Abstract
Background
Major questions remain regarding the age-stratified trends of allergic diseases and asthma in Korea.
Purpose
To identify the estimated recent prevalence and 10-year trends in asthma, allergic rhinitis, and atopic dermatitis among the Korean population from 2008 to 2017.
Methods
This nationwide cross-sectional survey (Korean National Health and Nutrition Examination Survey) over 10 years (2008–2017) examined representative samples of the Korean population (n=85,006) including 2,131 infants, 4,352 preschool children, 12,919 school-age children, 44,200 adults, and 21,404 elderly adults.
Results
In the 2016 to 2017 population, the estimated prevalence of asthma was 0.9% in infants, 2.3% in preschool children, 4.1% in school-age children, 2.3% in adults, and 4.1% in the elderly. The estimated prevalence of allergic rhinitis was 9.0%, 20.2%, 27.6%, 17.1%, and 6.9%, respectively. The estimated prevalence of atopic dermatitis was 5.9%, 11.3%, 14.6%, 3.9%, and 1.6%, respectively. Ten-year trends revealed a significant decrease in asthma prevalence in infants, preschool children, and the elderly. and in atopic dermatitis prevalence in infants and preschool children (P<0.05 for all trends). Furthermore, 10-year trends demonstrated a significant increase in allergic rhinitis prevalence in school-age children, adults, and the elderly, and in atopic dermatitis prevalence in school-age children and the elderly (P<0.05 for all trends).
Conclusion
These results improve our understanding of the age-stratified epidemiology of allergic diseases in Korea and suggest the need for the development of tailored and precise strategies to prevent allergic diseases in different age groups.
Keywords: Asthma; Allergic rhinitis; Atopic dermatitis; Korea, Prevalence
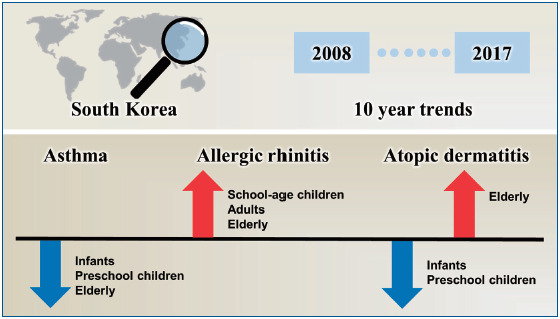
Graphical abstract. Prevalence of asthma, allergic rhinitis, and atopic dermatitis.
Introduction
In recent decades, the prevalence of allergic diseases such as asthma have dramatically increased worldwide, particularly in low and middle income countries [1]. In particular, vulnerable children and young adults bear the burden of global trends in allergic diseases [1,2]. However, the evidence supporting such trends in asthma, allergic rhinitis, and atopic dermatitis in Korea is controversial, as previous studies have reported both increasing [3-6] and decreasing prevalence [2,7-9]. Furthermore, major questions remain regarding the age-stratified trends in allergic diseases and asthma in Korean populations [10].
To address these questions, we investigated the estimated age-stratified prevalence and 10-year trends in 3 allergic diseases (asthma, allergic rhinitis, and atopic dermatitis), using data collected from the Korean National Health and Nutrition Examination Survey (KNHANES) from 2008 to 2017.
Methods
KNHANES is a series of stratified, multistage probability series of surveys conducted by the Korea Centers for Disease Control and Prevention (KCDC), designed to be a nationally representative health information survey of the Korean population. KNHANES sampling procedures were performed to account for sample weights (primary sample unit, household, and person), stratification, and clustering to provide nationally representative estimates [11]. Moreover, every year population sample represents the total Korean civilian population [12]. The survey included a health interview and a physical examination.
The study protocol was approved by the Institutional Review Board of the KCDC (2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C, 2013-07CON-03-4C, 2013-12EXP-03-5C, 2015-01-02-6C), and written informed consent was provided by all participants.
We used data obtained from the KNHANES from 2008 to 2017 to estimate the prevalence and 10-year trends in the following allergic diseases: asthma, allergic rhinitis, and atopic dermatitis. From 2008 to 2017, a total of 85,006 subjects (2,131 infants, younger than 2 years; 4,352 preschool children, 2 to 5 years; 12,919 school-age children, 6 to 18 years; 44,200 adults, 19 to 59 years; and 21,404 elderly adults, 60 years or more) participated in the surveys [13].
