Abstract
Introduction
Several articles have been published about the reorganisation of surgical activity during the COVID-19 pandemic but few, if any, have focused on the impact that this has had on emergency and trauma surgery. Our aim was to review the most current data on COVID-19 to provide essential suggestions on how to manage the acute abdomen during the pandemic.
Methods
A systematic review was conducted of the most relevant English language articles on COVID-19 and surgery published between 15 December 2019 and 30 March 2020.
Findings
Access to the operating theatre is almost exclusively restricted to emergencies and oncological procedures. The use of laparoscopy in COVID-19 positive patients should be cautiously considered. The main risk lies in the presence of the virus in the pneumoperitoneum: the aerosol released in the operating theatre could contaminate both staff and the environment.
Conclusions
During the COVID-19 pandemic, all efforts should be deployed in order to evaluate the feasibility of postponing surgery until the patient is no longer considered potentially infectious or at risk of perioperative complications. If surgery is deemed necessary, the emergency surgeon must minimise the risk of exposure to the virus by involving a minimal number of healthcare staff and shortening the occupation of the operating theatre. In case of a lack of security measures to enable safe laparoscopy, open surgery should be considered.
Keywords: Coronavirus, COVID-19, 2019-nCoV, SARS-CoV-2, Emergency surgery, Laparoscopy, Open surgery, Non-operative management, Acute abdomen
Introduction
An incomparable outbreak of respiratory illness in Wuhan, Hubei province, China, was declared in December 2019. A novel coronavirus, provisionally referred to as 2019 novel coronavirus (2019-nCoV) and later named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified on 12 January 2020. On 11 February 2020, the World Health Organization officially named the disease caused by the virus: COVID-19. Despite rigorous global containment and quarantine efforts, the incidence of COVID-19 has continued to rise rapidly. As of 31 March 2020, the pandemic had spread worldwide with over 750,000 confirmed cases, including over 36,000 deaths. In Europe, there were more than 423,000 confirmed cases with almost 27,000 deaths.1
The high transmissibility of the virus was quickly confirmed. Critically ill patients with COVID-19 required intensive care unit (ICU) admission and ventilation support. Hospitals were overwhelmed. Surgical theatres were converted into additional ICUs. Non-urgent, non-cancer surgical procedures were cancelled. Medical and paramedical staff were relocated to provide ventilatory support for patients with COVID-19 infection.
Several articles have addressed the reorganisation of surgical activity under COVID-19. However, only a few, if any, have focused on the impact on the management of emergency and trauma surgery and of the acute abdomen. We aimed to review the latest data on the COVID-19 pandemic so as to provide essential information for practice in emergency surgery.
Methods
A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P),2 through the MEDLINE® (PubMed), Embase™ and SCOPUS® databases. The following keywords and/or Medical Subject Headings were used: “COVID-19” or “pandemic” or “pneumonia” or “2019-nCoV” AND “surgery” or “abdominal pain”, “laparoscopy”, “emergency”, “open abdomen”; “SARS-CoV-2” or “prevention”. All available articles (reviews, editorials, epidemiological studies, case series etc) on COVID-19 and surgery published in the English language between 15 December 2019 and 30 March 2020 were included in the review.
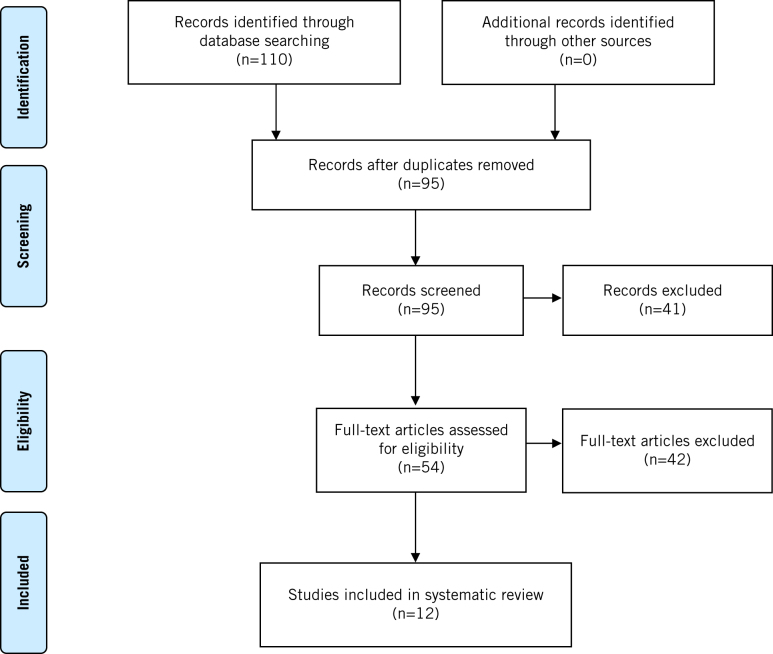
The article selection criteria were defined before initiating data collection for proper identification of articles eligible for analysis. All articles in which the primary objective was to describe the practice of surgery under the COVID-19 pandemic were reviewed. A flowchart of study identification and the inclusion/exclusion process is shown in Figure 1. Twelve papers were included in the systematic review.3–14
Figure 1.
