Abstract
Background
There is limited research examining the association between child maltreatment and cigarette smoking as a specific type of adolescent substance use, and research examining high-risk samples and variations based on maltreatment type and timing remain sparse.
Objectives
The primary aim of the study was to examine the relationship between child maltreatment and cigarette smoking trajectories.
Methods
Latent class growth analysis and multinomial logistic regression were performed on 903 youth drawn from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN).
Results
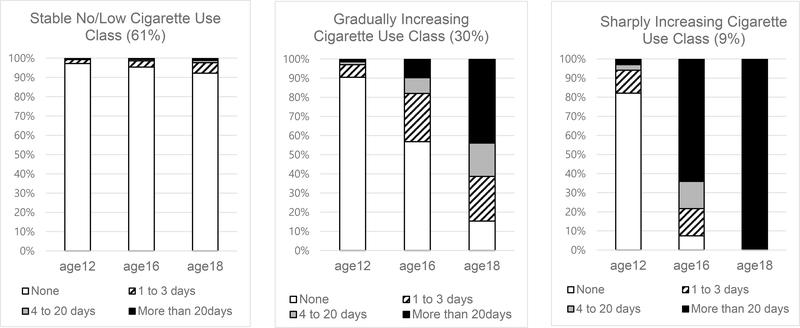
Three distinct classes of cigarette smoking trajectories were identified: 1) Stable no/low cigarette use (61%); 2) Gradually increasing cigarette use (30%); and 3) Sharply increasing cigarette use (9%). Physical abuse during early childhood and adolescence predicted membership in the sharply increasing cigarette use class. Neglect during early childhood predicted membership in the gradually increasing cigarette use class.
Conclusions
Findings suggest that interventions for adolescent cigarette smoking should integrate trauma-informed approaches. Further, the results highlight early childhood and adolescence as particularly vulnerable periods with respect to the influence of physical abuse and neglect on cigarette smoking, pointing to the need for additional maltreatment prevention efforts during these developmental stages.
Keywords: child maltreatment, cigarette smoking, adolescence, longitudinal
Child maltreatment refers to any acts by parents or caregivers that can lead to serious harm or the treat of harm to children 0–18 years of age (USDHHS, 2019). Child maltreatment – including physical abuse, sexual abuse, emotional abuse, and neglect – has been consistently identified by research as a risk factor for adolescent risk taking behavior, including substance use (Cicchetti & Handley, 2019; Duprey, Oshri, & Caughy, 2017; Thompson et al., 2017). Some studies have specifically highlighted the link between child maltreatment and cigarette smoking, (Hussey, Chang, & Kotch, 2006; Lewis et al., 2011, 2019; Kristman-Valente, Brown, & Herrenkohl, 2013; Moran, Vuchinich, & Hall, 2004; Tonmyr, Thornton, Draca, & Wekerle, 2010). Individuals with a history of maltreatment are also more likely to engage in cigarette smoking that persists into adulthood, and have demonstrated greater difficulty quitting cigarette use (Elliott et al., 2014; Taha, Galea, Hien, & Goodwin, 2014). Accordingly, these individuals will disproportionally experience myriad negative physical health outcomes to which cigarette smoking contributes (e.g., cardiovascular disease, diabetes, poor lung functioning, etc.; Afifi, Mota, MacMillan, & Sareen, 2013; Widom, Czaja, Bentley & Johnson, 2012). Most health impacts caused by smoking can be halted if smokers cease use by their early 30s (U.S. DHHS, 2012). To reduce disease burden among the most vulnerable, adolescence and young adulthood are critical times to intervene, especially among high-risk populations (Husten, 2007). However, how the type and timing of child maltreatment experiences may be associated with trajectories of cigarette smoking across this developmental period remains poorly understood.
Adolescent Cigarette Smoking
Adolescent cigarette smoking is a grave public health concern in the United States. In 2017, past 30-day use was 1.9% among 8th graders, 5.0% among 10th graders, and 9.7% among 12th graders (Miech et al., 2017). The overwhelming majority of people who smoke cigarettes throughout adulthood begin in adolescence prior to the age of 18, and those who begin earlier in adolescence are more likely to develop dependence on nicotine and have greater difficulties quitting later in life (Lydon, Wilson, Child, & Geier, 2014; Walker & Loprinzi, 2014). The regions of the brain responsible for reward reinforcement are permanently altered in the brains of adolescents exposed to nicotine (Lydon et al., 2014; Smith, McDonald, Bergstrom, Ehlinger, & Brielmaier, 2015). Therefore, adolescents who smoke are not only more likely to continue smoking into adulthood, their developing brains are predisposed to other substance use disorders (Cavazos-Rehg, Krauss, Spitznagel, Grucza, & Bierut, 2014). Adolescent cigarette smoking is also related to various problems with the respiratory system, including reduced lung function and weakened respiratory muscle strength (Tantisuwat & Thaveeratitham, 2014), as well as cardiovascular disease (Hackshaw, Morris, Boniface, Tang & Milenkovic 2017).
Different Patterns of Adolescent Cigarette Smoking Trajectories
Developmental psychopathology—the study of the origins and course of maladaptive behavior—encompasses the study of the effects of child maltreatment exposure on adolescent cigarette smoking (Cicchetti & Toth, 2005). The current study investigated heterogeneity in developmental trajectories of smoking behaviors, guided by the developmental psychopathology perspective’s emphasis on development over time that is amenable to longitudinal research (Cicchetti & Toth, 2005).
Trajectory analyses have the advantage of showing heterogeneity in development over time (i.e., subgroups showing different patterns of smoking trajectories over time), which is important in studies of adolescent cigarette smoking, which may be transitory or experimental in some youth and rapidly escalating patterns in others. Prior research employing trajectory analysis have identified four to six distinct smoking trajectories in addition to nonsmoking in adolescent student or community samples, with variations by age of onset, rate of escalation, and persistence (Chassin, Presson, Pitts, & Sherman, 2000; Dutra, Glantz, Lisha, & Song, 2017; Orlando, Tucker, Ellickson, & Klein, 2004). These studies suggest the existence of subgroups of adolescents with distinct trajectories in the development of cigarette smoking of varying levels of risk.
