Abstract
This study shows accommodative accuracy and distance accommodation facility in myopic children do not play a role in myopia progression. In 144 subjects, the monocular distance accommodative facility (DAF) and continuous accommodative stimulus–response curves (ASRCs) were measured at the enrolment. Retrospective and prospective refraction with regard to the enrolment visit were obtained from the outpatient database system based on noncycloplegic subjective spherical equivalent refraction (SER). The rate of myopic progression at enrolment was the first derivative of the Gompertz function, which was fitted with each subject's longitudinal refractive error data, including at least four records of SER with an interval of more than 6 months between each visit. A mixed linear model for multilevel repeated-measures data was used to explore the associations between the rate of myopia progression and accommodative parameters. The mean rate of myopia progression at enrolment was -0.61 ± 0.31 D/y with a mean age of 12.27 ± 1.61 years. By adjusting for age and SER, it was shown that the myopic progression rate was not associated with the accommodative lag (F = 0.269, P = 0.604), accommodative lag area (F = 0.086, P = 0.354), slope of ASRC (F = 0.711, P = 0.399), and DAF (F = 0.619, P = 0.432).
Subject terms: Refractive errors, Paediatric research
Introduction
Myopia is the most common refractive error. The prevalence of myopia in young adolescents has increased substantially in recent decades, especially in East and Southeast Asia1–3. Rapid myopia progression might lead to high myopia with severe irreversible blinding ocular complications4, such as retinal detachment and glaucoma, affecting vision and quality of life. Although myopia has become a public health problem and has been studied for more than a century, the how or why of the onset and progression of myopia is unclear.
Retinal hyperopic defocus is regarded as a possible factor contributing to myopia and is considered the link between nearwork and myopia. Animal experiments5,6 have shown that the growth of the eye can be regulated by the sign of blur resulting from an additive optical lens. Hyperopic defocus induced by a negative lens accelerates axial length growth, while myopic defocus induced by a positive lens inhibits this growth. In humans, hyperopic defocus can be induced by accommodative lag caused by reduced accommodative response during nearwork. Thus, accommodative lag has been proposed to promote axial elongation7–9. Indeed, numerous streams of evidence have implied that accommodative lag is related to myopia. Accommodative lag has been reported to be higher in myopic individuals than in emmetropes9,10 at the same stimulus distance. Moreover, myopic children tend to read at a closer distance when compared to emmetropic children11, which may lead to increased lag of accommodation, as lag increases with accommodative demand12. Additionally, myopia progression in children was reported to be significantly greater with closer nearwork distances13,14 and slower with progressive addition lenses for children with higher lags of accommodation versus single-vision spectacles15. Therefore, it has been suggested that higher accommodative lag can induce faster eye growth in myopic children. Lan et al.16 conducted a longitudinal study of the association between myopia progression and accommodative lag at 33 cm in 62 myopic children (7–13 years). However, no association between accommodative lag and myopia progression was found, in accordance with the result of the CLEERE study17 on 592 myopic children. The lack of association may be due to accommodative stimuli adopted in previous studies. The reading distances of Chinese children have been shown to be very close, e.g., 16.3 ± 4.1 cm for Grade 2 for emmetropic children18, and highly task dependent19. Hence, the accommodative lag for a certain distance or stimulus (e.g., 3 D16,20 or 4 D17) need not be consistent with all reading conditions. This results in a lack of a relationship between accommodative lag and myopia in some studies but not in others. Another explanation can be that accommodative lag measurements used in prior studies were not sensitive enough. The area of the accommodative response function7, representative of the amount of accommodative response based on the linear regression of the accommodative stimulus–response function, was found to be highly related to myopia progression. Since accommodative lag is assumed to be a risk for myopia, the area of underaccommodation (the amount of accommodative lag) covering a range of stimuli might be a more sensitive index to predict myopia progression.
Other accommodative parameters have also been found to be associated with myopia. Reduced distance accommodative facility21,22 and shallower slope10 of the accommodative stimulus–response curve (ASRC) are more frequently observed in myopes than emmetropes. For their role in myopia progression, distance accommodative facility20 and the slope of ASRC had no significant effect23 on myopic young adults. However, to the best of our knowledge, no investigation has been conducted to assess the association between these accommodative parameters and myopia progression in children since accommodative characteristics were reported to change with age24–26.
The purpose of this investigation is to explore the relationship between different parameters of accommodation and myopia progression in Chinese myopic children.
