Highlights
-
•
The exposure risk of SARS-CoV-2 in diverse environments in hospital was compared.
-
•
The nucleic acid of SARS-CoV-2 in air and surfaces suggested the potential risk.
-
•
It is necessary to monitor and disinfect the SARS-CoV-2 in hospital environment.
-
•
Ventilation, sterilization may help to reduce the potential risk for HCWs.
-
•
Different strategies were discussed in combating infectious disease.
Keywords: COVID-19, SARS-CoV-2, Nucleic acid test, HCWs, Occupational exposure risk
Abstract
The ongoing coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has imposed a significant impact on social and economic activities. As a high infectious pathogen, the existence of SARS-CoV-2 in public space is very important for its transmission. During the COVID-19 pandemic, hospitals are the main places to deal with the diseases. In this work, we evaluated the exposure risk of SARS-CoV-2 in hospital environment in order to protect healthcare workers (HCWs). Briefly, air and surface samples from 6 different sites of 3 hospitals with different protection levels were collected and tested for the SARS-CoV-2 nucleic acid by reverse transcription real-time fluorescence PCR method during the COVID-19 epidemic. We found that the positive rate of SARS-CoV-2 nucleic acid was 7.7 % in a COVID-19 respiratory investigation wards and 82.6 % in a ICUs with confirmed COVID-19 patients. These results indicated that in some wards of the hospital, such as ICUs occupied by COVID-19 patients, the nucleic acid of SARS-CoV-2 existed in the air and surface, which indicates the potential occupational exposure risk of HCWs. This study has clarified retention of SARS-CoV-2 in different sites of hospital, suggesting that it is necessary to monitor and disinfect the SARS-CoV-2 in hospital environment during COVID-19 pandemic, and will help to prevent the iatrogenic infection and nosocomial transmission of SARS-CoV-2 and to better protect the HCWs.
1. Introduction
To 19 June 2020, there have been 8,242,999 confirmed cases of coronavirus disease 2019 (COVID-19), including 445,535 deaths, reported to World Health Organization (WHO), which was declared as a pandemic and global public health emergency by the WHO. The ongoing COVID-19 seriously threatens global health, and has a significant impact on social and economic activities (Huang et al., 2020; Lai, Shih, Ko, Tang, & Hsueh, 2020; Li, Guan et al., 2020; Munster, Koopmans, van Doremalen, van Riel, & de Wit, 2020; Wang, Horby, Hayden, & Gao, 2020). Mitigating the adverse economic impact of COVID-19 lockdown is the significant concern to maintain the normal social activities and sustainable development of society (Rahman, 2020). The causative pathogen of the COVID-19 was identified as a new strain of coronavirus named the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses (ICTV) (Lu, Stratton, & Tang, 2020; WHO, 2020a). The SARS-CoV-2 is highly infectious and has showed a high transmissibility whose R0 value is estimated as 2.3 but could be as high as 5.7 (Bulut & Kato, 2020; Zhang, 2020). Recent studies showed that close contact with infected individuals, viral droplets and surfaces contaminated by SARS-CoV-2 could lead to the transmission of SARS-CoV-2 among people (Diseases, 2020). In addition, clinical observations and retrospective surveys have suggested that the aerosol transmission may be an important pathway for viral transmission, especially in the crowded place and enclosed space (Berlanga et al., 2020; WHO, 2020b; Zhang et al., 2019). Creating an antivirus-built environment could help for virus prevention and control and to overcome future challenges and to build healthy cities (Megahed & Ghoneim, 2020; Xu, Luo, Yu, & Cao, 2020).
Wuhan City in Hubei Province is the most seriously affected city in China by the COVID-19 since the emergence of the SARS-CoV-2 in December 2019 (Chen et al., 2020; Chung & Li, 2020; Munster et al., 2020). After the outbreak of the COVID-19, healthcare workers (HCWs) from other provinces have assembled in Wuhan to fight against the epidemic (Jin et al., 2020; Wang, Hu et al., 2020). Unfortunately, since little was known about the new virus in the early stages of the epidemic, some HCWs were exposed to high-risk environment and infected by SARS-CoV-2 (Prevention, 2020). So far, the HCWs are still the high-risk group in the global combating against COVID-19. Nosocomial outbreaks threaten the health of HCWs in most epidemics. The 2003 severe acute respiratory syndrome (SARS) outbreak led to over 900 HCWs infections in the mainland of China (China, 2003). The working environment of HCWs is the potential risk of their infection (Anderson et al., 2017; Beggs, Knibbs, Johnson, & Morawska, 2015). However, the existence of SARS-CoV-2 in different areas of hospital has not been fully revealed.
