Abstract
Background:
Because of reduced mortality, patients with HIV are living longer and presenting with chronic diseases. Little is known about racial differences in dermatologic conditions associated with HIV infection.
Objective:
This study examines associated dermatologic conditions in a large population of patients with HIV at a tertiary care center with a diverse patient population.
Methods:
Cross-sectional study of patients with HIV seen between July 14, 2013, and July 14, 2018, in a tertiary health care system. The burden of HIV-related dermatologic conditions was collected by using medical records. Patients with HIV were compared with control individuals of the same race, and significance was assessed using the chi-square test. A Bonferroni correction was performed to control for multiple hypothesis testing.
Results:
The study population (N = 4679) was 64.7% male and 69% African American, with 88.7% of patients receiving antiretroviral therapy. African American patients with HIV had a greater risk of oral hairy leukoplakia (odds ratio [OR], 64.49), herpes zoster (OR, 9.27), prurigo nodularis (OR, 8.80), and squamous cell carcinoma (OR, 5.72).
Limitations:
Our data describe patients seen by 1 health care system.
Conclusions:
African American patients with HIV may be at increased risk for pruritic disorders compared with race-matched control individuals and white patients with HIV.
Keywords: antiretroviral therapy, human immunodeficiency virus, Kaposi sarcoma, oral hairy leukoplakia, prurigo nodularis, pruritus
More than 1 million people in the United States are currently living with HIV, with nearly 40 000 new infections in the past year.1 With the onset of antiretroviral therapy (ART) in 1996, certain mucocutaneous manifestations of HIV immunodeficiency decreased, including neoplastic conditions, such as Kaposi sarcoma, and infectious etiologies, such as oral hairy leukoplakia, bacillary angiomatosis, molluscum, and thrush.2–7 In 1 cohort of 534 patients seen at a specialty HIV dermatology clinic, the most frequent dermatologic diagnoses were human papillomavirus, seborrheic dermatitis, xerosis, and dermatophytosis.8 However, the majority of patients were white men, limiting the applicability of the findings to other populations. In addition, newer guidelines recommending early ART initiation immediately at diagnosis may also change the types of dermatoses seen in ART-suppressed patients with HIV.9,10
We thus investigated the prevalence and relative frequency of dermatologic conditions of 4679 patients with HIV seen in an diverse, urban tertiary care center. Our study examined 58 skin conditions that frequently occur in populations with HIV, and we found several unique racial differences in dermatologic conditions.
METHODS
Institutional review board approval was waived because only anonymous aggregate-level data were used. We used the electronic medical record system Epic (Epic, Verona, WI) to collect data. Data were collected for all patients with HIV infection and control individuals seen between July 14, 2013, and July 14, 2018, at Johns Hopkins Hospitals. All patients were at least 18 years old. Patient race was determined by how the patient self-identified in Epic. Patients who with HIV were identified by visit diagnosis, billing diagnosis, or problem list entry of human immunodeficiency virus infection, human immunodeficiency virus positive, or human immunodeficiency virus antibody positive. To identify patients with dermatologic conditions, the SNOMED (London, UK) Clinical Terms concept disorder of skin was used. The comparison population was composed of all patients 18 years and older who presented to Johns Hopkins Hospitals between the same time period and who were HIV negative. See Table I for demographics of the groups.
Table I.
Demographics
| Characteristic | With HIV, % (N = 4679) | Without HIV, % (N = 346,950) |
|---|---|---|
| Sex | ||
| Male | 64.7 | 41.4 |
| Female | 35.3 | 58.6 |
| Race | ||
| African American | 69 | 24.6 |
| White | 26.1 | 62.6 |
| Other | 3.7 | 6.9 |
| Asian | 1 | 4.6 |
| American Indian/Alaskan | 0.7 | 0.3 |
| Unknown | 0.4 | 1.8 |
| Declined to answer | 0.2 | 0.3 |
| Native Hawaiian/Pacific | 0.1 | 0.1 |
| Islander | ||
| Treatment | ||
| Antiretroviral therapy | 88.7 | N/A |
N/A, Not applicable.
