ACE2 (angiotensin-converting enzyme 2) degrades Ang (angiotensin) I and II and is a cellular receptor for SARS-CoV-2, the virus that causes coronavirus disease 2019 (COVID-19). Viral entry into host cells occurs through binding of the viral spike (S) protein and ACE2.1 Preclinical data suggest that renin-angiotensin system (RAS) blockers upregulate ACE2.2,3 As a consequence, RAS blockers have been suggested to increase the risk of developing severe SARS-CoV-2 infection. However, recent large retrospective studies strongly argue against this hypothesis and rather suggest that RAS blockers be protective in such patients.4 Since the findings on RAS blocker-induced ACE2 upregulation are inconsistent, and differed not only per type of RAS inhibitors (ACE inhibitors versus ARB [angiotensin receptor blockers]),3 between blockers of a certain type (ie, between various ARBs), but also per organ, and required high doses, one further option is that this ACE2 upregulation is not the unavoidable consequence of RAS suppression, but rather reflects the nonspecific effects of a certain RAS blocker when applied at a high dose. Applying antisense oligonucleotides (ASO) as a tool to suppress the RAS would circumvent the latter. In the present study, we determined effects of an ACE inhibitor (enalapril) and an ARB (losartan) as well as AGT (angiotensinogen) ASO on tissue ACE2 in male C57BL/6J mice.
After 14 days of infusion, both enalapril and losartan increased plasma renin, measured as direct concentrations, by over 100-fold, confirming effective RAS inhibition (Figure [A]). ACE2 mRNA abundance was determined by quantitative PCR in lung, ileum, kidney, and heart tissues. Neither enalapril nor losartan changed the abundance of ACE2 mRNA in any of the tissues (Figure [B]). Ferrario et al3 reported that administration of lisinopril (an ACE inhibitor) or losartan for 12 days increases ACE2 mRNA abundance ≈3- to 5-fold in male rat heart. It is worth noting that ACE2 mRNA is much less abundant in heart compared with lung, ileum, and kidney (data not shown).
Figure.
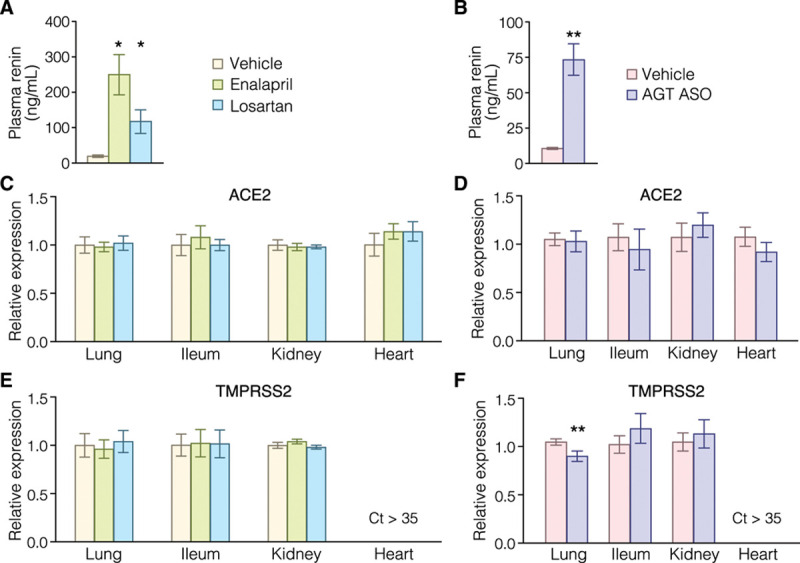
Effects of enalapril, losartan, and AGT (angiotensinogen) antisense oligonucleotides (ASO) on ACE2 and TMPRSS2 (transmembrane protease serine 2) mRNA abundance. A–C, Male C57BL/6J mice were infused subcutaneously with either enalapril (3 mg/kg perday) or losartan (15 mg/kg perday) for 14 days. D–F,Male C57BL/6J mice were administered AGT ASO (80 mg/kg at day 1 and 4, 40 mg/kg at day 8 and 15) or vehicle (PBS) subcutaneously. Plasma renin (A and D) were measured by ELISA. B, C, E, andF, ACE2 and TMPRSS2 mRNA abundance were quantified by qPCR with TaqMan probes (ID: Mm01159003_m1 and ID: Mm00443687_m1, respectively) and normalized to the geomean of three reference genes: ACTB, GAPDH, and PPIA. Genes with a cycle threshold (Ct) >35 were considered undetectable. Error bars denote SEM; n=5/group. *P<0.001 vs vehicle, 1-way ANOVA with Holm-Sidak method. **P<0.05 vs vehicle, Student ttest.