In order to better prevent nosocomial infections, reduce occupational exposure to HCWs and make more efficient use of protective devices, Chinese National Health and Health Commission has initiated hierarchical management of the nosocomial environment (China, 2020). According to the Circular of the General Office of the National Health and Health Commission on Printing and Distributing Guidelines on the Scope of Use of Common Medical Protective Equipment in Prevention and Control of Pneumonia Infected in novel coronavirus (Trial) (Medical letter of the General Office of the National Health and Health Commission No.75 [2020]), and based on the probability of contact with COVID-19 confirmed patients, hospital areas have been classified to different protection levels of Level 1 to Level 3 (See support information Table S1). However, the degree of environmental risk varies in different areas of the same ward (Beggs et al., 2015; Phan et al., 2020). By evaluating the environmental conditions of public space in the hospital, appropriate protection measures could be taken to protect HCWs better.
2. Method
2.1. Environmental characteristics
In this research, we chose one Level 1 protection site (hemodialysis room of Xiangya hospital), one Level 1.5 protection site (general fever clinic of Xiangya hospital), one Level 2 protection sites (COVID-19 respiratory investigation ward of Xiangya hospital), and three Level 3 protection sites (virus nucleic acid laboratory of Xiangya hospital, COVID-19 confirmed patient ward of Chenzhou second people's hospital and the confirmed intensive care patient's ward of Shaoyang central hospital). For easy reference in this study, these three hospitals were named as: Xiangya Hospital (H-X), Chenzhou Second People's Hospital (H-C), and Shaoyang Central Hospital (H-S), respectively.
Because H-X is not a designated hospital of COVID-19, once the patient is diagnosed confirmed, who will be transferred out of the hospital immediately. So confirmed cases usually stayed in hospital only for a short period of time. There were no positive samples reported in the virus nucleic acid laboratory within 9 days before the day of sampling. There were 9 confirmed patients in H-C, and all of them were mild cases. The date of their last nucleic acid positive test was earlier than the environmental sampling at least one week, and all of their IgM antibody tests results were positive on the day of sampling. In H-S, the nucleic acid test of the severe patient was still positive at the day before environmental sampling.
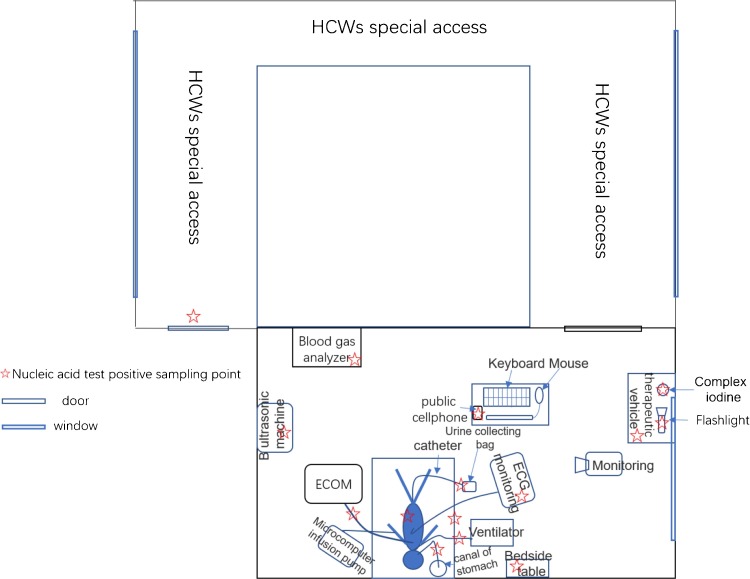
The severe patient in H-S was an 83-year old male. He was already in coma at that time, had been intubated and invasive ventilator-assisted ventilation. He was also indwelling catheterization, indwelling gastric tube, with PICC catheter, intravenous infusion port. Because the virus invaded the lungs, leading to pulmonary diffuse dysfunction, invasive ventilator could not meet his treatment needs. The patient was receiving ECOM membrane lung treatment at the same time. This patient's nucleic acid test was still positive on February 28. On the evening of February 28, this patient was rescued overnight. On the morning of February 29, the patient had just recovered to calm. During the sampling period, medical treatment and nursing operations were still very frequent. There were almost non-stop operations within half an hour, such as feeding medicine in gastric tube, replacing infusion pump, emptying urine bag, adjusting ventilator parameters, sputum suction, nursing at intubation port, turning over, etc. HCWs wiped or sprayed disinfection after every operation, and routine disinfection was acted every 4 h.