Results
One hundred forty-four subjects meeting the inclusion criteria were enrolled in this study. Thirty-one of the 144 subjects were excluded from the analyses because of their poor fit with R2 (less than 0.90 for the Gompertz function; 21 subjects) or lack of longitudinal data (less than 2 years; 10 subjects). The remaining 113 myopic children, consisting of 61 males and 52 females, were analysed. Table 1 shows the mean and range of each variable at enrolment.
Table 1.
Mean and range of the variables at enrolment.
| Variables | Minimum | Maximum | Mean ± SD |
|---|---|---|---|
| Age (years) | 7.82 | 15.3 | 12.27 ± 1.61 |
| Sphere (D) | − 6 | − 0.75 | − 2.99 ± 1.08 |
| Cylinder (D) | − 1.5 | 0 | − 0.34 ± 0.4 |
| SER (D) | − 6.75 | − 0.75 | − 3.16 ± 1.13 |
| Myopia progression (D/y) | − 1.42 | 0 | − 0.61 ± 0.31 |
| DAF (cpm) | 2 | 45.5 | 18.29 ± 7.42 |
| Slope of ASRC | 0.81 | 1.2 | 1.02 ± 0.08 |
| ALA 0–6 (D2) | 3.25 | 11.85 | 6.84 ± 1.65 |
| Accommodative lag at 0 D (D) | − 0.97 | 0.49 | − 0.27 ± 0.3 |
| Accommodative lag at 1 D (D) | − 0.13 | 1.35 | 0.51 ± 0.27 |
| Accommodative lag at 2 D (D) | 0.42 | 1.9 | 1.02 ± 0.28 |
| Accommodative lag at 3 D (D) | 0.64 | 2.21 | 1.33 ± 0.3 |
| Accommodative lag at 4 D (D) | 0.75 | 2.37 | 1.51 ± 0.33 |
| Accommodative lag at 5 D (D) | 0.75 | 2.52 | 1.61 ± 0.36 |
| Accommodative lag at 6 D (D) | 0.68 | 2.91 | 1.70 ± 0.4 |
SER spherical equivalent refraction, DAF distance accommodative facility, slope of ASRC the steepest slope of the accommodative stimulus–response curve, ALA 0–6 the accommodative lag area between 0 and 6 D.
The longitudinal follow-up time, including retrospective and prospective visits, was 4.47 ± 1.33 years, ranging from 2.31 to 8.75 years. The Gompertz functions fit the refractive data well with a mean R2 value of 0.98 ± 0.02. The velocity of the refractive change in individual subjects at enrolment was the first derivative of the classic Gompertz function.
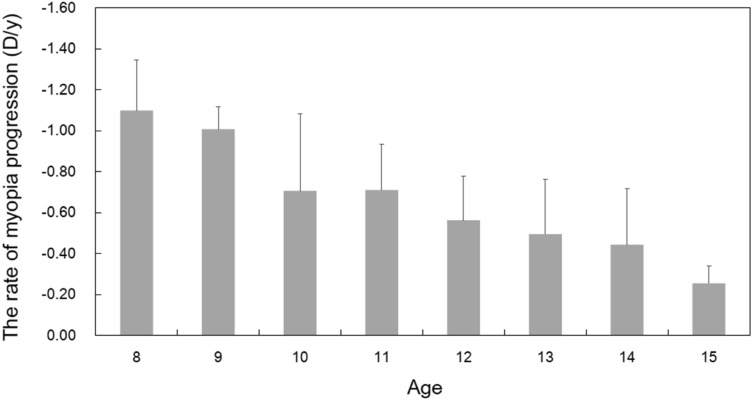
The regression model revealed that age and SER were related to the myopia progression rate (Table 2). Myopia progression was shown as a function of age in Fig. 1. The rate of myopia progression at enrolment was − 1.10 ± 0.25 D/y at age 8 and then decreased gradually, reaching − 0.25 ± 0.08 D at age 15. The mean rate of myopia progression was − 0.61 ± 0.31 D/y for 113 subjects with a mean age of 12.27 ± 1.61 years. SER was significantly associated with myopia progression (F = 8.067, P = 0.005). The positive coefficient of the model (Table 2) indicated that children with higher myopia refractive error was associated with faster myopia progression, increasing by 0.021 D with each dioptre of SER (95% coefficient interval [CI]: 0.007 to 0.036).
Table 2.