The presence of asthma, allergic rhinitis, and atopic dermatitis were defined by affirmative answers to the following question [12,14]: “Have you ever been diagnosed with asthma/allergic rhinitis/atopic dermatitis by a doctor?” The region of residence for each subject was grouped as follows: rural (Gangwon, Chungbuk, Chungnam, Jeonbuk, Jeonnam, Gyeongbuk, Gyeong nam, and Jeju) and urban (Seoul, Gyeonggi, Busan, Daegu, Incheon, Gwang ju, Daejeon, Ulsan, and Sejong) [12]. Body mass index was cal culated in kilograms per square meter and categorized as: normal (children, less than 85 percentile; adults, less than 25 kg/m2) and obese (children, more than 85 percentile; adults, more than 25 kg/m2) according to age- and sex-specific equations based on the 2007 Korean national growth charts [15,16].
We used data obtained from the KNHANES from 2008 to 2017 to calculate the total allergic disease prevalence (asthma, allergic rhinitis, and atopic dermatitis), stratified by age group (infants, preschool children, school-age children, adults, and the elderly). Data were analyzed using weighted complex sampling analysis, using the chi-square test and binomial or linear logistic regression, and presented as odds ratios (ORs) with 95% confidence intervals (CIs), or β-coefficients with 95% CIs. These analyses were performed using IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA) [17]. The estimated β (95% CI) and P for the trends (linear trend) were calculated using linear regression and the estimated OR (95% CI) and P value (quadratic trend) were considered using binomial regression.
This analysis included the KNHANES cycle (2008 to 2009, 2010 to 2012, 2013 to 2015, and 2016 to 2017) as a continuous variable. The estimated ORs (95% CI) and P values were calculated using binomial regression and this analysis included the KNHANES cycle (2016 to 2017 vs. first cycle). A P value below 0.05 was considered statistically significant.
Results
From 2008 to 2017, a total of 85,006 subjects (2,131 infants, younger than 2 years; 4,352 preschool children, 2 to 5 years; 12,919 school-age children, 6 to 18 years; 44,200 adults, 19 to 59 years; and 21,404 elderly adults, 60 years or more) participated in the KNHANES surveys. Table 1 presents the general characteristics of the study populations.
Table 1.
Sample size of Korean pediatric population, KNHANES, 2008–2017
| Variable | No. of participants by age groups |
||||
|---|---|---|---|---|---|
| Infants (>2 yr) | Preschool children (2–5 yr) | School-age children (6–18 yr) | Adults (19–59 yr) | Elderly (≥60 yr) | |
| Number (weighted %) | 2,131 (100) | 4,352 (100) | 12,919 (100) | 44,200 (100) | 21,404 (100) |
| Sex | |||||
| Male | 51.1 (48.7–53.4) | 52.6 (50.9–54.4) | 52.6 (51.6–53.7) | 43.6 (42.9–44.2) | 43.6 (42.9–44.2) |
| Female | 48.9 (46.6–51.3) | 47.4 (45.6–49.1) | 47.4 (46.3–48.4) | 48.9 (48.4–49.3) | 56.4 (55.8–57.1) |
| Body mass indexa) | |||||
| Normal | 79.5 (76.0–82.6) | 87.0 (85.3–88.6) | 80.5 (79.6–81.5) | 68.1 (67.5–68.6) | 64.1 (63.3–65.0) |
| Overweight and obese | 20.5 (17.4–20.4) | 13.0 (11.4–14.7) | 19.5 (18.5–20.4) | 31.9 (31.4–32.5) | 35.9 (35.0–36.7) |
| Region of residence | |||||
| Rural | 67.8 (64.7–70.7) | 63.9 (61.2–66.4) | 66.1 (64.2–68.0) | 67.5 (66.2–68.8) | 57.1 (57.1–60.2) |
| Urban | 32.2 (29.3–35.3) | 36.1 (33.6–38.8) | 33.9 (32.0–35.8) | 32.5 (31.2–33.8) | 41.4 (39.8–42.9) |
| Economic level | |||||
| Highest | 22.6 (20.5–24.8) | 24.9 (23.1–26.8) | 29.2 (27.6–30.8) | 33.9 (32.9–34.9) | 13.4 (12.5–14.3) |
| Middle high | 35.3 (32.9–37.7) | 35.9 (34.0–37.9) | 31.9 (30.6–33.2) | 32.3 (31.5–33.1) | 17.3 (16.5–18.1) |
| Middle low | 34.7 (32.3–37.3) | 31.3 (29.3–33.3) | 26.7 (25.4–28.1) | 24.6 (23.9–25.4) | 27.2 (26.3–28.2) |
| Lowest | 7.4 (6.1–8.8) | 7.9 (6.8–9.1) | 12.2 (11.2–13.3) | 9.2 (8.7–9.7) | 42.1 (40.9–43.3) |
Values are presented as weighted % (95% confidence interval).
KNHANES, Korean National Health and Nutrition Examination Survey.
Overweight and obese was defined as a body mass index more than 25 kg/m2 for adults and more than 85th percentile for children. Normal was defined as a body mass index less than 25 kg/m2 for adults and less than 85th percentile for children.