2.2. Environment sampling
Environmental health monitoring was carried out according to "Hospital Disinfection Health Standard" (GB15982-2012). All air samples were collected for 30 min using the National Institute for Occupational Safety and Health (NIOSH) bioaerosol sampler (BC251) with air pumps (XR5000, SKC) (Xie et al., 2020). The stream of air has been set to 3.5 L / minute. The NIOSH sampler works by pulling air into a round chamber and swirling the air around like a cyclone. Particles in the air were thrown against the wall of the chamber by centrifugal force, where they collect. The NIOSH sampler divided air sample into large particles (4 μm and larger), medium particles (1–4 μm) and small particles (<1 μm) according to their size. Environmental surfaces were sampled using swabs by scrubbing the object surfaces. After sampling, the swab head is inserted into a sterile 2 mL EP tube containing 1 mL RNAstore reagent (Cat No.DP408, TiANGEN, Beijing) and sealed. After collection, the whole NIOSH sampler and swabs were sealed and surface sterilized, and transported on ice to the testing laboratory for processing.
2.3. Sample treatment and RNA extraction
The NIOSH sampler was opened in the biosafety cabinet. Sampled airborne particles were re-suspended with 1 mL of minimal essential medium containing 1% bovine serum albumin (Sigma). Viral RNA (vRNA) was extracted from 200 μL of re-suspended media using the full automatic nucleic acid extraction and purification instrument (NPA-32 P, BIOER, Hangzhou). The extract sample viral nucleic acid was eluted in 60 μL elution buffer.
2.4. Detection of viral RNA
The viral RNA was detected by quantitative real-time polymerase chain reaction (qRT-PCR) according to the laboratory detection guidelines of coronavirus infection issued by the China Health Commission. The samples were tested by targeting the SARS-CoV-2 nucleocapsid protein (NP) gene fragment. The primer and probe sequences for the N gene region were N-F: 5′-GGGGAACTTCTCCTGCTAGAAT-3′, N-R: 5′-CAGACATTTTGCTCTCAAGCTG-3′ and 5′-FAM-TTGCTGCTGCTTGACAGATT-TAMRA-3′. The qRT-PCR assays were performed using Applied Biosystems 7500 Real-Time PCR machine (Thermo Fisher Scientific Inc., USA). Each PCR contained a positive control and a negative control. When then PCR had an apparent logarithmic phase in the amplification curve and the cycle threshold value (Ct value) less than 40, sample was considered as positive.
3. Results
There were 33 air samples and 112 surface samples in total (support information Table S2. We did not detect any positive surface sample in the 1 and 1.5 protection level places. The virus nucleic acid laboratory of H-X is a level 3 place, and there were no positive results that has been detected for 9 consecutive days in the laboratory before we sampling, and we did not detect positive from the environmental samples. In the infection department of H-C, where mild confirmed patients were admitted, all the 8 confirmed patients’ nucleic acid test turned negative and the IgM test turned positive at the day before sampling. No positive reports were found in environmental samples even parts of samples were collected from their used masks and their palms.
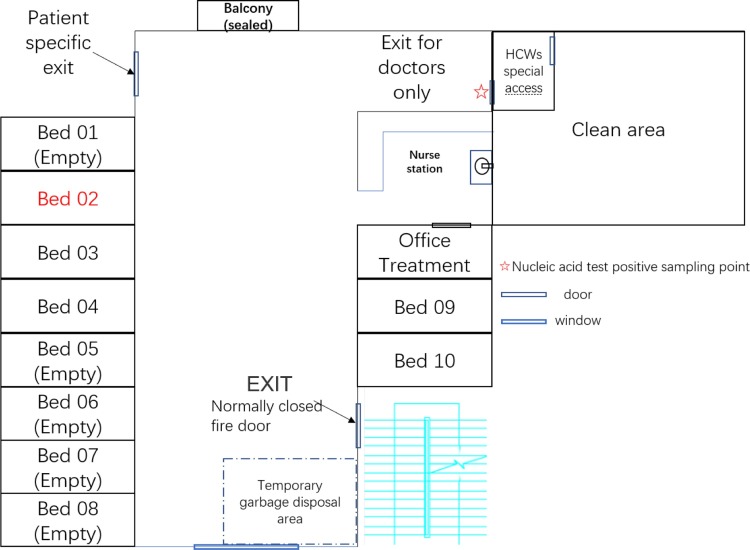
The situation was quite different when there was a patient whose nucleic acid test was positive at the sampling date (Table 1 ). In COVID-19 respiratory investigation ward of H-X, there was one patient (Bed No.02) had been confirmed by virus nucleic acid test on the day of sampling (Fig. 1 ). One positive surface sample was detected from the HCWs special access door handle on the HCW-only door, but not from the room accommodating the confirmed patient. Patients and caregivers are not allowed to access. Every HCW must touch the door handle with their gloves when leaving work and before taking off the protective equipment Figure 1.
