Short abstract
Watch an interview with the author
Abbreviations
- DAA
direct‐acting antiviral
- ECHO
Extension for Healthcare Outcomes
- HCV
hepatitis C virus
- IHS
Indian Health Service
- UNM
University of New Mexico
Sixteen years ago we founded Project ECHO (Extension for Healthcare Outcomes) to address New Mexico’s hepatitis C virus (HCV) crisis. More than 28,000 New Mexicans were diagnosed with HCV, but fewer than 5% were receiving treatment. Our Albuquerque clinic at the University of New Mexico (UNM) had an 8‐month waiting list. Many of our patients lived hundreds of miles away in rural communities, facing the costs of multiple long drives, missed work, and child care to get treatment. Too many of them arrived with cirrhosis or fatal liver cancers that could have been prevented. The cure for HCV existed, but patients were unable to access it.
Our solution, the ECHO model, used one‐to‐many videoconferencing technologies to connect a team of specialists at our UNM “hub” with community providers across the state for mentoring and guided practice to treat HCV in their own communities. HCV treatment at the time was a complex, chemotherapy‐like regimen of ribavirin and interferon, often involving significant side effects. ECHO program participants gradually became experts at managing HCV. Within 18 months, our clinic wait times fell to 2 weeks. Participants reported increased knowledge and self‐efficacy, and gave their patients the same level of care as the UNM specialists.1
Thanks to the development of direct‐acting antiviral (DAA) drugs, treatment for HCV is now simpler and more effective. Yet the global challenge remains: in 2017, the World Health Organization reported that 19% of the estimated 71 million people living with HCV infection knew their diagnosis, and only 5 million of those diagnosed had been treated.2 Significant barriers to treatment access persist, especially for marginalized or underserved populations. A major barrier is a shortage of providers trained to treat HCV effectively, despite the simplicity of DAA therapy.3 Guidance in the evaluation of liver disease and in the management of complex patients through integrative care is critical to the success of efforts to eradicate HCV.
Telemedicine (i.e., patient management using video or online asynchronous consultation with distant specialists) has shown promise in expanding patient access to care, especially as broadband technology and cell phone/Internet usage have expanded.4 Yet telemedicine remains limited so long as it enables only one specialist to treat one patient. It does not solve the specialist shortage and expand the capacity of health care systems to address the global HCV burden. More comprehensive approaches are needed, enabling task‐shifting so that nonspecialist providers (nurse practitioners, physician assistants, nurses, pharmacists) can provide treatment in areas where physicians are scarce. Such approaches should also facilitate integrated care protocols, recognizing HCV’s coexistence with other conditions and the complexity of individual patient’s lives and needs.5
As the use of the ECHO model for HCV has grown, we have found that ECHO programs, which focus on one‐to‐many mentoring, guided practice, and a multidisciplinary team approach to patient care, enable and scale both task‐shifting and integrated care approaches across geographical and cultural contexts6 (Fig. 1).
Figure 1.
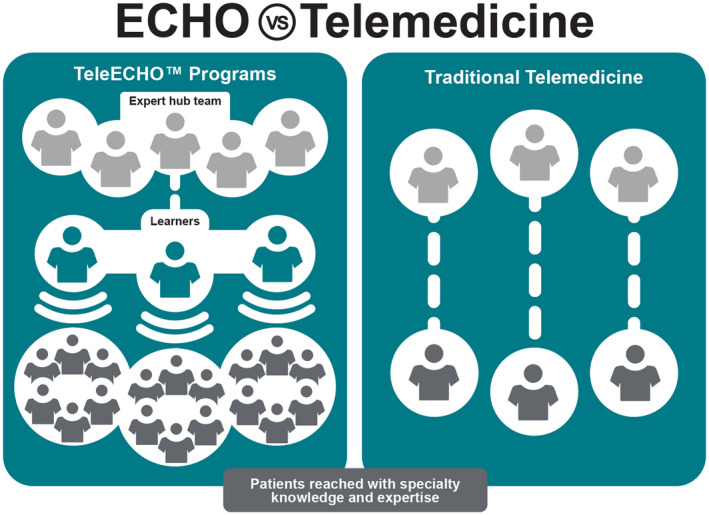
Project ECHO versus traditional telemedicine. Courtesy ECHO Institute.