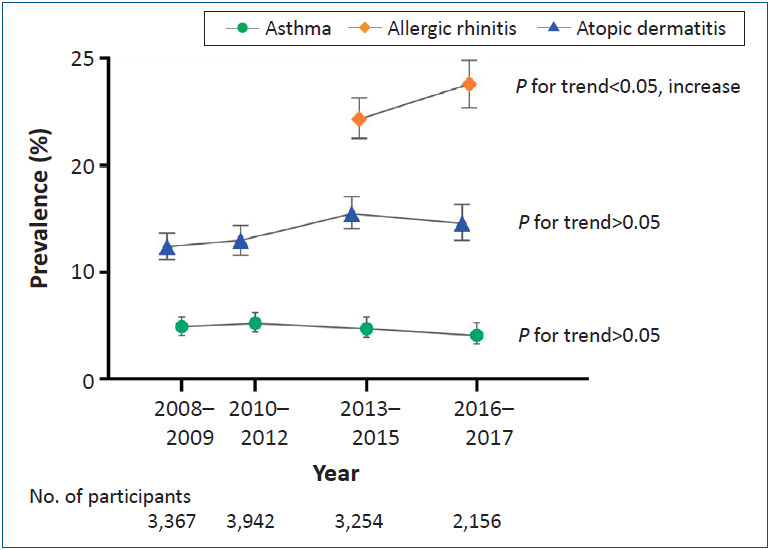
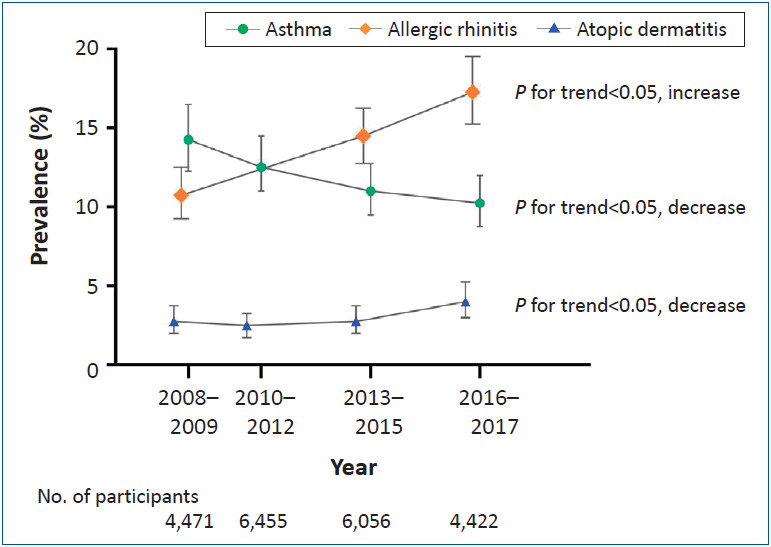
Table 2 illustrates the weighted crude prevalence and overall trend in allergic diseases (asthma, allergic rhinitis, and atopic dermatitis) in the Korean general pediatric population from 2008 to 2017. In infants, the estimated prevalence of asthma, allergic rhinitis, and atopic dermatitis from 2016 to 2017 were 0.9% (95% CI, 0.3%–2.5%), 9.0% (6.4% and 12.6%), and 5.9% (3.8%–9.0%), respectively. The 10-year trends in asthma and atopic dermatitis demonstrated a significant decrease in both linear trend (P for trend=0.009 and P<0.001, respectively) and quadratic trend (P=0.014 and P<0.001, respectively) (Fig. 1). In preschool children, the estimated prevalence of asthma, allergic rhinitis, and atopic dermatitis from 2016 to 2017 were 2.3% (1.3%–3.9%), 20.2% (17.1%–23.7%), and 11.3% (8.6%–14.6%), respectively. The 10-year trends in asthma and atopic dermatitis showed a significant decrease in linear trend (P<0.001 for all trends) and quadratic trend (P=0.009 and P<0.001, respectively) (Fig. 2). Moreover, in school-age children, the estimated prevalence of asthma, allergic rhinitis, and atopic dermatitis from 2016 to 2017 were 4.1% (3.3%–5.3%), 27.6% (25.4%–29.8%), and 14.6% (13.0%–16.4%), respectively. The 10-year trends in allergic rhinitis and atopic dermatitis demonstrated a significant increase in linear trend (P=0.029 and P=0.003, respectively) and quadratic trend (P=0.036 and P=0.028, respectively) (Fig. 3). In adults, the estimated prevalence of asthma, allergic rhinitis, and atopic dermatitis from 2016 to 2017 were 2.3% (1.9%–2.7%), 17.1% (16.2% and 18.1%), and 3.9% (3.4% and 4.4%), respectively. The 10-year trends in allergic rhinitis showed a significant increase in linear and quadratic trends (P<0.001 for all trends) (Fig. 4). In the elderly, the estimated prevalence of asthma, allergic rhinitis, and atopic dermatitis from 2016 to 2017 were 4.1% (3.5%–4.8%), 6.9% (6.1%–7.8%), and 1.6% (1.2%–2.1%), respectively. The 10year trends among the elderly revealed a significant decrease in asthma in both linear and quadratic trends (P<0.001 and P=0.002, respectively). Furthermore, there was an increase in allergic rhinitis in linear and quadratic trends (all P value<0.001) (Fig. 5).
