To the Editor:
Conservative management (active surveillance or watchful waiting) for low-risk prostate cancer is an increasingly used alternative to definitive radiation therapy or radical prostatectomy.1,2 Given the underrepresentation of black patients in clinical trials and concern about underlying aggressive disease,3,4 expert panels advise caution when applying conservative management to black patients.1 Therefore, we examined recent trends in the use of active surveillance or watchful waiting in black men, as compared with nonblack men, with low-risk prostate cancer in the United States.
The Surveillance, Epidemiology, and End Results Prostate with Watchful Waiting Database identified patients with low-risk prostate cancer (defined as a clinical stage of T1 to T2a [indicating early-stage disease], a Gleason score of ≤6 [on a scale from 2 to 10, with scores of ≤6 indicating low-risk cancer], and a prostate-specific antigen level of less than 10 ng per milliliter) for which the management type was known and that had been diagnosed between 2010 and 2015.5 Additional details about this cohort and the study design are provided in the Supplementary Appendix, available with the full text of this letter at NEJM.org.
We used the Cochran–Armitage test to evaluate trends in initial management over time. Multivariable logistic regression was used to define adjusted odds ratios and 95% confidence intervals for the receipt of active surveillance or watchful waiting as compared with definitive treatment, with race as the primary independent variable. We used the validated Yost index to adjust for socioeconomic status.5 Information regarding all the variables that were included in the models is provided in the Supplementary Appendix.
Of 50,302 patients, 7517 (14.9%) were black and 42,785 (85.1%) were nonblack. (The baseline characteristics of the patients are shown in the Supplementary Appendix.) From 2010 through 2015, the use of radical prostatectomy and definitive radiotherapy decreased from 41.4% and 46.0% to 28.8% and 34.8%, respectively, among black men and from 48.5% and 36.7% to 31.8% and 24.9% among nonblack men (P<0.001 for trend). In contrast, the use of active surveillance or watchful waiting increased from 12.6% to 36.4% among black men and from 14.8% to 43.3% among nonblack men (P<0.001 for trend) (Fig. 1A).