There are currently 27 HCV ECHO hubs in 21 US states and 16 international HCV ECHO programs. We partner with the New Mexico Departments of Health and Corrections to train providers serving urban, rural, and incarcerated populations. We work with the US Indian Health Service (IHS) on an HCV ECHO program with 16 IHS and tribal spoke clinics across New Mexico. Recent unpublished data have shown that in 2018, 100% of prescriptions for HCV medications filled by the IHS national supply center for NM were prescribed by ECHO participating sites. ECHO programs run by the Department of Veterans Affairs have improved survival rates of veterans with liver disease by 50% and have significantly increased rates of antiviral treatment in veterans with chronic HCV, with cure rates identical to those achieved in specialist care.7, 8 In India, the Government of Punjab used ECHO to scale up a free HCV treatment program, with more than 29,000 new patients diagnosed and treated during the program’s first year, and cure rates exceeding 90%.9 The country of Georgia is also using ECHO to support its HCV elimination program10 (Fig. 2).
Figure 2.

HCV ECHO programs around the world. Courtesy ECHO Institute.
We have the knowledge and treatments necessary to eliminate HCV if we can overcome systemic barriers to their dissemination. Innovations such as telemedicine, integrative care, and Project ECHO provide pathways forward.
Potential conflict of interest: Nothing to report.
References
- 1. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med 2011;364:2199‐2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jefferies M, Rauff B, Rashid H, et al. Update on global epidemiology of viral hepatitis and preventive strategies. World J Clin Cases 2018;6:589‐599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zevin B. Managing chronic hepatitis C in primary‐care settings: more than antiviral therapy. Public Health Rep 2007;122(Suppl. 2):78‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Serper M, Volk M. Current and future applications of telemedicine to optimize the delivery of care in chronic liver disease. Clin Gastroenterol Hepatol 2018;16:157‐161.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ho S, Brau N, Cheung R, et al. Integrated care increases treatment and improves outcomes of patients with chronic hepatitis C virus infection and psychiatric illness or substance abuse. Clin Gastroenterol Hepatol 2015;13:2005‐2014.e1‐3. [DOI] [PubMed] [Google Scholar]
- 6. Arora S. Project ECHO: Democratising knowledge for the elimination of viral hepatitis. Lancet Gastroenterol Hepatol 2019;4:91‐93. [DOI] [PubMed] [Google Scholar]
- 7. Beste L, Glorioso TJ, Ho PM, et al. Telemedicine specialty support promotes hepatitis C treatment by primary care providers in the Department of Veterans Affairs. Am J Med 2017;130:432‐438.e3. [DOI] [PubMed] [Google Scholar]
- 8. Su GL, Glass L, Tapper E, et al. Virtual consultations through the veterans administration SCAN‐ECHO project improves survival for veterans with liver disease. Hepatology 2018;68:2317‐2324. [DOI] [PubMed] [Google Scholar]
- 9. Dhiman R, Grover G, Premkumar M, et al. Decentralized care is effective in the management of patients with hepatitis C in a public health care setting: the Punjab model. European Association for the Study of the Liver 2018 Congress. Hepatology 2018;68(Suppl. 1):S50‐S64. [Google Scholar]
- 10. Tsertsvadze T, Gamkrelidze A, Chkhartishvili C, et al. Three years of progress towards achieving hepatitis C elimination in the country of Georgia, April 2015‐March 2018. Clin Infect Dis 2019;2019:ciz956. [DOI] [PMC free article] [PubMed] [Google Scholar]


