp CL, Martin JR, et al. Does prior surgery for femoroacetabular impingement compromise hip arthroplasty outcomes? J Arthroplasty 2016;31:1899–903. [DOI] [PubMed] [Google Scholar]
- [28].Zingg PO, Schallberger A, Rüdiger HA, et al. Does previous hip arthroscopy negatively influence the short term clinical result of total hip replacement? Arch Orthop Trauma Surg 2012;132:299–303. [DOI] [PubMed] [Google Scholar]
- [29].Vasileiadis GI, Amanatullah DF, Crenshaw JR, et al. Effect of heterotopic ossification on hip range of motion and clinical outcome. J Arthroplasty 2015;30:461–4. [DOI] [PubMed] [Google Scholar]
- [30].Neal B. Effects of heterotopic bone formation on outcome after hip arthroplasty. ANZ J Surg 2003;73:422–6. [DOI] [PubMed] [Google Scholar]


