Highlights
-
•
The scope in the SDGs spanning functions such health-system access and quality care.
-
•
Low-cost quality indicators represent an initiative to improve health outcomes.
-
•
We evaluate the rate of ED-visits and hospital readmission rate after discharge.
-
•
Improvement efforts to reduce these indicators are necessary.
-
•
Strategies to detect causes and avoid potentially preventable factors will be needed.
Keywords: Hospital readmission, Transitions of care, Quality of care, Emergency medical services
Abstract
Background and goal of study
The scope of health in the Sustainable Development Goals is much broader than the Millennium Development Goals, spanning functions such as health-system access and quality of care. Hospital readmission rate and ED-visits within 30 days from discharge are considered low-cost quality indicators. This work assesses an indicator of quality of care in a tertiary referral hospital in Argentina, using data available from clinical records.
Purpose
To estimate the rate of ED-visits and the hospital readmission rate (HRR) after a first hospitalization (First-H), and to identify associated factors.
Methods
This retrospective cohort included patients who had a First-H in Hospital Italiano de Buenos Aires between 2014–2015. Follow-up occurred from discharge until ED-visit, readmission, death, disaffiliation from health insurance, or 13 months. We present HRR at 30 days and ED-visits rate at 72 h, using the Cox proportional-hazards regression model to explore associated factors, and reporting adjusted hazard ratios (HR) with their respective 95 %CI.
Results
The study comprised 10,598 hospitalizations (median age was 68 years). Of these, 5966 had at least one consultation to the ED during follow up, resulting in a 24 h rate of consultations to ED of 1.51 % (95 %CI 1.29−1.72); at 48 h 3.18 % (95 %CI 2.86−3.54); at 72 h 4.71 % (95 %CI 4.32−5.13). In multivariable models, factors associated for 72 h ED-visits were: age (aHR 1.06), male (aHR 1.14), Charlson Comorbidity Index (aHR 1.16), unscheduled hospitalization (aHR 1.39), prior consultation with the ED (aHR 1.08) and long hospital stay (aHR 1.39). Meanwhile, 2345 patients had at least one hospital readmission (98 % unscheduled), resulting a 24 h rate of 0.5 % (95 %CI 0.42−0.71), at 48 h 0.98 % (95 %CI 0.80−1.18), at 72 h 1.4 % (95 %CI 1.2−1.6); at 30 days 7.7 % (95 %CI 7.2−8.2); at 90 days 13 % (95 %CI 12.4–13.8); and one-year 22.5 % (95 %CI 21.7−23.4). Associated factors for HRR at 30 days were: age (HR 1.16), male (HR 1.09), Charlson comorbidities score (HR 1.27), social service requirement during First-H (HR 1.37), unscheduled First-H (HR 1.16), previous ED-visits (HR 1.03) and length of stay (HR 1.08).
Conclusion
Priorities efforts to improve must include greater attention to patients’ readiness prior discharge, to explore causes of preventable readmissions, and better support for patient self-management.
1. Introduction
The 2030 Agenda for Sustainable Development, adopted by all United Nations Member States in 2015, provides a shared blueprint for peace and prosperity for the planet, now and into the future [1]. At its heart are the 17 Sustainable Development Goals (SDGs), which are an urgent call for action by all countries as a global partnership [2]. The SDGs are a set of global goals for fair and sustainable health at every level: from the planetary biosphere to the local community [3]. While only SDG 3 focuses on human health, a goal that aims “to ensure healthy lives and promote well-being for all at all ages”, all goals are interrelated [4]. In fact, it’s recognized that ending poverty and other deprivations must go hand-in-hand with strategies that improve health, education, reduction of inequality, and spur economic growth [5].
The scope of healthcare in the SDGs is much broader than the Millennium Development Goals, spanning functions such as health-system access and quality care. It especially has two monitoring indicators: (1) coverage of essential health services, and (2) catastrophic expenditure on health [6]. Changing health needs, growing public expectations, and ambitious new health goals are raising the bar for health systems to produce better health outcomes and greater social value.
Monitoring indicators plays a crucial role in health care. Hospital readmissions and Emergency Department (ED) visits within 30 days from hospital discharge are considered low-cost quality indicators once access to data through electronic health records are available [[7], [8], [9]]. This indicator has an estimated prevalence of 27 %, representing a frequent problem in all health care systems [10].
It is known that some readmissions can be avoided by improving the hospital discharge process [11]. Patients and their families are the main ones who suffer from this disruption in the health care process, as well as significant economic expenses [12]. Risk factors related to increased rates of readmissions have been already studied, Wang et al. reported an association between the Charlson Comorbidity Index (CCI) and the use of a nasogastric tube, showing an increased risk [13]. Another study by Auerbach et al. reported as risk factors for readmissions, a premature discharge, the lack of medical follow-up and the absence of hospital visits after discharge [14]. Over the years, predictive models have been generated to assess patients with higher probability of being readmitted, detecting vulnerable subgroups of patients to implement accurate strategies to target them [15].
