Abstract
Just over 11% of babies worldwide are born preterm (before 37 weeks of pregnancy) putting them at risk for problems with their heart, lungs, eyes, and brain development.1 Previous studies have suggested outdoor air pollution exposure may be a risk factor for preterm birth.2,3 Much of this research has focused on traffic-related air pollution. A recent study in Environmental Health Perspectives reports on the association between preterm birth and another source of air pollution—aircraft emissions.4
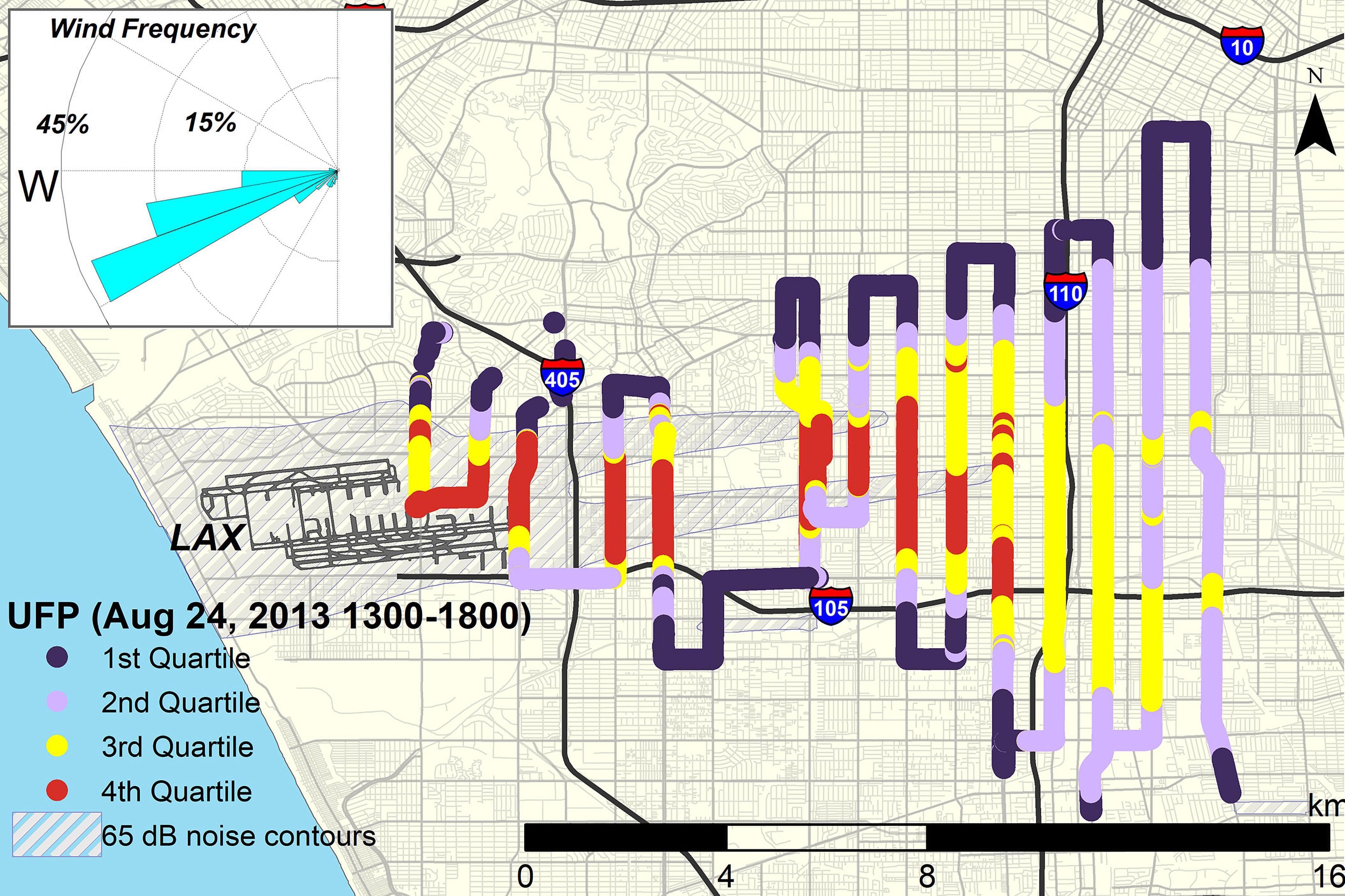
After modeling UFP exposures downwind of LAX, the authors of a new study estimated that pregnant women up to from the airport could potentially be exposed to concentrations over 2.5 times baseline levels. Image: Wing et al. (2020).4
The study focused on exposures to ultrafine particles (UFPs), which are less than in aerodynamic diameter. On an equal mass basis, UFPs may have a greater impact on tissues than larger particles—their small size allows them to move freely throughout the body, and their greater surface areas allow them to adsorb more toxic chemicals.5 However, UFPs are not routinely monitored or regulated by state or federal governments.6
Although there is evidence that UFPs can cross the placenta,7 it is not clear exactly how these particles might contribute to prematurity. However, experiments in mouse and human cells suggest that UFP exposures can cause inflammation and oxidative stress,8 which have been associated with preterm birth.9
For the new research, first author Sam Wing, a PhD candidate at the University of California, Los Angeles (UCLA), was guided by co–senior authors Scott Fruin of the University of Southern California Keck School of Medicine and Beate Ritz of UCLA. The investigators modeled preterm birth risk due to aircraft UFP emissions downwind of Los Angeles International Airport (LAX). Fruin and coauthor Tim Larson of the University of Washington first created a novel dispersion model for UFPs that assumed two steady-state incoming flight paths. The model was validated using mobile air measurements of daytime UFP concentrations that Fruin had previously collected10 around LAX. In that earlier testing, landings appeared to account for a large fraction of UFPs dispersed downwind of the airport.10
The authors then reviewed records for all births between 2008 and 2016 to mothers living within of the airport. They adjusted for nitrogen dioxide as a proxy for nearby traffic-related air pollution as well as for other variables that may affect risk of preterm birth, including airport-related noise and mother’s age, education level, and race.