Table 2.
Weighted crude prevalence of and trend in allergic diseases (asthma, allergic rhinitis, and atopic dermatitis) in the Korean general pediatric population, KNHANES, 2008–2017
| Age group | Trends in allergic diseases |
β (95% CI)a) | P for trend | 2016 to 2017 vs. first cycle, OR (95% CI)b) | P value | |||
|---|---|---|---|---|---|---|---|---|
| 2008 to 2009 | 2010 to 2012 | 2013 to 2015 | 2016 to 2017 | |||||
| Asthma | ||||||||
| Infants | 3.7 (2.3–5.9) | 2.1 (1.0–4.4) | 1.6 (0.8–3.3) | 0.9 (0.3–2.5) | -0.009 (-0.015 to -0.002) | 0.009 | 0.244 (0.079–0.749) | 0.014 |
| Preschool children | 5.1 (3.9–6.6) | 7.5 (5.8–9.7) | 4.1 (3.0–5.6) | 2.3 (1.3–3.9) | -0.013 (-0.019 to -0.006) | <0.001 | 0.433 (0.231–0.812) | 0.009 |
| School-age children | 4.9 (4.1–5.8) | 5.2 (4.4–6.2) | 4.7 (3.9–5.8) | 4.1 (3.3–5.3) | -0.003 (-0.007 to 0.001) | 0.203 | 0.840 (0.619–1.141) | 0.264 |
| Adults | 2.2 (1.9–2.5) | 2.5 (2.1–2.9) | 2.4 (2.1–2.8) | 2.3 (1.9–2.7) | 0.000 (-0.001 to 0.002) | 0.787 | 1.059 (0.842–1.331) | 0.624 |
| Elderly | 5.7 (4.9–6.6) | 5.0 (4.4–5.8) | 4.4 (3.8–5.1) | 4.1 (3.5–4.8) | -0.005 (-0.009 to -0.002) | <0.001 | 0.707 (0.565–0.883) | 0.002 |
| Allergic rhinitis | ||||||||
| Infants | - | - | 6.9 (4.9–9.6) | 9.0 (6.4–12.6) | 0.021 (-0.017 to 0.060) | 0.282 | 1.337 (0.794–2.249) | 0.274 |
| Preschool children | - | - | 19.7 (17.0–22.6) | 20.2 (17.1–23.7) | 0.005 (-0.038 to 0.049) | 0.806 | 1.034 (0.790–1.355) | 0.806 |
| School-age children | - | - | 24.3 (22.5–26.3) | 27.6 (25.4–29.8) | 0.033 (0.003–0.062) | 0.029 | 1.185 (1.018–1.379) | 0.028 |
| Adults | 13.5 (12.7–14.3) | - | 16.0 (15.2–16.8) | 17.1 (16.2–18.1) | 0.012 (0.008–0.016) | <0.001 | 1.320 (1.200–1.452) | <0.001 |
| Elderly | 4.3 (3.7–5.0) | - | 5.8 (5.1–6.5) | 6.9 (6.1–7.8) | 0.009 (0.005–0.012) | <0.001 | 1.655 (1.339–2.046) | <0.001 |
| Atopic dermatitis | ||||||||
| Infants | 14.1 (11.4–17.2) | 9.2 (7.1–11.9) | 9.3 (6.9–12.3) | 5.9 (3.8–9.0) | -0.230 (-0.035 to -0.011) | <0.001 | 0.383 (0.230–0.638) | <0.001 |
| Preschool children | 19.7 (17.1–22.5) | 15.7 (13.1–18.8) | 16.7 (14.3–19.5) | 11.3 (8.6–14.6) | -0.023 (-0.036 to -0.010) | <0.001 | 0.519 (0.369–0.730) | <0.001 |
| School-age children | 12.4 (11.2–13.7) | 13.0 (11.6–14.4) | 15.5 (14.1–17.1) | 14.6 (13.0–16.4) | 0.010 (0.004–0.017) | 0.003 | 1.210 (1.013–1.445) | 0.036 |
| Adults | 3.3 (2.9–3.7) | 3.5 (3.0–4.0) | 3.5 (3.1–3.9) | 3.9 (3.4–4.4) | 0.002 (0.000–0.004) | 0.125 | 1.183 (0.975–1.434) | 0.088 |
| Elderly | 1.1 (0.8–1.5) | 1.0 (0.7–1.3) | 1.1 (0.8–1.5) | 1.6 (1.2–2.1) | 0.002 (0.000–0.004) | 0.048 | 1.463 (0.954–2.243) | 0.081 |
Values are presented as weighted % (95% confidence interval).
