Abstract
It has been well established that dietary patterns play important roles in the pathogenesis and development of hypertension. Our aim was to investigate the association between pregnancy dietary patterns and the risk of hypertension among nulliparous pregnant Chinese women.
A cross-sectional, case-control study.
Three hospitals in Haikou, the capital of Hainan Province, South China.
A total of 2580 participants who reported dietary intake using a validated food frequency questionnaire (FFQ).
Four primary dietary patterns were identified by principal component factor analysis and labeled as traditional Chinese, animal food, Western food, and salty snacks patterns. Women with high scores on pattern characterized by salty snacks were at increased risk.
This study suggests that dietary pattern characterized by salty snack increases the risk of hypertension during pregnancy.
Keywords: China, dietary patterns, pregnancy-induced hypertension, salty snack
1. Introduction
Gestational hypertension or pregnancy-induced hypertension (PIH) is a condition occurred in pregnant women, who develop high blood pressure (higher than 140/90 on 2 separate occasions at least 6 hours apart) after 20 weeks’ gestation in the absence of urinary proteins or other signs of preeclampsia. PIH is significantly associated with an increased risk of maternal and morbidity.[1,2] As a subgroup of hypertensive disorders, PIH affects about 8% to 10% of pregnancy worldwide and leads to a variety of adverse complications (including type 2 diabetes, strokes, acute myocardial infarction, and cardiomyopathy) in both mothers and offspring.[3–5] In the United States, PIH is the second leading cause of maternal mortality after embolism, affecting more than 250,000 cases and accounting for 15% of deaths.[6] The great burden on medical and social expenditures highlights the need to study the risk factors that may contribute to lowering blood pressure and to the prevention of PIH.
Previous studies have demonstrated the linkage of different dietary patterns to pathological diseases, including type 2 diabetes,[7] newly diagnosed glucose tolerance abnormalities,[8] stroke,[9] anemia,[10] and breast cancer[11] in Chinese population. In addition, the involvement of dietary patterns in hypertension was also reported. Indeed, previous studies have demonstrated protective association of vegetable-rich diets with PIH. In a Norwegian Mother and Child Cohort Study including 72,072 women, the high new Nordic diet (a vegetable-rich diet) adherence was associated with a lower relative risk of preeclampsia and of spontaneous preterm delivery among nulliparous women.[12] In a 9 year follow-up study of 3582 women participating in the Australian Longitudinal Study on Women's Health, an independent protective dose-response association between prepregnancy consumption of a Mediterranean-style dietary pattern (a vegetable-rich diet) and hypertensive disorder of pregnancy risk was observed.[13] On the contrast, in a nationally representative cross-sectional study of 23,671 Chinese adults, a body mass index (BMI)-mediated positive relationship between the traditional northern pattern diet, characterized by high intakes of wheat flour products and starchy tubers, combined with low consumption of protein products, and hypertension was also reported.[14] Interestingly, several healthful dietary patterns have been shown to be effective in preventing hypertension in Western populations.[15,16] However, little is known about the relationship between dietary patterns and gestational hypertension in Chinese population. The purpose of this study was to determine if dietary patterns can affect the incidence of hypertensive disorders in Chinese pregnant women.
2. Subjects and methods
2.1. Ethics committee approval
The study has been ethically approved by the Institutional Review Ethics Committee for three hospitals in Haikou and written informed consent was obtained from all participants.
2.2. Study population
A cross-sectional study was conducted on nulliparous pregnant Chinese women in three hospitals in Haikou, the capital of Hainan Province, south China. A total of 2580 participants aged 20 to 40 years were recruited for this study from 2013 to 2016. A stratified cluster random-sampling method which has been described in detail previously was used.[17] Of these study samples, 1290 were with gestational hypertension and 1290 were normotensive control subjects. The control subjects were matched to the cases for age. None of these women had chronic hypertension, renal disease, diabetes mellitus and collagen vascular disorders.
2.3. Survey method
The examined parameters for the recruited individuals included blood pressure, body height, body weight, BMI. The blood pressure was measured 3 times by mercury sphygmomanometers and between the measurements, each subject was rested for 5 minutes in a seated position. BMI, a well-recognized indicator of body fat, was calculated as weight in kilograms divided by the square of height in meters.