Exposure to child maltreatment may influence adolescents’ memberships in these various trajectory groups. In examinations of other types of substance use, such as heavy drinking, maltreatment exposure has been associated with faster increases in use as well as persistent use over longer periods of time (Shin, Miller, & Teicher, 2013). However, although prior research has established links between child maltreatment and adolescent cigarette smoking (Hussey et al., 2006; Lewis et al., 2011; Kristman-Valente et al., 2013; Moran et al., 2004; Tonmyr et al., 2010), we are aware of no prior research that has examined how maltreatment may relate to trajectories of adolescent cigarette smoking.
Child Maltreatment Type and Timing and Adolescent Cigarette Smoking
Developmental psychopathology suggests that the nature (i.e., the type of maltreatment) and the timing (i.e., developmental stage or chronicity of maltreatment) of adverse experiences may lead to different vulnerability and resilience to the effects of the trauma (Cicchetti & Yoyh, 2005). Therefore, children with early trauma and maltreatment experiences may have different patterns of cigarette smoking trajectories in adolescence, depending on the type and timing of the trauma. Past research has suggested differential effects of various types of maltreatment on adolescent substance use (Yoon, Kobulsky, Yoon, & Kim, 2017), and cigarette smoking specifically (Kristman-Valente et al., 2013; Mills, Alati, Strathearn, & Najman, 2014; Moran et al., 2004). One study found that both physical and sexual abuse were linked to cigarette smoking in adolescent boys, but only sexual abuse was associated with cigarette smoking in adolescent girls (Kristman-Valente et al., 2013). However, this previous study was limited in that neglect and emotional abuse were not examined. Studies examining more comprehensive types of maltreatment simultaneously have had conflicting results (Moran et al., 2004; Mills et al., 2014). Moran and colleagues (2004) found significant associations between all types of self-reported maltreatment examined (i.e., emotional maltreatment, physical abuse, sexual abuse, and co-occurring physical and sexual abuse) and cigarette smoking in a cross-sectional survey of 2,164 adolescent students in Oregon. Another examination found that among various maltreatment types, child protective services (CPS) reported neglect/emotional abuse and co-occurring physical abuse were related to adolescent cigarette smoking in a large Australian sample of 14-year old youths (Mills et al., 2014). However, no significant relationships were found for sexual abuse and non-co-occurring physical abuse (Mills et al., 2014). An improved understanding of how various maltreatment types affect cigarette smoking may be helpful to guide prevention and intervention efforts.
The timing of maltreatment, such as the age of maltreatment occurrence and the chronicity of exposure, has also emerged as an important contributor in the development of adolescent substance use and other negative developmental outcomes, such as brain connectivity abnormalities and behavior problems (Cassiers et al., 2018; Jaffee & Maikovich-Fong, 2011; Jonson-Reid, Kohl, & Drake, 2012; Manly, Kim, Rogosch, & Cicchetti, 2001; Shin, Chung, & Rosenberg, 2016; Teicher, Samson, Anderson, & Ohashi, 2016; Thornberry, Henry, Ireland, & Smith, 2010). However, sparse research has examined these issues with regard to cigarette smoking, making it unclear whether the associations between maltreatment and adolescent cigarette use represent sleeper effects of earlier exposure, more synchronous relations, or both. In a study of 68,107 young women, physical abuse, sexual abuse, and co-occurring physical and sexual abuse during childhood (ages 0–11) and adolescence (ages 11–17) were related to adolescent smoking (Jun et al., 2008). This study suggests that regardless of the timing, child maltreatment may be significantly associated with adolescent smoking. However, the study was limited in that it was based on retrospective self-report of smoking onset and maltreatment exposure, and thus may be susceptible to recall bias. Furthermore, the study considered only physical and sexual abuse. Because emotional maltreatment and neglect were not considered, observed relations may have been spurious.
In summary, there is limited research examining the association between child maltreatment and cigarette smoking as a specific form of adolescent substance use, and research examining high risk samples and variations based on maltreatment type and timing remain sparse. No known research has examined how child maltreatment may predict heterogeneous classes of cigarette smoking trajectories in adolescence.
The Current Study
The current study contributed to the existing literature by modeling developmental trajectories of adolescent cigarette smoking in a sample of youth who were at risk for maltreatment, and by identifying how maltreatment timing and type are associated with distinct cigarette smoking trajectories. Findings from this study could offer valuable insights to prevent cigarette smoking in high-risk youth and promote behavioral health during critical periods of development. We addressed two research questions: 1) Are there different patterns of cigarette smoking trajectories among adolescents who experienced or were at risk for maltreatment in early life? 2) Do child maltreatment type and timing predict distinct patterns of cigarette smoking trajectories? Based on the developmental psychopathology perspective and the general population literature supporting heterogeneity in smoking trajectories in youth (Cicchetti & Toth, 2005; Chassin et al., 2000; Dutra et al., 2017; Orlando et al., 2004), it was hypothesized that there would be various patterns of cigarette smoking trajectories. Drawing from the developmental psychopathology perspective, which stresses the importance of early childhood experiences (Cicchetti & Toth, 2005), it was further hypothesized that early maltreatment experiences would be associated with poor patterns of cigarette smoking (e.g., increasing cigarettes use over time) during adolescence.
Methods
Sample
The current study was conducted using data from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN). LONGSCAN is a consortium of studies involving five study sites across different regions of the United States (Midwest, Southwest, Northwest, South, and East), with the aim of examining the causes and consequences of child abuse and neglect (Larrabee & Lewis, 2014). The target sample of the LONGSCAN study was children who were identified as maltreated or at risk for maltreatment. Each study site recruited participants (baseline: age 4) who experienced or were at risk of experiencing maltreatment (Larrabee & Lewis, 2014). While study sites had different sample recruitment strategies and selection criteria, representing different levels of risk or exposure to maltreatment, at risk for maltreatment generally referred to the presence of one or more risk factors in the family (e.g., low-income, failure to thrive, parental drug use, HIV infected mother) that may lead to child maltreatment. The East cohort included low-income, inner city children who were recruited from pediatric clinics. The Midwest, Southwest, and Northwest cohorts included children who were involved with CPS. The South cohort consisted of children who were identified as a high-risk group at birth, based on a state public health tracking system. The data were collected at child ages 4, 6, 8, 10, 12, 14, 16, and 18 (July 1991–January 2012).
The present study utilized data from 903 adolescents (out of the total 1,354 LONGSCAN sample) who completed at least two waves of age 12, 16, or 18 assessments. Adolescents in the study sample were more likely to be Black and have mothers with no spouse/partner. There were no other significant differences in key study variables between the baseline sample and the study sample.
