Abstract
Aims
The long‐term impact of coffee or tea consumption on subclinical left ventricular (LV) systolic or diastolic function has not been previously studied. We examined the association between coffee or tea consumption beginning in early adulthood and cardiac function in midlife.
Methods and results
We investigated 2735 Coronary Artery Risk Development in Young Adults (CARDIA) study participants with long‐term total caffeine intake, coffee, and tea consumption data from three visits over a 20 year interval and available echocardiography indices at the CARDIA Year‐25 exam (2010–2011). Linear regression models were used to assess the association between caffeine intake, tea, and coffee consumption (independent variables) and echocardiography outcomes [LV mass, left atrial volume, and global longitudinal strain (GLS), LV ejection fraction (LVEF), and transmitral Doppler early filling velocity to tissue Doppler early diastolic mitral annular velocity (E/e´)]. Models were adjusted for standard cardiovascular risk factors, socioeconomic status, physical activity, alcohol use, and dietary factors (calorie intake, whole and refined grain intake, and fruit and vegetable consumption). Mean (standard deviation) age was 25.2 (3.5) years at the CARDIA Year‐0 exam (1985–1986), 57.4% were women, and 41.9% were African‐American. In adjusted multivariable linear regression models assessing the relationship between coffee consumption and GLS, beta coefficients when comparing coffee drinkers of <1, 1–2, 3–4, and >4 cups/day with non‐coffee drinkers were β = −0.30%, P < 0.05; β = −0.35%, P < 0.05; β = −0.32%, P < 0.05; β = −0.40%, P > 0.05; respectively (more negative values implies better systolic function). In adjusted multivariable linear regression models assessing the relationship between coffee consumption and E/e´, beta coefficients when comparing coffee drinkers of <1, 1–2, 3–4, and >4 cups/day with non‐coffee drinkers were β = −0.29, P < 0.05; β = −0.38, P < 0.01; β = −0.20, P > .05; and β = −0.37, P > 0.05, respectively (more negative values implies better diastolic function). High daily coffee consumption (>4 cups/day) was associated with worse LVEF (β = −1.69, P < 0.05). There were no associations between either tea drinking or total caffeine intake and cardiac function (P > 0.05 for all).
Conclusions
Low‐to‐moderate daily coffee consumption from early adulthood to middle age was associated with better LV systolic and diastolic function in midlife. High daily coffee consumption (>4cups/day) was associated with worse LV function. There was no association between caffeine or tea intake and cardiac function.
Keywords: Coffee, Tea, caffeine, Left ventricle, Left ventricular function
1. Introduction
Coffee and tea are among the most widely consumed beverages. More than half of adults in the United States drink at least one cup of coffee each day, and this proportion is expected to increase with the aging of the population. 1 Given that a substantial amount of people drink coffee or tea, even small cardiovascular benefits or risks associated with their consumption may have significant population attributable risk. An important area of scientific inquiry is the role of coffee or tea consumption on heart failure (HF)—a leading causes of morbidity and mortality that is projected to worsen over the next decade. 2 Studies examining the association between coffee or tea consumption and HF have been inconsistent. Separate studies have shown positive, neutral, or negative associations between these beverages and adverse outcomes. 3 , 4 , 5 , 6 , 7 Examining associations between coffee, caffeine, or tea consumption and subclinical cardiac dysfunction may elucidate underlying mechanisms and provide further insights about HF risk. In this context, it is well established that antecedent cardiac dysfunction precedes the onset of overt HF. 8 We investigated the association between daily coffee, caffeine, or tea consumption in the early adult lifespan and subclinical cardiac function in middle age using data from the Coronary Artery Risk Development in Young Adults (CARDIA) study.
2. Methods
The CARDIA study is a community‐based cohort study designed to investigate the development and determinants of cardiovascular disease in 5115 men and women initially aged 18–30 years at study baseline. 9 Participants were recruited between 1985 and 1986 (Year‐0 exam) from four US communities (Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA) and followed up in seven subsequent visits up until 2011 in this analytical sample. 9 All participants provided written informed consent at each examination, and the institutional review boards of each institution approved the study in compliance with the Declaration of Helsinki.
2.1. Study design and participant selection
Out of the 3498 participants who attended the CARDIA Year‐25 exam, participants with valvular dysfunction (n = 32), implausibly high or low energy intake (n = 170) (<800 or >8000 kcal/day for men, <600 or >6000 kcal/day for women), missing dietary data or covariates (n = 561) were excluded from analysis, resulting in an analytic study sample of 2735 participants. Participants who were excluded were more likely to be black, men, and smokers, but there was no significant difference in baseline coffee or tea consumption.
2.2. Coffee, caffeine, and tea consumption assessment
The CARDIA study utilized validated interviewer‐administered dietary instruments, which have been described in prior studies. 10 , 11 Dietary history was obtained at Year‐0, Year‐7, and Year‐20. Participants were asked to report detailed food intake patterns. Daily coffee, tea, and caffeine consumption at CARDIA Year‐0, Year‐7, and Year‐20 were utilized because multiple points have been shown to be more precise estimates of intake compared with a single assessment. 10 , 11 Similar to prior CARDIA analysis, 11 daily total caffeine intake (milligrammes per day) was calculated from all caffeine containing beverages and foods reported and categorized in quintiles. A cup of coffee or tea was considered to be approximately 237 mL or 8 oz. Daily coffee consumption was categorized as <1, 1–2, 3–4, and >4 cups/day whereas tea consumption was categorized as <1, 1–2, and >2 cups/day. 11 The response rate for decaffeinated coffee was low (<25%). The CARDIA dietary history assessments also provided data on alcohol consumption, calorie intake, whole and refined grain intake, and fruit and vegetable consumption (servings/day).