All HIV-related dermatologic conditions previously noted in the literature were searched using Epic. The burdens of 58 conditions were compared among patients with HIV and race-matched control individuals. Ten of the 58 skin conditions queried occurred in fewer than 0.1% of patients, and therefore odds ratios (ORs) were not calculated. Significance was assessed by using the chi-square test, and a Bonferroni correction was performed to control for multiple hypothesis testing, setting the P value for significance at P < .0009. The 95% confidence intervals (CIs) were calculated with the Woolf method.11 All analyses were conducted with Stata 15.0 (StataCorp, College Park, TX).
RESULTS
Between July 14, 2013, and July 14, 2018, 346 950 patients without and 4679 patients with HIV (≥18 years old) were seen at Johns Hopkins Hospitals. More than half (58.6%) of the control patients were women, whereas 35.3% of the patients with HIV were women (Table I). In the population of patients with HIV, 26.1% were white and 69.0% were African American. A majority (88.7%) of patients with HIV were taking ART. All significant results hereafter met significance of P less than .0009.
Of the 48 skin conditions seen in more than 0.1% of patients, 13 were not significantly different between patients with HIV and control individuals. Overall, patients with HIV had increased odds of having 29 of the 48 (60.4%) dermatologic diagnoses queried. The most common skin conditions in patients with HIV infection were atopic dermatitis (18.2%), verruca vulgaris (16.8%), herpes simplex (14.5%), cellulitis (14.4%), and dermatophytosis (11.7%).
Patients with HIV were more than 135 times more likely to have Kaposi sarcoma than matched control individuals (OR, 135.54; 95% CI, 91.99–199.71). Many of the dermatologic conditions for which patients with HIV were at increased risk were infectious conditions, inflammatory conditions, and adverse drug reactions (Fig 1).
Fig 1.
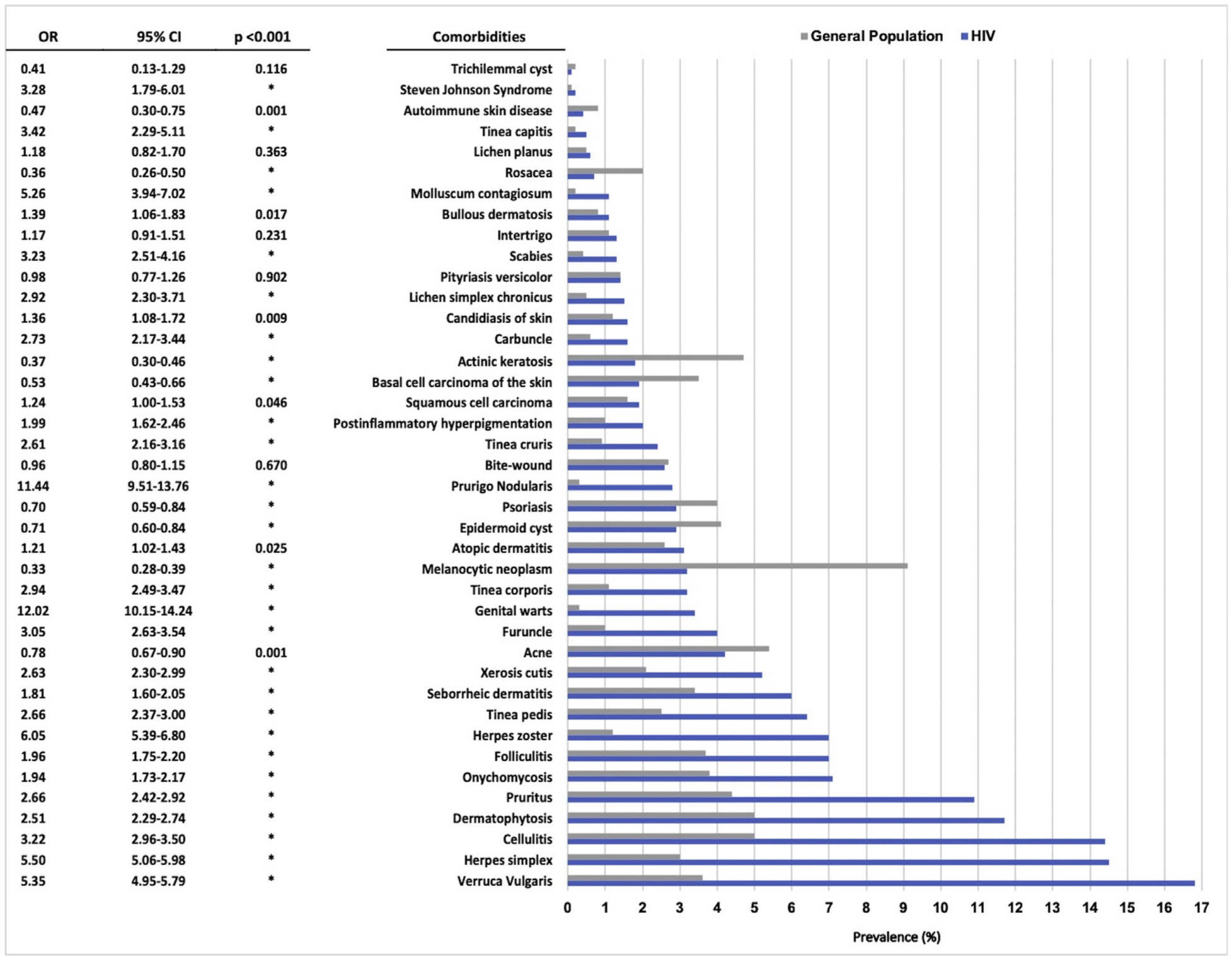
Association of dermatologic conditions with HIV infection. Prevalence of dermatoses in patients with HIV compared with patients without HIV in the Johns Hopkins Hospital population, corrected for race. Odds ratios and 95% confidence intervals for each condition are tabulated on the right.