Measures
Cigarette smoking
Adolescent cigarette smoking was measured using adolescent self-report of cigarette smoking in the past year. At ages 12, 16, and 18, the adolescents reported the number of days in the past year they smoked cigarettes, using the following response options: 0 = 0 days, 1 = 1 to 3 days, 2 = 4 to 20 days, 3 = more than 20 days.
Child maltreatment
The type, timing, and chronicity of child maltreatment experiences were measured using alleged lifetime (i.e., birth to 18 years of age) child maltreatment reports made to CPS. CPS-reported maltreatment allegation narratives were abstracted, reviewed, and coded by highly trained coders using the modified maltreatment classification system (MMCS; English, Bangdiwala, & Runyan, 2005). The MMCS has shown good inter-coder reliability (Kappas >.70; Larrabee & Lewis, 2014). Using the MMCS, four types of non-mutually exclusive maltreatment categories were created based on abstractions from allegation narrative: physical abuse, sexual abuse, emotional abuse, and neglect. The timing of maltreatment was assessed using Erikson’s four stages of development: Infancy/Toddlerhood (ages 0–2); Early childhood (ages 3–5); School Age (ages 6–11); Adolescence (ages 12–18). For each developmental stage, the four maltreatment type variables (0 = no, 1 = yes) were coded. For the chronicity of maltreatment, any type of maltreatment occurring across three or more adjacent development stages were coded as chronic maltreatment (0 = non-chronic maltreatment, 1 = chronic maltreatment, using a similar approach from Jaffee & Maikovich-Fong’s study (2011).
Control variables
We included child sex (0 = male, 1 = female) as a control variable because males tend to have higher rates of cigarette smoking than females in late adolescence (e.g., 12th graders; Johnston et al., 2018). We also controlled for child race reported by the caregivers at baseline. About 55% of the sample was Black, 25% was White, 7% was Hispanic, and the remaining 13% was other race. Based on previous studies consistently indicating higher rates of cigarette use among White U.S. adolescents (Bares, Kendler, & Maes, 2016; Johnston et al., 2018), race was dichotomized as 0 = Non-White and 1 = White. Based on empirical evidence suggesting family and peer cigarette use as predictors of adolescent cigarette use (Ennett et al., 2008; Gilman et al., 2009), family cigarette use and peer cigarette use were controlled for in the model. Family cigarette use was measured at age 12 by asking the youth if anyone with whom they live (i.e., a household member) smokes cigarettes (0 = no, 1= yes). For peer cigarette use, the youth were asked how many of their close friends (response categories: 0 = none, 1 = some, 2 = most) smoke cigarettes. The responses for peer cigarette use were dichotomized: 0 = no (none of my friends use cigarettes) and 1= yes (some or most of my friends use cigarettes). Family poverty status was measured using the caregiver’s self-report of the annual household income and the number of household members, and was coded as 1 = below the poverty level if the family income was below the federal poverty level and 0 otherwise. The five LONGSCAN sites (Midwest, Southwest, Northwest, South, and East) were dummy coded using East as a reference group.
Data Analysis
Latent class growth analysis (LCGA) was performed to examine heterogeneity in patterns of adolescent cigarette smoking. Adolescent self-reports of the number of days they smoked cigarettes in the past year, assessed at ages 12, 16, and 18, were entered into a series of unconditional LCGA models. LCGA is a special type of growth mixture modeling (GMM) in which all intercept and slope variances are fixed to zero (Jung & Wickrama, 2008). In our study, we chose LCGA over GMM and other longitudinal analytical models, such as longitudinal latent class analysis (LLCA), because LCGA models are more straightforward and parsimonious while yielding statistically equally reliable results when used with ordered categorical data (Feldman, Masyn, & Conger, 2009). The optimal number of classes was based on fit indices, class size (>5% of the total sample), interpretability, classification accuracy (entropy), and consistency with theory and previous literature (Jung & Wickrama, 2008). Fit indices used in the study included Bayesian Information Criterion (BIC); the Vuong-Lo-Mendell-Rubin Likelihood Ratio test (LMR-LRT); and Parametric Bootstrapped Likelihood Ratio (BLRT). A smaller value of BIC, and significant LMR-LRT and BLRT values indicate better model fit (Jung & Wickrama, 2008). Once the optimal number of classes was determined, the plots were carefully reviewed for the interpretability of the trajectories (i.e., latent classes), and each class was named. Finally, multinomial logistic regression was conducted to examine if the type, timing, and chronicity of maltreatment were significant predictors of membership in the identified classes. Maltreatment type/timing variables (e.g., early childhood sexual abuse, school age sexual abuse, adolescence sexual abuse) and the maltreatment chronicity variable (0 = non-chronic maltreatment, 1 = chronic maltreatment) were entered into the multinomial logistic regression as focal independent variables.
Results
Sample Characteristics
A little less than half of the adolescents were male (47.1%) and lived in a household with an annual income below the federal poverty level (48.6%). Approximately one quarter of the sample was White (23.8%). At age 12, the majority (94.1%) of the adolescents reported no cigarette use, and three quarters (75.2%) of the adolescents reported no cigarette use at age 16. At age 18, about 40% of the adolescents reported having smoked cigarettes in the past year, with 10.1% reporting 1 to 3 days, 5.1% reporting 4 to 20 days, and 23.7% reporting more than 20 days of cigarette use. About 60% of the adolescents reported having a family member who smoked cigarettes and 7.2% reported peer cigarette smoking. The descriptive statistics of study variables, including maltreatment experiences, are summarized in Table 1. Table 2 displays the descriptive statistics of cigarette smoking at ages 12, 16, and 18 by the type of maltreatment experienced.
Table 1.
Descriptives of the Study Variables (N=903)
| % / M (SD) | |
|---|---|
| Child’s age (years) | 12.35 (.43) |
| Child’s race (White) | 23.8 |
| Child’s gender (male) | 47.1 |
| Poverty (< federal poverty level) | 48.6 |
| Family cigarette smoking | 58.0 |
| Peer cigarette smoking | 7.2 |
| Chronic maltreatment | 12.0 |
| Early childhood physical abuse | 11.6 |
| Early childhood sexual abuse | 7.8 |
| Early childhood emotional abuse | 10.1 |
| Early childhood neglect | 23.3 |
| School age physical abuse | 19.0 |
| School age sexual abuse | 7.5 |
| School age emotional abuse | 17.5 |
| School age neglect | 24.1 |
| Adolescent physical abuse | 9.7 |
| Adolescent sexual abuse | 4.4 |
| Adolescent emotional abuse | 9.1 |
| Adolescent neglect | 10.2 |
Table 2.