2.3. Risk factor assessment
The CARDIA study risk factor assessments have been described in previous studies. 11 Briefly, three‐seated blood pressure measurements were obtained using a random zero sphygmomanometer. The average of the second and third measurements were used. Diabetes mellitus was ascertained on the basis of one or more of a combination of a history of medication use, fasting glucose ≥126 mg/dL, 2 h from a glucose tolerance test (glucose ≥200 mg/dL), or glycated haemoglobin ≥6.5. Smoking history was obtained from validated questionnaires. A physical activity score (exercise units) was obtained from the CARDIA physical activity history, a modified version of the Minnesota Leisure Time Physical Activity Questionnaire. A score of 100 exercise units is equivalent to 2 to 3 h/week of vigorous activity for 6 months of the year. High‐density lipoprotein cholesterol was quantified using enzymatic assays, and low‐density lipoprotein cholesterol was derived from the Friedewald equation.
2.4. Echocardiography protocol
Experienced sonographers using a standardized protocol across all field sites, performed an echocardiographic evaluation using an Artida cardiac ultrasound machine (Toshiba Medical Systems, Otawara, Japan). 12 Quality control and image analysis were performed at an echocardiography‐reading centre (Johns Hopkins University, Baltimore, Maryland). Traditional and tissue Doppler measurements were made from digitized images using a standard offline image analysis software system (Digisonics, Inc., Houston, Texas). Left ventricular (LV) mass (LVM), left atrial volume (LAV), and LV ejection fraction (LVEF) were obtained using recommendations from the American Society of Echocardiography. 13 LAV and LVM were indexed to body surface area were derived from tissue Doppler e´ was obtained from the average of septal and lateral annular velocities. Global longitudinal strain (GLS) was analysed on a 16‐segment basis for the LV mid‐wall layer performed offline using two‐dimensional wall motion tracking software (UltraExtend, version 2.7; Toshiba Medical Systems, Otawara, Japan). The average frame rate was 46.2 frames per second with a mean heart rate <70 beats/min. 14 A Lagrangian strain was derived from the change in regional length relative to the length at end‐diastole. 14 , 15 Global strain values were calculated as the average of segmental peak strains. More GLS values imply better systolic function. More negative e´ signifies impaired LV relaxation while a more positive transmitral Doppler early filling velocity to tissue Doppler early diastolic mitral annular velocity (E/e´) denotes worse diastolic function. The CARDIA echocardiographic examination showed good reproducibility profile. 15
2.5. Statistical analysis
Characteristics of the study participants at Year‐0, Year‐7, and Year‐20 were summarized using mean and standard deviations, and categorical variables were expressed as frequencies and percentages, as appropriate. The goals of the analysis were to assess the association between consumption of coffee, tea, total caffeine intake, and cardiac echocardiography measures. Accordingly, multivariable linear regression models using echocardiography measures as the dependent variable were used to assess associations with categories of coffee and tea intake. Covariates were derived from mean values from multiple assessments across cohort visits. Models were adjusted for age, sex, race, education, and employment status, smoking history, body mass index, systolic blood pressure, high‐density lipoprotein cholesterol, low‐density lipoprotein cholesterol, diabetes, physical activity, alcohol intake, and dietary factors (calorie intake, whole grain intake, refined grain intake, and fruit and vegetable consumption). In a secondary analysis, the relation between daily total caffeine intake (milligrammes) in quintiles and cardiac structure and function were also assessed and analysed similarly to the aforementioned regression models. There were no observed race or sex differences. Variance inflation factor was utilized to assess for potential collinearity of covariates in fully adjusted models. Analyses were performed using sas software version 9.4 (SAS Institute, Inc., NC) and stata (StataCorp, version 15; StataCorp, College Station, TX). A two‐sided P value <0.05 was considered statistically significant.
3. Results
3.1. Population characteristics
Table 1 displays the population and echocardiographic characteristics of 2735 study participants stratified by coffee consumption subgroups. Table S1 (Supporting Information) shows the distribution of clinical characteristics across cohort visits (Year‐0, Year‐7, and Year‐20). Mean age at an analytical baseline was 25.2 ± 3.5 years; 57.4% were women, and 58.4% were Caucasian. Participants who consumed >4 cups/day of coffee were more likely to be Caucasian and men. A higher proportion of participants with >4 cups/day of coffee were also current smokers (27.8%). Figure 1 shows a histogram illustrating the distribution of coffee and tea consumption in the study sample.
Table 1.