The coefficients of the mixed model regression analysis for myopia progression.
| Parameter | Estimate | 95% Confidence Interval | F | Sig | |
|---|---|---|---|---|---|
| Intercept | − 1.744 | − 2.022 | − 1.467 | 178.803 | < 0.001 |
| Age | 0.102 | 0.092 | 0.113 | 364.497 | < 0.001** |
| SER | 0.021 | 0.007 | 0.036 | 8.067 | 0.005* |
| Different levels of stimulus | 0.030 | 1.000 | |||
| Accommodative lag | − 0.017 | − 0.082 | 0.048 | 0.269 | 0.604 |
| ALA 0–6 (D2) | 0.007 | − 0.008 | 0.022 | 0.860 | 0.354 |
| Slope of ASRC | − 0.104 | − 0.344 | 0.137 | 0.711 | 0.399 |
| DAF | 0.001 | − 0.001 | 0.003 | 0.619 | 0.432 |
| Sex | 0.012 | − 0.020 | 0.044 | 0.519 | 0.471 |
SER spherical equivalent refraction, DAF distance accommodative facility, slope of ASRC the steepest slope of the accommodative stimulus–response curve, ALA 0–6 the accommodative lag area between 0 and 6 D.
Figure 1.
The rate of myopia progression at enrolment with age. The error bars represent the standard deviation.
The mixed model regression analysis showed that accommodative lag was not associated with the rate of myopia progression at enrolment (F = 0.269, P = 0.604) adjusted by age and SER. The negative coefficient from the model (Table 2) indicated that myopia progression was affected by only 0.017 D for every D of lag (95% coefficient interval [CI]: − 0.082 to 0.048). The mean value of the accommodative lag area between 0 and 6 D was 6.84 ± 1.65 D2, and there was no significant association between the area and myopia progression (F = 0.086, P = 0.354); the coefficient value was small, at 0.007 (95% coefficient interval [CI]: − 0.008 to 0.022). The largest slope of the ASRC was 1.02 ± 0.08 and was not significantly associated with myopia progression (F = 0.711, P = 0.399); the coefficient value was -0.104 (95% coefficient interval [CI]: − 0.344 to 0.137).The DAF was 18.29 ± 7.42 cpm and unrelated to myopia progression (F = 0.619, P = 0.432); the coefficient value was − 0.001 (95% coefficient interval [CI]: − 0.001 to 0.003).
Discussion
The purpose of present study was to investigate the association between accommodation and myopia progression of myopic children. It was found that myopia progression was not related to the accommodative lag at various proximities, accommodative lag area, slope of ASRC, or distance accommodative facility in enrolled subjects. The main outcome of our study was that although there was no significant association between accommodation and myopia progression, age and myopic refractive error were shown as predict factors.
In contrast to previous studies, we derived the myopia progression rate at enrolment from longitudinal datasets fitted with the Gompertz function. The high R2 value (mean value 0.98 ± 0.02) and low percentage of poor fit with R2 less than 0.90 (10.66% of subjects) supported that a double exponential function fits refractive data well during the myopization phase, in agreement with the findings of Thorn et al.27. The myopia progression rate decreased with age, which is consistent with the result of Donovan et al.28 for Asian children. The mean rate of myopia progression in our study (0.61 D) was slightly faster than the annual progression predicted by a quadratic equation at the same mean age in the study of Donovan et al. (0.48 D), probably due to the difference in calculation of the rate. Our result suggests that more attention should be given to younger myopes whose myopia progresses rapidly and who are more likely to become high myopes in later years. Myopia prevention strategies should therefore be started from an early age to decrease the prevalence of high myopia29.
The present study showed that children with higher levels of myopia were likely to have slightly faster progression, in accordance with previous studies14,30–32. It is possible that more relative hyperopic peripheral defocus associated with higher myopia33 leads to faster myopia progression34. In addition, a higher-order aberration35 in the more myopic eye might stimulate eye growth36.
For a few decades, accommodative lag has been considered a putative risk for the development of myopia. In this study, the accommodative response was measured using a Badal stimulator under which blur is the sole cue for accommodation. For a stimulus proximity of 4D, the average value of the lag of accommodation was 1.51 ± 0.33 D, comparable to the results of Berntsen et al.17 (1.51 ± 0.63 D) with similar accommodative testing conditions. The assumed relationship between accommodative lag at various proximities with myopia progression could not be identified in this study. Furthermore, the accommodative lag area between 0 and 6 D cannot predict myopia progression in our study. According to our data and in accordance with previous studies16,17, there is no clear evidence that accommodative lag is a risk for myopia progression, implying that the contribution of accommodation-induced hyperopic defocus in the development of myopia in myopic children may be negligible even with a high amount of defocus at a closer distance. One hypothesis explaining these results is that the mechanisms of myopia onset and myopia progression are different. Myopia progression is not regulated by accommodative lag in humans, despite the strong evidence that hyperopic defocus stimulated by optical lenses can induce myopia in animals. Lu et al.37 found that myopia developed rapidly within 2 days of negative-lens wear and slowly afterwards, then did not progress after 10 days in guinea pigs, supporting the hypothesis. Another possible explanation for this is that accommodative lag is a consequence of myopia38, rather than a cause. The negative result provides support for the observations that although the intensity of nearwork increases with age39, myopia progression does not increase with age. This finding also supports that multifocal lenses designed to reduce accommodative lag to retard myopia progression have a modest clinical significance40,41.
