Abstract
During the unprecedented times of the COVID 19 pandemic, the lives of people with diabetes have been severely impacted. This article discusses the extent of this impact presenting the obstacles and challenges from the perspective of the patient, including specifics of practical day-to-day diabetes self-management routines. Since the COVID19 outbreak, certain psychosocial factors have been amplified due to the manner in which mainstream media and policy makers have carelessly emphasized the vulnerability of people with diabetes. The authors discuss the increased importance of support networks due to people living in isolation and quarantine. A new layer of complexity has been added to the already difficult task of managing one's diabetes and it has increased anxiety and stress levels. Guidelines and tips for people living with diabetes are discussed based on the authors' personal experiences as well as those of the diabetes associations they work with.
Keywords: COVID19, Pandemic, People with diabetes, Patient perspective, Stress, Psychosocial, Anxiety, Diabetes management, Peer support, Diabetes self-management, Quality of life, Behavioural change
1. Introduction
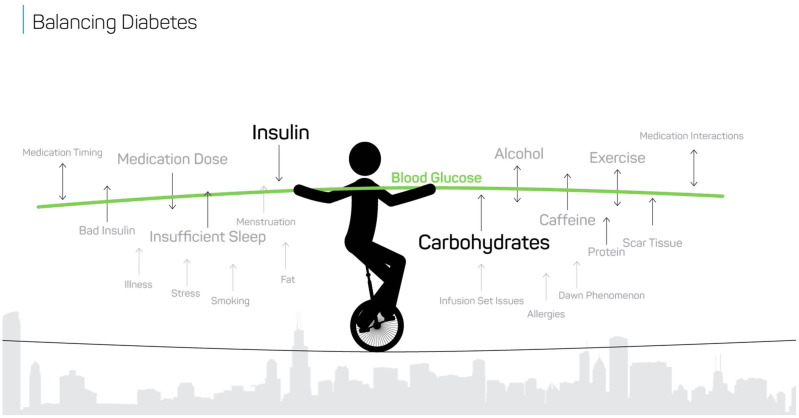
Living with diabetes is complex and can be overwhelming (see Fig. 1 ). Add a global pandemic to the already monumental expectations placed on us to live healthily and maintain glucose levels in range, and it’s not surprising that many people with diabetes are finding these trying times especially difficult (see Fig. 2 ).
Fig. 1.
Quote about diabetes management.
Fig. 2.
Source: Bigfoot Biomedical.
2. Impact of the pandemic
COVID-19 has exacerbated many factors involved in diabetes care and increased stress. Uncertainty around the new virus is frightening, and many people have the additional worry of loss of income [1]. The pandemic has severely disrupted routine diabetes self-management, including:
-
–
Food – Scarcity of healthy foods, as well as having to change diets, makes consistent diabetes management challenging. Certain products are not available. Many restaurants and stores have closed or changed their hours.
-
–
Medicine – Going to the pharmacy or seeing your doctor has become more difficult, and some people have reported problems when trying to refill prescriptions. Due to the risk of exposure to the virus, people are concerned about attending appointments, opting for telehealth/telemedicine when possible.
-
–
Physical Activity – There are obstacles to maintaining exercise, an essential element in diabetes therapy. Space is limited in our homes, parks and gyms are closed and many people face restrictions to leaving the house.
Diabetes management is not only about glucose numbers. It is also about emotional well-being and mental health [2]. During the pandemic, many people with diabetes have felt more anxious, even scared, about situations out of their control. While going into lockdown keeps us safe, it also has meant that our social circles, critical for support, have shrunk. Not knowing how or when this will end can increase anxiety levels.
3. Diabetes and COVID19
As has been widely reported, the elderly and people with chronic health conditions, such as diabetes, are considered especially vulnerable to complications of COVID-19 [3]. The dismissive and insensitive manner in which this has been repeated by the media and policy makers has been upsetting for many of us. We feel ‘disposable’. In addition to this constant reminder of our vulnerability are the often-unwelcome comments from the general community about how we should manage our diabetes. Although frequently well-intentioned, this ‘advice’ creates enormous pressure, and adds to the already considerable social stigma we face [4]. These comments rarely help and instead make us feel that we are being judged.