Boldface indicates a statistically significant difference with P<0.05.
KNHANES, Korean National Health and Nutrition Examination Survey; OR, odds ratio.
The estimated β (95% CI) and P for trend were calculated using linear regression and this analysis included the KNHANES cycle (2008 to 2009, 2010 to 2012, 2013 to 2015, and 2016 to 2017) as a continuous variable.
The estimated OR (95% CI) and P value were calculated using binomial regression and this analysis included the KNHANES cycle (2016 to 2017 vs. first cycle) as a categorical variable.
Fig. 1.
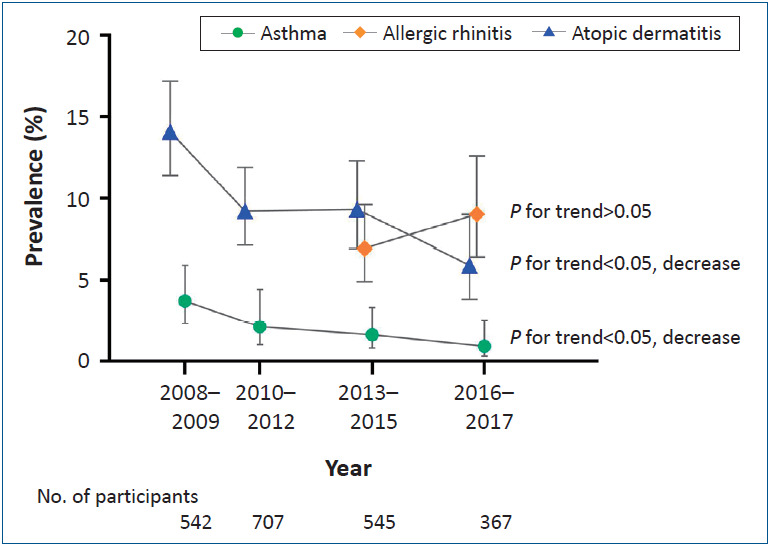
Ten-year trends of asthma, allergic rhinitis, and atopic dermatitis among the Korean infants (<2 years), Korean National Health and Nutrition Examination Survey (KNHANES), 2008–2017.
Fig. 2.
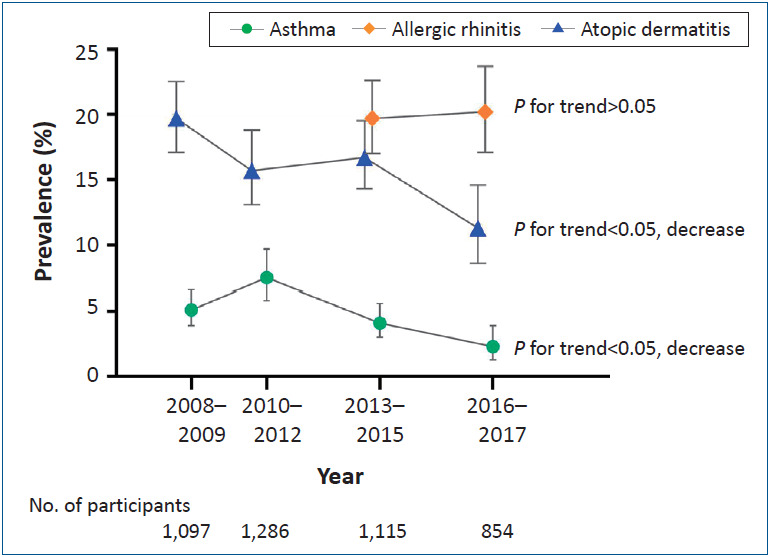
Ten-year trends of asthma, allergic rhinitis, and atopic dermatitis among the Korean preschool children (2–5 years), Korean National Health and Nutrition Examination Survey (KNHANES), 2008–2017.
Fig. 3.
age children (6–18 years), Korean National Health and Nutrition Examination Survey (KNHANES), 2008–2017.
Fig. 4.