The slope of the ASRC in our study (1.02 ± 0.08) was steeper than that previously published by Gwiazda et al.10 (0.78) in myopic children. This could be because the steepest slope of the ASRC, instead of the gradient of the linear regression, was adopted in our study. However, the slope was higher than that for young adults (0.80) with the same method and calculation in our previous study42. This discrepancy may be due to a larger accommodative response in younger subjects24. The present study reveals that the slope of the ASRC is not linked to myopia progression in children, in agreement with the result of young adults23, although this slope was reduced in progressing myopes but not in stable myopes8. Hence, the gradient of accommodative response appears to be mainly an index that reflects the accuracy of accommodation but not a risk factor for myopia progression.
As an indicator of accommodative dynamics, DAF was found to be reduced both in myopic children21 and myopic young adults22 compared with emmetropes, possibly because of the lower accommodative response to negative lenses10 and the lower velocity of accommodation and disaccommodation43. Similar to Allen and O'Leary20, who studied young adults, we did not find any association between myopia progression and DAF. This result is also consistent with other research44,45 that found that visual training to improve accommodative dynamics failed to retard myopia progression, implying that accommodative dynamics are not a factor for myopia progression.
This study has several limitations. First, myopia progression in our sample was derived from retrospective data in the outpatient system, and the time intervals between visits were uneven. However, we calculated the rate of myopia progression at enrolment from the fitting curve, compensating for this shortcoming to a certain extent. Second, our study fitted the Gompertz function with subjective refractions instead of cycloplegic autorefraction, which is considered the gold standard for determining refractive status46,47. However, it would only have a negligible effect on the Gompertz fit and the results of the myopia progression rate. Moreover, it was reported that subjective refraction was comparable to cycloplegic refraction in myopes48. Third, no information about other known risk factors could contribute to myopia progression, such as the time of near work or outdoor activity. It would have been more convincing to combine different accommodative lags with the time of nearwork, which represents the accumulated effect of hyperopic defocus.
In summary, a key finding of the present study was that accommodative accuracy and distance accommodative facility in myopic children were not associated with myopia progression in our sample. Myopization is a complex, multifactorial process that involves factors other than accommodation.
Methods
One hundred forty-four children from the Primary Care Department of the Eye Hospital affiliated with Wenzhou Medical University were enrolled between August 2014 and September 2015. Subjects meeting the following criteria were recruited: available retrospective data for more than 6 months prior to the enrolment from the outpatient system; aged 8 to 15 years at the time of enrolment; spherical equivalent of more than − 0.75 D in each eye, astigmatism less than 2.00 D in either eye, anisometropia less than 1.00 D, monocular best visual acuity better than 0.1 of logMAR; no strabismus by cover test with distance-corrected spectacle; no progressive addition lens or contact lens wearing history; and no history of any ocular disease. The study conformed to the tenets of the Declaration of Helsinki and was approved by the Ethical Committee of the Eye Hospital affiliated with Wenzhou Medical University. Informed consent was obtained from the subjects and their legal guardian.
Procedure
The subjects were measured by following procedures on the enrolled day.
Refraction
Retinoscopy was performed before subjective refraction to exclude subjects with greater fluctuations in accommodation, or with more than 0.50D-discrepancy between retinoscopy and subjective refraction. Subjective refraction was performed according to the principle of "maximal positive lens maximal visual acuity" to avoid overcorrection. Data were collected by an experienced optometrist.
Distance accommodative facility (DAF)
DAF was measured for the right eye, which fixated at the central letter in a 3 × 3 array of 20/30 letters placed 4.5 m away, while the left eye was occluded. A − 2.00 D trial lens was placed in the trial frame in front of the eyes, which made the letters blurred for a short time, and then the letters became clear again. As soon as the letters were clear, the subject informed the examiner. The examiner then removed the lens, which made the letters blurred again for a short duration, and the subject informed the examiner as soon as the letters could be seen clearly again. A full cycle consisted of two phases, i.e., with and without − 2.00 D. The number of cycles completed in 1 min was recorded. The subjects were given a guidance before starting the measurements to ensure that they understood the procedures. One-minute breaking was required between guidance and measurement to avoid the aftereffect of accommodation.
