Abstract
The aim of this paper is to present our experience with intraoral approach for submandibular gland excision in terms of effectiveness and safety in patients with chronic sialadenitis. This is a prospective study carried out from November, 2016 to April, 2018 analyzing 13 patients of chronic sialadenitis. The indication of intraoral approach was either failed attempt to remove the stone endoscopically, chronic sialadenitis or benign tumor. The surgical triangle was used as the landmark for hilar area and gland was dissected close to the capsule and removed via intraoral incision and preserving the sublingual gland. We were successfully able to remove the submandibular gland via intraoral approach in 10 cases. Two patients had to undergo transcervical gland excision and one patient refused for transcervical approach. Intraoral excision of submandibular gland is a safe and viable approach to be utilized in carefully selected patients. The major advantages being avoidance of transcervical scar and of injury to marginal mandibular branch of facial nerve.
Keywords: Intraoral approach, Chronic sialadenitis, Transcervical, Submandibular gland
Introduction
The excision of submandibular gland is indicated for a number of conditions such as recurrent sialadenitis, sialolithiasis, neoplasms and rarely sialorrhoea [1]. The submandibular gland excision is preferred traditionally by transcervical approach mostly using a natural skin crease incision as it gives easy direct access to the gland. This is generally a safe procedure with low morbidity but some complications such as aesthetic scarring and nerve injury can occur [2]. The postoperative scar is visible and prominent in the exposed part of the neck, which can be cosmetically unappealing, particularly in young patients. The scar may sometimes become worse with hypertrophy or keloid formation. The neurological complications in the transcervical approach were observed after surgery in several studies. The marginal mandibular branch of the facial nerve is the most commonly injured/affected (1–7.7%) followed by hypoglossal (2.9%) and lingual (1.4%) nerves [3–5]. But these nerves are rarely injured in the hands of experienced surgeons. Also, submandibular gland excision by transcervical approach may leave behind the pathology like anteriorly placed stones, strictures etc.
In the literature review, since Downtown and Qvist [6] first reported an intraoral approach for chronic sialadenitis of the submandibular gland in 1960, no further reports have been found until Hong and Kim [7] reported in 2000 and later by Smith et al. [8]. The intraoral approach avoids a cervical incision and also avoids dissection in close proximity to the marginal mandibular branch of facial nerve. The anatomic association of the submandibular gland, the lingual nerve, Wharton’s duct, and the hypoglossal nerve is highly variable at different points in the oral cavity. Due to difficulty in visualization of this anatomy, an transcervical approach has been advocated by most and this approach has been the standard of care till date. However, with the advent of better endoscopic tools and preference of patients towards minimal incision approach, intraoral approach has gained popularity as safe and effective technique [9].
But intraoral approach is not without problems as it may cause lingual nerve injury and limitation of tongue movements. In addition, intraoral dissection is difficult in chronically inflamed glands with severe adhesions to surrounding tissue, and conversion to transcervical approach may need to be made simultaneously. Identification and careful control of facial vessels at the posterior pole is also a key portion of the case.
In this article, we present our technique of intraoral submandibular gland excision using a smaller incision and preserving the sublingual gland. We started doing removal of submandibular ductal hilar stones by intraoral approach using the lateral technique described by Park [10] and then with our success in such cases, we further extended our technique to remove the gland in failed such cases and chronic sialadenitis cases. Here we present the first 13 cases of intraoral submandibular gland excision done by the technique we advocate.
Materials and Methods
From November 2016 till April 2018, we operated 13 patients of chronic sialadenitis via intraoral approach. The surgical options, all possible complications, and potential risks and benefits were explained to each patient and written informed consent to their participation was obtained. All the patients were evaluated by preoperative computed tomography and one of the patients had prior history of submandibular gland surgery.
Data was collected on personal and clinical details, histopathological diagnosis, duration of surgery, length of hospital stay, postoperative complications and cosmesis.