When stratified by race, there appeared to be effect modification by race. Among African American patients with HIV infections, the most common skin conditions were verruca vulgaris (16.7%), herpes simplex (14.3%), cellulitis (13.8%), dermatophytosis (13.3%), and pruritus (12.6%). The most common dermatoses in African American patients without HIV were acne (7.7%), dermatophytosis (7.5%), pruritus (6.8%), onychomycosis (5.9%), and folliculitis (5.9%). African American patients with HIV had increased risk of having a number of the same dermatoses as the overall patient population with HIV, including Kaposi sarcoma (OR, 134.11; 95% CI, 62.82–286.30) (Table II). However, African American patients with HIV had a greater risk of oral hairy leukoplakia (OR, 64.49; 95% CI, 12.55–333.57), herpes zoster (OR, 9.27; 95% CI, 7.97–10.77), prurigo nodularis (OR, 8.80; 95% CI, 7.16–10.81), and squamous cell carcinoma (OR, 5.72; 95% CI, 4.12–7.94) compared with control individuals. Among African American patients, HIV infection had a positive effect on the likelihood of having 23 of 45 (51%) skin conditions.
Table II.
African American patients with HIV and various comorbid conditions compared with patients in the general population who were seen at JHH over the past 5 years*
| Conditions | With HIV, n (%) | Without HIV, n (%) | p | OR (95% CI) |
|---|---|---|---|---|
| Neoplastic conditions | ||||
| Kaposi sarcoma | 41 (1.3) | 8 | † | 134.11 (62.82–286.30) |
| Squamous cell carcinoma | 44 (1.4) | 201 (0.2) | † | 5.72 (4.12–7.94) |
| Infectious conditions | ||||
| Oral hairy leukoplakia | 5 (0.2) | 2 | † | 64.69 (12.55–333.57) |
| Genital warts | 124 (3.8) | 327 (0.4) | † | 10.15 (8.23–12.52) |
| Herpes zoster | 241 (7.5) | 720 (0.9) | † | 9.27 (7.97–10.77) |
| Herpes simplex | 463 (14.3) | 3273 (3.9) | † | 4.10 (3.69–4.55) |
| Verruca vulgaris | 540 (16.7) | 2463 (3.0) | † | 6.60 (5.97–7.30) |
| Molluscum | 35 (1.1) | 217 (0.3) | † | 4.20 (2.94–6.02) |
| Tinea capitis | ns | |||
| Scabies | 48 (1.5) | 658 (0.8) | † | 1.90 (1.41–2.55) |
| Cellulitis | 446 (13.8) | 4057 (4.9) | † | 3.14 (2.82–3.48) |