ASRC measurements
The ASRC method was explained in a previous study42. The motorized Badal system consisted of a Badal lens with a power of + 5.75 D and a moving auxiliary lens with a power of + 3.33 D mounted on a Grand Seiko autorefractor (WAM-5500; Grand Seiko Co., Ltd., Japan) to produce a wide range of accommodative stimuli from − 1.61 D to + 14.83 D with a speed of 0.40 D/s. Accommodative response was measured with the WAM-5500 in high-speed mode at a sampling speed of 5 Hz. A computer program initiated the motor system of the auxiliary lens and synchronized its position with the measurements of the WAM-5500. The right eye viewed through the motorized Badal system, while the left eye was occluded. Any refractive error was fully corrected by trial lenses. The fixation target set at 4.5 m was a 3 × 3 array of 20/30 high-contrast letters49 printed on a white background with a mean luminance of 18 cd m−2. The subjects were instructed to keep the target as clear as possible and to fixate the target even if it became blurred or unresolvable.
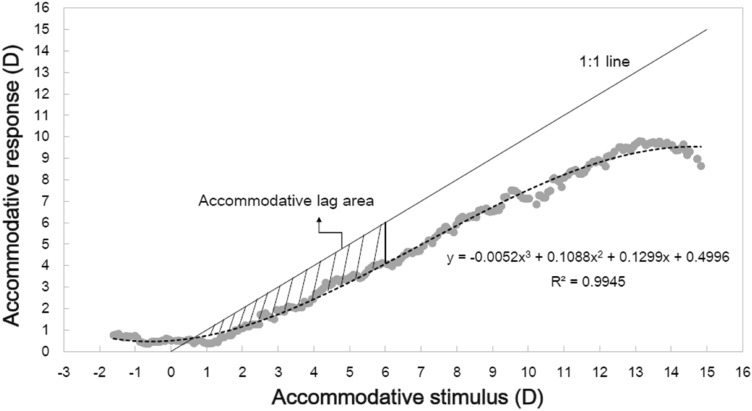
The accommodative stimulus and accommodative response were adjusted at the corneal plane50. Continuous accommodative responses were fitted with a 3-degree polynomial equation as a function of accommodative stimulus. The steepest slope of the curve was calculated. Accommodative lag area was defined as the area of underaccommodation between the 1:1 line and the response curve in the stimulus–response plot between 0 and 6 D (ALA 0–6) (see Fig. 2). The accommodative lag for a given stimulus was obtained by subtracting the accommodative response from the accommodative stimulus. The ASRC of each subject was measured at least three times, and the curve with the best fit (highest R2 value) was chosen for analysis.
Figure 2.
Accommodative stimulus–response curve and accommodative lag area. ASRCs were fitted with a 3-degree polynomial equation (dashed line). The shaded area represents the accommodative lag area between the 1:1 line and the fitted accommodative stimulus–response curve between 0 and 6 D.
Myopia progression at enrolment
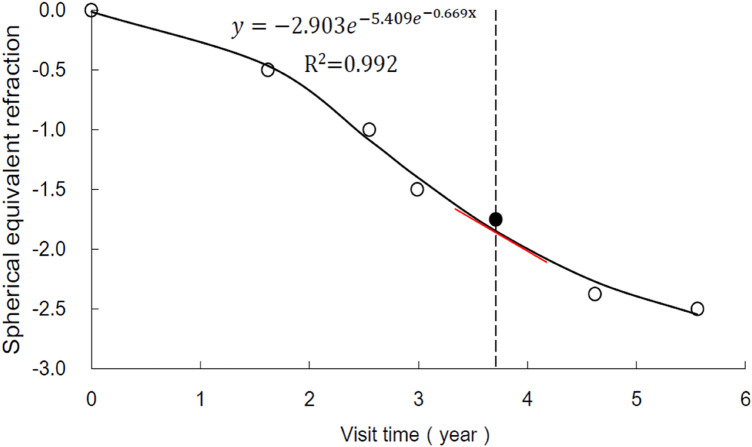
In this study, retrospective and prospective refraction from the enrolment could be obtained from the outpatient database system based on noncycloplegic subjective spherical equivalent refraction (SER). Because the development of myopia is nonlinear27, the classic Gompertz function is fitted with each subject's longitudinal dataset, including at least four records of SER with an interval of more than 6 months between each visit (Fig. 3). The equation is , where Y equals the refractive error at a given visit and x is the visit time relative to the visit that obtained the first record of SER. Myopia progression rate at enrolment is the first derivative of the Gompertz function, defined as the change in SER per year (Fig. 1).