Flowchart of studies included in review
Findings
Pathogenesis
COVID-19 is determined by the virus SARS-CoV-2, an enveloped non-segmented positive-sense RNA virus. Given the similarity of SARS-CoV-2 to bat SARS-CoV-like coronaviruses, it is likely that bats serve as reservoir hosts for its progenitor. Indeed, based on virus genome sequencing results and evolutionary analysis, bats have been suspected as the natural host of the virus origin and SARS-CoV-2 might be transmitted from bats via unknown intermediate hosts to infect humans.15–19
The human angiotensin converting enzyme 2 (ACE2) is the receptor for SARS-CoV-2. In the normal human lung, ACE2 is expressed on type 1 and type 2 alveolar epithelial cells. The binding of SARS-CoV-2 on ACE2 can lead to damage of the alveolar cells, triggering a series of severe systemic reactions and even death.17,19
Clinical features and diagnosis
The incubation period for COVID-19 is thought to be less than 14 days, with most cases occurring within 4 or 5 days after exposure.16 Huang et al found that 98% of patients had a fever, with 78% having a temperature of >38°C.20 They reported that 76% had a cough, 44% experienced fatigue and muscle pain, and 55% had dyspnoea. Fewer patients experienced expectoration (28%), headache (8%), haemoptysis (5%) or diarrhoea (3%).
Guan et al reported 1,099 cases of SARS-CoV-2 infection.21 They found that fever (87.9%) and cough (67.7%) were the most common symptoms. Diarrhoea (3.7%) and vomiting (5.0%) were rare. Table 1 summarises the key clinical and epidemiological findings suggestive of a COVID-19 infection. The route of transmission of COVID-19 is not yet fully understood but it is thought to be mainly respiratory. Cases of paediatric patients presenting with signs of conjunctivitis prior to respiratory and other systemic symptoms have been reported in the literature.22 Ocular involvement has not been described with either Middle East respiratory syndrome coronavirus (MERS-CoV) or SARS-CoV although polymerase chain reaction (PCR) testing on tears from patients with SARS-CoV infection has demonstrated the presence of the virus.23,24
Table 1.
Diagnostic criteria for COVID-19
| CDC | WHO | |
| Clinical features |
|
|
| Epidemiological risk |
|
|
| Radiological findings | Patchy ground glass opacities in multiple pulmonary lobules (bilateral) with peripheral distribution are typical chest CT features. | |
ARI = acute respiratory infection; CDC = Centers for Disease Control and Prevention; CT = computed tomography; WHO = World Health Organization
COVID-19 patients present with leucopenia and lymphocytopenia. Aspartate aminotransferase is often elevated. Infected patients could present with myocarditis and an increased level of hypersensitive troponin I.20 Inflammatory biomarkers such as C-reactive protein, erythrocyte sedimentation rate and proinflammatory cytokines are usually elevated, as are lactate dehydrogenase, creatinine and prothrombin time.25 Abnormal features on computed tomography of the chest appear to be evident in 100% of infected patients. Bilateral ground glass-like opacities and consolidation areas are also found in the majority. Patchy consolidation, alveolar exudates and interlobular involvement have been demonstrated in severe infection indicating deterioration.26,27 Critical patients could present with acute respiratory distress syndrome, arrhythmia, shock, acute kidney injury, acute cardiac injury, liver dysfunction or secondary infection.
Based on the current information, most patients have a good prognosis while a few patients deteriorate into critical condition, especially the elderly and those with chronic underlying diseases.28 The mortality rate is estimated to be below 2%, meaning it is likely that likely 98% of infected people will recover.28
Diagnosis of COVID-19 infection is usually made following real time PCR testing that provides nucleic acid detection in nasal and throat swab samples or other respiratory tract samples, and this is further confirmed by next generation sequencing.21 False negative results have been observed that are related to the quality of the kit, the collected sample and the performance of the test. If the test result is positive, it is recommended that the test is repeated for confirmation. In patients with a confirmed COVID-19 diagnosis, the laboratory evaluation should be repeated to verify viral clearance prior to being released from isolation.
Current treatment
Agents used previously to treat SARS and MERS are potential candidates for treating COVID-19. Various agents with apparent in vitro activity against SARS-CoV and MERS-CoV were used during the SARS and MERS outbreaks, with inconsistent efficacy. Meta-analyses of SARS and MERS treatment studies have found no clear benefit of any specific regimen. Some of them (in different combinations, alone or along with new therapeutic agents) have been tested in these first phases of the pandemic; currently, however, there is no evidence from randomised controlled trials that any potential therapy improves outcomes in patients with either suspected or confirmed COVID-19. All the most recent therapeutic investigations to treat COVID-19 have been summarised by Sanders et al and are listed in Table 2.29
Table 2.