Cigarette Smoking by Maltreatment Type (N=903)
| Physical abuse | Sexual abuse | Emotional Abuse | Neglect | Total Sample | |
|---|---|---|---|---|---|
| % | % | % | % | % | |
| Past year cigarette smoking at age 12 | |||||
| 0 days | 88.8 | 88.4 | 89.7 | 90.1 | 90.5 |
| 1 to 3 days | 4.3 | 5.4 | 2.7 | 4.2 | 4.3 |
| 4 to 20 days | 3.7 | 3.6 | 5.1 | 3.9 | 3.3 |
| More than 20 days | 3.2 | 2.6 | 2.5 | 1.8 | 1.9 |
| Past year cigarette smoking at age 16 | |||||
| 0 days | 70.6 | 64.4 | 85.4 | 76.4 | 74.4 |
| 1 to 3 days | 10.4 | 12.6 | 7.2 | 9.3 | 10.6 |
| 4 to 20 days | 6.1 | 5.6 | 1.0 | 4.9 | 5.1 |
| More than 20 days | 12.9 | 17.4 | 6.4 | 9.4 | 9.9 |
| Past year cigarette smoking at age 18 | |||||
| 0 days | 53.8 | 52.1 | 75.8 | 60.4 | 61.3 |
| 1 to 3 days | 11.1 | 11.2 | 8.4 | 8.9 | 10.0 |
| 4 to 20 days | 5.6 | 5.2 | 2.8 | 4.9 | 5.1 |
| More than 20 days | 29.5 | 31.5 | 13.0 | 25.8 | 23.6 |
Patterns of Cigarette Smoking Trajectories
Table 3 presents the model fit indices for the LCGA adolescent cigarette smoking trajectory models. The 3-class model had the smallest BIC value, suggesting the best-fitting model. The LMR and BLRT statistics in the 4-class model were not significant, indicating that adding a 4th class did not significantly improve the model fit, favoring the 3-class model over the 4-class model. The examination of the plots generated from Mplus for the 3-class model once again confirmed the interpretable and distinct classes in the 3-class model. Thus, the 3-class model was selected as the optimal model. Based on the patterns of cigarette use over time (see Figure 1), we named the classes as follows: 1) Stable no/low cigarette use; 2) Gradually increasing cigarette use; and 3) Sharply increasing cigarette use. Adolescents in the stable no/low cigarette use class (61%) showed no cigarette use or consistently low levels of cigarette use throughout the data collection period. Adolescents in the gradually increasing cigarette use class showed steadily increasing levels of cigarette use over time. Adolescents in the sharply increasing cigarette use class showed rapidly growing rates of cigarette smoking over time.
Table 3.
Model Fit Indices for Cigarette GMM Models
| Model | BIC | LMR | LMR p-value | BLRT | BLRT p-value | Sample in the Smallest class |
|---|---|---|---|---|---|---|
| 1-class | 3404.799 | |||||
| 2-class | 3186.918 | 227.171 | <.001 | 238.298 | <.001 | 30.3% |
| 3-class | 3185.880 | 20.454 | .0004 | 21.456 | <.001 | 9.30% |
| 4-class | 3200.715 | 5.322 | 0.0622 | 5.583 | .5000 | 0.7% |
Note. BIC=Bayesian Information Criterion; LMR=Lo-Mendell-Rubin Likelihood Ratio Test; BLRT=Parametric Bootstrapped Likelihood Ratio.
Figure 1.
Adolescent Cigarette Smoking Trajectory Classes
Predictors of Cigarette Smoking Trajectory Patterns
Table 4 displays the results of a multinomial logistic regression analysis examining the type, timing, and chronicity of maltreatment as predictors of membership in the identified cigarette smoking trajectory classes. The stable no/low cigarette use class was used as a reference group in analyzing and interpreting the models.
Table 4.
Predictors of Cigarette Smoking Trajectory Groups (Reference group: Stable Low)
| Comparison Group(s) | Sharp increase |
Gradual increase |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Maltreatment characteristics | ||||||
| Chronic maltreatment | .702 | [.29, 1.71] | .437 | 1.497 | [.82, 2.75] | .194 |
| Early childhood physical abuse | 2.301 | [1.14, 4.67] | .021 | 1.097 | [.64, 1.88] | .736 |
| Early childhood sexual abuse | 1.480 | [.66, 3.32] | .341 | .618 | [.32, 1.20] | .156 |
| Early childhood emotional abuse | 1.382 | [.61, 3.13] | .437 | .972 | [.55, 1.73] | .923 |
| Early childhood neglect | 1.302 | [.68, 2.50] | .426 | 1.890 | [1.24, 2.87] | .003 |
| School age physical abuse | 1.091 | [.53, 2.25] | .814 | .619 | [.38, 1.01] | .057 |
| School age sexual abuse | 1.151 | [.46, 2.89] | .765 | 1.169 | [.62, 2.21] | .631 |
| School age emotional abuse | .931 | [.44, 1.99] | .853 | 1.041 | [.63, 1.73] | .878 |
| School age neglect | .787 | [.41, 1.51] | .472 | 1.097 | [.72, 1.68] | .669 |
| Adolescent physical abuse | 3.703 | [1.66, 8.26] | .001 | 1.057 | [.56, 1.99] | .863 |
| Adolescent sexual abuse | 1.896 | [.65, 5.55] | .243 | 1.473 | [.66, 3.30] | .347 |
| Adolescent emotional abuse | 1.350 | [.56, 3.25] | .504 | 1.816 | [.94, 3.51] | .076 |
| Adolescent neglect | 1.488 | [.67, 3.32] | .331 | 1.525 | [.86, 2.70] | .148 |
| Control Variables | ||||||
| Child’s gender (male) | 1.726 | [1.04, 2.88] | .036 | 1.467 | [1.07, 2.02] | .018 |
| Child’s race (White) a | 2.445 | [1.27, 4.70] | .007 | 1.331 | [.86, 2.06] | .198 |
| Poverty (< federal poverty level) | 1.062 | [.63, 1.81] | .823 | .765 | [.55, 1.07] | .116 |
| Peer cigarette smoking | 2.300 | [1.01, 5.28] | .049 | 1.644 | [.87, 3.10] | .124 |
| Family cigarette smoking | 1.525 | [.86, 2.72] | .153 | 1.277 | [.91, 1.80] | .160 |
| LONSCAN siteb | ||||||
| Midwest | 1.132 | [.41, 3.17] | .813 | 1.319 | [.78, 2.25] | .307 |
| Northwest | 1.225 | [.45, 3.33] | .690 | 1.444 | [.81, 2.56] | .208 |
| Southwest | 1.776 | [.69, 4.56] | .232 | 1.932 | [1.15, 3.26] | .014 |
| South | 4.098 | [1.67, 10.04] | .002 | 2.451 | [1.45,4.15] | .001 |
Note. OR= odds ratio
Non-White is the reference group
East is the reference group.