| Furuncle | 141 (4.4) | 2156 (2.6) | † | 1.72 (1.45–2.05) |
| Tinea corporis | 109 (3.4) | 1269 (1.5) | † | 2.26 (1.85–2.76) |
| Carbuncle | ns | |||
| Tinea pedis | 245 (7.6) | 3481 (4.2) | † | 1.89 (1.65–2.16) |
| Tinea cruris | 82 (2.5) | 849 (1.0) | † | 2.53 (2.01–3.19) |
| Dermatophytosis | 428 (13.3) | 6275 (7.5) | † | 1.88 (1.69–2.09) |
| Folliculitis | ns | |||
| Onychomycosis | 248 (7.7) | 4931 (5.9) | † | 1.32 (1.16–1.51) |
| Inflammatory conditions | ||||
| Prurigo nodularis | 124 (3.8) | 377 (0.5) | † | 8.80 (7.16–10.81) |
| Lichen simplex chronicus | 59 (1.8) | 685 (0.8) | † | 2.25 (1.72–2.94) |
| Pruritus | 408 (12.6) | 5653 (6.8) | † | 1.99 (1.79–2.22) |
| Xerosis cutis | 195 (6.0) | 2523 (3.0) | † | 2.06 (1.77–2.39) |
| Postinflammatory hyperpigmentation | ns | |||
| Seborrheic dermatitis | 202 (6.3) | 3070 (3.7) | † | 1.75 (1.51–2.02) |
| Atopic dermatitis | ||||
| Bullous dermatosis | 49 (1.5) | 711 (0.9) | † | 1.79 (1.34–2.40) |
| Drug reactions | ||||
| TEN | ns | |||
| SJS | ns |
CI, Confidence interval; JHH, Johns Hopkins Hospital; ns, not significant; OR, odds ratio.
Data are for all African American patients 18 years or older, including 3228 patients with HIV and 83 405 patients in the general population.
P < .0009.
Among white patients with HIV, verruca vulgaris (17.3%), cellulitis (16.7%), herpes simplex (15.1%), melanocytic neoplasms (9.4%), and dermatophytosis (8.4%) were the 5 most common skin conditions (Table III). Among white patients without HIV, melanocytic neoplasms (12.8%), actinic keratosis (7.1%), cellulitis (5.4%), basal cell carcinomas (5.4%), and psoriasis (5.3%) were most common. As seen with the overall patient population with HIV and the African American patients with HIV, white patients with HIV were at greatest increased risk of Kaposi sarcoma (OR, 198.34; 95% CI, 114.78–342.74). White patients with HIV were also more likely than control individuals to have genital warts (OR, 9.66; 95% CI, 6.62–14.09), herpes simplex (OR, 6.20; 95% CI, 5.29–7.27) and tinea capitis (OR, 5.97; 95% CI, 2.44–14.57). Overall, 20 of 42 (47.6%) skin conditions were more likely to be found in white patients with HIV than white patients without HIV.
Table III.