Under general anaesthesia, after transnasal intubation and proper oral preparation, the submandibular papilla was identified and tongue retracted to opposite side. The incision was made through the mucosa of the lateral floor of the mouth 2 cm away from the mandibular arch taking a maximal curvilinear incision (opposite to the first premolar till the last molar tooth) (Fig. 1). This incision was the extension of the incision which we used for removal of hilar stones. After doing series of cases of hilar stones, we became familiar with the hilar area and directly exposed firstly this area using the “surgical triangle” as landmark, without dissecting or removing the sublingual gland. The boundary of the surgical triangle is delineated by the lingual nerve, the medial border of the mandible, and the posterior border of the mylohyoid muscle. (10) Dissection was done using artery forceps and effort made to identify lingual nerve. In some cases, lingual nerve was found superficial and recognizable immediately after incision. In some cases, nerve was found quiet deep overshadowed by posterior prolongation of sublingual gland and sometimes by submandibular gland tissue itself. Lingual nerve is identified (Fig. 2) and dissected free from its attachment to the SMG, duct and sharply dividing the attachment to submandibular ganglion. Wharton’s duct was then carefully freed from the lingual nerve and followed to the deep lobe of the gland. The gland was then dissected all through the undersurface of the mylohyoid and from its attachment to genioglossus and hyoglossus muscle and it was aided by external digital pressure applied beneath the submandibular triangle to push the gland into the surgical field. The posterior dissection was done at the last to avoid injury to the facial vessels which get lifted off with the capsule of the gland. A cuff of mucosa on the gingival side is preserved to allow for tension free closure and to prevent restriction of tongue movement due to scar contracture. Because of the narrow surgical field, the dissection and delivery of submandibular gland is not simple. The good exposure and external pressure are important. Occasionally, inflammatory adhesions necessitate a more difficult and careful dissection. The gland was gripped with long tissue forceps or tonsil hemostatic forceps or babecocks forceps and dissected using a Gywnne Evans tonsillar dissector and pulled up through the incision (Fig. 3).
Fig. 1.
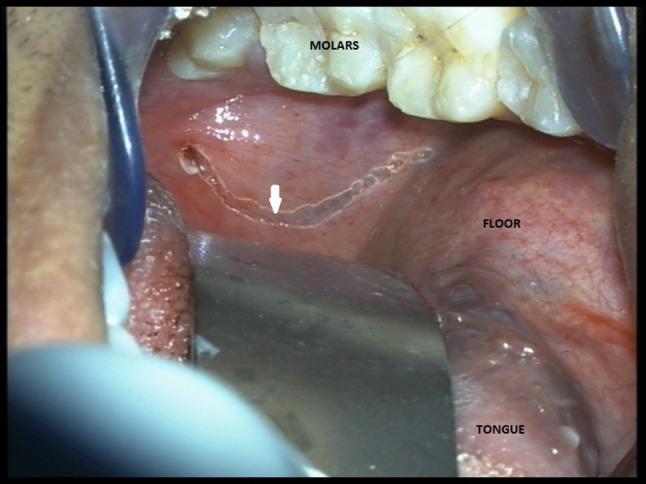
Intraoral incision with maximum curvilinear shape (white arrow)
Fig. 2.
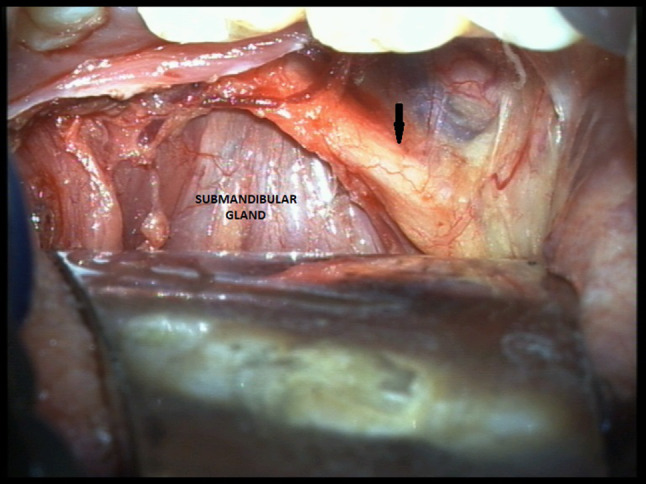
Lingual nerve identified (black arrow)
Fig. 3.

Submandibular gland removed via intraoral approach for obstructive hilar stone
The facial artery and its branches should be dissected and freed carefully at the posterior pole of the gland and if needed ligated. The hypoglossal nerve is usually found inferior and lateral to the gland. The wound is carefully inspected for hemostasis and incised mucosa of the floor of mouth was sutured back loosely in a single layer with interrupted absorbable suture without drain. Injectable antibiotic given for 48 h followed by oral antibiotics for a total of 7 days along with betadiene mouth rinses.
Results
Of the 13 cases included in this study, there were 8 female and 5 male patients. The sex ratio was 5:8 (male:female). The age of the patients ranged from 10 to 62 years with a mean age of 25.4 years. Five of thirteen had previously been treated with antibiotics for acute sialadenitis episodes. The average length of stay in the hospital was 7.9 days.
The mean surgical time of the first 5 cases was 2 h 20 min, that of next 4 cases was 1 h 45 min and that of the last case was 45 min. With increasing surgical experiences, the surgical time was getting shorter.