Current treatment for COVID-19
| Clinical syndrome associated with COVID-19 | Supportive therapy | Specific therapy | Comment | |
| Patients with moderate respiratory symptoms and/or chest x-ray with interstitial pneumonia |
|
Supportive therapy (oxygen) | Lopinavir/ritonavir 400mg/100mg by mouth every 12 hours for up to 14 days + hydroxychloroquine 200mg twice daily for 5–20 days or chloroquine 500mg twice daily for 20 days |
Interferon alfa is also used (eg 5 million units by aerosol inhalation twice daily). |
| Patients with mild respiratory symptoms but age >70 years and/or comorbidities or risk of increased mortality | ||||
| Patients with severe symptoms |
|
Resuscitation evaluation or intensive care transfer | If available: Remdesivir (with a loading dose on first day of 200mg IV, followed by a maintenance dose of 100mg IV per day for another 9 days) + hydroxychloroquine or chloroquine (see above) Or: Lopinavir/ritonavir (200mg/50mg) + hydroxychloroquine or chloroquine (see above) |
Corticosteroids should be used prudently in critically ill patients with COVID-19 pneumonia (0.5–1mg/kg per day methylprednisolone or equivalent for ≤7 days). |
| Mild illness | Fever and non-specific symptoms (eg asthenia, cough, anorexia, dysgeusia, headache, nasal congestion, general malaise, muscle pain) | Treatment of symptoms | None | |
| Asymptomatic patients | None | Surveillance | None |
ARDS = acute respiratory distress syndrome; IV = intravenous
General strategies for prevention
The World Health Organization and the Centers for Disease Control and Prevention recommend avoiding travel to high risk areas and contact with symptomatic individuals.30,31 Basic hand hygiene measures are also recommended, including frequent handwashing, use of portable hand sanitiser, and avoiding contact with face and mouth after interacting with a possibly contaminated environment. Healthcare workers caring for infected individuals should employ contact and airborne precautions (including personal protective equipment [PPE] such as N95 or FFP3 masks, eye protection, gowns and gloves) to prevent transmission of the pathogen.
Decision making for patients presenting as a surgical emergency
During the COVID-19 pandemic, hospital leadership and individual providers are facing increasingly difficult decisions about how to conserve critical resources (such as hospital and ICU beds, respirators and transfusion capacity) as well as PPE, which is vital for protecting both patients and staff from intrahospital transmission. The emergency surgeon has to take into consideration that there is limited access to operating theatres (many having been converted into ICUs) and that the risk of virus dissemination exists even in theatre. According to available data, SARS-CoV-2 is presumed to spread primarily via respiratory droplets and close contact. However, since these transmission modes do not explain all cases, there is still inconclusive evidence of airborne transmission.11
Moreover, the proportion of individuals infected by SARS-CoV-2 who remain asymptomatic throughout the course of infection has not yet been definitely assessed.32 It is known that:32–34
SARS-CoV-2 can be transmitted by asymptomatic infectors;
SARS-CoV-2 can be transmitted by droplets, fomites and contact;
faecal–oral transmission and aerosol transmission cannot be excluded;
human coronaviruses can persist on inanimate surfaces such as metal, glass or plastic for up to nine days.
As emergency surgeons, we should bear in mind two aims when planning a surgical procedure: safety and prevention. The emergency surgeon’s objectives during the COVID-19 pandemic are summarised in Table 3.
Table 3.
The emergency surgeon’s objectives when planning a surgical procedure during the COVID-19 pandemic
| • Minimise virus exposure in operating theatre |
| • Decrease risk of environmental contamination |
| • Minimise occupation of operating theatre |
| • Reduce hospital stay of patient undergoing emergency surgery |
After careful clinical examination of a patient presenting with acute abdominal pain and considering imaging results, the first question should be whether postponement of the surgical treatment is possible (ie until the patient is no longer considered potentially infectious or at risk of perioperative complications). If an emergency surgical procedure is necessary (life threatening complication, high risk patient, haemodynamic compromise or shock), the emergency surgeon should check the availability of a dedicated operating theatre with functional and suitable human and technical resources. The golden rule is to involve the smallest number of healthcare staff, correctly protected. Furthermore, given that there is currently no clear recommendation on which group of patients COVID-19 testing should be performed, we suggest using the minimum recommended PPE measures for infection prevention as summarised in Table 4 for all patients.35
Table 4.