Despite continuous and robust efforts, few data exist to define the frequency of preventable readmissions [16,17]; but there is no doubt that hospital readmissions are expensive and may reflect poor quality of care [18]. In Argentina, risk factors associated have not been deeply studied. The aim of this study was to estimate the consulting rate to ED and the hospital readmission rate (HRR) after a first hospitalization (First-H), and to identify associated factors.
2. Materials and methods
2.1. Setting and participants
Our study took place in the Hospital Italiano de Buenos Aires (HIBA), which includes two highly complex hospitals with a total bed capacity of 785. Additionally, we also have our own private insurance plan (PS-HIBA) with approximately 160.000 affiliated patients.
Eligible patients were 18 years or older, affiliated to PS-HIBA, who had a first episode of hospitalization (first-H) between January 2014 and December 2015. Patients who died during this first-H were excluded from analyses.
Regarding sample size, we assume a readmission rate 30 days after hospital discharge of 11 %, according from bibliography [19], using a precision estimation of 5000 hospitalizations with a hemi amplitude of ±1% and 99 %CI, we decided to include all hospitalizations during the study period.
2.2. Study design and outcomes
We conducted a retrospective cohort using secondary databases. Patients were followed from discharge until consulting to ED, readmission, death, disaffiliation from health insurance or 13 months.
The main outcomes were: the first readmission and/or the first ED-visit during the follow-up period.
The following variables were considered as possible risk factors associated with readmissions or ED-visit: patient's characteristics such as gender, age, marital status, nationality, comorbidities (CCI, COPD). Also, we used administrative information such as first-H type (emergency or scheduled), length of stay, social service or critical care requirements, time using PS-HIBA services, amount of hospitalizations or ED-visits in previous years.
2.3. Data collection
All patient health information is stored in a single Clinical Data Repository (CDR) fed by the hospital electronic health record (EHR). The hospital health system has been evaluated by a recognized international organization (HIMSS, Level 7+) and accredited by the Joint Commission International. The CDR stores clinical documents for each patient, with the highest quality standards worldwide, from different sources such as test results, images, clinical notes, outpatient visits, ED visits, in-hospital care, among other examples.
Ethics approval was obtained from IRB and the project has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. All data were treated with confidentiality and restricted access was given only to researchers involved.
2.4. Statistical analysis
Regarding time to the event for readmissions and ED-visits, it was calculated as a starting point the discharge date of the first-H. The readmission rate and ED-visit rate are presented at 24 h, 48 h, 3 days, 30 days, 90 days, as well as one-year after hospital discharge. To explore associated factors, we first characterized the study patients using univariable methods. Then, we selected potential contributing factors using multivariable models, using the cox proportional-hazards regression model, due this model is a powerful and popular method to analyze survival data (which allows us to formulate the results, when the factor is present, according to the increase in the studied time interval), with the main advantage of the possibility to present unadjusted and adjusted hazard ratios (HRs) with their accompanying 95 %CIs. The choice of Cox model was made based on convenience (for the user and the reader interpretation), availability of computer software, and expertise of researchers team; due the follow-up time was sufficiently short or the survival rate was high.
3. Results
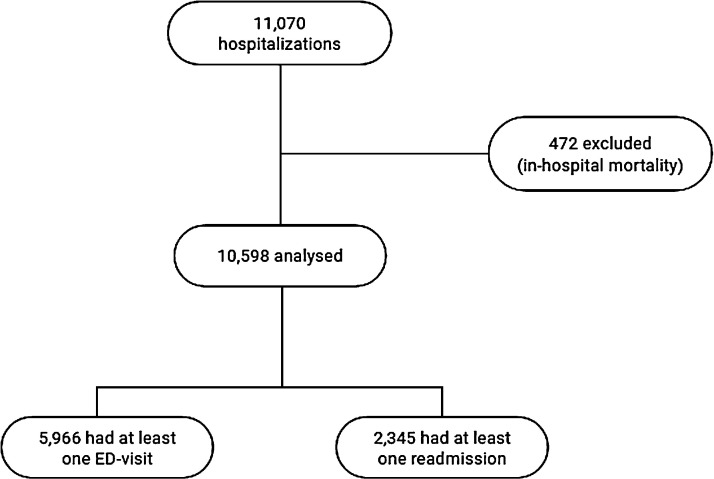
During the study period, 11,070 hospitalizations occurred. Due to in-hospital mortality during First-H, a total of 472 patients were excluded, with 10,598 hospitalizations for the analyses (Fig. 1 ).
Fig. 1.
Flowchart of the study.
The median age of this cohort was 68 years (IQR 45–81), 35.1 % (3717) were male, with a median hospital stay of 3 days (IQR 1−5). Other characteristics of the cohort are listed in Table 1 .
Table 1.