2.4. Interviews and questionnaire
A general information questionnaire was used to collect age, gender, education level, total energy intake, physical activity, area of residence, physical activity level, BMI, smoking and annual household income. A validated semiquantitative food frequency questionnaire (FFQ) including 58 food items, previously described in the 2010 China National Nutrition and Health Survey (CNNHS), was used to assess the information of nutrient intake and food consumption of pregnant Chinese women. We analyzed the spearman regression coefficients of 3-day weighed food records and relative under-reporting or over-reporting rate to investigate their correlations. In addition, these food items were divided into 17 food groups based on the nutritional characteristics of food in diet. Participants were asked to indicate the frequency of each food item during the first 5 month of pregnancy starting from around week 22 of gestation. The frequency of food intake was divided into nine categories: never eat, <1 time/month, 1 to 3 time(s)/month, 1 to 2 time(s)/week, 3-4 times/week, 5 to 6 times/week, 1 time/day, 2 times/day, and 3 times/day. The amount of consumption in the unit of Liang (1 Liang = 50 g) were obtained from subjects.[14,18] The validity of the FFQ used in this study for assessing the food consumption and nutrient intake of Chinese adults was described previously.[19]
2.5. Dietary patterns
The food that did not fit a distinctive food group, for instance, eggs, tea, and coffee, have been defined as individual categories. The validity and reliability of this FFQ has been examined. The loading high factors have been used to define for each dietary pattern.[18,20] The food groups were classified as follow: rice; coarse grains, steamed bun/noodles, tubers (potatoes), fresh vegetables and fruits, pickled vegetables, mushrooms, red meat, processed and cooked meat, fish and shrimp, seafood, bacon and salted fish, miscellaneous bean, bean sauce, fats/oils, fast foods(pizza and hamburgers), snacks, and chocolates. A factor analysis of this 20 predefined food groups was used to generate dietary patterns.
2.6. Statistical analysis
Statistical analyses were performed with the Statistical Product and Service Solutions (SPSS) version 16.0 (SPSS Inc., Chicago, IL). Dietary patterns in the FFQ were identified by using factor analysis. The model was controlled for sex, age, economic status, physical activity, education level, BMI, and energy intake. Continuous variable factors were shown as mean ± standard deviation (SD) and categorical variable factors were shown as percentages of the sum. The significance of categorical variables was determined by Chi-square test. Dietary factor scores were categorized into four quartiles for each dietary pattern. Quartile 4 was a high consumption level and quartile 1 was a low consumption of this pattern.
3. Results
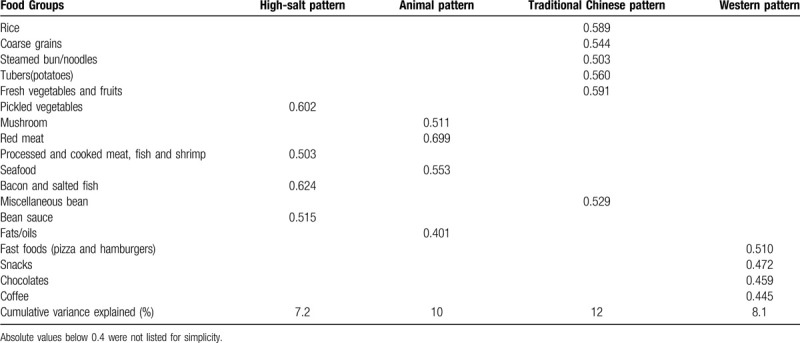
Four dietary patterns out of the 20 investigated food groups, including animal pattern, traditional Chinese pattern, western pattern and high-salt pattern, were selected by factor analysis as described above. The correlation among the variables was sufficiently strong for a factor analysis. Table 1 showed the factor-loading matrixes for dietary patterns. The 4 dietary patterns accounted for 37.3%.
Table 1.
Factor-loading matrix for dietary patterns: Freshmen (n = 2580) Aged 20 to 40 years.