Minimum standard of PPE for any staff caring for a patient with confirmed/suspected COVID-19
| Recommended PPE | Why |
| NIOSH-certified N95 respirator | Filters at least 95% of airborne particles but is not resistant to oil |
| Eye protection (either goggles or full-face shield) | To avoid contact of droplets with mucosa and conjunctiva |
| Cap | To avoid contact with contaminated surfaces or biological liquids |
| Gown | To avoid contact with contaminated surfaces or biological liquids |
| Gloves (Double gloves may be considered and the outer pair should be changed when contaminated.) | To avoid contact with contaminated surfaces or biological liquids |
| Powered air-purifying respirator | Especially in aerosol generating procedures (such as during induction of anaesthesia and intubation) when available |
NIOSH = National Institute for Occupational Safety and Health; PPE = personal protective equipment
Non-operative management or urgent surgical treatment?
Early clinical diagnosis, adequate source control to stop ongoing contamination, appropriate antimicrobial therapy and prompt resuscitation in critically ill patients are the cornerstone of management of intra-abdominal infection.36 Triage of patients is fundamental to assessing the severity of the underlying intra-abdominal disease. This enables the emergency surgeon to decide on non-operative management (NOM) or surgery. Initial clinical (signs of localised or generalised peritonitis at abdominal examination) and biological parameters (inflammatory biomarkers such as C-reactive protein, procalcitonin, lactates) should be rapidly assessed.
Haemodynamic status after initial resuscitative manoeuvres remains the main tool to risk stratify patients in need of immediate surgery. In addition, general parameters (eg age, comorbidities) or more specific, clinical scores (eg ASA [American Society of Anesthesiologists] grade, Alvarado score, sequential organ failure assessment score) can assist in the emergency surgeon’s decision making process.
Intra-abdominal infection can be classified as uncomplicated (ie involving the organ and not the peritoneum) or complicated (ie localised or diffuse peritonitis).36 NOM of uncomplicated intra-abdominal infection could be a valid option, to be considered on a case-by-case basis, according to World Society of Emergency Surgery (WSES) guidelines. In case of NOM, it is crucial to plan close clinical and radiological surveillance at 12–24-hour intervals until the situation is under control.36 If the patient presents with persistent abdominal pain, fever or signs of shock, surgical treatment is mandatory.
Appendicitis
Generally, the gold standard treatment for acute appendicitis is laparoscopic appendicectomy in all patients. With COVID-19, caution should be employed in the choice of the laparoscopic approach because of concerns about the presence of the virus in the pneumoperitoneum. However, NOM with antibiotic therapy has proved to be successful in uncomplicated appendicitis. The WSES Jerusalem guidelines and the 2020 update of these consider it appropriate to use NOM in selected patients (adults or children) with uncomplicated appendicitis who wish to avoid surgery and are willing to accept the risk of disease recurrence of up to 39%.37
NOM does not increase the perforation rate and most cases of recurrence are still uncomplicated appendicitis, making NOM and the ‘antibiotic first’ strategy a safe alternative to surgery in selected cases on a short-term basis.37 In this scenario, the high risk of recurrence does not appear to be pivotal in decision making and an ‘antibiotic first’ policy can be a safe means of avoiding surgery for uncomplicated acute appendicitis during the COVID-19 pandemic and postponing it to (eventually) treat a recurrence.
Similarly, during the pandemic, patients presenting with complicated appendicitis with a well defined abscess in the right iliac fossa can be managed with percutaneous drainage if it is available, coupled with intravenous antibiotics. Patients with evidence of perforation may be managed with percutaneous drainage or surgery depending on the patient’s condition. Patients who fail NOM should be expedited for surgery.37
Acute cholecystitis
Laparoscopic cholecystectomy remains the treatment of choice for acute cholecystitis.38 In particular, early laparoscopic cholecystectomy is better than delayed laparoscopic cholecystectomy. Multiple randomised and controlled trials have shown early cholecystectomy to be associated with a shorter hospital stay without any significant difference in the complication rate or conversion when compared. However, the recommendation of early surgery could be challenged owing to COVID-19 related restrictions. Managing the infection with intravenous antibiotics and analgesics to delay surgery should be seriously considered in such a context. Percutaneous cholecystostomy with intravenous antibiotics has been advocated as an alternative to surgery in critically ill patients. In fact, the 2016 WSES guidelines do not recommend it as an alternative to laparoscopic cholecystectomy except in the most unfit patients because of the significantly higher mortality rate.38 The recent CHOCOLATE trial confirmed that finding and was interrupted owing to the poor results in the percutaneous cholecystostomy group.39
Diverticulitis
According to WSES guidelines, the treatment of choice for uncomplicated acute diverticulitis is NOM with intravenous antibiotics, considering transition to oral antibiotics as soon as possible.40 Patients who present with generalised peritonitis should undergo surgery. Hinchey class I and II diverticulitis should be managed with percutaneous drainage in addition to antimicrobial therapy if a large (>4cm) abscess is visualised on computed tomography. If percutaneous drainage is not available, the patient could be managed with antibiotics but surgery should be considered if there are signs of sepsis or shock. Patients who fail NOM should be expedited for surgery.