Table 1.
Patients' Condition and Sample Positive Rate of Every Environment.
| Hospital | Protection level | Place name | Bed number of confirmed patients | Disease severity of confirmed patient | Nucleic acid test results |
COVID-19 IgM |
Date of sampling | Epidemiological history | Positive rate of environmental samples | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Positive date | Negative date | Positive date | Negative date | ||||||||
| Xiangya Hospital (H –X) |
Level 1 | Hemodialysis room a | There was no confirmed patient of COVID-19 in theory. | – | – | – | – | – | – | 0 | |
| Level 1.5 | General fever clinica | – | – | – | – | – | – | 0 | |||
| Level 2 | COVID-19 respiratory investigation ward b | 02 | Moderate | Feb.18 | – | – | – | Feb.18 | Yes. | 7.7 % | |
| Level 3 | Virus nucleic acid laboratory c | There was no new confirmed case was reported within 9 days before sampling. | – | – | – | – | – | – | 0 | ||
|
Chenzhou Second People's Hospital (H-C) |
Level 3 | COVID-19 confirmed patient ward | 18 | Mild | Feb. 18 | Feb. 22/26 | Feb. 24 | Feb. 25 | Feb.25 | Yes. | 0 |
| 33 | Feb. 13 | Feb. 18/24 | Feb. 21/24 | – | Yes. | ||||||
| 35 | Feb. 8 | Feb. 16/18/20/21 | Feb. 24 | Feb. 16 | Yes. | ||||||
| 36 | Feb. 12 | Feb. 17/22/24 | Feb. 21 | Feb. 24 | Yes. | ||||||
| 37 | Feb. 12 | Feb. 21/22/24 | Feb. 24 | – | Yes. | ||||||
| 38 | Feb. 9 | Feb. 21/22/24 | Feb. 24 | – | Yes. | ||||||
| 39 | Feb. 9 | Feb.16/18/21/24 | Feb. 12/24 | – | Yes. | ||||||
| 40 | Feb. 9 | Feb. 18/21/24 | Feb. 12/24 | – | Yes. | ||||||
| Shaoyang Central Hospital (H–S) | Level 3 | The ward of confirmed intensive care patient | ICU | Severe | Feb 28 | – | – | – | Feb.29 | Yes. | 82.6 % |
All dialysis patients of hemodialysis room of Xiangya hospital (H-X) must check lung CT and blood routine to exclude COVID-19 before hemodialysis. Fever patients were not allowed to enter hemodialysis room. The general fever clinic of H-X also only accepted fever patients without high risk factors of COVID-19. In theory, there will be no confirmed patients in those environments.
COVID-19 respiratory investigation ward of H-X mainly received COVID-19 suspected patients. But H-X was not a designated hospital of COVID-19 confirmed case. Once confirmed, the patient will be transferred to a special hospital immediately. There was just one confirmed patient on our sampling day. The patient had stayed in the ward for about 10 days. The first 4 nucleic acid tests were negative and just turned positive on the day of sampling.
Virus nucleic acid laboratory of H-X collected nasopharyngeal swab specimens of all confirmed patients in the whole hospital. But no positive result was reported within 9 days before sampling.
Fig. 1.
Room Layout Showing Environmental Sampling Sites in COVID-19 respiratory investigation ward of Xiangya Hospital (H-X).
There was one patient with positive nucleic acid test in 02 beds in the ward on the day of sampling. The patient was a 60-year-old male and had been in the ward for a week, but the first four nucleic acid tests were negative. The nucleic acid test of this patient's nasopharyngeal swab was positive for the first time on the day of sampling. No positive sample was detected in the ward except for the door handle of HCWs special access.