Population characteristics stratified by coffee consumption subgroups
| Coffee consumption categories | |||||
|---|---|---|---|---|---|
| Non‐coffee drinkers n = 608 | <1 coffee cup/day n = 970 | 1–2 coffee cups/day n = 532 | 3–4 coffee cups/day n = 454 | >4 coffee cups/day n = 171 | |
| Population characteristics | |||||
| Age, years (Year‐0) | 24.6 ± 3.7 | 24.8 ± 3.6 | 25.8 ± 3.3 | 26.2 ± 3.3 | 26.6 ± 2.9 |
| Women, % | 354 (58.2) | 592 (61) | 300 (56.4) | 249 (54.9) | 76 (44.4) |
| Caucasian % | 269 (42.2) | 434 (44.7) | 364 (68.4) | 369 (81.3) | 154 (90.1) |
| Current smokers, % | 71 (11.8) | 118 (12.4) | 71 (13.5) | 75 (16.7) | 47 (27.8) |
| Body mass index (kg/m2) | 31.3 ± 7.8 | 30.3 ± 7.3 | 28.9 ± 6.5 | 29.5 ± 6.6 | 29.0 ± 5.9 |
| Systolic blood pressure, (mmHg) | 120.1 ± 16.0 | 120.3 ± 16.7 | 117.3 ± 15.0 | 117.5 ± 15.2 | 119.1 ± 15.9 |
| HDL Cholesterol, (mg/dL) | 56.0 ± 17.2 | 57.5 ± 16.9 | 59.9 ± 17.7 | 60.4 ± 18.8 | 59.5 ± 21.5 |
| LDL Cholesterol, (mg/dL) | 110 ± 31.5 | 112.5 ± 33.5 | 114.1 ± 31.2 | 113.7 ± 31.6 | 110.4 ± 34.2 |
| Non‐tea drinkers | 168(27.6) | 138(14.2) | 86(16.2) | 72(15.9) | 35(20.5) |
| <1 tea cups/day | 332(54.6) | 650(67.0) | 369(69.4) | 282(62.1) | 103(60.2) |
| 1–2 tea cups/day | 62(10.2 | 114(11.8) | 51(9.6) | 68(15.0) | 17(9.9) |
| >2 tea cups/day | 46(7.6) | 68(7.0) | 26(4.9) | 32(7.1) | 16(9.4) |
| Total caffeine intake/day (mg) | 57.3 ± 68.4 | 91.6 ± 70.7 | 223.6 ± 76.9 | 418.2 ± 139.0 | 936.6 ± 531.1 |
| Echocardiography indices | |||||
| LV Mass (g) | 174.1 ± 61.4 | 167.8 ± 52.2 | 166.1 ± 50.6 | 163.3 ± 44.2 | 171.0 ± 47.8 |
| LA volume (mL) | 50.6 ± 16.4 | 50.1 ± 16.1 | 48.6 ± 15.3 | 48.5 ± 13.8 | 49.6 ± 16.0 |
| GLS (%) | −14.7 ± 2.5 | −15.1 ± 2.5 | −15.4 ± 2.3 | −15.4 ± 2.3 | −15.4 ± 2.4 |
| LVEF (%) | 61.5 ± 7.1 | 61.9 ± 7.0 | 61.8 ± 6.7 | 62.0 ± 6.7 | 59.9 ± 7.2 |
| E/e´ | 8.11 ± 2.4 | 7.8 ± 2.3 | 7.5 ± 2.2 | 7.7 ± 2.0 | 7.5 ± 2.1 |
E/e´, ratio of transmitral inflow velocity to early diastolic mitral annular velocity; g, gramme; HDL, high‐density lipoprotein; kg, kilogramme; LA, left atrial; LDL, low‐density lipoprotein; LVEF, left ventricular ejection fraction; m2, metres squared; mg, milligramme; mL, millilitres; GLS, global longitudinal strain.
Data are expressed as mean ± standard deviation or frequencies (proportion), as appropriate.
Coffee and tea consumption categories represent the mean values from three cohort visits (Year‐0, Year‐7, and Year‐20). Population characteristics are reported for the CARDIA examination Year‐25 exam except tea and coffee, which represent the mean from three cohort visits.
Figure 1.
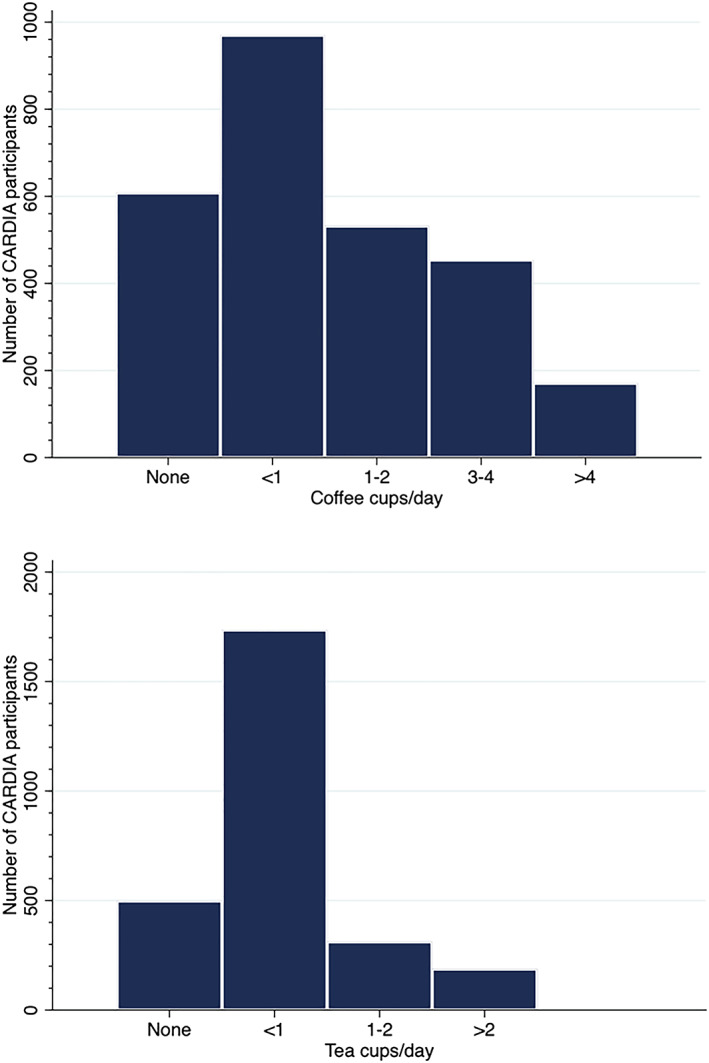
Histograms illustrating the distributions of coffee and tea consumption.
