To the Editor:
Patients at high risk for mortality from COVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), are more likely to be older and male and have chronic diseases such as hypertension, diabetes, cardiovascular, and chronic lung disease [1, 2]. Although the mechanisms behind these associations are poorly understood, this increased risk could be partly associated with increased expression of the cellular receptor of SARS-CoV-2, angiotensin-converting enzyme-2, found at elevated levels in older individuals, men, and in cardiovascular and inflammatory conditions [3, 4]. It maintains homeostasis of the renin-angiotensin system and converts angiotensin II to angiotensin 1-7, which has vasodilatory and anti-inflammatory properties. The membrane-bound form (mACE2) is highly expressed in the heart, airways, kidney, and liver tissue, and the enzymatically active soluble form (sACE2) is generated in response to inflammatory signals and disease via mACE2 shedding.
We interrogated the associations between plasma concentrations of sACE2 and biomarkers of metabolic syndrome (body mass index, BMI; blood pressure; glycemic markers; and lipid levels), adiposity (plasma leptin and serum adiponectin), inflammation (high-sensitivity C-reactive protein, hsCRP, white blood cell count, and interleukin-8), and liver damage (alanine aminotransferase, aspartate transaminase, and gamma-glutamyl-transferase, GGT) in a large cohort of participants in a commercial wellness program who had undergone comprehensive multi-omic profiling (N = 2051; 1238 women and 813 men, aged 22 to 87 years, M = 47.3, SD = 11.71) (see [5] for details). Clinical laboratory tests were performed in CLIA-certified laboratories by Quest Diagnostics or LabCorp. Plasma sACE2 and leptin levels were measured via proximity extension immunoassaying using Olink® Cardiovascular II proteomics panel. Analyses were performed using transformed and scaled biomarker values in a robust linear regression framework controlling for age, sex (where appropriate), 8 genetic principal components, smoking, vendor, season, use of diabetes, cholesterol-lowering, and ACE-inhibitor medications.
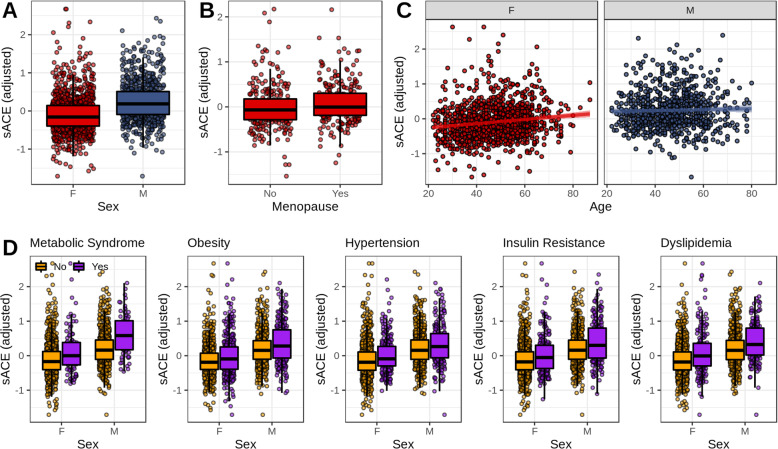
Confirming results from recent studies [3, 4], we found higher plasma sACE2 levels in men compared to women (P = 2 × 10−16), and in older individuals (P = 8.6 × 10−11), with the age association more pronounced in women (for the interaction, Pint = 0.02). We found higher levels of sACE2 in post-menopausal women, compared to pre-menopausal women (P = 0.02; see Fig. 1).
Fig. 1.
The associations of plasma sACE2 levels with sex, age, and metabolic syndrome (MetS). a Sex differences in plasma sACE2 levels. b Differences in sACE2 levels between pre- (N = 272) and post-menopausal (N = 251) women over 35 years of age. c Associations between sACE2 and age. d Differences in sACE2 levels in individuals who do vs. who do not meet diagnostic criteria for MetS and its subcomponents. The following diagnostic criteria, based on WHO guidelines, were used: obesity, BMI > 30 kg/m2; hyperglycemia, fasting glucose > 100 mg/dl or other evidence of insulin resistance (e.g., prescription); hypertension, systolic/diastolic blood pressure ≥ 140/90 mm/hg; dyslipidemia, triglycerides > 150 or HDL-C < 35 for men and < 39 for women. Overall status was determined as MetS if the individual met criteria for insulin resistance and satisfied at least one other domain criterion for the syndrome. sACE2, soluble ACE2 (normalized protein expression, NPX, values adjusted for covariates and scaled)
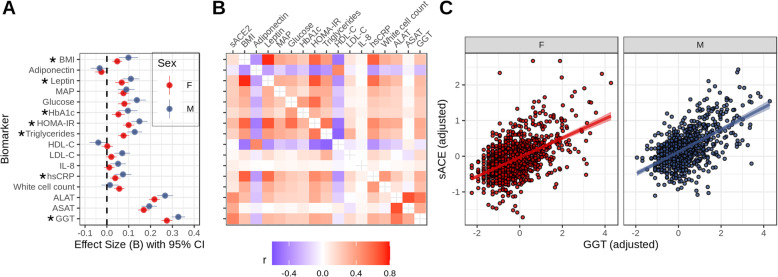
Individuals who met World Health Organization’s diagnostic criteria for metabolic syndrome (MetS) (N = 171) displayed elevated plasma sACE2 levels compared to controls (N = 1880; P = 4.7 × 10− 5); the effect was stronger in men (Pint = 8.9 × 10− 5). All of MetS component biomarkers were positively associated with plasma sACE2 (see Fig. 2). The associations were significantly stronger in men for biomarkers of obesity and adiposity (BMI, Pint = 0.0123; leptin, Pint = 0.0342) and insulin resistance and hyperglycemia (HbA1c, Pint = 0.0368; HOMA-IR, Pint = 0.042), as well as triglycerides (Pint = 0.0134) and serum hsCRP (Pint = 0.041). The strongest association was observed between sACE2 and GGT (P = 3.44 × 10−90), an important indicator of oxidative stress, liver, and bile duct damage. This association was also stronger in men (Pint = 0.01).