Baseline characteristics.
| All (n = 10,598) | |
|---|---|
| Demographics characteristics | |
| Age, in yearsa | 68.7 (IQR 45.1–81.1) |
| Male gender | 35.7 % (3717) |
| Marital status | |
| Married or common law | 54.6 % (5173) |
| Single, divorced or widow | 45.4 % (4306) |
| Patient background and comorbidities | |
| Time affiliated to PS-HIBA, in yearsa | 8.91 (IQR 4.23–14.54) |
| COPD | 5.8 % (610) |
| Charlson Comorbidity Indexa | 0 (IQR 0–2) |
| First hospitalization characteristics | |
| Scheduled first-H | 46.81 % (4961) |
| Length of stay, in daysa | 3 (IQR 1−5) |
| Long hospital stay (over 5 days) | 24.7 % (2617) |
| Social service requirement | 2.64 % (280) |
| Hospitalized in a surgical unit | 51.76 % (5485) |
| Without one-year prior admission | 87.64 % (9288) |
| With one-year prior critical care requirement | 18.82 % (1995) |
| Without prior ED-visit | 56.29 % (5966) |
Median (IQR: interquartile range).
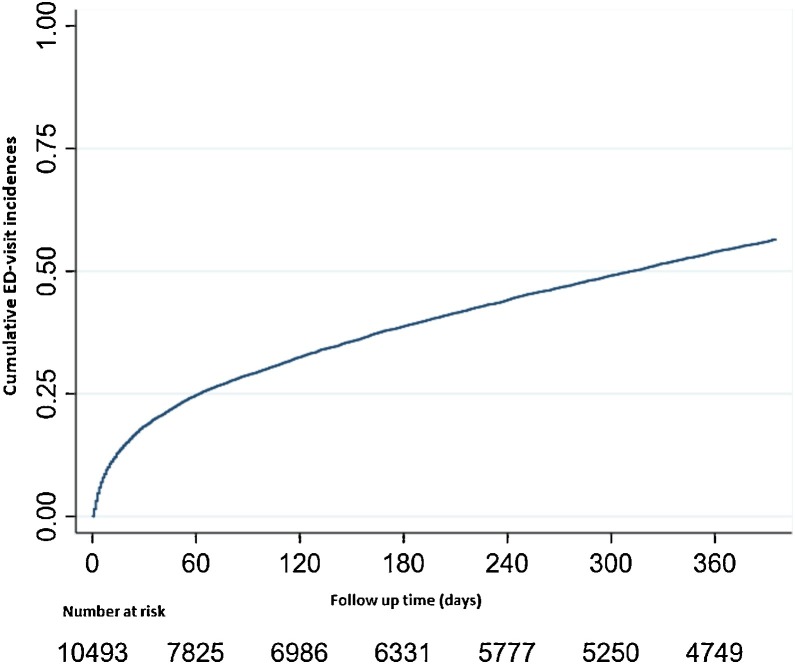
Follow-up during one year period was completed with the exception of 207 patients (1.95 %) who died. Patients who had at least one ED-visit were 5,966. The 24-h ED-visit rate was 1.51 % (95 %CI 1.29−1.72); at 48 h 3.18 % (95 % CI 2.86−3.54); at 3 days 4.71 % (95 %CI 4.32−5.13); at 30 days 18.44 % (95 %CI 17.71−19.19); at 90 days 28.87 % (95 %CI 28.01−29.75); and at one year 54.35 % (95 %CI 53.39−55.31). Table 2 summarizes the cumulative ED-visits for each period, and Fig. 2 shows the cumulative ED-visit incidences after First-H.
Table 2.
Cumulative ED-visits and readmissions incidences in each pre-specified study period.
| ED-visit (n = 5966) | Readmission (n = 2345) | |
|---|---|---|
| 24 h | 1.51 % (95 %CI 1.29−1.72) | 0.5 % (95 %CI 0.42−0.71) |
| 48 h | 3.18 % (95 %CI 2.86−3.54) | 0.98 % (95 %CI 0.80−1.18) |
| 3 days | 4.71 % (95 %CI 4.32−5.13) | 1.4 % (95 %CI 1.2−1.6) |
| 30 days | 18.44 % (95 %CI 17.71−19.19) | 7.7 % (95 %CI 7.2−8.2) |
| 90 days | 28.87 % (95 %CI 28.01−29.75) | 13 % (95 %CI 1.4−13.8) |
| One year | 54.35 % (95 %CI 53.39−55.31) | 22.5 % (95 %CI 21.7−23.4) |
Fig. 2.
Kaplan Meier for cumulative ED-visit incidences after First-H.
After multivariable models, significative associated factors for early ED-visits (less than 72 h) were: age (aHR 1.06; 95 %CI 1.04–1.1; p < 0.01), male gender (aHR 1.14; 95 %CI 1.06−1.24; p < 0.01), unscheduled First-H (aHR 1.39; 95 %CI 1.28−1.50; p < 0.01), prior ED-Visit (aHR 1.08; 95 %CI 1.06−1.08; p < 0.01) and long hospital stay (aHR 1.39; 95 %CI 1.27−1.52; p < 0.01). Table 3 shows other potential underlying factors associated with early ED-visits, even non-significant results.
Table 3.