Figure 2.
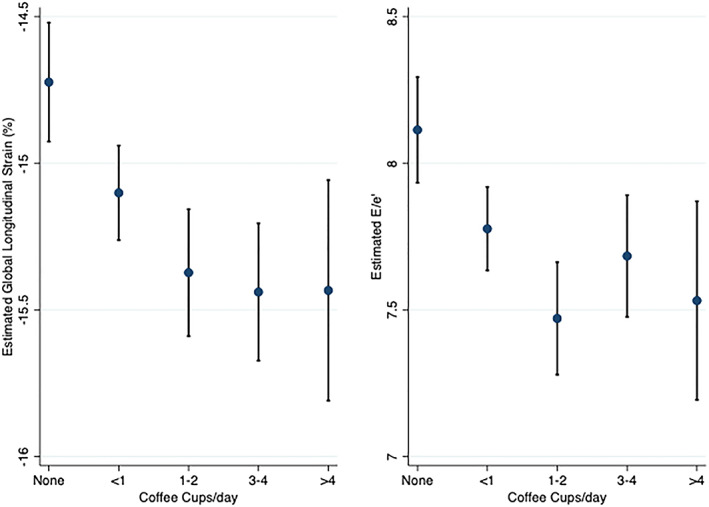
Coffee consumption from early adulthood to middle age and cardiac function in midlife. Description: Least squared means plots with 95% confidence intervals for the showing of the association between coffee consumption in cups/day and global longitudinal strain (GLS) and E/e´. Plots were derived from multivariable regression models. More negative or lower values of GLS and E/e´ signify better function. Low‐to‐moderate coffee consumption was associated with better GLS and E/e´.
3.2. Coffee, tea, caffeine consumption, and cardiac function
The association between coffee consumption and cardiac structure and function is shown in Table 2 . In adjusted multivariable linear regression models assessing the relationship between coffee consumption and GLS, beta coefficients when comparing coffee drinkers of <1, 1–2, 3–4, and >4 cups/day with non‐coffee drinkers were β = −0.30%, P < 0.05; β = −0.35%, P < 0.05; β = −0.32%, P < 0.05; and β = −0.40%, P > 0.05; respectively (more negative values implies better systolic function). In adjusted multivariable linear regression models assessing the relationship between coffee consumption and E/e´, beta coefficients when comparing coffee drinkers of <1, 1–2, 3–4, and >4 cups/day with non‐coffee drinkers were β = −0.29, P < 0.05; β = −0.38, P < 0.01; β = −0.20, P > .05; β = −0.37, P > 0.05, respectively (more negative values implies better diastolic function). High daily coffee consumption (>4 cups/day) was associated with worse LVEF β = −1.69, P < 0.05). There were no significant associations between coffee consumption and LVM or LAV. As shown in Table 3 , although tea consumption was related to lower LVM in unadjusted models, in fully adjusted models accounting for confounding by cardiovascular risk factors, particularly socioeconomic status, there was no relation between tea consumption and LVM. Tea consumption was not significantly associated with any indices of cardiac structure and function. As shown in Table S2 (Supporting Information), no evidence of an association was observed between total caffeine intake and measures of cardiac structure and function.
Table 2.