Sharply increasing cigarette use class
Adolescents who experienced early childhood physical abuse were 2.30 times more likely to be in the sharply increasing cigarette use class compared with the stable no/low class. Physical abuse during adolescence was associated with 3.70 times higher odds of membership in this group. Adolescents who were male, White, and had peers who smoked cigarettes also had higher odds of being in this class. Youth recruited from the South site were also more likely to be in the sharply increasing cigarette use class.
Gradually increasing cigarette use class
Adolescents who were neglected during early childhood were 1.89 times more likely to be in the gradually increasing cigarette use class than in the stable no/low class. Being male and recruitment from Southern areas (i.e., Southwest and South sites) were also predictive of membership in the gradually increasing cigarette use class.
Discussion
The purpose of the current study was to better understand the role of maltreatment type at different developmental time points in relation to cigarette smoking trajectories during adolescence, a sensitive period of development. We found heterogeneous patterns of adolescent smoking trajectories; this is consistent with previous literature (e.g., Chassin et al., 2000; Dutra et al., 2017). The findings extend the existing literature by observing distinct patterns in a group of youth who are high-risk for maltreatment. In contrast to past literature (Chassin et al., 2000; Dutra et al., 2017; Orlando et al., 2004), trajectories were differentiated mainly on the rate of increase of cigarette use rather than the age of onset and stability of use. The high-risk sample examined in this study may explain these differences, as could the methodological differences such as number of time points and variable scaling.
Especially in the context of a high-risk sample, we are cautiously optimistic of the relatively large proportion of adolescents in the stable no/low cigarette use class. This finding is consistent with the child welfare literature documenting resilience among child welfare-involved and other high-risk youth (Bell, Romano, & Flynn, 2015; Goldstein, Faulkner, & Wekerle, 2013). We find that about 60% of the high-risk sample show extremely low levels of cigarette use over time. This suggests that youth can exhibit resilient behavioral functioning and adjustment even in the face of adverse life circumstances (Yoon, 2018). However, it is of note that the higher attrition of White youth from the LONGSCAN study and higher rates of smoking in the general population could also have affected this finding (Johnston et al., 2018).
We found that physical abuse during early childhood and physical abuse in adolescence both predicted membership in the sharply increasing cigarette use class. These findings are in line with previous research which found that physical abuse is a predictor of adolescent substance use (Kobulsky, Holmes, Yoon, & Perzynski, 2016; Moran et al., 2004; Simpson & Miller, 2002). It is interesting that physical abuse, especially during early childhood and, was associated with rapidly escalating smoking over time. Findings seem to indicate that physical abuse may have a particularly strong association with cigarette smoking in adolescence.
Whereas physical abuse was strongly associated with a sharp increase in cigarette use, neglect during early childhood predicted membership in the gradually increasing cigarette use class. This finding is in line with previous research that found neglect as a predictor of later substance use (Dube et al., 2003). The role of neglect in gradual increases in cigarette use may suggest that inadequate levels of supervision or parental monitoring are associated with negative or harmful behavior in adolescence, as the majority of neglect cases involve supervisory neglect (Mennen, Kim, Sang, & Trickett, 2010).
Considering that physical abuse during early childhood and adolescence predicted membership in the sharply increasing cigarette use class and neglect during early childhood predicted membership in the gradually increasing cigarette use class, our findings appear to point early childhood and adolescence to be two time periods that are crucial for understanding adolescent cigarette smoking. Early childhood is a period of substantial development of emotional regulation, or the ability to manage internal emotional states and external emotional expression (Calkins & Fox, 2002; Eisenberg, 2000). Emotional regulatory control can impact subsequent behavior regulation (Calkins & Fox, 2002). One review found that parenting style is related to child development of emotional regulation, and that maltreatment can result in patterns of emotional dysregulation in children (Morris, Silk, Steinberg, Myers, & Robinson, 2007). Thus, emotional dysregulation may partially explain the observed relationship between maltreatment in early childhood and the later development of substance use disorders (Wolff et al., 2016), making early childhood a sensitive developmental period and critical point for intervention to prevent subsequent smoking onset and cigarette use patterns.
Adolescence is also a sensitive period during which the prefrontal cortex—a brain region responsible for impulse control, decision-making, and future-oriented thinking—gradually develops. This structure does not finish developing until around 25 years of age (Giedd, 2004), which may partially explain increased risk-taking behaviors in adolescence (Steinberg, 2007). The combination of risk-taking behavior and difficulty controlling impulses during a period of intensive neurodevelopment may leave adolescents particularly susceptible to acquiring substance use disorders (Chambers, Taylor, & Potenza, 2003; Crews, He, & Hodge, 2007). This risk is compounded for youth who have experienced abuse or neglect, as trauma and maltreatment histories make youth more susceptible to executive dysfunction in adolescence (Spann et al., 2012). It seems that risk for maltreatment and trauma during these two key developmental stages (i.e., early childhood, adolescence) may place adolescents in a vulnerable position for behavioral maladaptation, such as smoking cigarettes. However, it should be noted that maltreatment during adolescence (ages 12–18) and adolescent cigarette smoking were measured concurrently, and thus we are unable to draw any causal inference between maltreatment and cigarette use during this developmental stage.