The most positive samples were detected from the intensive care patient's ward of H-S. All air samples and 78.95 % of surface samples were positive. The overall positive rate was 82.6 %. There was a 30-metre-long u-shaped passage between the ward of intensive care patient and the door handle of HCWs special access. However, the SARS-CoV-2 nucleic acid was still detected on the door handle (Fig. 2 ).
Fig. 2.
Room Layout Showing Environmental Sampling Sites in the intensive care patient's ward of Shaoyang central hospital (H-S).
The condition of the severe patient in ICU of Shaoyang Central Hospital was very bad at that time. He was an 83-year-old male and had already needed invasive ventilator and received ECOM treatment at the same time. This patient also needed indwelling catheterization and indwelling gastric tube to receive enteral nutrition due to coma. The night before sampling, the patient was rescued for up to 10 h. We detected SARS-CoV-2 nucleic acid in most of the environmental samples around this patient. It is important to note that, despite strict disinfection and separated by a long u-shaped corridor, SARS-CoV-2 nucleic acids still had been detected on the door-handle of the HCWs access.
All of the samples’ details were show in Table S2 in support information.
4. Discussion
There was no positive of SARS-CoV-2 in level 1 and level 1.5 protection environments, including hemodialysis room and general fever clinic of H-X. This result indicated that after strict triaged, in non COVID-19 treatment area (level 1 and level 1.5 protection environment), the occupational exposure risk of HCWs was relatively low. In addition, although the virus nucleic acid testing room was a level 3 place, there was no nucleic acid positive, the occupational exposure risk of HCWs was also very low.
In H-C, there were 8 confirmed patients stayed in the Level 3 wards. All of them were mild cases, and their virus nucleic acid test turned negative and the IgM antibody turned positive before this sampling. For all the samples were negative, it was speculated that those patients might not expelled the virus after the nucleic acid test turned negative. This result suggested that monitoring the virus in patient and doing the patient triage could be beneficial to the both of HCW and patient.
The virus nucleic acid was detected on the door handle of HCW-only access in COVID-19 respiratory investigation ward of H-X, the virus was probably stuck to the door handle by contacting with HCWs’ gloves (Fig. 1). Therefore, hand hygiene of HCWs should be put in the first place (De la Rosa-Zamboni et al., 2018; Dunne, Kingston, Slevin, & O’Connell, 2018; Mielke & Hansis, 2018; Monistrol et al., 2012; Salama, Jamal, Mousa, Al-Abdulghani, & Rotimi, 2013).
The high positive rate of viral nucleic acid was found in the ICU with a confirmed intensive care patient in H-S. This could be due to the virus released from the severe patient, and on the other hand, iatrogenic manipulation resulted in a wider range of viral contamination (Goyal & Chaudhry, 2019; Guest, Keating, Gould, & Wigglesworth, 2019; Pirincci & Altun, 2016; Pittet et al., 2006; Popp et al., 2019; Siegel, Rhinehart, Jackson, Chiarello, Health Care Infection Control Practices Advisory, & Committee, 2007; Steul, Exner, & Heudorf, 2019). Even though the HCWs of H-S wiped or sprayed disinfection the area surrounded the patient after each operation, and routine disinfection was acted every 4 h, the virus’ nucleic acid was still detected in most part of the room. All the air samples collected from the ward of severe patient in ICU of H-S were positive, which indicated that the iatrogenic process may produce the aerosol containing the virus and pollute the air. The positive samples in the room might be caused by HCWs contact or viral aerosol deposition. For there was a u-shaped corridor between the ward and the exit of the HCWs special access, and there were many opened windows surrounded the access, the virus on the door handle of the exit was more likely to be caused by contact.
The COVID-19 is still prevalent and the medical system is the last guarantee to protect public health. Protection of the HCWs is very important to avoid the overload of the medical system. Previous studies and our results suggested that monitoring the virus in patient and doing the patient triage could help to avoid cross infection (McMichael et al., 2020). Our study also showed that the viral nucleic acid exiting in same air samples and surfaces of the environments in hospitals during the COVID-19 pandemic, suggesting potential infection risk, though we did not confirm the infectivity of the virus. To protect the public and HCWs, the ventilation of the medical area may reduce the presence of virus in the air, and sterilization of medical apparatus and instruments and personal protective equipment may help to reduce the potential infection risk for HCWs when treating patient.