Figure 3.
The trend in myopia progression of one subject fitted with the Gompertz function (solid line). The filled circle represents the SER at enrolment, while open circles represent the retrospective and prospective SER. The slope of the tangential line (red line) at enrolment is the first derivative of the Gompertz function (dashed line), which represents the rate of myopic progression at enrolment.
Statistical analysis
Data from the right eye were analysed by IBM SPSS Statistics software, version 25 (SPSS, Inc., Chicago, IL). A nonlinear regression analysis was used to fit the refractive data with the Gompertz function. The goodness of curve fit depended on the R2 value. A mixed linear model for multilevel repeated-measures data was used to explore the associations between the rate of myopia progression at enrolment and accommodative parameters adjusted by age and SER. The covariates evaluated in the models were the accommodative lag at different stimuli, largest slope of ASRC, accommodative lag area, DAF and sex.
Acknowledgements
This study was supported by the National Health Commission (wkj-zj-1707) and the National Key Research and Development Program of China (grant nos. 2016YFC0100200 and 2016YFC0100201) and was partially funded by Essilor International S.A.
Author contributions
F.L. and J.H.B. designed the study, Y.Y.C. performed the study and wrote the manuscript, H.C. and B.D. supervised the study, C.C.Z. collected the data, N.S. and D.P.S. revised the manuscript, and all the authors reviewed the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Fan Lu and Jinhua Bao.
Contributor Information
Jinhua Bao, Email: baojessie@163.com.
Fan Lu, Email: lufan62@mail.eye.ac.cn.
References
- 1.Rose KA, French AN, Morgan IG. Environmental factors and myopia: Paradoxes and prospects for prevention. Asia Pac. J. Ophthalmol. (Phila) 2016;5:403–410. doi: 10.1097/apo.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 2.Morgan IG, He M, Rose KA. Epidemic of pathologic myopia: What can laboratory studies and epidemiology tell us? Retina. 2017;37:989–997. doi: 10.1097/iae.0000000000001272. [DOI] [PubMed] [Google Scholar]
- 3.Morgan IG, et al. The epidemics of myopia: Aetiology and prevention. Prog. Retina Eye Res. 2018;62:134–149. doi: 10.1016/j.preteyeres.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Ikuno Y. Overview of the complications of high myopia. Retina. 2017;37:2347–2351. doi: 10.1097/iae.0000000000001489. [DOI] [PubMed] [Google Scholar]
- 5.Norton TT, Siegwart JT, Jr, Amedo AO. Effectiveness of hyperopic defocus, minimal defocus, or myopic defocus in competition with a myopiagenic stimulus in tree shrew eyes. Invest. Ophthalmol. Vis. Sci. 2006;47:4687–4699. doi: 10.1167/iovs.05-1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaeffel F, Glasser A, Howland HC. Accommodation, refractive error and eye growth in chickens. Vision Res. 1988;28:639–657. doi: 10.1016/0042-6989(88)90113-7. [DOI] [PubMed] [Google Scholar]
- 7.Gwiazda J, Bauer J, Thorn F, Held R. A dynamic relationship between myopia and blur-driven accommodation in school-aged children. Vision Res. 1995;35:1299–1304. doi: 10.1016/0042-6989(94)00238-H. [DOI] [PubMed] [Google Scholar]
- 8.Abbott ML, Schmid KL, Strang NC. Differences in the accommodation stimulus response curves of adult myopes and emmetropes. Ophthal. Physiol. Opt. 1998;18:13–20. doi: 10.1046/j.1475-1313.1998.97000720.x. [DOI] [PubMed] [Google Scholar]
- 9.Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom. Vis. Sci. 2005;82:273–278. doi: 10.1097/01.OPX.0000159363.07082.7D. [DOI] [PubMed] [Google Scholar]
- 10.Gwiazda J, Thorn F, Bauer J, Held R. Myopic children show insufficient accommodative response to blur. Invest. Ophthalmol. Vis. Sci. 1993;34:690–694. [PubMed] [Google Scholar]
- 11.Haro C, Poulain I, Drobe B. Investigation of working distance in myopic and non-myopic children. Optom. Vis. Sci. 2000;77:189. doi: 10.1097/00006324-200012001-00316. [DOI] [Google Scholar]