Potential factors associated with early (less than 72 h) ED-visit or readmission.
| Early ED-visit |
Early readmission |
|||
|---|---|---|---|---|
| Crude HR | Adjusted HR (#) | Crude HR | Adjusted HR (#) | |
| Age, in years * | 1.15 (95 %CI 1.13−1.17) p < 0.001 |
1.06 (95 %CI 1.04−1.10) p < 0.001 | 1.36 (95 %CI 1.32−1.42) p < 0.001 | 1.18 (95 %CI 1.14−1.23) p < 0.001 |
| Male gender | 1.27 (95 %CI 1.18−1.37) p < 0.001 |
1.14 (95 %CI 1.06−1.24) p = 0.001 | 1.27 (95 %CI 1.13−1.43) p < 0.001 | 1.05 (95 %CI 0.93−1.19)p = 0.370 |
| Charlson ** comorbidity index | 1.25 (95 %CI 1.22−1.27) p < 0.001 |
1.16 (95 %CI 1.13−1.20)p < 0.001 | 1.40 (95 %CI 1.36−1.44)p < 0.001 | 1.25(95 %CI 1.21−1.30)p < 0.001 |
| COPD | 1.61 (95 %CI 1.4−18.4) p < 0.001 |
0.92(95 %CI 0.80−1.06)p = 0.285 | 2.14(95 %CI 1.77−2.58)p < 0.001 | 0.92(95 %CI 0.75−1.20)p = 0.412 |
| Social service requirement | 1.65 (95 %CI 1.36−1.99) p < 0.001 |
1.06 (95 %CI 0.87−1.30) p=0.512 |
2.79 (95 %CI 2.19−3.55) p < 0.001 |
1.28 (95 %CI 1.00–1.66) p = 0.049 |
| Non-scheduled First-H | 1.66 (95 %CI 1.54−1.8) p < 0.001 |
1.39 (95 %CI 1.28−1.50) p < 0.001 |
2.78 (95 %CI 2.43−3.19) p < 0.001 |
2.06 (95 %CI 1.78−2.37) p < 0.001 |
| Critical care requirement | 1.51 (95 %CI 1.39−1.65) p < 0.001 |
1.12 (95 %CI 1.02−1.23) p=0.010 |
1.62 (95 %CI 1.42−1.85) p < 0.001 |
1.03 (95 %CI 0.9−1.2) p = 0.581 |
| Prior admissions | 1.1 (95 %CI 1.07−1.13) p < 0.001 |
1 (95 %CI 0.96−1.03) p = 0.929 |
1.17 (95 %CI 1.14−1.21) p < 0.001 |
1.07 (95 %CI 1.02−1.11) p < 0.001 |
| Prior ED-visits | 1.08 (95 %CI 1.07−1.09) p < 0.001 |
1.08(95 %CI 1.06−1.08)p < 0.001 | 1.08(95 %CI 1.07−1.09) p < 0.001 |
1.05 (95 %CI 1.03−1.07) p < 0.001 |
| Length of stay, in days | 1 (95 %CI 1.01−1.02) p < 0.001 |
1 (95 %CI 1.01–1.02) p < 0.001 |
1.01 (95 %CI 1.01−1.02) p < 0.001 |
1 (95 %CI 1−1.01) p < 0.001 |
| Long hospital stay (over 5 days) | 1.9 (95 %CI 1.76−2.06) p < 0.001 |
1.39(95 %CI 1.27−1.52)p < 0.001 | 3,02 (95 % CI 2,69−3,40)p < 0,001 | 1.75 (95 %CI 1.53−2) p < 0.001 |
(#)Adjustment for other significant covariates.
*HR for an increase in 10 years old.
**HR with each increase in one unit of the Charlson comorbidity index.
Meanwhile, significative associated factors for ED-visits at 30 days resulted: age (aHR 1.06; 95 %CI 1.05−1.08; p < 0.01), CCI (aHR 1.16; 95 %CI 1.13−1.18; p < 0.01), unscheduled First-H (aHR 1.26; 95 %CI 1.19−1.33; p < 0.01), previous ED-Visit (aHR 1.07; 95 %CI 1.07−1.08; p < 0.01) and long hospital stay (aHR 1.05; 95 %CI 1.16−1.32; p < 0.01). Table 4 shows all potential risk factors evaluated regarding ED-visits 30 days postdischarge.
Table 4.
Risk factors associated with the first ED-visit or readmission at 30 days (after discharge from First-H).