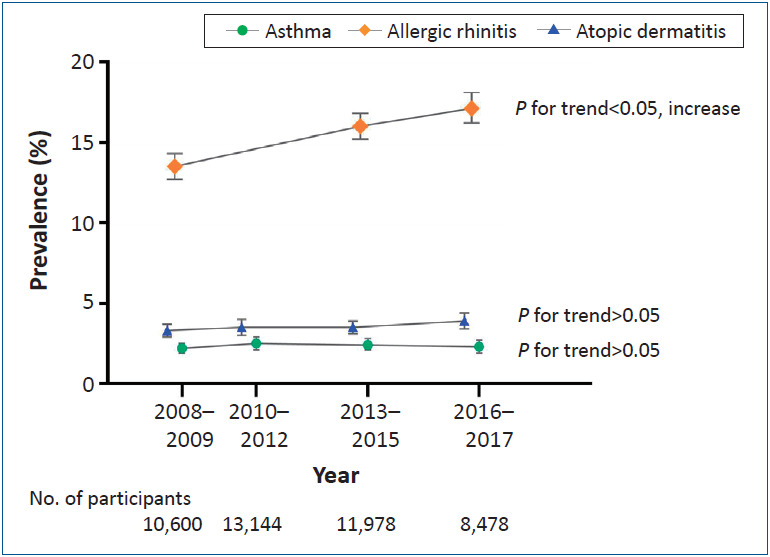
Ten-year trends of asthma, allergic rhinitis, and atopic dermatitis among the Korean Adults (19–59 years), Korean National Health and Nutrition Examination Survey (KNHANES), 2008–2017.
Fig. 5.
Ten-year trends of asthma, allergic rhinitis, and atopic dermatitis among the Korean elderly (≥60 years), Korean National Health and Nutrition Examination Survey (KNHANES), 2008–2017.
Discussion
In this nationally representative sample of the Korean population, which included children and adults, the estimated 10-year trends in asthma remained low and stable from 2008 through to 2017. Meanwhile, the estimated 10-year trends in allergic rhinitis either significantly increased or remained stable from 2008 to 2017. Although the estimated 10-year trends in atopic dermatitis in infants and preschool children significantly decreased, the trends in school-age children and the elderly significantly increased from 2008 to 2017.
We found the estimated recent prevalence of allergic diseases from 2016 to 2017 were 0.9% (asthma, infants), 2.3% (asthma, preschool-age children), 4.1% (asthma, school-age children), 2.3% (asthma, adults), 4.1% (asthma, elderly), 9.0% (allergic rhinitis; infants), 20.2% (allergic rhinitis, preschool-age children), 27.6% (allergic rhinitis, school-age children), 17.1% (allergic rhinitis, adults), 6.9% (allergic rhinitis, elderly), 5.9% (atopic dermatitis; infants), 11.3% (atopic dermatitis, preschool-age children), 14.6% (atopic dermatitis, school-age children), 3.9% (atopic dermatitis, adults), and 1.6% (atopic dermatitis, elderly).
The main strengths of our study were the large sample size, the representative data of the Korean population, and the comprehensive investigation of the age-stratified, 10-year trends of all allergic diseases. However, our study also had several limitations. First, the presence of allergic diseases could cause a recall bias in parents of children. Second, although the diagnostic tool and criteria changed over time, we included under-diagnosed or over-diagnosed allergic diseases. As a result, we considered a consistent definition of allergic diseases across the entirety of KNHANES, and hence, we were unable to investigate data of allergic rhinitis in 2008 to 2012 among the pediatric population. Finally, because we used only questionnaire-based definition of allergic diseases, we may have unintentionally included some infants and children who had acute bronchiolitis, seborrheic dermatitis and/or respiratory infection and some elderly who had chronic obstructive pulmonary disease and/or other chronic diseases.
1. Why do estimated 10-year trends in asthma tend to decrease in younger children and the elderly?
Previous studies reported that the prevalence of asthma in children and the elderly peaked in 2011 and decreased thereafter [2], this result was consistent with our result. First, since 2010, the Korean government and local governments have attempted to control childhood allergic diseases and have promoted research on exposure to outdoor and indoor environmental factors on allergic symptoms, and such efforts may have reduced the prevalence of asthma [7]. Moreover, asthma education is sufficiently provided over time by well-trained physicians [18]. Second, an influenza pandemic wave in 2009 to 2010 and a Mycoplasma pneumoniae pandemic wave in 2011 may be attributed to an increased risk of asthma, especially in vulnerable younger children and the elderly [19,20]. Third, Koreans continue to experience inhalation hazards from humidifier disinfectants [21]. A previous study indicated that approximately 30% of Korean children were exposed to a humidifier disinfectant from 1994 to 2011, and these products withdrawn from the market in 2011 [22]. Inhalation of a humidifier disinfectant typically leads to inflammation and fibrosis of the entire lungs, and a previous study indicated a relationship between humidifier disinfectant usage and asthma [22]. Inhalation of a humidifier disinfectant may lead to an increased risk of asthma and atopic dermatitis in vulnerable young children.