Figure 1. Initial Management of Low-Risk Prostate Cancer and Odds Ratios for Receipt of Active Surveillance or Watchful Waiting, as Compared with Definitive Therapy, among Black Men and Nonblack Men.
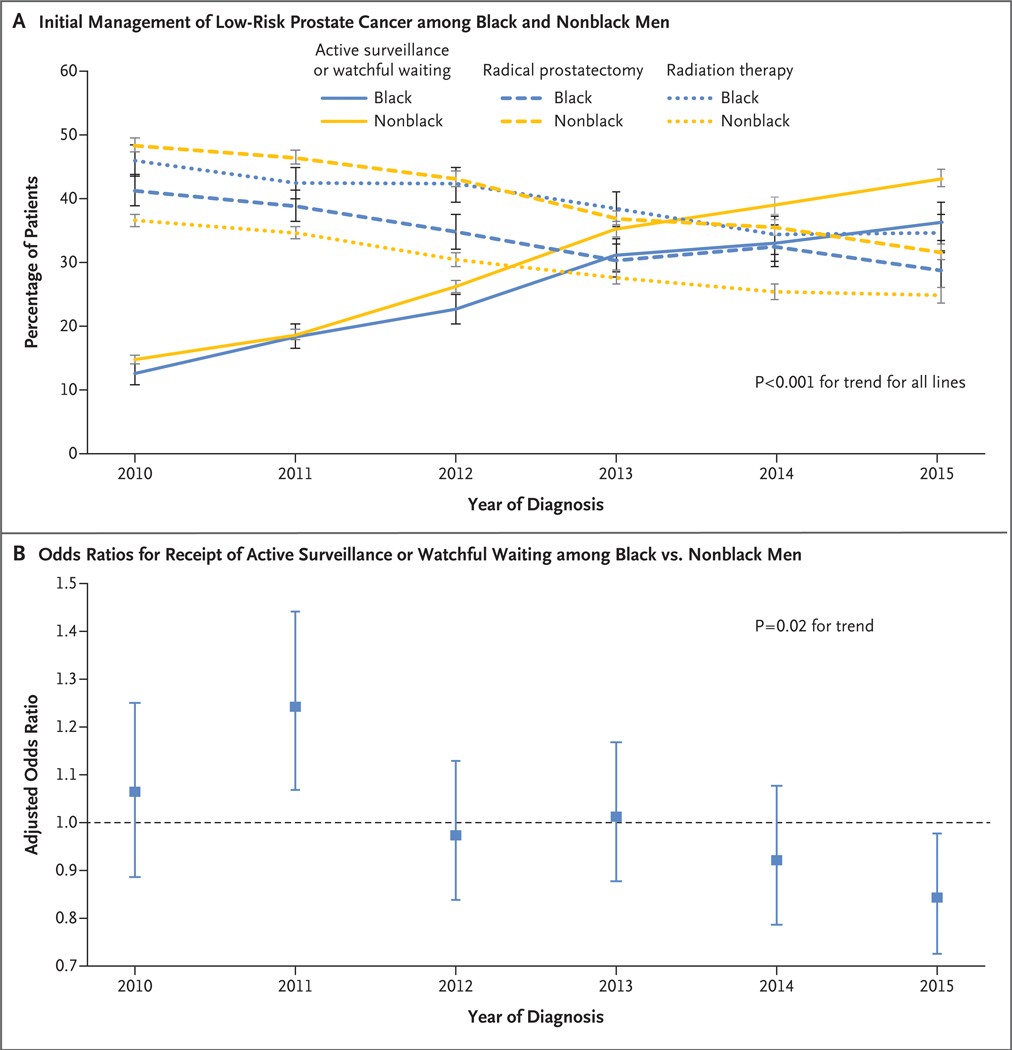
Panel A shows the percentages of initial strategies to manage low-risk prostate cancer in the United States from 2010 through 2015 among 7517 black men, as compared with 42,785 nonblack men. I bars indicate 95% confidence intervals. Panel B shows a temporal plot of multivariable-adjusted odds ratios for receipt of active surveillance or watchful waiting as compared with definitive therapy (radical prostatectomy or any radiation therapy) for the independent variable of race (black vs. nonblack [referent]). The analysis was adjusted for all the variables listed in the Supplementary Appendix, including the Yost index for socioeconomic status and insurance status.
In an analysis that was not adjusted for socioeconomic status or insurance status, black men had lower odds of receipt of active surveillance or watchful waiting than nonblack men (adjusted odds ratio, 0.93; 95% confidence interval [CI], 0.88 to 0.99; P = 0.02). However, race was no longer significantly associated with receipt of active surveillance or watchful waiting after the analysis was adjusted for socioeconomic status and insurance status (adjusted odds ratio among black men, 1.01; 95% CI, 0.95 to 1.07; P = 0.86) (see the Supplementary Appendix). For the years from 2010 through 2015, the multivariable adjusted odds ratios for receipt of active surveillance or watchful waiting among black men as compared with nonblack men were as follows: 1.06 (95% CI, 0.89 to 1.25; P = 0.52) in 2010; 1.24 (95% CI, 1.07 to 1.44; P = 0.004) in 2011; 0.97 (95% CI, 0.84 to 1.13; P = 0.72) in 2012; 1.01 (95% CI, 0.88 to 1.17; P = 0.86) in 2013; 0.92 (95% CI, 0.79 to 1.08; P = 0.31) in 2014; and 0.84 (95% CI, 0.73 to 0.98; P = 0.02) in 2015 (P = 0.02 for trend) (Fig. 1B).