| ED-visits at 30 days |
Readmission at 30 days |
|||
|---|---|---|---|---|
| Crude HR | Adjusted HR (#) | Crude HR | Adjusted HR (#) | |
| Age * | 1.14 (95 %CI 1.12−1.15) p < 0.001 |
1.06 (95 %CI 1.05−1.08) p < 0.001 |
1.45 (95 %CI 1.4−1.,5) p < 0.001 |
1.16 (95 %CI 1.13−1.20) p < 0.001 |
| Male gender | 1.2 (95 %CI 1.1−1.2) p < 0.001 |
1.07(95 %CI 1.02−1.13)p = 0.007 | 1.22(95 %CI 1.12−1.32) p < 0.001 |
1.09 (95 %CI 1.01−1.17) p < 0.001 |
| CCI ** | 1.2 (95 %CI 1.2−1.3) p < 0.001 |
1.16(95 %CI 1.13−1.18)p < 0.001 | 1.11(95 %CI 1.41−1.46)p < 0.001 | 1.27(95 %CI 1.23−1.29) p < 0.001 |
| COPD | 1.6 (95 %CI 1.5−1.8) p < 0.001 |
0.98 (95 %CI 0.88−1.08) p = 0.719 |
2.4(95 %CI 2.1−2.8) p < 0.001 |
0.94 (95 %CI 0.83−1.06) p = 0.347 |
| Social service requirement | 1.8 (95 %CI 1.5−2.0) p < 0.001 |
1.22(95 %CI 1.06−1.42)p = 0.006 | 3.3 (95 %CI 2.8−3.9)p < 0.001 | 1.37(95 %CI 1.15−1.62) p < 0.001 |
| Non-scheduled First-H | 1.44 (95 %CI 1.4−1.5) p < 0.001 |
1.26(95 %CI 1.19−1.33) p < 0.001 |
2.7 (95 %CI 2.5−2.9) p < 0.001 |
1.16(95 %CI 1.08−1.25) p < 0.001 |
| Critical care requirement | 1.44 (95 %CI 1.4−1.5) p < 0.001 |
1.1(95 %CI 1.03−1.17) p = 0.004 | 1.7(95 %CI 1.5−1.8)p < 0.001 | 0.96(95 %CI 0.89−1.05) p = 0.449 |
| Prior admission (one-year) | 1.1 (95 %CI 1.06−1.11) p < 0.001 |
1(95 %CI 0.98−1.03)p = 0.568 | 1.18 (95 %CI 1.15−1.21)p < 0.001 | 1.17(95 %CI 1.14−1.20) p = 0.014 |
| Prior ED-visit (one-year) | 1.08 (95 %CI 1.07−1.08) p < 0.001 |
1.07(95 %CI 1.07−1.08)p < 0.001 | 1.05 (95 %CI 1.07−1.09) p < 0.001 |
1.03(95 %CI 1.02−1.05)p < 0.001 |
| Length of stay, in days | 1.09 (95 %CI 1.08−1.11) p < 0.001 |
1.05(95 %CI 1.03−1.07) p < 0.001 |
1.01 (95 %CI 1.01−1.02) p < 0.001 |
1.08(95 %CI 1.06−1.10) p < 0.001 |
| Long hospital stay (over 5 days) | 1.65 (95 %CI 1.56−1.75) p < 0.001 |
1.24 (95 %CI 1.16−1.32) p < 0.001 |
2.78 (95 %CI 2.56−3.00) p < 0.001 |
1.52 (95 %CI 1.38−1.67) p < 0.001 |
(#) adjustment for other significant covariates.
*HR for an increase in 10 years old.
**HR with each increase in one unit of the Charlson comorbidity index.
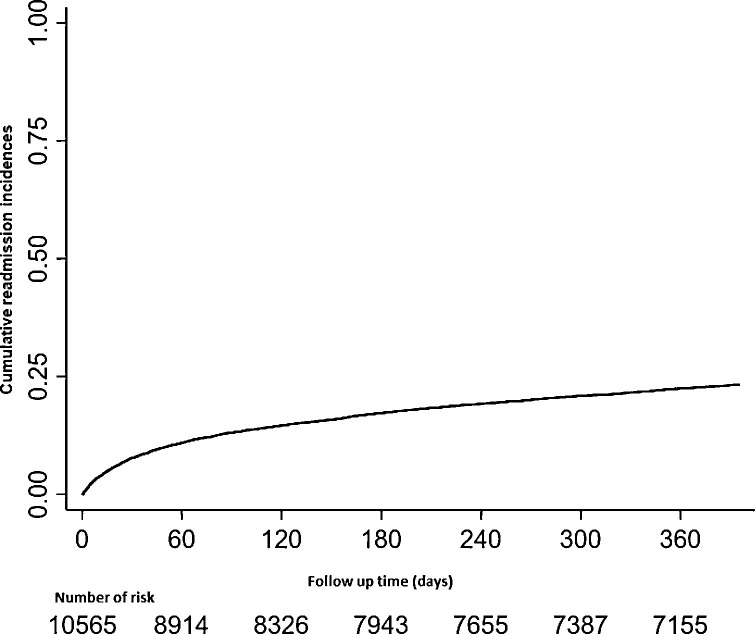
Patients who presented at least one readmission during the follow-up period were 2,345. Of these, 98.46 % (2309) were unscheduled hospitalizations (defined as readmissions that were not scheduled, so patients were admitted by ED entrance). HRR at 24 h was 0.5 % (95 %CI 0.42−0.71), at 48 h 0.98 % (95 %CI 0.80−1.18), at 72 h 1.4 % (95 %CI 1.2−1.6); at 30 days 7.7 % (95 %CI 7.2−8.2); at 90 days 13 % (95 %CI 12.4–13.8); and one-year 22.5 % (95 %CI 21.7−23.4). Table 2 summarizes the cumulative incidences of readmissions for each period. Fig. 3 shows the cumulative readmission incidence after the First-H.