Patients with pneumoperitoneum (free air distant to the sigmoid) and peritonitis should be considered for surgery. In this scenario, the surgical options are:40
Hartmann’s procedure for managing diffuse peritonitis in critically ill patients and in selected patients with multiple comorbidities;
primary resection with anastomosis with or without a diverting stoma in clinically stable patients with no major comorbidities.
Emergency laparoscopic sigmoidectomy should be avoided owing to the risk of aerosolisation, especially if a long operative duration is expected.
Colonic obstruction and perforation
According to WSES guidelines, left colonic obstruction would be best treated by a loop colostomy (short operative time) or Hartmann’s procedure.41 The latter should be preferred over simple colostomy to avoid a longer hospital stay and multiple operations. On the other hand, the loop colostomy can temporarily treat the occlusion (bridge to surgery option) and definitive surgery can be planned in accordance with the management of hospital resources under the COVID-19 pandemic.
Generally, we recommend reserving loop colostomy for patients with unresectable tumours, or those unfit for major surgery or even general anaesthesia. Colonic stent placement could have a role but endoscopy can promote spreading of the virus. Consequently, we suggest considering it in COVID-19 patients only if they are unfit for surgery and general anaesthesia.41
Colonic resection and primary anastomosis, with or without loop ileostomy, should be the preferred option for uncomplicated malignant left-sided large bowel obstruction. However, it may increase operative time, with a high risk of viral exposure. Patients with high surgical risk would be better managed with Hartmann’s procedure.
In the absence of major caecal distension, bowel ischaemia or synchronous patent right colonic cancer, total colectomy should not be undertaken.41 In the case of obstructive right-sided colon cancer, right colectomy with primary anastomosis is the preferred option. An end ileostomy with colonic fistula represents a valid alternative when a primary anastomosis is deemed too hazardous.41 For unresectable right-sided colon cancer, a side-to-side anastomosis ileotransverse internal bypass or a loop ileostomy could be performed.41
Adhesive small bowel obstruction
Even during the COVID-19 pandemic, NOM (ie nil by mouth, nasogastric decompression) should always be the first approach in patients with adhesive small bowel obstruction (ASBO) unless there are signs of peritonitis, strangulation or bowel ischaemia. NOM is effective in approximately 70–90% of patients with ASBO. While evidence for the optimal duration of NOM is lacking, most authors consider up to 72 hours as safe and appropriate.42
Incarcerated abdominal hernia
Patients should undergo emergency hernia repair immediately when intestinal strangulation is suspected in order to avoid intestinal ischaemia.43 In case of an incarcerated inguinal hernia, local anaesthesia can be used (in the absence of bowel gangrene) to decrease the risk of aerosol spreading of the virus in the operating theatre.
Laparoscopic or open approach?
Patients who have failed NOM for a surgical condition or who present with haemodynamic instability should be considered for surgery. In emergency surgery, laparoscopy has many advantages, including reduced length of hospital stay, less pain, less impact on respiratory movements and rapid postoperative recovery.44
In clinical practice, the laparoscopic approach for emergency and trauma surgery remains controversial because of technical difficulties and the high conversion rate in non-experienced hands.45–48 In surgical patients with COVID-19, great care must be taken when carrying out a laparoscopic procedure as there is a theoretical risk of occupational exposure and infection of the operating theatre staff.5,9,10,14,49 although to our knowledge, there has been no study that has firmly confirmed the presence of the virus in theatre during laparoscopic procedures.
In a brief report, Wang and Du state that aerosols are particles formed by solid or liquid particles dispersed and suspended in the air.50 These may contain soil particles, industrial dust particles, particulates emitted by automobiles, bacteria, microorganisms, plant spore powders or other components. When a person infected with the virus coughs, sneezes, breathes vigorously or speaks loudly, the virus will be excreted from the body and may dissolve with the aerosols, becoming bioaerosols. The particles in a bioaerosol are generally 0.3–100μm in diameter but only the respirable size fraction of 1–10μm is of particular concern. Bioaerosols ranging in size from 1.0μm to 5.0μm usually remain in the air whereas larger particles are deposited on surfaces. Droplets of saliva are discharged by people sneezing or coughing and their particle size is generally 1–5mm. These spread in a space of about 1–2m from the source of the infection. However, the aerosol can travel hundreds of meters or more. More importantly, current researches have proved that aerosols are involved in the spread of SARS, MERS, H1N1 and by extrapolation, COVID-19.
As reported for SARS, SARS-CoV-2 seems to spread mostly by direct exposure to infectious droplets and secretions but further evidence has indicated that indirect transmission by environmental contamination could be responsible in cases of nosocomial transmission of the virus.8,12,51 Van Doremalen et al have demonstrated that SARS-CoV-2 is more stable in aerosols and on various surfaces (plastic and stainless steel) under experimental conditions than SARS-CoV-1, and that it can remain viable and infectious in aerosols for hours and on surfaces, for days (depending on the inoculum shed).12
According to these data, the four surgical royal colleges in the UK and Ireland as well as other societies have already provided advice (updated on 7 April 2020) with regard to laparoscopy.52 They suggest considering laparoscopy only in highly selected individual cases where clinical benefit to the patient substantially exceeds the risk of potential viral transmission in that particular situation.