2. Why does the estimated prevalence of allergic rhinitis tend to increase in school-age children, and adults?
Previous studies have reported that the worldwide prevalence of allergic rhinitis has increased and affects 10% to 40% of adults and 2% to 25% of children [23]. Moreover, rapid economic development with Westernized lifestyles and urbanization is associated with an increasing trend in allergic rhinitis [24]. Further more, a previous study reported that various outdoor environmen tal factors (i.e., air pollution, weather condition, aero allergen, and respiratory virus infection) and endocrine disrup tion chemicals (i.e., phthalate, paraben, and triclosan) may have affected the prevalence of allergic rhinitis [13,25,26]. The signifi cant increase in allergic rhinitis prevalence requires the establish ment of a global strategy of effective prevention and treatment [24].
3. Why does the estimated prevalence of atopic dermatitis tend to decrease in infants and preschool children and increase in school-age children and the elderly?
The prevalence of atopic dermatitis in children and young adults has recently decreased in several studies [5,23], and the cause of the divergent trends could not explain about the hygiene hypothesis and/or allergic epidemic (outdoor allergen levels, diet change, vaccination, smoking, and pet exposure) [5,23,27]. Therefore, the age-dependent divergent trends of atopic dermatitis would be more explainable by environmental and social change [5,23,27].
In conclusion, between 2008 to 2009 and 2016 to 2017, the 10-years trends in asthma prevalence remained low and stable in the Korean population. Meanwhile, the 10-year trends in allergic rhinitis remained high in the Korean population. Although the 10-year trends in atopic dermatitis among infants and preschool children significantly decreased, those in school-age children and the elderly significantly increased from 2008 to 2017. These results provide an improved understanding of the age-stratified epidemiology of allergic diseases in Korea, and suggest the need for the development of tailored and precise strategies to prevent allergic diseases in different age groups.
Key message
Question: What were 10-year trends of asthma, allergic rhinitis, and atopic dermatitis among the Korean population from 2008 through 2017?
Finding: In this serial cross-sectional study that included 85,006 subjects, 10-year trends in asthma remained low and stable, meanwhile, 10-year trends in allergic rhinitis significantly increased or remained stable.
Meaning: These results suggest a need for the development of tailored strategies to prevent allergic diseases in different age groups.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Pawankar R. Allergic diseases and asthma: a global public health concern and a call to action. World Allergy Organ J. 2014;7:12. doi: 10.1186/1939-4551-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kang SY, Song WJ, Cho SH, Chang YS. Time trends of the prevalence of allergic diseases in Korea: A systematic literature review. Asia Pac Allergy. 2018;8:e8. doi: 10.5415/apallergy.2018.8.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sol IS, Kim YH, Kim SY, Choi SH, Kim JD, Kim BO, et al. Prescription patterns and burden of pediatric asthma in Korea. Allergy Asthma Immunol Res. 2019;11:280–90. doi: 10.4168/aair.2019.11.2.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song WJ, Wong GWK. Changing trends and challenges in the management of asthma in Asia. J Allergy Clin Immunol. 2017;140:1272–4. doi: 10.1016/j.jaci.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Kim BK, Kim JY, Kang MK, Yang MS, Park HW, Min KU, et al. Allergies are still on the rise? A 6-year nationwide population-based study in Korea. Allergol Int. 2016;65:186–91. doi: 10.1016/j.alit.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Yoo B, Park Y, Park K, Kim H. A 9-year Trend in the prevalence of allergic disease based on National Health Insurance Data. J Prev Med Public Health. 2015;48:301–9. doi: 10.3961/jpmph.15.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho YM, Kim CB, Yeon KN, Lee ES, Kim K. Trends in the prevalence of childhood asthma in Seoul Metropolitan City, Korea: The Seoul Atopy ∙ Asthma-friendly School Project. J Prev Med Public Health. 2018;51:275–80. doi: 10.3961/jpmph.18.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee JY, Yang HK, Kim M, Kim J, Ahn K. Is the prevalence of atopic dermatitis in Korean children decreasing? : National Database 2009-2014. Asian Pac J Allergy Immunol. 2017;35:144–9. doi: 10.12932/AP0797. [DOI] [PubMed] [Google Scholar]