Fig. 2.
Associations between sACE2 and biomarkers of metabolic syndrome, inflammation, and liver damage. a Marginal Effect size (B) estimates from robust linear regressions predicting sACE2 from biomarkers estimated for men and women separately. Biomarkers for which a significant interaction with sex was established are marked with an asterisk. b Partial Spearman correlations between study biomarkers and sACE2 levels. c Scatterplot of associations between GGT and sACE2. BMI, body mass index; MAP, mean arterial blood pressure; HbA1c, glycohemoglobin A1c; HOMA-IR, homeostatic model assessment of insulin resistance; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; IL-8, interleukin 8; hsCRP, high-sensitivity C-reactive protein; ALAT, alanine aminotransferase; ASAT, aspartate transaminase; GGT, gamma-glutamyl-transferase
The robust pattern of associations between increased plasma sACE and MetS points to the possible shared pathways in cardiometabolic disease and COVID-19, implicating insulin resistance, chronic inflammation, and liver damage. This is intriguing given that both sACE2 and mACE2 have been shown to be upregulated in a rat model of chronic liver disease [6] and that sACE2 levels are higher in patients with heart failure [4]. The upregulation may be related to the tissue-specific patterns of increased SARS-CoV-2 infectivity in patients with cardiometabolic disease and/or liver damage and warrants further research on sACE2 as a potential biomarker for COVID-19 severity.
Acknowledgements
The authors express their gratitude to the members of the Arivale program for granting the permission to use their deidentified data for research and to Mr. Brett Smith at the Institute for Systems Biology for his contribution to the study.
Abbreviations
- sACE2/mACE2
Soluble/membrane-bound angiotensin-converting enzyme-2
- MetS
Metabolic syndrome
- GGT
Gamma-glutamyl-transferase
- BMI
Body mass index
- HbA1c
Glycohemoglobin A1c
- HOMA-IR
Homeostatic model assessment of insulin resistance
- hsCRP
High-sensitivity C-reactive protein
Authors’ contributions
SK, ILB, KJ, JL, CD, and AM conceptualized the study and drafted the manuscript. SK, CD, and AM performed data quality control and assurance, transformation, and data analysis. All authors critically revised the manuscript. The authors read and approved the final manuscript.
Funding
No external funding was received to complete this study.
Availability of data and materials
The dataset supporting the conclusions of this article is available from the authors upon request.
Ethics approval and consent to participate
All research was conducted in accordance to regulations and guidelines for observational research in human subjects. The study was reviewed and approved by the Western IRB (study number 1178906). The research was performed entirely using deidentified and aggregated data of individuals who had signed a research authorization allowing the use of their anonymized data in research. Per current US regulations for use of deidentified data, informed consent was not required.
Consent for publication
Not applicable.
Competing interests
The authors were previously employed by Arivale, Inc. and held stock options in the company. Arivale is now closed.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tian W, Jiang W, Yao J, et al. Predictors of mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. J Med Virol. 2020. 10.1002/jmv.26050. [DOI] [PMC free article] [PubMed]
- 2.Guo W, LM, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diab Metab Res Rev. 2020:e3319. [DOI] [PMC free article] [PubMed]
- 3.Swärd P, Edsfeldt A, Reepalu A, Jehpsson L, Rosengren BE, Karlsson MK. Age and sex differences in soluble ACE2 may give insights for COVID-19. Crit Care. 2020;24(1):221. doi: 10.1186/s13054-020-02942-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sama IE, Ravera A, Santema BT, et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J. 2020;41(19):1810–1817. doi: 10.1093/eurheartj/ehaa373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zubair N, Conomos M, Hood L, et al. Genetic predisposition impacts clinical changes in a lifestyle coaching program. Sci Rep. 2019;9:6805. doi: 10.1038/s41598-019-43058-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herath CB, Warner FJ, et al. Upregulation of hepatic Upregulation of hepatic angiotensin-converting enzyme 2 (ACE2) and angiotensin-(1–7) levels in experimental biliary fibrosis. J Hepatol. 2007;47(3):387–395. doi: 10.1016/j.jhep.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is available from the authors upon request.