Short from prohibiting laparoscopy, several authors recommend filtering the surgical smoke during an operation.5,9,10,14,49,50 For some, a laparoscopic approach could be associated with longer operative time (and therefore increased risk of exposure), especially in an emergency setting. For others, laparoscopic procedures create a functional barrier between the surgeon and the disease because the abdomen is not opened, reducing exposure to the disease (including the dissemination of aerosol) compared with open surgery.
Having reviewed the available literature on COVID-19, we concur that when considering the laparoscopic approach in an emergency, every effort should be made to limit the leakage of gas. Recommended techniques include using constant pressure insufflators to reduce the aerosol effect of insufflation and central aspirator systems to drain the smoke. For example, some authors suggest using the closed circuit of pressurised intraperitoneal aerosol chemotherapy if available or connecting one of the laparoscopic ports to a water seal created with a sealed container using extension lines.5,9,10 Before making the incision for retrieval of an operative specimen, the ‘gas’ must be turned off and the pneumoperitoneum must be emptied by means of the negative pressure connected to the water seal.5 Special attention should be paid to evacuating residual carbon dioxide from the container and the abdominal cavity before removing the trocars.
In conclusion, if not all of the described precautions (summarised in Table 5) can be adopted, laparoscopy would better be avoided, especially in an emergency setting.3,5,53
Table 5.
Tips and tricks to make laparoscopy safer during the COVID-19 pandemic
| 1. Use a closed suction system. |
| 2. Avoid redundant incisions. |
| 3. Use leak free trocars such as balloon trocars. |
| 4. Avoid creating a leak for smoke evacuation. |
| 5. Aspirate the entire pneumoperitoneum before retrieving a specimen, at the end of the procedure before removing the trocars or before conversion to open surgery. |
| 6. In case of a lack of skills and adapted materials enabling a safe laparoscopic surgical intervention, laparotomy should be preferred. |
Damage control surgery and open abdomen
A strategy for damage control surgery may have a role in haemodynamically compromised patients.54 Patients treated with either damage control surgery or open abdomen will need to be admitted to the ICU. However, as ICUs are currently overwhelmed because of the pandemic, the indications for performing open abdomen surgery should be carefully evaluated on a case-by-case basis.
General measures to prepare the operating theatre
It is important to define a dedicated in-hospital route for patients with suspected or confirmed COVID-19.11 All staff who come into contact with the patient must perform strict hand hygiene and wear PPE (including FFP2 mask, eye protection, cap, oversized waterproof long-sleeved gown, knee-high shoe protection and a double pair of gloves). Healthcare workers are advised to avoid touching any mucosal membranes (eyes, nose or mouth).11,13 Every surgical procedure involving a COVID-19 patient must be performed in a negative pressure environment to reduce dissemination of the virus beyond the operating theatre. A high frequency of air renewal (25 times per hour) in a standard positive pressure operating theatre could help reduce the viral load.6,11,13
The number of staff involved in any surgical procedure should be limited. The name of all participating staff members should be recorded to facilitate contact tracing. Theatre doors must be closed for the entire duration of the operation. Movement of staff in and out of the operating theatre should also be restricted.4,7,55 Only selected equipment and drugs should be brought into theatre to reduce the number of items that need to be cleaned or discarded following the procedure. A runner, stationed outside the operating theatre, should be available if additional drugs or equipment are needed.6,11,13 Anaesthetic monitors, laptop computers and ultrasonography machine surfaces should be covered with plastic wrap to decrease the risk of contamination and to facilitate cleaning.
The patient should be examined, induced and recovered in the operating theatre itself to restrict contamination to just one room. The surgical team will don scrubs following the usual procedure for performing surgery but replacing the surgical mask with a FFP2 mask, wearing high shoe protection and a waterproof gown. Eye protection (goggles) or facial protection (face mask) should be always worn.
At the end of the operation, surgeons and all staff who are not directly involved in the care of the patient should leave the operating theatre and descrub in the ante-room, following the recommendations. All staff must shower and change into a clean set of scrubs before resuming their regular duties. Any used PPE must be disposed of in containers for infectious waste.
The operating theatre must be sanitised as soon as possible after each operation. After operating on patients with confirmed COVID-19, a hydrogen peroxide vaporiser should be used to decontaminate the operating theatre. Human coronaviruses can be efficiently inactivated by surface disinfection procedures with 62–71% ethanol, 0.5% hydrogen peroxide or 0.1% sodium hypochlorite within one minute. Other biocidal agents such as 0.05–0.2% benzalkonium chloride or 0.02% chlorhexidine digluconate are less effective.34 All safe procedures to be performed after surgery are summarised in Table 6.
Table 6.