Association between coffee consumption and cardiac structure and function
| Beta estimate (standard error) | ||
|---|---|---|
| LVMi | LVMi | |
| Coffee consumption | Univariate (R 2 0.0016) | Multivariable (R 2 0.20) |
| Non‐coffee drinkers | Reference | Reference |
| <1 cup/day | −1.19(1.2) | −0.08(1.1) |
| 1–2 cups/day | −1.19(1.3) | −0.11(1.3) |
| 3–4 cups/day | −2.53(1.4) | −1.23(1.3) |
| >4 cups/day | 0.39 (2.0) | −0.57(1.9) |
| LAVi | LAVi | |
| Coffee consumption | Univariate (R 2 0.0015) | Multivariable (R 2 0.05) |
| Non‐coffee drinkers | Reference | Reference |
| <1 cup/day | 0.25 (0.4) | 0.32(0.4) |
| 1–2 cups/day | −0.31 (0.4) | −0.17(0.4) |
| 3–4 cups/day | −0.44(0.4) | −0.18(0.5) |
| >4 cups/day | −0.31(0.6) | −0.008(0.6) |
| GLS | GLS | |
| Coffee consumption | Univariate (R 2 0.012) | Multivariable (R 2 0.12) |
| Non‐coffee drinkers | Reference | Reference |
| <1 cup/day | −0.38(0.1) ** | −0.30(0.1) * |
| 1–2 cups/day | −0.65 (0.2) *** | −0.35(0.1) * |
| 3–4 cups/day | −0.72 (0.2) *** | −0.32(0.1) * |
| >4 cups/day | −0.71 (0.22) ** | −0.40(0.2) |
| LVEF | LVEF | |
| Coffee consumption | Univariate (R 2 0.005) | Multivariable (R 2 0.029) |
| Non‐coffee drinkers | Reference | Reference |
| <1 cup/day | 0.42(0.4) | 0.36(0.4) |
| 1–2 cups/day | 0.33(0.4) | 0.10(0.4) |
| 3–4 cups/day | 0.54(0.4) | 0.28(0.5) |
| >4 cups/day | −1.52(0.6)* | −1.69(0.6) * |
| E/e´ | E/e´ | |
| Coffee consumption | Univariate (R 2 0.01) | Multivariable (R 2 0.15) |
| Non‐coffee drinkers | Reference | Reference |
| <1 cup/day | −0.34(0.1) ** | −0.29(0.1) * |
| 1–2 cups/day | −0.64(0.1) *** | −0.38(0.1) ** |
| 3–4 cups/day | −0.43(0.1) ** | −0.20(0.1) |
| >4 cups/day | −0.58(0.2) ** | −0.37(0.2) |
LV, left ventricular; LVMi, LV mass indexed to body surface area; LAVi, left atrial volume indexed to body surface area; GLS, global longitudinal strain; EF, ejection fraction; E/e´, ratio of peak early diastolic velocity (E) and early peak diastolic mitral annular velocity (e')
Multivariable linear regression models showing association between coffee consumption and cardiac structure and function. Models were adjusted for age, sex, race, education, employment status, smoking, body mass index, systolic blood pressure, high‐density lipoprotein cholesterol (HDL‐C), low‐density lipoprotein cholesterol (LDL‐C), diabetes, physical activity, alcohol intake, calorie intake, whole grain intake, refined grain intake and fruit and vegetable consumption.
P < 0.05.
P < 0.01.
P < 0.001.
Table 3.
Association between tea consumption and cardiac structure and function
| Beta estimate (standard error) | ||
|---|---|---|
| LVMi | LVMi | |
| Tea consumption | Univariate (R 2 0.008) | Multivariable (R 2 0.20) |
| Non‐tea drinkers | Reference | Reference |
| <1 cup/day | −4.9(1.1) *** | −1.95(1.1) |
| 1–2 cups/day | −5.1(1.6) ** | −1.12(1.5) |
| >2cups/day | −5.4 (1.9) ** | −0.69(1.8) |
| LAVi | LAVi | |
| Tea consumption | Univariate (R 2 0.003) | Multivariable (R 2 0.05) |
| Non‐tea drinkers | Reference | Reference |
| <1 cup/day | 0.06(0.4) | 0.07 (0.37) |
| 1–2 cups/day | −0.60(0.5) | −0.48(0.5) |
| >2cups/day | −1.21(0.6) * | −1.09(0.6) |
| GLS | GLS | |
| Tea consumption | Univariate (R 2 0.0018) | Multivariable (R 2 0.12) |
| Non‐tea drinkers | Reference | Reference |
| <1 cup/day | −0.16(0.1) | 0.05(0.1) |
| 1–2 cups/day | −0.35(0.2) | 0.004(0.2) |
| >2cups/day | −0.33(0.2) | 0.05(0.2) |
| LVEF | LVEF | |
| Tea consumption | Univariate (R 2 0.0006) | Multivariable (R 2 0.024) |
| Non‐tea drinkers | Reference | Reference |
| <1 cup/day | 0.16(0.4) | −0.05(0.4) |
| 1–2 cups/day | −0.15(0.5) | −0.4 (0.5) |
| >2cups/day | 0.64(0.6) | 0.23(0.6) |
| E/e´ | E/e´ | |
| Tea consumption | Univariate (R 2 0.001) | Multivariable (R 2 0.15) |
| Non‐tea drinkers | Reference | Reference |
| <1 cup/day | −0.09(0.1) | 0.08(0.1) |
| 1–2 cups/day | −0.25(0.2) | 0.07(0.2) |
| >2cups/day | 0.04(0.2) | 0.31(0.19) |
LV, left ventricular; LVMi, LV mass indexed to body surface area; LAVi, left atrial volume indexed to body surface area; GLS, global longitudinal strain; LVEF, LV ejection fraction; E/e´, ratio of peak early diastolic velocity (E) and early peak diastolic mitral annular velocity (e´).
Multivariable linear regression models showing the association between tea consumption and cardiac structure and function. Models were adjusted for age, sex, race, education, employment status, smoking, body mass index, systolic blood pressure, high‐density lipoprotein cholesterol (HDL‐C), low‐density lipoprotein cholesterol (LDL‐C), diabetes, physical activity, alcohol intake, calorie intake, whole grain intake, refined grain intake and fruit and vegetable consumption.