Strengths and Limitations
This study had several limitations. The sample only included youth who were categorized as high risk for maltreatment. While this group represents a valuable population of interest to public health policy-makers, practitioners, and researchers, findings may not generalize to other populations of youth. Furthermore, limitations in CPS surveillance methods may have led to an increased risk of Type II error. For example, the frequency of sexual abuse was very low in the sample, which may explain the null relationship between sexual abuse and cigarette smoking trajectories. Although beyond the scope of the current study, polyvictimization —exposure to multiple forms of violence, crime, and abuse — (Finkelhor, Turner, Hamby, & Ormrod, 2011) may play an important role in explaining heterogeneity in developmental trajectories of cigarette use among vulnerable youth. Therefore, future research should consider testing the effects of polyvicimization on various patterns of cigarette use trajectories in adolescence.
Also of potential concern is the scaling of the item used to measure cigarette smoking. The response options were not well suited to capture the true range of variability in smoking patterns within a year and may limit generalizability. Unfortunately, this item was the only measure of smoking available in the dataset for all three time points (ages 12, 16, and 18). Further, it is unclear how attrition may have affected study findings. Data were also dependent solely on youth self-report of cigarette smoking. Self-report data from youth may not always be reliable, particularly regarding risky behaviors (Williams & Nowatzki, 2005). Youth have been found to report their cigarette use more reliably in the short term (~2 weeks) versus the long term (Rosenbaum, 2009). When reporting use over a longer period, as in the current study, youth may have been more susceptible to social desirability bias, leading them to under-report their actual cigarette use. Future research should consider including biomarkers to corroborate findings and eliminate potential biases inherent to self-report data.
Another notable limitation is that we focused on cigarettes use only and did not capture other related forms of tobacco and nicotine use, such as dip or vaping (i.e., electronic cigarette use), due to the lack of available data. Although we acknowledge the importance of other forms of tobacco and nicotine use, cigarette smoking warrants specific research because it remains the leading cause of preventable disease and death in the United States (Centers for Disease Control and Prevention, 2019). Furthermore, cigarette smoking is highly concentrated among most vulnerable youth and drives major health disparities between privileged and more marginalized adolescent populations. It is also worth noting that e-cigarette use is a risk factor for cigarette smoking onset for adolescents generally considered to be at low risk of cigarette smoking (Wills, Sargent, Gibbons, Pagano, & Schweitzer, 2017) and that adolescents who vape or use e-cigarettes are those who would not initiate the use of tobacco or nicotine products (Barrington-Trimis et al., 2016). This trend may be in part due to adolescent decisions to first try vaping being driven by taste and flavoring (Miech, Patrick, O’malley, & Johnston, 2017; Pepper, Ribisl, & Brewer, 2016) rather than by a desire to use nicotine or adopt an emotional/behavioral coping strategy. As the use of vaping typically precedes traditional tobacco cigarette use and is more rampant among a low-risk sample of youth, consideration of vaping and e-cigarette use may be less applicable to the high-risk group of adolescents considered in the present study. Nonetheless, future studies should consider examining various patterns of e-cigarette use trajectories as well as the impact of child maltreatment on vaping trajectory patterns, given the adolescent vaping epidemic in the U.S. (Farzal, Perry, Yarbrough, & Kimple, 2019).
These limitations are balanced by the notable strengths of this study. The longitudinal design allowed for predictions to be made based on the data. A sophisticated methodological approach was employed to identify trajectories and patterns in youth behavior over time. Because of the benefits of the methodology, this study was the first to identify differential cigarette smoking patterns among youth at high-risk for maltreatment. This study also contributed to enhancing our understanding of the associations of different aspects of maltreatment (i.e., type, timing, chronicity) with cigarette smoking trajectories in adolescence. Past research has not examined these specific characteristics of maltreatment in relation to cigarette smoking, a distinct form of substance use, during adolescence. Finally, the study considered the role of several potential confounds (e.g., poverty, family cigarette use, peer cigarette use) of the maltreatment to adolescent cigarette smoking relation.
Implications
The findings from this study provide some empirical evidence for the existence of heterogeneity in the developmental trajectories of adolescent cigarette smoking among populations at high-risk for maltreatment. Additional research using similar person-centered methodological approaches is needed to identify patterns of developmental trajectories of other substances beyond cigarettes among this population. For instance, future studies should examine other forms of tobacco and nicotine use, such as dip, e-cigarettes, or vaping (juuling) in adolescence to capture additional variance or nuance that may not have been detected in the current study due to its narrow focus on cigarette smoking.
The study has significant implications for practice. Data revealed that cigarette use was very low across groups at age 12, but had substantially increased by age 16. This finding suggests that prevention efforts should be targeted early, beginning in pre-adolescence, to prevent cigarette use during mid to late adolescence. Additionally, more intensive intervention efforts should target youth with experiences of physical abuse and neglect, as these experiences were significantly related to increasing cigarette use in adolescence. Early childhood and adolescence seem to be particularly vulnerable periods of maltreatment affecting later cigarette smoking. Around these developmental stages, additional prevention efforts should be instituted; these efforts may include parental education around appropriate supervision and disciplinary practices, among other maltreatment prevention services. Finally, practitioners seeking to intervene with frequent adolescent cigarette smoking should assess for maltreatment exposure and integrate trauma-informed approaches to help alleviate the ongoing symptoms as they contribute to maladaptive coping strategies, such as adolescent cigarette use.
Acknowledgments
This document includes data from the Consortium of Longitudinal Studies of Child Abuse and Neglect (LONGSCAN), which was funded by the Office on Child Abuse and Neglect (OCAN), Children’s Bureau, Administration for Children and Families, Dept. of Health and Human Services (The National Center on Child Abuse and Neglect (NCCAN). The data were made available by the National Data Archive on Child Abuse and Neglect (NDACAN), Cornell University, Ithaca, NY, and have been used with permission. The collector of the original data, the funder, NDACAN, Cornell University and their agents or employees bear no responsibility for the analyses or interpretations presented here.
This research was funded by The Ohio State University Institute for Population Research through a grant from the Eunice Kennedy Shriver NICHD, P2CHD058484. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver NICHD or the NIH.