Hospitals are critical sites for controlling and combating COVID-19. Besides that, owing to the high transmissibility, high infectious and high pathogenicity of SARS-CoV-2, and its serious impact on social life and economy, the central and local governments of China took a series of forceful measures to deal with the COVID-19 pandemic, including isolation of suspected patients, monitoring of contact clinical status of patients, and developing diagnostic and treatment procedures, controlling the public transportation and airports/railway stations, postponing the schools and etc to prevent the disease transmission (Li, You et al., 2020). The COVID-19 has been effectively controlled in China, and most countries of the world have adopted different strategies to deal with the pandemic and achieved certain results (Lipsitch, Swerdlow, & Finelli, 2020; Muller, Neuhann, & Razum, 2020). However, the SARS-CoV-2 and its infection have some new features, like the asymptomatic infection, which brings difficulties to the virus prevention and control (Long et al., 2020). The SARS-CoV-2 may last for a long time. Thus, China proposed the concept of normalization prevention and control of COVID-19. Recently, a cluster of COVID-19 cases in Beijing associated with a wholesale market have reported a total of 172 cases as of 18 June 2020. The wholesale market infection event indicates that SARS-CoV-2 spreads through aerosol or close contact in the densely populated enclosed space probably. Previous studies showed that ventilation can effectively reduce the risk of virus infection for interior space (Yue, 2020). This event also highlighted the importance of the natural ventilation for buildings (B. Wang & Malkawi, 2019). The pandemic of COVID-19 also proposed the new requirements for disease prevention and control strategies and more functions of future buildings (Xu et al., 2020). In addition, environmental monitoring of virus, smart city technologies and artificial intelligence (temperature screening systems, tracking people, intelligent robot and etc), and big data are playing a more important role in combating infectious disease and maintaining the sustainable development of society (Kummitha, 2020; Liu & Li, 2020; Zhou, He, Cai, Wang, & Su, 2019).
Declaration of Competing Interest
The authors declare no competing interests.
Acknowledgements
This work was jointly funded by the National Natural Science Foundation Youth Fund (grant number 2170020935, 32041001), Hunan Provincial Health Committee's General Subsidy Project (grant number 20200100), Hunan Provincial Foundation (grant number 2020SK3001), Emergency Project of Prevention and Control for COVID-19 of Central South University (grant number 160260003).
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.scs.2020.102413.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Anderson D.J., Chen L.F., Weber D.J., Moehring R.W., Lewis S.S., Triplett P.F., Program C. D. C. Prevention Epicenters. Enhanced terminal room disinfection and acquisition and infection caused by multidrug-resistant organisms and Clostridium difficile (the Benefits of Enhanced Terminal Room Disinfection study): A cluster-randomised, multicentre, crossover study. Lancet. 2017;389(10071):805–814. doi: 10.1016/S0140-6736(16)31588-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beggs C., Knibbs L.D., Johnson G.R., Morawska L. Environmental contamination and hospital-acquired infection: Factors that are easily overlooked. Indoor Air. 2015;25(5):462–474. doi: 10.1111/ina.12170. [DOI] [PubMed] [Google Scholar]
- Berlanga F.A., Liu L., Nielsen P.V., Jensen R.L., Costa A., Olmedo I.…de Adana M.R. Influence of the geometry of the airways on the characterization of exhalation flows. Comparison between two different airway complexity levels performing two different breathing functions. Sustainable Cities and Society. 2020;53 doi: 10.1016/J.Scs.2019.101874. [DOI] [Google Scholar]
- Bulut C., Kato Y. Epidemiology of COVID-19. Turkish Journal of Medical Sciences. 2020;50(3):563–570. doi: 10.3906/sag-2004-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y.…Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China . National Health Commission of the People’s Republic of China; 2003. National Health Commission of the People’s Republic of China. General epidemic situation of SARS in China (May 29, 2003) website. [Google Scholar]
- China . National Health Commission of the People’s Republic of China; 2020. National Health Commission of the People’s Republic of China. General epidemic situation of SARS in China (February 27, 2020) website. [Google Scholar]