Fig. 3.
Kaplan Meier for cumulative readmission incidences after the First-H.
Regarding associated factors after adjusting for co-variables with 30-day readmissions, the following were significant: age (HR 1.16; 95 %CI 1.13−1.20; p < 0.001), male gender (HR 1.09; 95 %CI 1.01−1.17; p < 0.001), CCI (HR 1.27; 95 %CI 1.23−1.29; p < 0.001), social service requirement during First-H (HR 1.37; 95 %CI 1.15−1.62; p < 0.001), unscheduled First-H (HR 1.16; 95 %CI 1.08−1.25; p < 0.001), previous ED-visits (HR 1.03; 95 %CI 1.02−1,05; p < 0.001) and length of stay (HR 1.08; (95 %CI 1.06−1.10; p < 0.001). Table 4 shows other potential underlying factors that are not significantly associated with 30-day readmissions.
4. Discussion
In our hospital, 18 % of patients made a new consultation at the ED and 8% of patients were readmitted within 30 days after discharge. These rates represent two manifestations of the same phenomenon underlying the need for medical care, both are easy to measure and the data necessary for their calculation were highly available.
Our findings were similar to other contexts, Wang et al. estimated these rates at a tertiary hospital in Taiwan yielding 12 % and 14 % respectively [20]. Although they share characteristics of the population in terms of age, sex, and comorbidities, they differ in the type of cohort: our study was based on a closed cohort of patients with exclusive care within the same system, while the other used an open system with patients referred or attended in other centers from which the follow-up information is lost. However, it was lower compared to that reported by Padilla et al. (11.16 %, 95 %CI 10.99–11.33) at the Hospital Alemán [21]. Although both studies were carried out in private hospitals with similar characteristics in the same city, they were not comparable as they included 12 % of first index hospitalizations corresponding to pediatric patients.
It is of great clinical relevance to defining the readmission time window since very short time windows could lose readmissions while very long time windows increase the probability that readmissions are not related to index hospitalization [22]. That is why the use of these rates as an indicator of quality of care is useful as a self-comparison measure over time with the aim of detecting the associated factors that allow rethinking and installing improvement cycles [23].
Regarding associated factors, in our study, we report some variables related to indirect indicators of severity of the index hospitalization, such as unscheduled hospitalization in the First-H, transfer to a closed unit, prior ED-visits and long hospital stays. Similarly, Shu et al. reported that an increase in hospital stay in the index hospitalization was associated with an increased risk of unscheduled hospitalizations [24]. On the other hand, and similar to a study by Navathe et al. where they reported an association of social factors such as poor social support in hospitalized patients [25], we detected that the presence of social service requirements, as an indirect indicator of social risk at discharge, in the index hospitalization was associated with ED-visits and unscheduled readmissions.
Another limitation to recognize is the potential information bias in the registry of some of the variables (comorbidities and COPD), also due to the retrospective nature of the study in which secondary bases were used [26]. Although, a strength undoubtedly to be mentioned is the importance of the electronic medical record as a key factor for the feasibility of data collection for our study, as well as for the improvement in its recording. The EHR made it possible to provide local data on the rate of readmissions that have not been studied in-depth in our country. This represents an essential first step to be able to use them as a quality indicator. Additionally, as it was a closed cohort study, it was possible to calculate the rates with better precision, minimizing selection bias.
Organizing and a better understanding of hospital monitoring indicators becomes highly important nowadays due to the new COVID‐19 threatening the world [27]. In consequence, hospitals and EDs are facing a hard time to adapt. The enormous demand for handling the outbreak challenges the health care personnel, the medical supply, and the health system organization as a whole.
The COVID-19 pandemic increases the need to have high-quality monitored health systems able to adapt to each given context, responding to population needs [3]. The hospital, and particularly the ED, undertook the mission of clinical reception, primary diagnosis, and initial treatment for COVID‐19 cases [28]. That's why the ED has become one of the highest priorities. We focused on providing staff and qualified protection equipment, rescheduling non-urgent visits, and in canceling scheduled surgeries to reduce possible hospital overload [28].
Health systems need to develop the capacity to measure, use of data to learn and respond. This article represents an example of the use of digital solutions and data science initiatives to collect, process, analyze, and disseminate data to track progress and informed decision support to achieve the health-related SDGs. Our experience represents an empirical monitoring effort on moving towards more standardized and universal assessments. Continued collaboration is important to bring proxy measures closer to definitions and their metadata. According to a goal that aims to SDG 3 [29], future data could help to gain insight in order to understand driving mechanisms behind high readmission rates, in order to ensure the quality of care, and that no one is left out due to lack of access to health care.
5. Conclusions
Multicomponent care transition programs are a desired approach to improve patient outcomes in the period after acute care. Our results only suggest a potential approach with interventions that guarantee a continuum of care necessary to support patients and improve outcomes during the period after hospitalization. In this way, efforts must focus to prepare patients more effectively for discharge, and to provide better ability for patients, caregivers, and health care professionals. Further attention to measurement readmissions will be necessary, such as to explore causes, as an opportunity to reduce them.