References
- Afifi TO, Mota N, MacMillan HL, & Sareen J (2013). Harsh physical punishment in childhood and adult physical health. Pediatrics, 132(2), e333–e340. [DOI] [PubMed] [Google Scholar]
- Bares CB, Kendler KS, & Maes HH (2016). Racial differences in heritability of cigarette smoking in adolescents and young adults. Drug & Alcohol Dependence, 166, 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington-Trimis JL, Urman R, Leventhal AM, Gauderman WJ, Cruz TB, Gilreath TD, … & McConnell R (2016). E-cigarettes, cigarettes, and the prevalence of adolescent tobacco use. Pediatrics, 138(2), e20153983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell T, Romano E, & Flynn RJ (2015). Profiles and predictors of behavioral resilience among children in child welfare. Child Abuse & Neglect, 48, 92–103. [DOI] [PubMed] [Google Scholar]
- Calkins SD, & Fox NA (2002). Self-regulatory processes in early personality development: A multilevel approach to the study of childhood social withdrawal and aggression. Development and Psychopathology, 14(3), 477–498. [DOI] [PubMed] [Google Scholar]
- Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Grucza RA, & Bierut LJ (2014). Youth tobacco use type and associations with substance use disorders. Addiction, 109(8), 1371–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2019). Smoking & Tobacco Use. Retrieved from https://www.cdc.gov/tobacco/data_statistics/index.htm
- Chambers RA, Taylor JR, & Potenza MN (2003). Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. American Journal of Psychiatry, 160(6), 1041–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Presson CC, Pitts SC, & Sherman SJ (2000). The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychology, 19(3), 223. [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2005). Child maltreatment. Annu. Rev. Clin. Psychol, 1, 409–438. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Handley ED (2019). Child maltreatment and the development of substance use and disorder. Neurobiology of Stress, 100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crews F, He J, & Hodge C (2007). Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacology Biochemistry and Behavior, 86(2), 189–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, & Anda RF (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics, 111(3), 564–572. [DOI] [PubMed] [Google Scholar]
- Duprey EB, Oshri A, & Caughy MO (2017). Childhood neglect, internalizing symptoms and adolescent substance use: does the neighborhood context matter?. Journal of Youth and Adolescence, 46(7), 1582–1597. [DOI] [PubMed] [Google Scholar]
- Dutra LM, Glantz SA, Lisha NE, Song AV (2017) Beyond experimentation: Five trajectories of cigarette smoking in a longitudinal sample of youth. PLoS ONE 12(2): e0171808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N (2000). Emotion, regulation, and moral development. Annual review of Psychology, 51(1), 665–697. [DOI] [PubMed] [Google Scholar]
- Elliott JC, Stohl M, Wall MM, Keyes KM, Goodwin RD, Skodol AE, … & Hasin DS (2014). The risk for persistent adult alcohol and nicotine dependence: the role of childhood maltreatment. Addiction, 109(5), 842–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- English DJ, Bangdiwala SI, & Runyan DK (2005). The dimensions of maltreatment: Introduction. Child Abuse & Neglect, 29(5), 441–460. [DOI] [PubMed] [Google Scholar]
- Ennett ST, Faris R, Hipp J, Foshee VA, Bauman KE, Hussong A, & Cai L (2008). Peer smoking, other peer attributes, and adolescent cigarette smoking: A social network analysis. Prevention Science, 9(2), 88–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farzal Z, Perry MF, Yarbrough WG, & Kimple AJ (2019). The Adolescent Vaping Epidemic in the United States—How It Happened and Where We Go From Here. JAMA Otolaryngology–Head & Neck Surgery. [DOI] [PubMed] [Google Scholar]
- Feldman BJ, Masyn KE, & Conger RD (2009). New approaches to studying problem behaviors: a comparison of methods for modeling longitudinal, categorical adolescent drinking data. Developmental Psychology, 45(3), 652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Turner H, Hamby SL, & Ormrod R (2011). Polyvictimization: Children’s Exposure to Multiple Types of Violence, Crime, and Abuse. Washington, DC: US Government Printing Office. [Google Scholar]
- Giedd JN (2004). “Structural magnetic resonance imaging of the adolescent brain.” Adolescent Brain Development: Vulnerabilities and Opportunities: 77–85. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Rende R, Boergers J, Abrams DB, Buka SL, Clark MA, … & Lloyd-Richardson EE (2009). Parental smoking and adolescent smoking initiation: an intergenerational perspective on tobacco control. Pediatrics, 123(2), e274–e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein AL, Faulkner B, & Wekerle C (2013). The relationship among internal resilience, smoking, alcohol use, and depression symptoms in emerging adults transitioning out of child welfare. Child Abuse & Neglect, 37(1), 22–32. [DOI] [PubMed] [Google Scholar]
- Hackshaw A. Morris, J. K., Boniface S Tange J & Milnkovic D (2018). Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ, 360: doi: 10.1136/bmj.j5855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics, 118,933–42. [DOI] [PubMed] [Google Scholar]
- Husten CG (2007). Smoking Cessation in Young Adults. American Journal of Public Health, 97(8), 1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristman-Valente AN, Brown EC, & Herrenkohl TI (2013). Child physical and sexual abuse and cigarette smoking in adolescence and adulthood. Journal of Adolescent Health, 53(4), 533–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonson-Reid M, Kohl PL, & Drake B (2012). Child and adult outcomes of chronic child maltreatment. Pediatrics, 129(5), 839–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2018). Monitoring the Future national survey results on drug use: 1975–2017: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan [Google Scholar]
- Jun HJ, Rich-Edwards JW, Boynton-Jarrett R, Austin SB, Frazier AL, & Wright RJ (2008). Child abuse and smoking among young women: the importance of severity, accumulation, and timing. Journal of Adolescent Health, 43(1), 55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung T, & Wickrama KAS (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317. [Google Scholar]
- Kobulsky JM, Holmes MR, Yoon S, & Perzynski AT (2016). Physical abuse after child protective services investigation and adolescent substance use. Children and Youth Services Review, 71, 36–44. [Google Scholar]
- Larrabee HM, & Lewis T (2014). Longitudinal studies of child abuse and neglect (LONGSCAN) assessments 0–18: User’s guide. Ithaca, NY: National Data Archive on Child Abuse and Neglect, Cornell University. [Google Scholar]