Ten out of thirteen operations were completed successfully using the intraoral approach without any need for transcervical incision. Four patients presented with chronic sialadenitis, three with pleomorphic adenoma and three having obstructing sialoliths which were sialendoscopic removal failure.
The most common early post operative complication which was observed in maximum number of patients (80%) was temporary lingual nerve paresis leading to paraesthesia of tongue. This was due to the stretching and retraction of the nerve while dissecting the gland. This was temporary and resolved completely in 1–2 months duration. Two patients experienced restriction of tongue movement which resolved completely in 3–4 weeks. The scar contracture causes this asymmetric movements of the tongue. One patient had infection at the incision site, floor of mouth breakdown and delay in healing. Injectable antibiotics were given for 1 week duration with good oral hygiene and infection resolved with conservative measures, patient had hospital stay of 12 days. One cases was suspected of having hypoglossal nerve paresis which resolved in 1 month. No permanent sequelae of any nerve injury was noted. All the patients were satisfied.
Out of the three failed cases, one had oral intubation which restricted the surgical field and the case was abandoned as the patient hadn’t given consent for transcervical approach. After this case, we resorted to only nasal intubation. Other two cases had extensive fibrosis due to chronic sialadenitis and from a previous procedure, both cases were converted to transcervical approach in the same sitting.
Discussion
Numerous diseases of submandibular gland such as chronic inflammatory disease, benign tumors, sialorrhoea among others require excision of submandibular gland. The transcervical approach is widely accepted and relatively simple, and the salivary gland tissue could be removed without difficulty and this is still the most prevalent technique with surgeons worldwide. However, this approach has frequently been associated with neurological complications including the facial symmetry and result in an unsightly keloid or hypertrophic scar. Patients have become increasing concerned about the safety and effectiveness of techniques in addition to cosmetic appearance. Even a small postoperative scar on the visible area of the neck is an unacceptable sequel for most patients, especially younger patients and women, and can influence their quality of life. This plays a part in the patient’s decision, and evidence suggests that an increasing number of patients are opting for procedures with least adverse cosmetic outcomes and this has lead to development of various techniques to reduce the risk of visible scar and with equal safety and effectiveness.
The intraoral approach has been described since 1960 by Downtown and Qvist [6] however, with better endoscopic equipment, improved tools, and increased surgeon familiarity with the intraoral anatomy, the intraoral approach gained popularity. Hong et al. [7] later used this technique with success in 31 patients. Smith et al. [8] reported a similar technique in the plastic surgery literature, whereas Guerrissi et al. [11] described the addition of endoscopic assisted method to improve exposure. The resurgence seems probably because of more familiarity with the area due to sialendoscopes and overall preference of the patient for scarless surgery.
We have modified the technique using our own experience. We started removal of hilar stones using the lateral approach described by Park et al. [10] then as we became familiar with the intraoral anatomy and had success in a series of such cases, we extended the technique for removing submandibular gland. In the present approach, we incise the mucosa on the floor of mouth only in the posterior part leaving the anterior half intact as we do not remove the sublingual gland. This is a variation to the technique used by other surgeons for intraoral approach as majority give incision from the papilla till the hilar area and remove the sublingual gland for better visualization of the submandibular gland. We however leave the sublingual gland in situ and by careful meticulous retraction, get an appropriate surgical exposure. The advantage of this modification lies in the fact that we have not encountered any postoperative ranula or residual cyst. These result due to injury to sublingual ducts or gland [12, 13].
From the risk benefit standpoint, the intraoral approach offers several distinct advantages. First, there are no transcervical incisions or scar, which would obviously be preferable for the patient. This also limits the possibility of orocutaneous fistula in individuals who have been previously irradiated. Secondly, the risk to marginal mandibular branch of facial nerve is minimized, as its position in the subplatysmal plane will remain untouched in the intraoral technique. Also, incidence of injury to hypoglossal nerve is high in this technique as compared to intraoral technique. In intraoral technique, the limitation of tongue movement was due to scar contracture and tongue and floor of mouth edema which was completely resolved with no permanent damage. Finally, no drain needs to be placed as passive efflux of blood can occur through the intraoral incision without much notice to the patient.
However, there are few drawbacks of this technique as well. Selection of the proper patient with the appropriate pathology and adequate jaw opening, mandibular size, and tongue mobility provides the highest likelihood for a successful intraoral operation [14]. Also, although anatomic relationships remain the same, the change in vantage point could potentially cause some confusion if the anatomy is not completely understood. Third, due to stretching and manipulation of the lingual nerve, temporary paresis and paraesthesia of tongue is more frequent in this approach. Although no permanent sequelae seen. This can further be reduced by avoiding the complete skeletonisation of the nerve as we have observed in the later cases where we did not skeletonise the entire length of the nerve. Finally, the control of vascular pole of the gland is more challenging since the facial vessels are located at posterior aspect of the gland, but there was no hemostatic complication in our series due to meticulous dissection and leaving the gland capsule intact.