From 2010 through 2015, the use of active surveillance or watchful waiting nearly tripled among both black men and nonblack men. Multivariable analyses suggest that racial differences in the receipt of active surveillance or watchful waiting may be driven by differences in socioeconomic status. Still, black men were less likely than nonblack men to receive active surveillance or watchful waiting by 2015, even after adjustment for socioeconomic status — a finding that suggests a possible lower relative uptake of active surveillance or watchful waiting over time for black men. Studies with additional years of data collection, distinction between active surveillance and watchful waiting, and information on delayed radical interventions will be needed to monitor for trends in racial differences in conservative management.
Supplementary Material
THIS WEEK’S LETTERS.
| 2070 | Active Surveillance for Low-Risk Prostate Cancer in Black Patients |
| 2072 | Omadacycline for Bacterial Infections |
| 2074 | Alirocumab after Acute Coronary Syndrome |
| 2078 | Diagnostic Utility of Exome Sequencing for Kidney Disease |
| 2081 | A Woman with Delusional Thinking and Paresthesia of the Right Hand |
| e40 | Aspiration Pneumonia |
Acknowledgments
Supported by the American Society for Radiation Oncology, by the Prostate Cancer Foundation, by a grant (CA18473) from the Department of Health and Human Services, and by a Prostate Cancer Foundation–American Society for Radiation Oncology Award to End Prostate Cancer (to Dr. Mahal).
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
Contributor Information
Santino Butler, Dana–Farber Cancer Institute Boston, MA
Vinayak Muralidhar, Dana–Farber Cancer Institute Boston, MA
Janice Chavez, Dana–Farber Cancer Institute Boston, MA
Zoe Fullerton, Dana–Farber Cancer Institute Boston, MA
Aman Mahal, Yale School of Medicine New Haven, CT
Michelle Nezolosky, Dana–Farber Cancer Institute Boston, MA
Marie Vastola, Dana–Farber Cancer Institute Boston, MA
Shuang G. Zhao, University of Michigan Ann Arbor, MI
Anthony V. D’Amico, Dana–Farber Cancer Institute Boston, MA
Robert T. Dess, University of Michigan Ann Arbor, MI
Felix Y. Feng, University of California, San Francisco San Francisco, CA
Martin T. King, Dana–Farber Cancer Institute Boston, MA
Kent W. Mouw, Dana–Farber Cancer Institute Boston, MA
Daniel E. Spratt, University of Michigan Ann Arbor, MI
Quoc-Dien Trinh, Dana–Farber Cancer Institute Boston, MA
Paul L. Nguyen, Dana–Farber Cancer Institute Boston, MA
Timothy R. Rebbeck, Dana–Farber Cancer Institute Boston, MA
Brandon A. Mahal, Harvard Radiation Oncology Program Boston, MA
References
- 1.Mohler JL, Kantoff PW, Armstrong AJ, et al. Prostate cancer, version 2.2014. J Natl Compr Canc Netw 2014; 12: 686–718. [DOI] [PubMed] [Google Scholar]
- 2.Mahal BA, Butler S, Franco I, et al. Use of active surveillance or watchful waiting for low-risk prostate cancer and management trends across risk groups in the United States, 2010–2015. JAMA 2019. February 11 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sundi D, Ross AE, Humphreys EB, et al. African American men with very low-risk prostate cancer exhibit adverse oncologic outcomes after radical prostatectomy: should active surveillance still be an option for them? J Clin Oncol 2013; 31: 2991–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahal BA, Berman RA, Taplin ME, Huang FW. Prostate cancer-specific mortality across Gleason scores in black vs nonblack men. JAMA 2018; 320: 2479–81. [DOI] [PubMed] [Google Scholar]
- 5.Surveillance, Epidemiology, and End Results Program. Prostate with watchful waiting database (2010–2015). Bethesda, MD: National Cancer Institute, 2018. (https://seer.cancer.gov/seerstat/databases/prostate-ww/index.html ). DOI: 10.1056/NEJMc1900333 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