Support from our peers is particularly important during these unprecedented times. Most often, it is those with first-hand diabetes experience who understand how difficult it is to achieve in-range glucose levels, and how COVID-19 is impacting us. Lifestyle changes, many imposed on us by this pandemic, are difficult and add to the arduous daily management tasks diabetes demands [5]. Additionally, diabetes impacts us all in very different ways [2].
Rarely do two individuals react the exact same way to the exact same factor and there are many variables to consider [6]. People with diabetes try to balance everything simultaneously while using glucose monitoring technology as a guide. Often, it is a nonstop, all-consuming job which can be overwhelming enough without facing a pandemic.
In the current environment, the following suggestions may be helpful.
-
–
Make sure you have all your diabetes supplies and medications. Stockpiling prevents others from obtaining what they need, however, having at least a month’s supply available is wise, if possible. Specific items such as alcohol swabs have had intermittent supply disruption, but global manufacturers of diabetes medications/medical devices have stated no disruption in the supply chain is foreseen. This provides reasonable assurances, particularly for those of us living in the developed world. Unfortunately, we are aware of a number of areas where there was already an inconsistent supply of life-saving drugs such as insulin. There are also certain ‘hot-zones’ where COVID-19 lockdowns have impacted insulin distribution and delivery. There are a number of manufacturer programs intended to assist people experiencing difficulties during the pandemic. Check with manufacturers’ local affiliates or distributors and also relevant humanitarian programs such as Life for a Child and Insulin for Life.
-
–
Stay connected to your support networks. Use social media, virtual meetings and call friends with diabetes to share how you are doing.
-
–
Keep in touch with your healthcare team, especially for urgent care. Other medical problems don’t stop during COVID-19, so it’s important to seek help when you feel something is not right. An important example is keeping alert for signs of diabetic ketoacidosis.
-
–
Do the best with the situation around you. In certain areas, particularly those with high population density, social distancing/PPE guidelines cannot be followed all the time. If proper infrastructure is not in place, for example, in factories, markets, schools, hospitals, or on public transport, families of people with diabetes should take as many precautions as possible. We understand that culture and society will not change overnight, but unfortunately COVID-19 won’t wait so it is important to address these risks as best as you can.
-
–
Be safe. Wash hands frequently, maintain physical distance, wear personal protective equipment such as masks, and avoid large gatherings.
-
–
Whether you receive your news via television, radio, or internet/social media, if the constant stream is making you anxious, consider taking a break! It can be exhausting to hear about matters beyond our control day-after-day. Rely on trusted sources of information, such as local diabetes organizations and the WHO.
4. Conclusion
At a time when there is so much uncertainty, added stress in our daily lives is to be expected. Since diabetes doesn’t allow us to take a break, it’s important to adopt a methodical approach to reducing risks where possible, keeping in mind that we all need support from time to time. Together we are stronger, even with an extra few meters of space between us!
Funding
The authors received no funding from an external source.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Reference
- 1.“Tracking the impact of COVID-19 on the diabetes community in the United States” Report, dQ&A – The Diabetes Research Company, 07-May-2020: San Francisco.
- 2.Young-Hyman D., et al. Psychosocial care for people with diabetes: a position statement of the ADA. Diabetes Care. 2016 Dec;39(12):2126–2140. doi: 10.2337/dc16-2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hussein A, et al. COVID-19 and diabetes: knowledge in progress. Diabetes Research and Clinical Practice; 2020 Apr 9: 108142. [DOI] [PMC free article] [PubMed]
- 4.Browne JL, et al. ‘I call it the blame and shame disease’: a qualitative study about perceptions of social stigma surrounding type 2 diabetes. [DOI] [PMC free article] [PubMed]
- 5.Unger, Jeff. Diabetes Management in Primary Care. Philadelphia, USA: Lippincott Williams & Wilkins; 2013. p. 397–398.
- 6.https://diatribe.org/42factors (Diatribe: October 2019).