- 9.Hong S, Son DK, Lim WR, Kim SH, Kim H, Yum HY, et al. The prevalence of atopic dermatitis, asthma, and allergic rhinitis and the comorbidity of allergic diseases in children. Environ Health Toxicol. 2012;27:e2012006. doi: 10.5620/eht.2012.27.e2012006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anandan C, Nurmatov U, van Schayck OC, Sheikh A. Is the prevalence of asthma declining? Systematic review of epidemiological studies. Allergy. 2010;65:152–67. doi: 10.1111/j.1398-9995.2009.02244.x. [DOI] [PubMed] [Google Scholar]
- 11.Kim Y. The Korea National Health and Nutrition Examination Survey (KNHANES): current status and challenges. Epidemiol Health. 2014;36:e2014002. doi: 10.4178/epih/e2014002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koh HY, Kim TH, Sheen YH, Lee SW, An J, Kim MA, et al. Serum heavy metal levels are associated with asthma, allergic rhinitis, atopic dermatitis, allergic multimorbidity, and airflow obstruction. J Allergy Clin Immunol Pract. 2019;7:2912–5. doi: 10.1016/j.jaip.2019.05.015. [DOI] [PubMed] [Google Scholar]
- 13.Lee SW, Yon DK, James CC, Lee S, Koh HY, Sheen YH, et al. Short-term effects of multiple outdoor environmental factors on risk of asthma exacerbations: Age-stratified time-series analysis. J Allergy Clin Immunol. 2019;144:1542–50. doi: 10.1016/j.jaci.2019.08.037. [DOI] [PubMed] [Google Scholar]
- 14.Noh H, An J, Kim MJ, Sheen YH, Yoon J, Welsh B, et al. Sleep problems increase school accidents related to allergic diseases. Pediatr Allergy Immunol. 2020;31:98–103. doi: 10.1111/pai.13132. [DOI] [PubMed] [Google Scholar]
- 15.Yon DK, Lee SW, Ha EK, Lee KS, Jung YH, Jee HM, et al. Serum lipid levels are associated with allergic rhinitis, nasal symptoms, peripheral olfactory function, and nasal airway patency in children. Allergy. 2018;73:1905–8. doi: 10.1111/all.13484. [DOI] [PubMed] [Google Scholar]
- 16.Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, et al. 2007 Korean National Growth Charts: review of developmental process and an outlook. Korean J Pediatr. 2008;51:1–25. [Google Scholar]
- 17.Yon DK, Hwang S, Lee SW, Jee HM, Sheen YH, Kim JH, et al. Indoor exposure and sensitization to formaldehyde among inner-city children with increased risk for asthma and rhinitis. Am J Respir Crit Care Med. 2019;200:388–93. doi: 10.1164/rccm.201810-1980LE. [DOI] [PubMed] [Google Scholar]
- 18.Boulet LP. Asthma education: an essential component in asthma management. Eur Respir J. 2015;46:1262–4. doi: 10.1183/13993003.01303-2015. [DOI] [PubMed] [Google Scholar]
- 19.Park M, Wu P, Goldstein E, Joo Kim W, Cowling BJ. Influenza-associated excess mortality in South Korea. Am J Prev Med. 2016;50:e111–e119. doi: 10.1016/j.amepre.2015.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang HJ, Song DJ, Shim JY. Mechanism of resistance acquisition and treatment of macrolide-resistant Mycoplasma pneumoniae pneumonia in children. Korean J Pediatr. 2017;60:167–74. doi: 10.3345/kjp.2017.60.6.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoon J, Cho HJ, Lee E, Choi YJ, Kim YH, Lee JL, et al. Rate of humidifier and humidifier disinfectant usage in Korean children: a nationwide epidemiologic study. Environ Res. 2017;155:60–3. doi: 10.1016/j.envres.2017.01.030. [DOI] [PubMed] [Google Scholar]
- 22.Yoon J, Lee SY, Lee SH, Kim EM, Jung S, Cho HJ, et al. Exposure to humidifier disinfectants increases the risk of asthma in children. Am J Respir Crit Care Med. 2018;10 doi: 10.1164/rccm.201805-0840LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–43. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Zhang L. Increasing prevalence of allergic rhinitis in China. Allergy Asthma Immunol Res. 2019;11:156–69. doi: 10.4168/aair.2019.11.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yon DK, Cho YS, Ha EK, Jee HM, Song JY, Jung YH, Lee KS, et al. Exposure to phthalates is associated with acute urticaria in children. Pediatr Allergy Immunol. 2018;29:657–60. doi: 10.1111/pai.12932. [DOI] [PubMed] [Google Scholar]
- 26.D'Amato G, Vitale C, Rosario N, Neto HJC, Chong-Silva DC, Mendonça F, et al. Climate change, allergy and asthma, and the role of tropical forests. World Allergy Organ J. 2017;10:11. doi: 10.1186/s40413-017-0142-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams H, Stewart A, von Mutius E, Cookson W, Anderso GrHRoups, International Study of Asthma and Allergies in Childhood (ISAAC) Phase One and Three Study Groups Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008;121:947–54. doi: 10.1016/j.jaci.2007.11.004. [DOI] [PubMed] [Google Scholar]