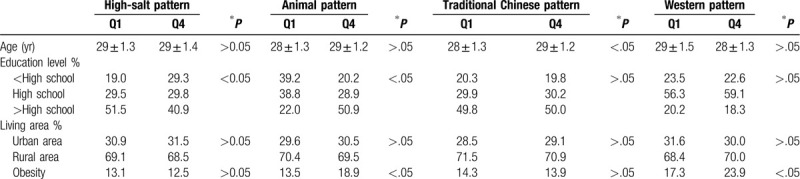
The general characteristics of all participants were shown in Table 2. Hypertensive disorders of pregnancy (HDPs) were more likely to occur in participants who are less educated and overweight. The characteristics of participants according to quartile (Q) categories of different dietary patterns were shown in Table 3. Participants in the high Western pattern score were younger and had higher income and education level. Participants with high high-salt score had lower education level and income compared to those of the participants with low high-salt score.
Table 2.
The characteristics of all participants were shown.

Table 3.
Characteristics of participants according to quartile (Q) categories of different dietary pattern.
After adjusting for living area, income, educational level, physical activity level, obesity and energy intake, participants receiving high-salt pattern diets had higher systolic blood pressure (r = 0.110, P < .05). However, no significant association between the diet patterns and hypertension was observed in groups of animal pattern, traditional Chinese pattern and western pattern (r = 0.045, 0.078, 0.069, respectively, P > .05).
4. Discussion
PIH includes preeclampsia and gestational hypertension, which is reported to be associated with the development of hypertension and cardiovascular disease later in life.[21,22] Pregnancy complications may initiate vascular damage alter metabolism, or lead to a high risk of future disease such as systemic inflammation and endothelial dysfunction.[23,24] In this study of Chinese pregnancy women, we identified the four dietary patterns during the first half pregnancy and systematically investigated their association with hypertension. After adjusting the living area, income, educational level, physical activity level, obesity, and energy intake, we showed that the high-salt food pattern was significantly associated with hypertension. However, no linkage with hypertension was observed for animal pattern, traditional Chinese pattern and Western pattern.
To our knowledge, this is the first investigation to study the association between pregnancy dietary patterns and HDPs. Previous studies have shown that higher blood pressure level in northern pattern than the southern pattern foods.[18,25] The dietary factors explained the north-south pattern diet differences in hypertension. Obesity was also an risk factor for atherosclerosis.[26] In the Western populations, the Western dietary pattern was associated with increased risk of hypertension.[27] However, we did not found the association between the blood pressure and Western pattern in the nulliparous pregnant Chinese women.
The salty diet characterized in our investigation was partially similar with the diet patterns used in the Norwegian study and supports the hypothesis that less healthy diets serve as risk factors of PIH. A recent study also found that dietary patterns might be associated with the risk of pregnancy-related complications in three major dietary patterns such as western dietary pattern, traditional dietary pattern, and healthy dietary pattern.[28] Pregnancy is a physiological condition associated with a reduced adaptation of aldosterone to changes in Na+ intake, and any changes in sodium intake would alter aldosterone, a hormone previously described beneficial in pregnancy. As demonstrated in previous study, aldosterone is a prerequisite for adequate plasma volume expansion, a condition required for adequate placental perfusion and fetal growth.[29] In another study, both gestational hypertension and preeclampsia were found to be associated with high triglycerides, low high-density lipoprotein cholesterol and high systolic blood pressure.[30] Compared to the healthy pregnancy, plasma renin and angiotensin II changed in dietary salt intake in hypertensive pregnancies, indicating the changes of Renin-Angiotensin-Aldosterone system were the reason for PIH.[31]
5. Conclusion
In this study, we found that the high-salt food pattern was significantly associated with hypertension in pregnancy. However, no linkage with hypertension was observed for animal pattern, traditional Chinese pattern and Western pattern. There are limitations in this study. First, we did not take diet during prepregnancy into account. Some evidence from previous investigations suggested that women might have minimal change in diet from before to during pregnancy.[32,33] Second, we did not investigate the reason induced the changes of pregnant Chinese women. Third, pregnancy-related complications are associated with increased risks of adverse outcomes for mother and her infant, but the influence of PIH induced by salt diet on the offspring remained unknown. Therefore, the next step will be to formally resolve above problems.