- Lewis T, Kotch J, Proctor L, Thompson R, English D, Smith J, … & Dubowitz H (2019). The role of emotional abuse in youth smoking. American journal of preventive medicine, 56(1), 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TL, Kotch J, Wiley TR, Litrownik AJ, English DJ, Thompson R, … & Dubowitz H (2011). Internalizing problems: a potential pathway from childhood maltreatment to adolescent smoking. Journal of Adolescent Health, 48(3), 247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydon DM, Wilson SJ, Child A, & Geier CF (2014). Adolescent brain maturation and smoking: what we know and where we’re headed. Neuroscience & Biobehavioral Reviews, 45, 323–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennen FE, Kim K, Sang J, & Trickett PK (2010). Child neglect: Definition and identification of youth’s experiences in official reports of maltreatment. Child Abuse & Neglect, 34(9), 647–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R, Patrick ME, O’malley PM, & Johnston LD (2017). What are kids vaping? Results from a national survey of US adolescents. Tobacco Control, 26(4), 386–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, Schulenberg JE, Johnston LD, Bachman JG, O’Malley PM, & Patrick ME (2017). “National Adolescent Drug Trends in 2017: Findings Released.” Monitoring the Future. Retrieved from: Retrieved March 19, 2018 from http://www.monitoringthefuture.org
- Mills R, Alati R, Strathearn L, & Najman JM (2014). Alcohol and tobacco use among maltreated and non-maltreated adolescents in a birth cohort. Addiction, 109(4), 672–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran PB, Vuchinich S, & Hall NK (2004). Associations between types of maltreatment and substance use during adolescence. Child Abuse & Neglect, 28(5), 565–574. [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, & Robinson LR (2007). The role of the family context in the development of emotion regulation. Social Development, 16(2), 361–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlando M, Tucker JS, Ellickson PL, & Klein DJ (2004). Developmental Trajectories of Cigarette Smoking and Their Correlates From Early Adolescence to Young Adulthood. Journal of Consulting and Clinical Psychology, 72(3), 400–410. [DOI] [PubMed] [Google Scholar]
- Pepper JK, Ribisl KM, & Brewer NT (2016). Adolescents’ interest in trying flavoured e-cigarettes. Tobacco Control, 25(Suppl 2), ii62–ii66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum JE (2009). Truth or consequences: the intertemporal consistency of adolescent self-report on the Youth Risk Behavior Survey. American Journal of Epidemiology, 169(11), 1388–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SH, Chung E, & Rosenberg R (2016). Identifying sensitive periods for alcohol use: The roles of timing and chronicity of child physical abuse. Alcoholism: Clinical and Experimental Research, 40(5), 1020–1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SH, Miller DP, & Teicher MH (2013). Exposure to childhood neglect and physical abuse and developmental trajectories of heavy episodic drinking from early adolescence into young adulthood. Drug & Alcohol Dependence, 127(1), 31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson TL, & Miller WR (2002). Concomitance between childhood sexual and physical abuse and substance use problems: A review. Clinical Psychology Review, 22(1), 27–77. [DOI] [PubMed] [Google Scholar]
- Smith RF, McDonald CG, Bergstrom HC, Ehlinger DG, & Brielmaier JM (2015). Adolescent nicotine induces persisting changes in development of neural connectivity. Neuroscience & Biobehavioral Reviews, 55, 432–443. [DOI] [PubMed] [Google Scholar]
- Spann MN, Mayes LC, Kalmar JH, Guiney J, Womer FY, Pittman B, … & Blumberg HP (2012). Childhood abuse and neglect and cognitive flexibility in adolescents. Child Neuropsychology, 18(2), 182–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L (2007). Risk taking in adolescence: New perspectives from brain and behavioral science. Current Directions in Psychological Science, 16(2), 55–59. [Google Scholar]
- Taha F, Galea S, Hien D, & Goodwin RD (2014). Childhood maltreatment and the persistence of smoking: a longitudinal study among adults in the US. Child Abuse & Neglect, 38(12), 1995–2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tantisuwat A, & Thaveeratitham P (2014). Effects of smoking on chest expansion, lung function, and respiratory muscle strength of youths. Journal of Physical Therapy science, 26(2), 167–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Henry KL, Ireland TO, & Smith CA (2010). The causal impact of childhood-limited maltreatment and adolescent maltreatment on early adult adjustment. Journal of Adolescent Health, 46(4), 359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R, Lewis T, Neilson EC, English DJ, Litrownik AJ, Margolis B, … & Dubowitz H (2017). Child maltreatment and risky sexual behavior: indirect effects through trauma symptoms and substance use. Child Maltreatment, 22(1), 69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonmyr L, Thornton T, Draca J, & Wekerle C (2010). A review of childhood maltreatment and adolescent substance use relationship. Current Psychiatry Reviews, 6(3), 223–234. [Google Scholar]
- U.S. DHHS. (2012). Preventing tobacco use among youth and young adults : a report of the Surgeon General. Rockville, MD: U.S. Dept. of Health and Human Services, Public Health Service, Office of the Surgeon General. [Google Scholar]
- U.S. DHHS Administration for Children and Families. (2019). Child Maltreatment 2017. Washington, D.C. Retrieved from https://www.acf.hhs.gov/sites/default/files/cb/cm2017.pdf. [Google Scholar]
- Walker JF, & Loprinzi PD (2014). Longitudinal examination of predictors of smoking cessation in a national sample of US adolescent and young adult smokers. Nicotine & Tobacco Research, 16(6), 820–827. [DOI] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, Bentley T, & Johnson MS (2012). A prospective investigation of physical health outcomes in abused and neglected children: new findings from a 30-year follow-up. American Journal of Public health, 102(6), 1135–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams RJ, & Nowatzki N (2005). Validity of adolescent self-report of substance use. Substance Use & Misuse, 40(3), 299–311. [DOI] [PubMed] [Google Scholar]
- Wills TA, Sargent JD, Gibbons FX, Pagano I, & Schweitzer R (2017). E-cigarette use is differentially related to smoking onset among lower risk adolescents. Tobacco Control, 26(5), 534–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff S, Holl J, Stopsack M, Arens EA, Höcker A, Staben KA, … & CANSAS Study Group. (2016). Does emotion dysregulation mediate the relationship between early maltreatment and later substance dependence? Findings of the CANSAS Study. European Addiction Research, 22(6), 292–300. [DOI] [PubMed] [Google Scholar]
- Yoon S (2018). Fostering Resilient Development: Protective Factors Underlying Externalizing Trajectories of Maltreated Children. Journal of Child and Family Studies, 27(2), 443–452. [Google Scholar]
- Yoon S, Kobulsky JM, Yoon D, & Kim W (2017). Developmental pathways from child maltreatment to adolescent substance use: The roles of posttraumatic stress symptoms and mother-child relationships. Children and Youth Services Review, 82, 271–279. [DOI] [PMC free article] [PubMed] [Google Scholar]