P < 0.05.
P < 0.01.
P < 0.001.
4. Discussion
In this large community‐based cohort study of young adults transitioning into middle age, our main findings were that low‐to‐moderate daily coffee consumption was associated with better subclinical systolic and diastolic function. (lower LV E/e´ and better LV GLS). Conversely, we observed that a high daily coffee consumption (>4 cups/day) was associated with worse LV systolic function (lower LVEF). There were no associations between daily tea drinking or total caffeine intake and cardiac structure and function. Our study findings remained statistically significant even after robust accounting for confounding by standard cardiovascular risk factors; socioeconomic status; physical activity; alcohol use; and dietary factors (calorie intake, whole and refined grain intake, and fruit and vegetable consumption). This is the first study to demonstrate that long‐term low‐to‐moderate coffee consumption was associated with better subclinical cardiac function—an observation that may represent an underlying pathophysiological pathway for noted associations between moderate coffee consumption and HF.
Coffee consumption typically in early adulthood. In fact, by ages 18 to 24 years, one out of two individuals in the USA already consume coffee on a daily basis. 1 It is noteworthy that the CARDIA study recruited participants from age 18 to 30 years, limiting prevalent exposure bias that may occur before the onset of the study. 9
Our results are particularly relevant because early adulthood represents a crucial window to mitigate the influence of aging‐related cardiac risk factors on cardiovascular health through dietary modifications, lifestyle changes, or medical therapy.
Several lines of evidence from observational studies, but not all, support an inverse association between habitual coffee and tea consumption and clinical outcomes. 5 , 16 , 17 , 18 Studies comprising of data from predominantly European cohorts have investigated the association between coffee consumption and HF. These studies noted a U‐shaped association with reduced risk of HF in persons who drink 4 coffee cups/day, but an increased HF risk with consumption of >10 cups/day. 3 Results from these European studies are similar to ours and should be interpreted in the context that the size of a standard cup of coffee in the USA is typically about two times larger than the standard serving size in Europe. 19 Our study findings of neutral or detrimental associations with LV function among high daily coffee drinkers reinforce the importance of moderation in coffee drinking. In the current study, there was no relationship between coffee consumption and LVM. The reason for this lack of association is not clear, but it may be reasonable to theorize that coffee consumption may be closer related to LV functional rather than structural alterations in early adulthood. Because of a low response rate, we were unable to reliably assess the independent role of decaffeinated coffee. However, we observed that daily total caffeine intake (obtained from all dietary sources) was not associated with LV function. Consistent with this finding, in a prior report of 9.2 million adults, it was observed that accounting for variations in genetic polymorphisms that also influence caffeine metabolism, did not modify mortality risk with coffee consumption. 20 Taken together with our findings is highlighted. Although we noted a favourable association between tea drinking and LVM in unadjusted models, this association was not statistically significant in models that accounted for confounding factors, particularly socioeconomic status. A majority of studies accessing the benefits of tea drinking have focused on green tea consumption. We speculate that this may be partly related to the observation that black tea (which is more prevalent in western populations such as ours), contains less chemo‐protective agents when compared with green tea. 21
4.1. Potential mechanisms
Several explanatory mechanisms that may explain an association between coffee consumption and subclinical cardiac function exist. From a biological perspective, beyond caffeine, coffee contains bioactive substances such as flavonoids, diterpenes, and melanoidins that can modulate antioxidant effects, increase nitric oxide production, and superoxide free‐radicals scavenging. 22 , 23 Experimental studies suggest that flavonoids—present in coffee—modulate gene expression and signalling pathways such as enhancement and activation of 5‐monophosphate‐activated protein kinase, increased toll‐like receptor‐4 expression, increased nitrite oxidase synthase, and reduced production of reactive oxygen species. 23 Further potentiation of these chemo‐protective properties can occur when the gut interacts with a colonic microbiome and metabolic conversion to smaller more potent phenolic substances than their parent compounds occur. 24 The molecular attributes of these cellular proteins and signalling pathways influence other downstream pleiotropic effects such as decreased arterial stiffness, 25 reductions in LDL cholesterol, 26 lower insulin resistance, improved glycemic control, and a lower risk of metabolic syndrome and diabetes mellitus. 19 Although transient increases in blood pressure following short‐term administration of coffee has been noted, 27 it has not translated to a long‐term risk for hypertension. 28 It is speculated that with long‐term coffee consumption, there is a counterbalancing effect of non‐caffeine constituents that augments an increased tolerance to acute hemodynamic effects of coffee. 29
4.2. Study strengths and limitations
The clear strengths of this study included recruitment of participants in early adulthood; inclusion of a biracial cohort of community‐dwelling individuals; estimation of coffee consumption at multiple time points; comprehensive accounting for confounders such as cardiovascular disease risk factors; socioeconomic status; physical activity; dietary and calorie intake; and echocardiographic assessment in a large community‐based sample. Our study observations do not aim to infer causality. Furthermore, coffee or tea subtypes, brewing methods, and epigenetic effects were not assessed. The role of decaffeinated coffee could not be independently assessed in the present study because a low response rate, but we were able to examine total caffeine consumptions from all sources and contrast it with the consumption of any coffee subtype. Our cross‐sectional analysis did not adjust for echocardiography indicators at study enrolment. We were also unable to assess differences by the degree of fermentation during tea processing, which may play a contributory role. Long‐term observational cohort studies such as ours can be susceptible to nonresponse over time; however, the CARDIA study showed good cohort retention and followed rigorous quality control protocols. 15
5. Conclusions
Our observations in this community‐based sample underscore an association between low‐to‐moderate coffee consumption from early adulthood to middle age and favourable changes in LV systolic and diastolic function in midlife. High coffee consumption (>4 cups/day) was however associated with worse LV systolic function. There was no relation between tea or caffeine intake and cardiac function.