White patients 18 years and older with HIV and various comorbid conditions compared with patients in the general population who were seen at JHH over the past 5 years*
| Conditions | With HIV, n (%) | Without HIV, n (%) | p | OR (95% CI) |
|---|---|---|---|---|
| Neoplastic conditions | ||||
| Kaposi sarcoma | 27 (2.2) | 25 | † | 198.34 (114.78–342.74) |
| Squamous cell carcinoma | 43 (3.5) | 4991 (2.3) | ns | 1.57 (1.15–2.13) |
| Infectious conditions | ||||
| Oral hairy leukoplakia | 0 | 1 | ns | N/A |
| Genital warts | 29 (2.4) | 551 (0.3) | † | 9.66 (6.62–14.09) |
| Herpes zoster | 75 (6.2) | 3093 (1.4) | † | 4.58 (3.61–5.79) |
| Herpes simplex | 184 (15.1) | 6101 (2.8) | † | 6.20 (5.29–7.27) |
| Verruca vulgaris | 211 (17.3) | 8723 (4.0) | † | 5.04 (4.34–5.86) |
| Molluscum | 9 (0.7) | 410 (0.2) | † | 3.96 (2.04–7.69) |
| Tinea capitis | 5 (0.4) | 151 (0.1) | † | 5.97 (2.44–14.57) |
| Scabies | ns | |||
| Cellulitis | 203 (16.7) | 11 813 (5.4) | † | 3.50 (3.01–4.08) |
| Furuncle | 42 (3.4) | 2109 (1.0) | † | 3.67 (2.69–5.01) |
| Tinea corporis | 32 (2.6) | 2165 (1.0) | † | 2.70 (1.90–3.84) |
| Carbuncle | ns | |||
| Tinea pedis | 50 (4.1) | 4156 (1.9) | † | 2.21 (1.66–2.94) |
| Tinea cruris | 25 (2.1) | 2036 (0.9) | † | 2.23 (1.50–3.32) |
| Dermatophytosis | 103 (8.4) | 9072 (4.1) | † | 2.14 (1.74–2.62) |
| Folliculitis | 82 (6.7) | 6541 (3.0) | † | 2.34 (1.87–2.93) |
| Onychomycosis | 66 (5.4) | 7104 (3.2) | † | 1.71 (1.33–2.19) |
| Inflammatory conditions | ||||
| Prurigo nodularis | 9 (0.7) | 413 (0.2) | † | 3.94 (2.03–7.64) |
| Lichen simplex chronicus | ns | |||
| Pruritus | 80 (6.6) | 7295 (3.3) | † | 2.04 (1.62–2.56) |
| Xerosis cutis | 43 (3.5) | 3761 (1.7) | † | 2.09 (1.54–2.84) |
| Postinflammatory hyperpigmentation | ns | |||
| Seborrheic dermatitis | 65 (5.3) | 7204 (3.3) | † | 1.66 (1.29–2.13) |
| Atopic dermatitis | ns | |||
| Bullous dermatosis | ns | |||
| Drug reactions | ||||
| TEN | ns | |||
| SJS | ns |
CI, confidence interval; JHH, Johns Hopkins Hospital; N/A, not applicable; ns, not significant; OR, odds ratio.
Data are for all white patients 18 years or older, including 1219 patients with HIV and 218 935 patients in the general population.
P < .0009.
DISCUSSION
In this study, we show that patients with HIV are at a significantly increased risk of several dermatologic conditions, primarily of infectious, neoplastic, and inflammatory origins. Conditions found more often in patients with HIV were viral, bacterial, and fungal infectious diseases, suggesting aberrations in the immune system despite adequate HIV treatment. These included genital warts, herpes simplex, herpes zoster, verruca vulgaris, tinea infections, and molluscum contagiosum. Although basal cell carcinoma is more common in white patients with HIV, this condition was less common in our overall population with HIV because of racial differences between our patient and control cohorts. We did find a significantly increased risk of squamous cell carcinoma in African American patients with HIV compared with race-matched control individuals, a finding that deserves further study. More than half of the squamous cell carcinomas in this patient population were not anogenital. This finding may be due to aberrant function of the immune system despite adequate viral suppression.
Significant racial differences in the prevalence and risk of dermatologic conditions in patients with HIV were found (Table IV). To our knowledge, this is 1 of the first studies to look at racial differences in dermatologic conditions in patients with HIV treated with ART. Most notably, African American patients with HIV had an increased likelihood of having inflammatory, pruritic skin conditions compared with control individuals and with white individuals. In particular, black patients with HIV were nearly twice as predisposed to pruritus overall and also had a higher prevalence of lichen simplex chronicus and prurigo nodularis, which is supported by our previous findings.12–14 One hypothesis as to why patients with HIV are at an increased risk of pruritic conditions is the possibility that these patients may still have increased levels of certain T helper type 2 cytokines, despite ART treatment, which may promote a pruritic response.15,16
Table IV.