Author contributions
Guarantor of integrity of the entire study: Yiling Ding.
Study concepts: Xiaoju Chen.
Study design: Xiaoju Chen, Yiling Ding.
Definition of intellectual content: Xiaoju Chen.
Literature research: Xiaoju Chen.
Clinical studies: Xiaoju Chen, Lei Shi.
Experimental studies: Xiaoju Chen, Dongcai Wu.
Data acquisition: Xiaoju Chen, Yuqiao Mo.
Data analysis: Xiaoju Chen, Fangrong Chen.
Statistical analysis: Xiaoju Chen, Li Wang.
Manuscript preparation: Xiaoju Chen.
Manuscript editing: Yiling Ding.
Manuscript review: Yiling Ding.
Footnotes
Abbreviations: BMI = body mass index, FFQ = food frequency questionnaire, HDPs = hypertensive disorders of pregnancy, PIH = pregnancy-induced hypertension, SD = standard deviation.
How to cite this article: Chen X, Ding Y, Shi L, Wu D, Wang L, Chen F, Mo Y. Dietary patterns and gestational hypertension in nulliparous pregnant Chinese women: a CONSORT report. Medicine. 2020;99:29(e20186).
The authors have no funding and conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Inoue R, Ohkubo T, Kikuya M, et al. Stroke risk of blood pressure indices determined by home blood pressure measurement: the Ohasama study. Stroke 2009;40:2859–61. [DOI] [PubMed] [Google Scholar]
- [2].Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol 2009;113:1299–306. [DOI] [PubMed] [Google Scholar]
- [3].Mustafa R, Ahmed S, Gupta A, et al. A comprehensive review of hypertension in pregnancy. J Pregnancy 2012;2012:105918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Thoulass JC, Robertson L, Denadai L, et al. Hypertensive disorders of pregnancy and adult offspring cardiometabolic outcomes: a systematic review of the literature and meta-analysis. J Epidemiol Community Health 2016;70:414–22. [DOI] [PubMed] [Google Scholar]
- [5].Wang Z, Wang Z, Wang L, et al. Hypertensive disorders during pregnancy and risk of type 2 diabetes in later life: a systematic review and meta-analysis. Endocrine 2017;55:809–21. [DOI] [PubMed] [Google Scholar]
- [6].Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am J Obstet Gynecol 2000;183:S1–22. [PubMed] [Google Scholar]
- [7].Villegas R, Yang G, Gao YT, et al. Dietary patterns are associated with lower incidence of type 2 diabetes in middle-aged women: the Shanghai Women's Health Study. Int J Epidemiol 2010;39:889–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].He Y, Ma G, Zhai F, et al. Dietary patterns and glucose tolerance abnormalities in Chinese adults. Diabetes Care 2009;32:1972–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Li Y, He Y, Lai J, et al. Dietary patterns are associated with stroke in Chinese adults. J Nutr 2011;141:1834–9. [DOI] [PubMed] [Google Scholar]
- [10].Shi Z, Hu X, Yuan B, et al. Association between dietary patterns and anaemia in adults from Jiangsu Province in Eastern China. Br J Nutr 2006;96:906–12. [DOI] [PubMed] [Google Scholar]
- [11].Cui X, Dai Q, Tseng M, et al. Dietary patterns and breast cancer risk in the shanghai breast cancer study. Cancer Epidemiol Biomarkers Prev 2007;16:1443–8. [DOI] [PubMed] [Google Scholar]
- [12].Hillesund ER, Overby NC, Engel SM, et al. Associations of adherence to the New Nordic Diet with risk of preeclampsia and preterm delivery in the Norwegian Mother and Child Cohort Study (MoBa). Eur J Epidemiol 2014;29:753–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Schoenaker DA, Soedamah-Muthu SS, Callaway LK, et al. Prepregnancy dietary patterns and risk of developing hypertensive disorders of pregnancy: results from the Australian Longitudinal Study on Women's Health. Am J Clin Nutr 2015;102:94–101. [DOI] [PubMed] [Google Scholar]