Conflict of interest
The authors have no conflict of interest relevant to this manuscript.
Funding
The CARDIA is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I and HHSN268201800007I), Northwestern University (HHSN268201800003I), University of Minnesota (HHSN268201800006I), and Kaiser Foundation Research Institute (HHSN268201800004I). This manuscript has been reviewed by the CARDIA study for scientific content.
CLINICAL PERSPECTIVE
Competency in Medical Knowledge
Low‐to‐moderate consumption of coffee from early adulthood to midlife was associated with better left ventricular systolic and diastolic function in middle age, which may partly underlie observations of a reduced risk of clinical HF. However, long‐term excessive coffee consumption is associated with deleterious effects on cardiac function. The present study findings highlight the importance of moderation in coffee drinking in order to reap the cardiovascular benefits and potentially avoid harm.
Translational Outlook
Additional research is needed to clarify the epigenetic and contributory factors that may modulate the dose‐dependent effects of coffee consumption on the human heart.
Supporting information
Table S1. Population characteristics of study participants (N = 2735).
Table S2. Association between total caffeine intake and cardiac structure and function.
Table S3. Characteristics of included and not included coronary artery risk development in young adults study participants at study enrollment (n = 5115).
Nwabuo, C. C. , Betoko, A. S. , Reis, J. P. , Moreira, H. T. , Vasconcellos, H. D. , Guallar, E. , Cox, C. , Sidney, S. , Ambale‐Venkatesh, B. , Lewis, C. E. , Schreiner, P. J. , Lloyd‐Jones, D. , Kiefe, C. I. , Gidding, S. S. , and Lima, J. A. C. (2020) Coffee and tea consumption in the early adult lifespan and left ventricular function in middle age: the CARDIA study. ESC Heart Failure, 7: 1510–1519. 10.1002/ehf2.12684.
References
- 1. Loftfield E, Freedman ND, Dodd KW, Vogtmann E, Xiao Q, Sinha R, Graubard BI. Coffee drinking is widespread in the United States, but usual intake varies by key demographic and lifestyle factors. J Nutr 2016; 146: 1762–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation 2019. Mar 5; 139: e56–e528. [DOI] [PubMed] [Google Scholar]
- 3. Mostofsky E, Rice MS, Levitan EB, Mittleman MA. Habitual coffee consumption and risk of heart failure: a dose‐response meta‐analysis. Circ Heart Fail 2012; 5: 401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wilhelmsen L, Rosengren A, Eriksson H, Lappas G. Heart failure in the general population of men‐‐morbidity, risk factors and prognosis. J Intern Med 2001; 249: 253–261. [DOI] [PubMed] [Google Scholar]
- 5. Ahmed HN, Levitan EB, Wolk A, Mittleman MA. Coffee consumption and risk of heart failure in men: an analysis from the cohort of Swedish Men. Am Heart J 2009; 158: 667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Peters U, Poole C, Arab L. Does tea affect cardiovascular disease? A meta‐analysis. Am J Epidemiol 2001; 154: 495–503. [DOI] [PubMed] [Google Scholar]
- 7. Zhang C, Qin YY, Wei X, Yu FF, Zhou YH, He J. Tea consumption and risk of cardiovascular outcomes and total mortality: a systematic review and meta‐analysis of prospective observational studies. Eur J Epidemiol 2015; 30: 103–113. [DOI] [PubMed] [Google Scholar]
- 8. Nwabuo CC, Armstrong AAC, Ambale‐Venkatesh B, Vasconcellos HD, Mewton N, Lima JAC, Moreira HT, Opdahl A, Lloyd‐Jones D, Ogunyankin KO, Jacobs DR Jr, Schreiner PJ, Lewis CE, Gidding SS. Left ventricular global function index predicts incident heart failure and cardiovascular disease in young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Eur Heart J Cardiovasc Imaging 2018; 20: 533–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988; 41: 1105–1116. [DOI] [PubMed] [Google Scholar]
- 10. Liu K, Slattery M, Jacobs D Jr, Cutter G, McDonald A, Van Horn L, Hilner JE, Caan B, Bragg C, Dyer A. A study of the reliability and comparative validity of the cardia dietary history. Ethn Dis 1994. Winter; 4: 15–27. [PubMed] [Google Scholar]
- 11. Reis JP, Loria CM, Steffen LM, Zhou X, van Horn L, Siscovick DS, Jacobs DR Jr, Carr JJ. Coffee, decaffeinated coffee, caffeine, and tea consumption in young adulthood and atherosclerosis later in life: the CARDIA study. Arterioscler Thromb Vasc Biol 2010; 30: 2059–2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nwabuo CC, Moreira HT, Vasconcellos HD, Ambale‐Venkatesh B, Yoneyama K, Ohyama Y, Sharma RK, Armstrong AC, Ostovaneh MR, Lewis CE, Liu K, Schreiner PJ, Ogunyankin KO, Gidding SS, Lima JAC. Association of aortic root dilation from early adulthood to middle age with cardiac structure and function: the CARDIA study. J Am Soc Echocardiogr 2017; 30: 1172–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lang RM, Badano LP, Mor‐Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015. Jan; 28: 1–39.e14. [DOI] [PubMed] [Google Scholar]