Ultimately, the researchers estimated that expectant mothers in the highest quartile of average UFP exposure were about 14% more likely to have a preterm birth than mothers in the lowest quartile. “The data suggest that airplane pollution contributes to preterm births above and beyond the main source of air pollution in this area, which is traffic,” says Ritz.
“In many urban areas, airports are located very close to population centers. It is important to recognize that not just traffic but also airport emissions can have adverse impacts on preterm births and potentially other health outcomes,” says Jun Wu, an epidemiologist at the University of California, Irvine, who was not involved in the study. Furthermore, Wu says, while the impact of aircraft UFP pollution on preterm births may appear small in relative terms, the potential risk could be important on the population level since so many people worldwide live near airports.
The researchers could not confirm how much time the pregnant women may have spent at home, exposed to airport UFP pollution, or whether they lived in climate-controlled homes with indoor air filtering systems. Time spent outside the home or farther from the airport also would have affected their exposure levels.
Future studies could explore whether similar associations are seen in pregnant women living near other airports around the world, Ritz says. They also could look at biomarkers in mothers’ blood or urine to better understand how UFPs behave in the body, she says, noting that some mothers may have stronger reactions than others. Wing adds, “Hopefully, more studies like this can start to drive the conversation about plans to measure and regulate these particles.”
Biography
Lindsey Konkel is a New Jersey–based journalist who reports on science, health, and the environment.
References
- 1.Blencowe H, Cousens S, Chou D, Oestergaard MZ, Say L, Moller A-B, Kinney M, Lawn J. 2012. Chapter 2. 15 million preterm births: priorities for action based on national, regional and global estimates In: Born Too Soon: The Global Action Report on Preterm Birth. Geneva, Switzerland: World Health Organization; March of Dimes; Partnership for Maternal, Newborn, & Child Health; Save the Children, 16–31. https://www.who.int/pmnch/knowledge/publications/preterm_birth_report/en/index1.html [accessed 24 June 2020]. [Google Scholar]
- 2.Klepac P, Locatelli I, Korošec S, Künzli N, Kukec A. 2018. Ambient air pollution and pregnancy outcomes: a comprehensive review and identification of environmental public health challenges. Environ Res 167:144–159, PMID: 30014896, 10.1016/j.envres.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Wu J, Ren C, Delfino RJ, Chung J, Wilhelm M, Ritz B. 2009. Association between local traffic-generated air pollution and preeclampsia and preterm delivery in the South Coast Air Basin of California. Environ Health Perspect 117(11):1773–1779, PMID: 20049131, 10.1289/ehp.0800334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wing SE, Larson TV, Hudda N, Boonyarattaphan S, Fruin S, Ritz B, et al. . 2020. Preterm birth among infants exposed to in utero ultrafine particles from aircraft emissions. Environ Health Perspect 128(4):47002, PMID: 32238012, 10.1289/EHP5732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.HEI Review Panel on Ultrafine Particles. 2013. Understanding the Health Effects of Ambient Ultrafine Particles. HEI Perspectives 3. Boston, MA: Health Effects Institute; https://www.healtheffects.org/system/files/Perspectives3.pdf [accessed 24 June 2020]. [Google Scholar]
- 6.U.S. EPA (U.S. Environmental Protection Agency). 2020. Policy Assessment for the Review of the Particulate Matter National Ambient Air Quality Standards. EPA-452/R-20-002. https://www.epa.gov/sites/production/files/2020-01/documents/final_policy_assessment_for_the_review_of_the_pm_naaqs_01-2020.pdf [accessed 24 June 2020].
- 7.Bové H, Bongaerts E, Slenders E, Bijnens EM, Saenen ND, Gyselaers W, et al. . 2019. Ambient black carbon particles reach the fetal side of the human placenta. Nat Commun 10(1):3866, PMID: 31530803, 10.1038/s41467-019-11654-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li N, Sioutas C, Cho A, Schmitz D, Misra C, Sempf J, et al. . 2003. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect 111(4):455–460, PMID: 12676598, 10.1289/ehp.6000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferguson KK, McElrath TF, Chen Y-H, Loch-Caruso R, Mukherjee B, Meeker JD. 2015. Repeated measures of urinary oxidative stress biomarkers during pregnancy and preterm birth. Am J Obstet Gynecol 212(2):208.e1–208.e8, PMID: 25111586, 10.1016/j.ajog.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hudda N, Gould T, Hartin K, Larson TV, Fruin SA. 2014. Emissions from an international airport increase particle number concentrations 4-fold at 10 km downwind. Environ Sci Technol 48(12):6628–6635, PMID: 24871496, 10.1021/es5001566. [DOI] [PMC free article] [PubMed] [Google Scholar]