Black versus white patients with HIV with various dermatologic conditions within the population of patients seen at JHH over the past 5 years*
| Conditions | Black Patients With HIV, n (%) | White Patients With HIV, n (%) | p |
|---|---|---|---|
| Neoplastic conditions | |||
| Kaposi sarcoma | 41 (1.3) | 27 (2.2) | .022 |
| Squamous cell carcinoma | 44 (1.4) | 43 (3.5) | <.001 |
| Infectious conditions | |||
| Oral hairy leukoplakia | 5 (0.2) | 0 | N/A |
| Genital warts | 124 (3.8) | 29 (2.4) | .017 |
| Herpes zoster | 241 (7.5) | 75 (6.2) | .128 |
| Herpes simplex | 463 (14.3) | 184 (15.1) | .526 |
| Verruca vulgaris | 540 (16.7) | 211 (17.3) | .645 |
| Molluscum | 35 (1.1) | 9 (0.7) | .298 |
| Tinea capitis | 20 (0.6) | 5 (0.4) | .405 |
| Scabies | 48 (1.5) | 11 (0.9) | .129 |
| Cellulitis | 446 (13.8) | 203 (16.7) | .017 |
| Furuncle | 141 (4.4) | 42 (3.4) | .167 |
| Tinea corporis | 109 (3.4) | 32 (2.6) | .202 |
| Carbuncle | 67 (2.1) | 9 (0.7) | .002 |
| Tinea pedis | 245 (7.6) | 50 (4.1) | <.001 |
| Tinea cruris | 82 (2.5) | 25 (2.1) | .342 |
| Dermatophytosis | 428 (13.3) | 103 (8.4) | <.001 |
| Folliculitis | 240 (7.4) | 82 (6.7) | .416 |
| Onychomycosis | 248 (7.7) | 66 (5.4) | .008 |
| Inflammatory conditions | |||
| Prurigo nodularis | 124 (3.8) | 9 (0.7) | <.001 |
| Lichen simplex chronicus | 59 (1.8) | 9 (0.7) | .008 |
| Pruritus | 408 (12.6) | 80 (6.6) | <.001 |
| Xerosis cutis | 195 (6.0) | 43 (3.5) | .001 |
| Postinflammatory hyperpigmentation | 86 (2.7) | 3 (0.2) | <.001 |
| Seborrheic dermatitis | 202 (6.3) | 65 (5.3) | .247 |
| Atopic dermatitis | 127 (3.9) | 13 (1.1) | <.001 |
| Bullous dermatosis | 49 (1.5) | 3 (0.2) | <.001 |
| Drug reactions | |||
| TEN | 2 (0.1) | 0 | N/A |
| SJS | 7 (0.2) | 1 (0.1) | .344 |
JHH, Johns Hopkins Hospital; N/A, not applicable; SJS, Stevens-Johnson syndrome; TEN, toxic epidermal necrolysis.
Data are for all black or white patients 18 years or older, including 3228 black patients with HIV and 1219 white patients with HIV.
Limitations of this study include inability to determine causality and detection bias in patients with HIV infection, who may have more thorough and frequent clinician visits and physical examinations than the general population. Additionally, because these data were collected from the entire hospital system, patient dermatologic conditions may not have been well documented unless the patient was seen by a dermatologist. Baseline demographics are also different between the groups due to the population that the hospital serves. Because of the anonymized data collection method, individual patient CD4 counts and viral loads were not available. Therefore, we do not have certainty of patient adherence to ART. We were unable to stratify patients by sex or age based on the software tool used for this study; it is possible that data regarding age-related skin conditions may be skewed because of this. Finally, the majority of patients captured in this study were either African American or white, with low percentages of other ethnic and racial groups.
In the age of early and suppressive ART treatment for HIV, individuals with HIV infection have increased survival and are more likely to present with comorbid skin conditions. Greater awareness is needed for the detection and management of commonly associated dermatologic conditions in this patient population, particularly with regard to racial differences.17 Future studies may investigate why black patients with HIV tend to have greater prevalence of inflammatory, pruritic skin diseases than white patients with HIV.
CAPSULE SUMMARY.
In the era of highly active antiretroviral therapy, individuals with HIV commonly present with chronic diseases.
Individuals with HIV have elevated risk of many infectious, inflammatory, and neoplastic dermatologic conditions, some of which are affected by race. Awareness of these conditions is important when caring for patients with HIV.
Funding sources:
None.