- 12.Harb E, Thorn F, Troilo D. Characteristics of accommodative behavior during sustained reading in emmetropes and myopes. Vision Res. 2006;46:2581–2592. doi: 10.1016/j.visres.2006.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parssinen O, Lyyra AL. Myopia and myopic progression among schoolchildren: A three-year follow-up study. Invest. Ophthalmol. Vis. Sci. 1993;34:2794–2802. [PubMed] [Google Scholar]
- 14.Hsu CC, et al. Risk factors for myopia progression in second-grade primary school children in Taipei: A population-based cohort study. Br. J. Ophthalmol. 2017 doi: 10.1136/bjophthalmol-2016-309299. [DOI] [PubMed] [Google Scholar]
- 15.Gwiazda JE, et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest. Ophthalmol. Vis. Sci. 2004;45:2143–2151. doi: 10.1167/iovs.03-1306. [DOI] [PubMed] [Google Scholar]
- 16.Lan W, Yang Z, Liu W, Chen X, Ge J. A longitudinal study on the relationship between myopia development and near accommodation lag in myopic children. Ophthal. Physiol. Opt. 2008;28:57–61. doi: 10.1111/j.1475-1313.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- 17.Berntsen, D. A., Sinnott, L. T., Mutti, D. O., Zadnik, K. & Group, C. S. Accommodative lag and juvenile-onset myopia progression in children wearing refractive correction. Vision Res.51, 1039–1046, https://doi.org/10.1016/j.visres.2011.02.016 (2011). [DOI] [PMC free article] [PubMed]
- 18.Wang Y, Bao J, Ou L, Thorn F, Lu F. Reading behavior of emmetropic schoolchildren in China. Vision Res. 2013;86:43–51. doi: 10.1016/j.visres.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Bao J, et al. Influence of near tasks on posture in myopic Chinese schoolchildren. Optom. Vis. Sci. 2015;92:908–915. doi: 10.1097/opx.0000000000000658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Allen PM, O'Leary DJ. Accommodation functions: Co-dependency and relationship to refractive error. Vision Res. 2006;46:491–505. doi: 10.1016/j.visres.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Pandian A, et al. Accommodative facility in eyes with and without myopia. Invest. Ophthalmol. Vis. Sci. 2006;47:4725–4731. doi: 10.1167/iovs.05-1078. [DOI] [PubMed] [Google Scholar]
- 22.O'Leary DJ, Allen PM. Facility of accommodation in myopia. Ophthal. Physiol. Opt. 2001;21:352–355. doi: 10.1046/j.1475-1313.2001.00597.x. [DOI] [PubMed] [Google Scholar]
- 23.Rosenfield M, Desai R, Portello JK. Do progressing myopes show reduced accommodative responses? Optom. Vis. Sci. 2002;79:268–273. doi: 10.1097/00006324-200204000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Aldaba M, Vilaseca M, Arjona M, Pujol J. Age-related changes in accommodation measured with a double-pass system. Ophthal. Physiol. Opt. 2013;33:508–515. doi: 10.1111/opo.12038. [DOI] [PubMed] [Google Scholar]
- 25.Kasthurirangan S, Glasser A. Age related changes in accommodative dynamics in humans. Vision Res. 2006;46:1507–1519. doi: 10.1016/j.visres.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 26.Kalsi M, Heron G, Charman WN. Changes in the static accommodation response with age. Ophthal. Physiol. Opt. 2001;21:77–84. doi: 10.1046/j.1475-1313.2001.00546.x. [DOI] [PubMed] [Google Scholar]
- 27.Thorn F, Gwiazda J, Held R. Myopia progression is specified by a double exponential growth function. Optom. Vis. Sci. 2005;82:286–297. doi: 10.1097/01.OPX.0000159370.66540.34. [DOI] [PubMed] [Google Scholar]
- 28.Donovan L, et al. Myopia progression rates in urban children wearing single-vision spectacles. Optom. Vis. Sci. 2012;89:27–32. doi: 10.1097/OPX.0b013e3182357f79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holden BA, et al. Nearly 1 billion myopes at risk of myopia-related sight-threatening conditions by 2050—Time to act now. Clin. Exp. Optom. 2015;98:491–493. doi: 10.1111/cxo.12339. [DOI] [PubMed] [Google Scholar]
- 30.Braun CI, Freidlin V, Sperduto RD, Milton RC, Strahlman ER. The progression of myopia in school age children: data from the Columbia Medical Plan. Ophthal. Epidemiol. 1996;3:13–21. doi: 10.3109/09286589609071597. [DOI] [PubMed] [Google Scholar]
- 31.French AN, Morgan IG, Burlutsky G, Mitchell P, Rose KA. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013;120:1482–1491. doi: 10.1016/j.ophtha.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 32.Fan DS, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest. Ophthalmol. Vis. Sci. 2004;45:1071–1075. doi: 10.1167/iovs.03-1151. [DOI] [PubMed] [Google Scholar]