- Chung R.Y., Li M.M. Anti-Chinese sentiment during the 2019-nCoV outbreak. Lancet. 2020;395(10225):686–687. doi: 10.1016/S0140-6736(20)30358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De la Rosa-Zamboni D., Ochoa S.A., Laris-Gonzalez A., Cruz-Cordova A., Escalona-Venegas G., Perez-Avendano G.…Xicohtencatl-Cortes J. Everybody hands-on to avoid ESKAPE: Effect of sustained hand hygiene compliance on healthcare-associated infections and multidrug resistance in a paediatric hospital. Journal of Medical Microbiology. 2018;67(12):1761–1771. doi: 10.1099/jmm.0.000863. [DOI] [PubMed] [Google Scholar]
- Diseases NCIRD-National Center for Immunization and Respiratory. 2020. How COVID-19 spreads.https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html [Google Scholar]
- Dunne C.P., Kingston L., Slevin B., O’Connell N.H. Hand hygiene and compliance behaviours are the under-appreciated human factors pivotal to reducing hospital-acquired infections. The Journal of Hospital Infection. 2018;98(4):328–330. doi: 10.1016/j.jhin.2018.02.022. [DOI] [PubMed] [Google Scholar]
- Goyal M., Chaudhry D. Impact of educational and training programs on knowledge of healthcare students regarding nosocomial infections, standard precautions and hand hygiene: A study at tertiary care hospital. Indian Journal of Critical Care Medicine : Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine. 2019;23(5):227–231. doi: 10.5005/jp-journals-10071-23166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest J.F., Keating T., Gould D., Wigglesworth N. Modelling the costs and consequences of reducing healthcare-associated infections by improving hand hygiene in an average hospital in England. BMJ Open. 2019;9(10) doi: 10.1136/bmjopen-2019-029971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y.H., Cai L., Cheng Z.S., Cheng H., Deng T., Fan Y.P., Health, Care A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Military Medical Research. 2020;7(1):4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kummitha R.K.R. Smart technologies for fighting pandemics: The techno- and human- driven approaches in controlling the virus transmission. Government Information Quarterly. 2020:101481. doi: 10.1016/j.giq.2020.101481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents. 2020:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. The New England Journal of Medicine. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J.Y., You Z., Wang Q., Zhou Z.J., Qiu Y., Luo R.…Ge X.Y. The epidemic of 2019-novel-coronavirus (2019-nCoV) pneumonia and insights for emerging infectious diseases in the future. Microbes and Infection. 2020;22(2):80–85. doi: 10.1016/j.micinf.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19-Studies needed. The New England Journal of Medicine. 2020;382(13):1194–1196. doi: 10.1056/Nejmp2002125. [DOI] [PubMed] [Google Scholar]
- Liu H., Li Y. Smart cities for emergency management. Nature. 2020;578(7796):515. doi: 10.1038/d41586-020-00523-5. [DOI] [PubMed] [Google Scholar]
- Long Q.X., Tang X.J., Shi Q.L., Li Q., Deng H.J., Yuan J.…Huang A.L. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nature Medicine. 2020 doi: 10.1038/s41591-020-0965-6. [DOI] [PubMed] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. Journal of Medical Virology. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael T.M., Currie D.W., Clark S., Pogosjans S., Kay M., Schwartz N.G., Team, CDC COVID 19 Invest Epidemiology of Covid-19 in a long-term care facility in King County, Washington. The New England Journal of Medicine. 2020;382(21):2005–2011. doi: 10.1056/Nejmoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megahed N.A., Ghoneim E.M. Antivirus-built environment: Lessons learned from Covid-19 pandemic. Sustainable Cities and Society. 2020;61 doi: 10.1016/j.scs.2020.102350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielke M., Hansis M. “Prevention of surgical site infections” : Current recommendation of the German commission of hospital hygiene and infection prevention. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz. 2018;61(4):371–373. doi: 10.1007/s00103-018-2721-3. [DOI] [PubMed] [Google Scholar]
- Monistrol O., Calbo E., Riera M., Nicolas C., Font R., Freixas N.…Garau J. Impact of a hand hygiene educational programme on hospital-acquired infections in medical wards. Clinical Microbiology and Infection : the Official Publication of the European Society of Clinical Microbiology and Infectious Diseases. 2012;18(12):1212–1218. doi: 10.1111/j.1469-0691.2011.03735.x. [DOI] [PubMed] [Google Scholar]