The intraoral approach may offer more chances for contamination from oral cavity to submandibular space. However, with proper preoperative preparation and maintaining good oral hygiene, an infection is preventable [13].
In the three cases of pleomorphic adenoma, we noticed that there was spillage of tumor in the submandibular space due to injury by instrumentation so we donot advocate this technique for tumor cases. This is in contrast to tumors of parotid gland which are eccentrically placed and not covered with capsule. Also, malignant and likely malignant pathologies shouldn’t be risked with this technique.
Conclusion
Intraoral excision of submandibular gland is a safe and viable approach to be utilized in carefully selected patients. The major advantages being avoidance of transcervical scar and of injury to marginal mandibular branch of facial nerve. With the modification as we propose, the incision can be limited and also sublingual gland will be preserved resulting in fewer complications. However, due to the different intraoral surgical anatomy, there is a learning curve for this technique. And this technique can be safely used for chronic sialadenitis cases without difficulty.
Funding
None.
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and Animal Rights
This article does not contain any study with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from the participant included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Beahrs OH, Woolner LB. Surgical treatment of diseases of salivary gland. J Oral Surg. 1969;27(2):119–128. [PubMed] [Google Scholar]
- 2.Berini-Aytes L, Gay-Escoda C. Morbidity associated with removal of the submandibular gland. J Craniomaxillofac Surg. 1992;20(5):216–219. doi: 10.1016/S1010-5182(05)80318-X. [DOI] [PubMed] [Google Scholar]
- 3.Laskawi R, Ellies M, Argeble C, Schott A. Surgical management of benign tumors of the submandibular gland: a follow-up study. J Oral Maxillofac Surg. 1995;53(5):506–508. doi: 10.1016/0278-2391(95)90057-8. [DOI] [PubMed] [Google Scholar]
- 4.Goh YH, Sethi DS. Submandibular gland excision: a 5-year review. J Laryngol Otol. 1998;112(3):269–273. doi: 10.1017/S0022215100158323. [DOI] [PubMed] [Google Scholar]
- 5.Leonardo BA, Cosme GE. Morbidity associated with the removal of the submandibular gland. J Craniomaxillofac Surg. 1992;20:216–219. doi: 10.1016/S1010-5182(05)80318-X. [DOI] [PubMed] [Google Scholar]
- 6.Downton D, Qvist G. Intra-oral excision of the submandibular gland. Proc R Soc Med. 1960;53:543–544. doi: 10.1177/003591576005300713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hong KH, Kim YK. Intraoral removal of the submandibular gland: a new surgical approach. Otolaryngol Head Neck Surg. 2000;122:798–802. doi: 10.1016/S0194-5998(00)70004-0. [DOI] [PubMed] [Google Scholar]
- 8.Smith AD, Elahi MM, Kawamoto HK, Jr, Lorenz HP, Hedrick MH. Excision of the submandibular gland by an intraoral approach. Plast Reconstr Surg. 2000;105(6):2092–2095. doi: 10.1097/00006534-200005000-00027. [DOI] [PubMed] [Google Scholar]
- 9.Beahm DD, Peleaz L, Nuss DW, Schaitkin B, Sedlmayr JC, Rivera-Serrano CM, et al. Surgical approaches to the submandibular gland: a review of literature. Int J Surg. 2009;7:503–509. doi: 10.1016/j.ijsu.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Park HS, Pae SY, Kim KY, Chung SM, Kim HS. Intraoral removal of stones in the proximal submandibular duct: usefulness of a surgical landmark for the hilum. Laryngoscope. 2013;123:934–937. doi: 10.1002/lary.23825. [DOI] [PubMed] [Google Scholar]
- 11.Guerrissi J, Taborda G. Endoscopic excision of the submandibular gland by an intraoral approach. J Craniofacial Surg. 2001;12:299–303. doi: 10.1097/00001665-200105000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Goudal JY, Bertrand JC. Complications of surgical treatment for submandibular calculi. Rev Stomatol Chir Maxillofac. 1979;80:349–350. [PubMed] [Google Scholar]
- 13.Hong KH, Yang YS. Surgical results of the intraoral removal of the submandibular gland. Otolaryngol Head Neck Surg. 2008;139:530–534. doi: 10.1016/j.otohns.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Kauffman RM, Netterville JL, Burkey BB. Intraoral excision of the submandibular gland: techniques and results of nine cases. Laryngoscope. 2009;119:502–507. doi: 10.1002/lary.20029. [DOI] [PubMed] [Google Scholar]