- 33.Lin Z, et al. Peripheral defocus with single-vision spectacle lenses in myopic children. Optom. Vis. Sci. 2010;87:4–9. doi: 10.1097/OPX.0b013e3181c078f1. [DOI] [PubMed] [Google Scholar]
- 34.Mutti DO, et al. Relative peripheral refractive error and the risk of onset and progression of myopia in children. Invest. Ophthalmol. Vis. Sci. 2011;52:199–205. doi: 10.1167/iovs.09-4826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karimian F, Feizi S, Doozande A. Higher-order aberrations in myopic eyes. J. Ophthal. Vis. Res. 2010;5:3–9. [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang N, et al. Relationship between higher-order aberrations and myopia progression in schoolchildren: A retrospective study. Int. J. Ophthalmol. 2013;6:295–299. doi: 10.3980/j.issn.2222-3959.2013.03.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lu F, et al. Axial myopia induced by hyperopic defocus in guinea pigs: A detailed assessment on susceptibility and recovery. Exp. Eye Res. 2009;89:101–108. doi: 10.1016/j.exer.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 38.Mutti DO, et al. Accommodative lag before and after the onset of myopia. Invest. Ophthalmol. Vis. Sci. 2006;47:837–846. doi: 10.1167/iovs.05-0888. [DOI] [PubMed] [Google Scholar]
- 39.French AN, Morgan IG, Mitchell P, Rose KA. Patterns of myopigenic activities with age, gender and ethnicity in Sydney schoolchildren. Ophthal. Physiol. Opt. 2013;33:318–328. doi: 10.1111/opo.12045. [DOI] [PubMed] [Google Scholar]
- 40.Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest. Ophthalmol. Vis. Sci. 2012;53:640–649. doi: 10.1167/iovs.11-7769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.41Correction of Myopia Evaluation Trial 2 Study Group for the Pediatric Eye Disease Investigator, G. Progressive-addition lenses versus single-vision lenses for slowing progression of myopia in children with high accommodative lag and near esophoria. Invest. Ophthalmol. Vis. Sci.52, 2749–2757, 10.1167/iovs.10-6631 (2011). [DOI] [PMC free article] [PubMed]
- 42.Chen Y, et al. Comparison of three monocular methods for measuring accommodative stimulus-response curves. Clin. Exp. Optom. 2017;100:155–161. doi: 10.1111/cxo.12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Radhakrishnan H, Allen PM, Charman WN. Dynamics of accommodative facility in myopes. Invest. Ophthalmol. Vis. Sci. 2007;48:4375–4382. doi: 10.1167/iovs.07-0269. [DOI] [PubMed] [Google Scholar]
- 44.Allen PM, et al. A randomised clinical trial to assess the effect of a dual treatment on myopia progression: The Cambridge Anti-Myopia Study. Ophthal. Physiol. Opt. 2013;33:267–276. doi: 10.1111/opo.12035. [DOI] [PubMed] [Google Scholar]
- 45.Price H, et al. The Cambridge Anti-myopia Study: Variables associated with myopia progression. Optom. Vis. Sci. 2013;90:1274–1283. doi: 10.1097/opx.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 46.Fotedar R, et al. Necessity of cycloplegia for assessing refractive error in 12-year-old children: A population-based study. Am. J. Ophthalmol. 2007;144:307–309. doi: 10.1016/j.ajo.2007.03.041. [DOI] [PubMed] [Google Scholar]
- 47.Choong YF, Chen AH, Goh PP. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am. J. Ophthalmol. 2006;142:68–74. doi: 10.1016/j.ajo.2006.01.084. [DOI] [PubMed] [Google Scholar]
- 48.Hashemi H, et al. Cycloplegic autorefraction versus subjective refraction: The Tehran Eye Study. Br. J. Ophthalmol. 2016;100:1122–1127. doi: 10.1136/bjophthalmol-2015-307871. [DOI] [PubMed] [Google Scholar]
- 49.Allen PM, Charman WN, Radhakrishnan H. Changes in dynamics of accommodation after accommodative facility training in myopes and emmetropes. Vision Res. 2010;50:947–955. doi: 10.1016/j.visres.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 50.Mutti DO, Jones LA, Moeschberger ML, Zadnik K. AC/A ratio, age, and refractive error in children. Invest. Ophthalmol. Vis. Sci. 2000;41:2469–2478. [PubMed] [Google Scholar]