Abbreviations used:
- ART
antiretroviral therapy
- CI
confidence interval
- OR
odds ratio
Footnotes
Disclosure: Dr Kwatra is an advisory board member for Menlo and Trevi Therapeutics and has grant funding from Kiniksa Pharmaceuticals. Dr Sewon Kang is an advisory board member of Almirall, Menlo, Sun Pharma, and Unilever. Drs Bender and Ständer, Ms Tang, and Ms Khanna have no conflicts of interest to declare.
IRB approval status: Waived because only anonymous aggregate-level data counts were used.
REFERENCES
- 1.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance datadUnited States and 6 dependent areas, 2016. HIV Surveillance Supplemental Report. 2018;23(4). Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-23-4.pdf. [Google Scholar]
- 2.Cockerell CJ. Human immunodeficiency virus infection and the skin: a crucial interface. Arch Intern Med. 1991;151(7):1295–1303. [PubMed] [Google Scholar]
- 3.Hammer SM, Katzenstein DA, Hughes MD, et al. A trial comparing nucleoside monotherapy with combination therapy in HIV-infected adults with CD4 cell counts from 200 to 500 per cubic millimeter. New Engl J Med. 1996;335(15):1081–1090. [DOI] [PubMed] [Google Scholar]
- 4.Maurer TA. Dermatologic manifestations of HIV infection. Top HIV Med. 2005;13(5):149–154. [PubMed] [Google Scholar]
- 5.Zancanaro PC, McGirt LY, Mamelak AJ, Nguyen RH, Martins CR. Cutaneous manifestations of HIV in the era of highly active antiretroviral therapy: an institutional urban clinic experience. J Am Acad Dermatol. 2006;54(4):581–588. [DOI] [PubMed] [Google Scholar]
- 6.Dlova NC, Mosam A. Inflammatory noninfectious dermatoses of HIV. Dermatol Clin. 2006;24(4):439–448. [DOI] [PubMed] [Google Scholar]
- 7.Khambaty MM, Hsu SS. Dermatology of the patient with HIV. Emerg Med Clin North Am. 2010;28(2):355–368. [DOI] [PubMed] [Google Scholar]
- 8.Tan J, Pina A, Borges-Costa J. Skin diseases in the era of highly active antiretroviral therapy: a retrospective study of 534 patients. J Int Assoc Provid AIDS Care. 2018;17: 2325957417752255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Günthard HF, Saag MS, Benson CA, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2016 recommendations of the International Antiviral SocietyeUSA panel. JAMA. 2016;316(2):191–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altman K, Vanness E, Westergaard RP. Cutaneous manifestations of human immunodeficiency virus: a clinical update. Curr Infect Dis Rep. 2015;17(3):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Woolf B On estimating the relation between blood group and disease. Ann Hum Genet. 1955;19(4):251–253. [DOI] [PubMed] [Google Scholar]
- 12.Boozalis E, Tang O, Patel S, et al. Ethnic differences and comorbidities of 909 prurigo nodularis patients. J Am Acad Dermatol. 2018;79(4):714–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whang KA, Kang S, Kwatra SG. Inpatient burden of prurigo nodularis in the United States. Medicines. 2019;6(3):88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang AH, Canner JK, Khanna R, Kang S, Kwatra SG. Real-world prevalence of prurigo nodularis and burden of associated diseases. J Invest Dermatol. 2020;140(2):480–483.e4. [DOI] [PubMed] [Google Scholar]
- 15.Shebl FM, Yu K, Landgren O, Goedert JJ, Rabkin CS. Increased levels of circulating cytokines with HIV-related immunosuppression. AIDS res Hum retroviruses. 2012;28(8): 809–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ständer S, Weisshaar E, Raap U. Emerging drugs for the treatment of pruritus. Expert Opin Emerg Drugs. 2015;20(3): 515–521. [DOI] [PubMed] [Google Scholar]
- 17.Paul S, Evans R, Maurer T, Muhe LM, Freeman EE. Treatment of dermatological conditions associated with HIV/AIDS: the scarcity of guidance on a global scale. AIDS Res Treat. 2016; 2016:3272483. [DOI] [PMC free article] [PubMed] [Google Scholar]