- 14. Moreira HT, Nwabuo CC, Armstrong AC, Kishi S, Gjesdal O, Reis JP, Schreiner PJ, Liu K, Lewis CE, Sidney S, Gidding SS, Lima JAC, Ambale‐Venkatesh B. Reference ranges and regional patterns of left ventricular strain and strain rate using two‐dimensional speckle‐tracking echocardiography in a healthy middle‐aged black and white population: the CARDIA study. J Am Soc Echocardiogr 2017. Jul; 30: 647–658.e642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Armstrong AC, Ricketts EP, Cox C, Adler P, Arynchyn A, Liu K, Stengel E, Sidney S, Lewis CE, Schreiner PJ, Shikany JM, Keck K, Merlo J, Gidding SS, Lima JA. Quality control and reproducibility in M‐mode, two‐dimensional, and speckle tracking echocardiography acquisition and analysis: the CARDIA study, Year 25 examination experience. Echocardiography 2015; 32: 1233–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang Y, Tuomilehto J, Jousilahti P, Antikainen R, Mahonen M, Mannisto S, Katzmarzyk PT, Hu G. Coffee consumption and the risk of heart failure in Finnish men and women. Heart 2011; 97: 44–48. [DOI] [PubMed] [Google Scholar]
- 17. Levitan EB, Ahmed HN, Mittleman MA, Wolk A. Coffee consumption and incidence of heart failure in women. Circ Heart Fail 2011; 4: 414–418. [DOI] [PubMed] [Google Scholar]
- 18. Ding M, Bhupathiraju SN, Satija A, van Dam RM, Hu FB. Long‐term coffee consumption and risk of cardiovascular disease: a systematic review and a dose‐response meta‐analysis of prospective cohort studies. Circulation 2014; 129: 643–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Dam RM, Hu FB. Coffee consumption and risk of type 2 diabetes: a systematic review. JAMA 2005; 294: 97–104. [DOI] [PubMed] [Google Scholar]
- 20. Loftfield E, Cornelis MC, Caporaso N, Yu K, Sinha R, Freedman N. Association of coffee drinking with mortality by genetic variation in caffeine metabolism: findings from the UK biobank. JAMA Intern Med 2018; 178: 1086–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ramadan G, El‐Beih NM, Abd El‐Ghffar EA. Modulatory effects of black v. green tea aqueous extract on hyperglycaemia, hyperlipidaemia and liver dysfunction in diabetic and obese rat models. Br J Nutr 2009; 102: 1611–1619. [DOI] [PubMed] [Google Scholar]
- 22. Yanagimoto K, Ochi H, Lee KG, Shibamoto T. Antioxidative activities of fractions obtained from brewed coffee. J Agric Food Chem 2004; 52: 592–596. [DOI] [PubMed] [Google Scholar]
- 23. Mozaffarian D, Wu JHY. Flavonoids, dairy foods, and cardiovascular and metabolic health: a review of emerging biologic pathways. Circ Res 2018; 122: 369–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mosele JI, Macia A, Motilva MJ. Metabolic and microbial modulation of the large intestine ecosystem by non‐absorbed diet phenolic compounds: a review. Molecules 2015; 20: 17429–17468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lin QF, Qiu CS, Wang SL, Huang LF, Chen ZY, Chen Y, Chen G. A cross‐sectional study of the relationship between habitual tea consumption and arterial stiffness. J Am Coll Nutr 2016. ‐Jun; 35: 354–361. [DOI] [PubMed] [Google Scholar]
- 26. Zhao Y, Asimi S, Wu K, Zheng J, Li D. Black tea consumption and serum cholesterol concentration: systematic review and meta‐analysis of randomized controlled trials. Clin Nutr 2015; 34: 612–619. [DOI] [PubMed] [Google Scholar]
- 27. Jee SH, He J, Whelton PK, Suh I, Klag MJ. The effect of chronic coffee drinking on blood pressure: a meta‐analysis of controlled clinical trials. Hypertension 1999; 33: 647–652. [DOI] [PubMed] [Google Scholar]
- 28. Klag MJ, Wang NY, Meoni LA, Brancati FL, Cooper LA, Liang KY, Young JH, Ford DE. Coffee intake and risk of hypertension: the Johns Hopkins precursors study. Arch Intern Med 2002; 162: 657–662. [DOI] [PubMed] [Google Scholar]
- 29. Riksen NP, Rongen GA, Smits P. Acute and long‐term cardiovascular effects of coffee: implications for coronary heart disease. Pharmacol Ther 2009; 121: 185–191. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Population characteristics of study participants (N = 2735).
Table S2. Association between total caffeine intake and cardiac structure and function.
Table S3. Characteristics of included and not included coronary artery risk development in young adults study participants at study enrollment (n = 5115).