Viral entry also depends on TMPRSS2 (transmembrane protease serine 2) to prime S protein.1 TMPRSS2 mRNA was highly abundant in lung and ileum, moderately in kidney, while barely detectable in heart (data not shown). Thus, ACE2 and TMPRSS2 are co-expressed most abundantly in lung and ileum, consistent with their roles in SARS-CoV-2 infection. As with ACE2, TMPRSS2 mRNA abundance was not altered by either enalapril or losartan (Figure [C]).
Next, we determined whether depletion of AGT, the unique substrate of the RAS, changes ACE2 and TMPRSS2 mRNA abundance. AGT ASO led to elevation of plasma renin concentrations, an immediate consequence of RAS blockade (Figure [D]). However, abundance of ACE2 mRNA was unchanged in all tissues (Figure [E]). Interestingly, AGT ASO significantly decreased TMPRSS2 mRNA abundance in lungs (Figure [F]).
In summary, RAS inhibition did not affect mRNA abundance of ACE2 in male C57BL/6J mice administered enalapril, losartan, or AGT ASO. AGT ASO reduces TMPRSS2 mRNA expression in lungs, which is potentially protective against viral entry. These data support that RAS inhibition per se does not regulate ACE2 and hence is unlikely to increase the risk for COVID-19. In agreement with this concept, Sama et al5 recently were unable to detect changes in circulating ACE2 in patients taking RAS inhibitors.
Sources of Funding
C.Wu is an National Institutes of Health (NIH)/NHLBI K99 awardee. This work was supported by NIH grants K99HL145117 and R01HL139748.
Disclosures
A. Daugherty and H.S. Lu filed a patent application for use of AGT (angiotensinogen) antisense oligonucleotides (ASO) in aortic aneurysmal disease. A.E. Mullick is an employee in Ionis Pharmaceuticals, Inc, who provided the AGT ASO. The other authors report no conflicts.
Footnotes
C. Wu and D. Ye are joint first authors.
References
- 1.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020; 181:271–280.e8. doi: 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danser AHJ, Epstein M, Batlle D. Renin-angiotensin system blockers and the COVID-19 pandemic: at present there is no evidence to abandon renin-angiotensin system blockers. Hypertension. 2020; 751382–1385. doi: 10.1161/HYPERTENSIONAHA.120.15082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, Diz DI, Gallagher PE. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005; 111:2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461 [DOI] [PubMed] [Google Scholar]
- 4.Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin-angiotensin-aldosterone system inhibitors in patients with covid-19. N Engl J Med. 2020; 382:1653–1659. doi: 10.1056/NEJMsr2005760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sama IE, Ravera A, Santema BT, van Goor H, Ter Maaten JM, Cleland JGF, Rienstra M, Friedrich AW, Samani NJ, Ng LL, Dickstein K, Lang CC, Filippatos G, Anker SD, Ponikowski P, Metra M, van Veldhuisen DJ, Voors AA. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J. 2020; 41:1810–1817. doi: 10.1093/eurheartj/ehaa373 [DOI] [PMC free article] [PubMed] [Google Scholar]