Safe procedures to be performed after surgery during the COVID-19 pandemic
| • All staff must shower and change into a clean set of scrubs before resuming their regular duties. |
| • Any personal protective equipment used must be disposed of in containers for infectious waste. |
| • The name of all participating staff members should be recorded to facilitate contact tracing. |
| • The operating theatre must be sanitised as soon as possible. Human coronaviruses can be efficiently inactivated by surface disinfection procedures with 62–71% ethanol, 0.5% hydrogen peroxide or 0.1% sodium hypochlorite within one minute. Other biocidal agents such as 0.05–0.2% benzalkonium chloride or 0.02% chlorhexidine digluconate are less effective.34 |
Discussion
Given its rapid spread and its severity, COVID-19 infection can be considered a mass casualty incident as it is an event resulting in more ‘injured’ patients than hospital systems can handle with standard protocols.55 From the beginning of this pandemic, surgical theatres have been converted into additional ICUs, and non-urgent, non-cancer surgical procedures were stopped to reallocate nurses and anaesthetists, and to free up ventilators. Patients with cancer were prioritised according to the availability of resources; patients requiring postoperative ICU admission were transferred to specific government defined centres in order to enable vital resources to be used elsewhere.7
In order to ensure safe management of apparently healthy patients presenting with an emergency surgical disease, hospitals were divided into hub COVID-19 positive and COVID-19 negative facilities, a temporary measure. In every hub COVID hospital, coordination between the anaesthesiologist and the emergency surgeon is fundamental to better use of limited resources and minimising the risk of exposure. There is no consensus on whether dedicated COVID-19 staff should be allocated to infected patients requiring surgery.
Moreover, patients are not yet being routinely tested for COVID-19, especially if they are asymptomatic. Evidence suggests that even someone who is asymptomatic could spread COVID-19 with high contagiousness. This implies that all surgical patients should be considered as possibly COVID-19 positive in order to limit the contamination of healthcare workers. The increasing number of infected physicians warrants aggressive measures of protection (PPE, N95 masks, goggles or face mask and protective gowns).4
Conclusions
Emergency surgeons need to ensure the management of surgical patients with a high standard of care during the COVID-19 pandemic. They must evaluate whether it is possible to postpone surgical treatment until the patient is no longer considered potentially infectious or at risk of perioperative complications. If an emergency surgical procedure is necessary (life threatening situation, high risk patient, haemodynamic compromise or shock), the emergency surgeon must supervise the implementation of safety measures in the operating theatre. Trained staff, adequate instruments and strict application of the recommendations are crucial to avoid increasing the risk of contamination. In case of a lack of skills or adapted materials enabling a safe laparoscopic surgical intervention, laparotomy should be preferred.
During the COVID-19 pandemic, healthcare workers have been overwhelmed and ICUs overcrowded as respiratory support is required for the majority of COVID-19 patients. Consequently, we recommend careful evaluation of every surgical indication on a case-by-case basis.
References
- 1.World Health Organization Coronavirus Disease 2019 (COVID-19) Situation Report –71. Geneva: WHO; 2020. [Google Scholar]
- 2.Moher D, Shamseer L, Clarke M et al. Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev 2015; : 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrett WL, Garber SM. Surgical smoke: a review of the literature. Is this just a lot of hot air? Surg Endosc 2003; : 979–987. [DOI] [PubMed] [Google Scholar]
- 4.Chang D, Xu H, Rebaza A et al. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med 2020; : e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Saverio S, Pata F, Gallo G et al. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis 2020. March 31 [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 6.Kamer E, Çolak T. What to do when a patient infected with COVID-19 needs an operation: a pre-surgery, peri-surgery and post-surgery guide. Turk J Colorectal Dis 2020; : 1–8. [Google Scholar]
- 7.Luo Y, Zhong M. Standardized diagnosis and treatment of colorectal cancer during the outbreak of corona virus disease 2019 in Renji hospital. Zhonghua Wei Chang Wai Ke Za Zhi 2020; : 211–216. [DOI] [PubMed] [Google Scholar]
- 8.Ong SW, Tan YK, Chia PY et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020. March 4 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pellino G, Spinelli A. How COVID-19 outbreak is impacting colorectal cancer patients in Italy: a long shadow beyond infection. Dis Colon Rectum 2020. March 17 [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 10.Spinelli A, Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg 2020. March 19 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ti LK, Ang LS, Foong TW, Ng BS. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth 2020. March 6 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Doremalen N, Bushmaker T, Morris D et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New Engl J Med 2020. April 16 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wen X, Li Y. Anesthesia procedure of emergency operation for patients with suspected or confirmed COVID-19. Surg Infect 2020; : 299. [DOI] [PubMed] [Google Scholar]
- 14.Yu GY, Lou Z, Zhang W. Several suggestions of operation for colorectal cancer under the outbreak of corona virus disease 2019 in China. Zhonghua Wei Chang Wai Ke Za Zhi 2020; : 208–211. [DOI] [PubMed] [Google Scholar]
- 15.Andersen KG, Rambaut A, Lipkin WI et al. The proximal origin of SARS-CoV-2. Nat Med 2020; : 450–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cascella M, Rajnik M, Cuomo A et al. Features, Evaluation and Treatment Coronavirus (COVID-19). https://www.ncbi.nlm.nih.gov/books/NBK554776 [updated 2020 Mar 8]. [PubMed] [Google Scholar]