Summary table
What was already known before the study
-
•
The scope in the SDGs spanning functions such as health-system access and quality care.
-
•
Low-cost quality indicators represents an initiative to improve health outcomes.
What this study has added to the body of knowledge
-
•
Describes the development and use of quality indicators: rate of ED-visits and hospital readmission rate (HRR) after hospital discharge.
-
•
Our findings suggest a potential approach with the necessary interventions to ensure continuity of care and improve outcomes after hospitalization.
-
•
Efforts will need to be improved, as well as strategies to detect causes and avoid potentially preventable factors to reduce these indicators.
Contributors’ information
DHG and JP conceived the original idea. BRB, LA and MFGR wrote the protocol and they made the statistical analyses. SMF, BB and MFGR wrote and translated the manuscript. BM and DL made critical feedback and institutional support. All authors contributed to the final version of the manuscript.
Funding
This work has been partly supported by an unrestricted research grant from: “BECA ISALUD de Investigación 2017 Dr. Mario González Astorquiza”, by giving the first author 30 % of his working time available for research.
Role of the sponsor
The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Declaration of competing interests
The authors have no conflict of interests to declare.
Acknowledgements
Dr Ada CHAROSKY. Unidad de planificación de altas (UPA), Servicio de Clínica Médica, Hospital Italiano de Buenos Aires. Buenos Aires (HIBA), Argentina.
Dr Norberto Claudio DI MASCIO. Unidad de planificación de altas (UPA), Servicio de Clínica Médica, Hospital Italiano de Buenos Aires. Buenos Aires (HIBA), Argentina.
Dr Marina ALONSO SERENA. Department of Internal Medicine, Hospital Italiano de Buenos Aires, Ciudad de Buenos Aires, Argentina.
Dr Gabriela A. BLUGERMAN. Gestión de la Información para la Investigación, Departamento de Investigación - Hospital Italiano de Buenos Aires, Argentina.
References
- 1.Morton S., Pencheon D., Squires N. Sustainable Development Goals (SDGs), and their implementation: a national global framework for health, development and equity needs a systems approach at every level. Br. Med. Bull. 2017;124(December (1)):81–90. doi: 10.1093/bmb/ldx031. [DOI] [PubMed] [Google Scholar]
- 2.2020. United Nations Official Document. Transforming our world: the 2030 Agenda for Sustainable Development: Resolution adopted by the General Assembly on 25 September 2015. Available from: http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E [Cited 18 June 2020] [Google Scholar]
- 3.Kruk M.E., Gage A.D., Arsenault C., Jordan K., Leslie H.H., Roder-DeWan S. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob. Health. 2018;6(November (11)):e1196–e1252. doi: 10.1016/S2214-109X(18)30386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acharya S., Lin V., Dhingra N. The role of health in achieving the sustainable development goals. Bull. World Health Organ. 2018;96(September (9)) doi: 10.2471/BLT.18.221432. 591–591A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brolan C.E., Hall N., Creamer S., Johnston I., Dantas J.A. Health’s role in achieving Australia’s sustainable development goal commitments. Med. J. Aust. 2019;210(March (5)) doi: 10.5694/mja2.50040. 204–6.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Witthayapipopsakul W., Kulthanmanusorn A., Vongmongkol V., Viriyathorn S., Wanwong Y., Tangcharoensathien V. Achieving the targets for universal health coverage: how is Thailand monitoring progress? WHO South East Asia J. Public Health. 2019;8(April (1)):10–17. doi: 10.4103/2224-3151.255343. [DOI] [PubMed] [Google Scholar]
- 7.Donabedian A. 1980. The Definition of Quality and Approaches to Its Assessment. p.163. [Google Scholar]
- 8.Pincus H.A., Spaeth-Rublee B., Watkins K.E. The case for measuring quality in mental health and substance abuse care. Health Aff. 2011;30(4):730–736. doi: 10.1377/hlthaff.2011.0268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine (US) Committee on Quality of Health Care in America . National Academies Press (US); Washington (DC): 2014. Crossing the Quality Chasm: A New Health System for the 21st Century. [PubMed] [Google Scholar]