- [14].Wang D, He Y, Li Y, et al. Dietary patterns and hypertension among Chinese adults: a nationally representative cross-sectional study. BMC Public Health 2011;11:925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kokkinos P, Panagiotakos DB, Polychronopoulos E. Dietary influences on blood pressure: the effect of the Mediterranean diet on the prevalence of hypertension. J Clin Hypertens (Greenwich) 2005;7:165–70. quiz 171-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Sacks FM, Campos H. Dietary therapy in hypertension. N Engl J Med 2010;362:2102–12. [DOI] [PubMed] [Google Scholar]
- [17].Tipton E. Stratified sampling using cluster analysis: a sample selection strategy for improved generalizations from experiments. Eval Rev 2013;37:109–39. [DOI] [PubMed] [Google Scholar]
- [18].Shu L, Zheng PF, Zhang XY, et al. Association between dietary patterns and the indicators of obesity among Chinese: a cross-sectional study. Nutrients 2015;7:7995–8009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Li YP, He YN, Zhai FY, et al. Comparison of assessment of food intakes by using 3 dietary survey methods. Zhonghua Yu Fang Yi Xue Za Zhi 2006;40:273–80. [PubMed] [Google Scholar]
- [20].Newby PK, Tucker KL. Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev 2004;62:177–203. [DOI] [PubMed] [Google Scholar]
- [21].Fraser A, Nelson SM, Macdonald-Wallis C, et al. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon Longitudinal Study of Parents and Children. Circulation 2012;125:1367–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hermes W, Franx A, van Pampus MG, et al. Cardiovascular risk factors in women who had hypertensive disorders late in pregnancy: a cohort study. Am J Obstet Gynecol 2013;208:474.e1-8. [DOI] [PubMed] [Google Scholar]
- [23].Craici I, Wagner S, Garovic VD. Preeclampsia and future cardiovascular risk: formal risk factor or failed stress test? Ther Adv Cardiovasc Dis 2008;2:249–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Steegers EA, von Dadelszen P, Duvekot JJ, et al. Pre-eclampsia. Lancet 2010;376:631–44. [DOI] [PubMed] [Google Scholar]
- [25].Zhao L, Stamler J, Yan LL, et al. Blood pressure differences between northern and southern Chinese: role of dietary factors: the International Study on Macronutrients and Blood Pressure. Hypertension 2004;43:1332–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Roberts JM, Balk JL, Bodnar LM, et al. Nutrient involvement in preeclampsia. J Nutr 2003;133:1684S–92S. [DOI] [PubMed] [Google Scholar]
- [27].Berg CM, Lappas G, Strandhagen E, et al. Food patterns and cardiovascular disease risk factors: the Swedish INTERGENE research program. Am J Clin Nutr 2008;88:289–97. [DOI] [PubMed] [Google Scholar]
- [28].Hajianfar H, Esmaillzadeh A, Feizi A, et al. The association between major dietary patterns and pregnancy-related complications. Arch Iran Med 2018;21:443–51. [PubMed] [Google Scholar]
- [29].Gennari-Moser C, Escher G, Kramer S, et al. Normotensive blood pressure in pregnancy: the role of salt and aldosterone. Hypertension 2014;63:362–8. [DOI] [PubMed] [Google Scholar]
- [30].Magnussen EB, Vatten LJ, Smith GD, et al. Hypertensive disorders in pregnancy and subsequently measured cardiovascular risk factors. Obstet Gynecol 2009;114:961–70. [DOI] [PubMed] [Google Scholar]
- [31].Nielsen LH, Ovesen P, Hansen MR, et al. Changes in the Renin-Angiotensin-Aldosterone system in response to dietary salt intake in normal and hypertensive pregnancy. A randomized trial. J Am Soc Hypertens 2016;10:881–90. e4. [DOI] [PubMed] [Google Scholar]
- [32].Cuco G, Fernandez-Ballart J, Sala J, et al. Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur J Clin Nutr 2006;60:364–71. [DOI] [PubMed] [Google Scholar]
- [33].Crozier SR, Robinson SM, Godfrey KM, et al. Women's dietary patterns change little from before to during pregnancy. J Nutr 2009;139:1956–63. [DOI] [PMC free article] [PubMed] [Google Scholar]