- 17.Guo YR, Cao QD, Hong ZS et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil Med Res 2020; : 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van der Hoek L, Pyrc K, Jebbink MF et al. Identification of a new human coronavirus. Nat Med 2004; : 368–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao Y, Zhao Z, Wang Y et al. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. bioRxiv 2020. January 26 [Epub ahead of print.] [Google Scholar]
- 20.Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; : 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guan WJ, Ni ZY, Hu Y et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020. February 28 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020. February 24 [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 23.Li JO, Lam DS, Chen Y, Ting DS. Novel coronavirus disease 2019 (COVID-19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol 2020; : 297–298. [DOI] [PubMed] [Google Scholar]
- 24.Loon SC, Teoh SC, Oon LL et al. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol 2004; : 861–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol 2020; : 441–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shi H, Han X, Jiang N et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020; : 425–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu X, Yu C, Qu J et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging 2020; : 1275–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang X, Yu Y, Xu J et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020. February 24 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA 2020. April 13 [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization Coronavirus disease (COVID-19) advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (cited April 2020). [Google Scholar]
- 31.Centers for Disease Control and Prevention How to protect yourself & others. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.htm (cited April 2020).
- 32.Bai Y, Yao L, Wei T et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020. February 21 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology 2020. March 3 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020; : 246–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wong J, Goh QY, Tan Z et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth 2020. March 11 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sartelli M, Chichom-Mefire A, Labricciosa FM et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg 2017; : 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Di Saverio S, Podda M, De Simone B et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 2020; : 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ansaloni L, Pisano M, Coccolini F et al. 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg 2016; : 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Loozen CS, van Santvoort HC, van Duijvendijk P et al. Laparoscopic cholecystectomy versus percutaneous catheter drainage for acute cholecystitis in high risk patients (CHOCOLATE): multicentre randomised clinical trial. BMJ 2018; : k3965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sartelli M, Catena F, Ansaloni L et al. WSES guidelines for the management of acute left sided colonic diverticulitis in the emergency setting. World J Emerg Surg 2016; : 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pisano M, Zorcolo L, Merli C et al. 2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation. World J Emerg Surg 2018; : 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ten Broek RP, Krielen P, Di Saverio S et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the World Society of Emergency Surgery ASBO working group. World J Emerg Surg 2018; : 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.De Simone B, Birindelli A, Ansaloni L et al. Emergency repair of complicated abdominal wall hernias: WSES guidelines. Hernia 2020; : 359–368. [DOI] [PubMed] [Google Scholar]
- 44.Arnold M, Elhage S, Schiffern L et al. Use of minimally invasive surgery in emergency general surgery procedures. Surg Endosc 2020; : 2258–2265. [DOI] [PubMed] [Google Scholar]
- 45.Jimenez Rodriguez RM, Segura-Sampedro JJ, Flores-Cortés M et al. Laparoscopic approach in gastrointestinal emergencies. World J Gastroenterol 2016; : 2701–2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lupinacci RM, Menegaux F, Trésallet C. Emergency laparoscopy: role and implementation. J Visc Surg 2015; (6 Suppl): S65–S71. [DOI] [PubMed] [Google Scholar]
- 47.Mandrioli M, Inaba K, Piccinini A et al. Advances in laparoscopy for acute care surgery and trauma. World J Gastroenterol 2016; : 668–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nielsen LB, Tengberg LT, Bay-Nielsen M. Laparoscopy in major abdominal emergency surgery seems to be a safe procedure. Dan Med J 2017; : A5370. [PubMed] [Google Scholar]
- 49.Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg 2020. March 26 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang J, Du G. COVID-19 may transmit through aerosol. Ir J Med Sci 2020. March 24 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen YC, Huang LM, Chan CC et al. SARS in hospital emergency room. Emerg Infect Dis 2004; : 782–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Royal College of Surgeons of England. Updated intercollegiate general surgical guidance on COVID-19. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2 (cited April 2020).
- 53.Kwak HD, Kim SH, Seo YS, Song KJ. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup Environ Med 2016; : 857–863. [DOI] [PubMed] [Google Scholar]
- 54.Coccolini F, Roberts D, Ansaloni L et al. The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Emerg Surg 2018; : 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ben-Ishay O, Mitaritonno M, Catena F et al. Mass casualty incidents – time to engage. World J Emerg Surg 2016; : 8. [DOI] [PMC free article] [PubMed] [Google Scholar]