- 10.Auerbach A.D., Kripalani S., Vasilevskis E.E., Sehgal N., Lindenauer P.K., Metlay J.P. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern. Med. 2016;176(4):484. doi: 10.1001/jamainternmed.2015.7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finlayson K., Chang A.M., Courtney M.D., Edwards H.E., Parker A.W., Hamilton K. Transitional care interventions reduce unplanned hospital readmissions in high-risk older adults. BMC Health Serv. Res. 2018;18(December (1)):956. doi: 10.1186/s12913-018-3771-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou H., Della P.R., Roberts P., Goh L., Dhaliwal S.S. Utility of models to predict 28-day or 30-day unplanned hospital readmissions: an updated systematic review. BMJ Open. 2016;6(June (6)) doi: 10.1136/bmjopen-2016-011060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang C.-L., Ding S.-T., Hsieh M.-J., Shu C.-C., Hsu N.-C., Lin Y.-F. Factors associated with emergency department visit within 30 days after discharge. BMC Health Serv. Res. 2016;16(May):190. doi: 10.1186/s12913-016-1439-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Auerbach A.D., Kripalani S., Vasilevskis E.E., Sehgal N., Lindenauer P.K., Metlay J.P. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern. Med. 2016;176(4):484. doi: 10.1001/jamainternmed.2015.7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou H., Della P.R., Roberts P., Goh L., Dhaliwal S.S. Utility of models to predict 28-day or 30-day unplanned hospital readmissions: an updated systematic review. BMJ Open. 2016;6(June (6)) doi: 10.1136/bmjopen-2016-011060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Walraven C., Bennett C., Jennings A., Austin P.C., Forster A.J. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(April (7)):E391–E402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jackson A.H., Fireman E., Feigenbaum P., Neuwirth E., Kipnis P., Bellows J. Manual and automated methods for identifying potentially preventable readmissions: a comparison in a large healthcare system. BMC Med. Inform. Decis. Mak. 2014;14(April):28. doi: 10.1186/1472-6947-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Walraven C., Jennings A., Forster A.J. A meta-analysis of hospital 30-day avoidable readmission rates. J. Eval. Clin. Pract. 2012;18(December (6)):1211–1218. doi: 10.1111/j.1365-2753.2011.01773.x. [DOI] [PubMed] [Google Scholar]
- 19.Padilla I.S., Centeno J., Engwald C.D., Díaz Maffini M.M. VI Congreso Argentino De Informática Y Salud (CAIS) — JAIIO 44 (Rosario, 2015) 2015. Uso secundario de una historia clínica digital para el análisis de las reinternaciones en un hospital de la comunidad en Argentina. Available from: http://hdl.handle.net/10915/54835 [Cited 9 October 2017] [Google Scholar]
- 20.Wang C.-L., Ding S.-T., Hsieh M.-J., Shu C.-C., Hsu N.-C., Lin Y.-F. Factors associated with emergency department visit within 30 days after discharge. BMC Health Serv. Res. 2016;16(May):190. doi: 10.1186/s12913-016-1439-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Padilla I.S., Centeno J., Engwald C.D., Díaz Maffini M.M. VI Congreso Argentino De Informática Y Salud (CAIS) — JAIIO 44 (Rosario, 2015) 2015. Uso secundario de una historia clínica digital para el análisis de las reinternaciones en un hospital de la comunidad en Argentina. Available from: http://hdl.handle.net/10915/54835 [Cited 9 October 2017] [Google Scholar]
- 22.Fischer C., Lingsma H.F., de Mheen P.J.M., Kringos D.S., Klazinga N.S., Steyerberg E.W. Is the readmission rate a valid quality Indicator? A review of the evidence. PLoS One. 2014;9(11) doi: 10.1371/journal.pone.0112282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barzegari H., Fahimi M.A., Dehghanian S. Emergency department readmission rate within 72 hours after discharge; a letter to editor. Emerg. (Tehran) 2017;5(April (1)):e64. [PMC free article] [PubMed] [Google Scholar]
- 24.Shu C.-C., Lin Y.-F., Hsu N.-C., Ko W.-J. Risk factors for 30-day readmission in general medical patients admitted from the emergency department: a single centre study. Intern. Med. J. 2012;42(June (6)):677–682. doi: 10.1111/j.1445-5994.2011.02562.x. [DOI] [PubMed] [Google Scholar]
- 25.Navathe A.S., Zhong F., Lei V.J., Chang F.Y., Sordo M., Topaz M. Hospital readmission and social risk factors identified from physician notes. Health Serv. Res. 2018;53(April (2)):1110–1136. doi: 10.1111/1475-6773.12670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grande Ratti M.F., Posadas-Martínez M.L., Giunta Diego H. Vol. 36. 2016. pp. 17–18. (Estudios de cohorte. Revista Hospital Italiano de Buenos Aires). March (No 1), Available from: https://www1.hospitalitaliano.org.ar/multimedia/archivos/noticias_attachs/47/documentos/24549_17-18-HI1-3-Ratti-A.pdf. [Google Scholar]
- 27.Yi Y., Lagniton P.N.P., Ye S., Li E., Xu R.-H. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int. J. Biol. Sci. 2020;16(March (10)):1753–1766. doi: 10.7150/ijbs.45134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cao Y., Li Q., Chen J., Guo X., Miao C., Yang H. Hospital emergency management plan during the COVID-19 epidemic. Acad. Emerg. Med. 2020;(April (4)):309–311. doi: 10.1111/acem.13951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Asma S., Lozano R., Chatterji S., Swaminathan S., de Fátima Marinho M., Yamamoto N. Monitoring the health-related Sustainable Development Goals: lessons learned and recommendations for improved measurement. Lancet. 2020;395(January (10219)):240–246. doi: 10.1016/S0140-6736(19)32523-1. [DOI] [PubMed] [Google Scholar]