- Muller O., Neuhann F., Razum O. Epidemiology and control of COVID-19. Deutsche Medizinische Wochenschrift (1946) 2020;145(10):670–674. doi: 10.1055/a-1162-1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China - key questions for impact assessment. The New England Journal of Medicine. 2020;382(8):692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- Phan L.T., Sweeney D.M., Maita D., Moritz D.C., Bleasdale S.C., Jones R.M., Program C.D.C. Prevention Epicenters. Respiratory viruses in the patient environment. Infection Control and Hospital Epidemiology. 2020;41(3):259–266. doi: 10.1017/ice.2019.299. [DOI] [PubMed] [Google Scholar]
- Pirincci E., Altun B. An analysis of hospital cleaning staff’s attitudes and conduct regarding hand hygiene and cleaning. International Journal of Occupational Safety and Ergonomics : JOSE. 2016;22(2):241–245. doi: 10.1080/10803548.2015.1100906. [DOI] [PubMed] [Google Scholar]
- Pittet D., Allegranzi B., Sax H., Dharan S., Pessoa-Silva C.L., Donaldson L.…Who Global Patient Safety Challenge, World Alliance for Patient Safety Evidence-based model for hand transmission during patient care and the role of improved practices. The Lancet Infectious Diseases. 2006;6(10):641–652. doi: 10.1016/S1473-3099(06)70600-4. [DOI] [PubMed] [Google Scholar]
- Popp W., Alefelder C., Bauer S., Daeschlein G., Geistberger P., Gleich S., Exner M. Air quality in the operating room: Surgical site infections, HVAC systems and discipline - position paper of the German Society of Hospital Hygiene (DGKH) GMS Hygiene and Infection Control. 2019;14 doi: 10.3205/dgkh000335. Doc20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevention The First Level Response Situation Analysis and Risk Assessment Team of Pneumonia Infected in novel coronavirus of China Center for Disease Control and Prevention: The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chinese Journal of Epidemiology. 2020;42:145–151. [Google Scholar]
- Rahman M.A. Data-driven dynamic clustering framework for mitigating the adverse economic impact of Covid-19 lockdown practices. Sustainable Cities and Society. 2020;62 doi: 10.1016/j.scs.2020.102372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salama M.F., Jamal W.Y., Mousa H.A., Al-Abdulghani K.A., Rotimi V.O. The effect of hand hygiene compliance on hospital-acquired infections in an ICU setting in a Kuwaiti teaching hospital. Journal of Infection and Public Health. 2013;6(1):27–34. doi: 10.1016/j.jiph.2012.09.014. [DOI] [PubMed] [Google Scholar]
- Siegel J.D., Rhinehart E., Jackson M., Chiarello L., Health Care Infection Control Practices Advisory, Committee 2007 guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. American Journal of Infection Control. 2007;35(10 Suppl. 2):S65–164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steul K., Exner M., Heudorf U. Personal preconditions for the prevention of nosocomial infections-guidelines of the German Commission for Hospital Hygiene and Infection Prevention (KRINKO), federal state hygiene regulations in Germany, and compliance by hospitals in Frankfurt am Main. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz. 2019;62(3):329–340. doi: 10.1007/s00103-019-02896-z. [DOI] [PubMed] [Google Scholar]
- Wang B., Malkawi A. Design-based natural ventilation evaluation in early stage for high performance buildings. Sustainable Cities and Society. 2019;45:25–37. doi: 10.1016/j.scs.2018.11.024. [DOI] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: Interim guidance. [Google Scholar]
- WHO . 2020. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19)https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-oncovid-19-final-report.pdf [Google Scholar]
- Xie C.Y., Lau E.H.Y., Yoshida T., Yu H., Wang X., Wu H.T., Yen H.L. Detection of influenza and other respiratory viruses in air sampled from a university campus: A longitudinal study. Clinical Infectious Diseases. 2020;70(5):850–858. doi: 10.1093/cid/ciz296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu C.W., Luo X.L., Yu C., Cao S.J. The 2019-nCoV epidemic control strategies and future challenges of building healthy smart cities. Indoor and Built Environment. 2020;29(5):639–644. doi: 10.1177/1420326x20910408. [DOI] [Google Scholar]
- Yue L. Ventilation in the dental clinic: An effective measure to control droplets and aerosols during the coronavirus pandemic and beyond. The Chinese Journal of Dental Research: the Official Journal of the Scientific Section of the Chinese Stomatological Association (CSA) 2020;23(2):105–107. doi: 10.3290/j.cjdr.a44746. [DOI] [PubMed] [Google Scholar]
- Zhang X.D. Epidemiology of Covid-19. The New England Journal of Medicine. 2020;382(19):1869. doi: 10.1056/Nejmc2005157. [DOI] [PubMed] [Google Scholar]
- Zhang Y.X., Feng G.H., Bi Y., Cai Y.L., Zhang Z., Cao G.Y. Distribution of droplet aerosols generated by mouth coughing and nose breathing in an air-conditioned room. Sustainable Cities and Society. 2019;51 doi: 10.1016/J.Scs.2019.101721. [DOI] [Google Scholar]
- Zhou H., He S.J., Cai Y.Y., Wang M., Su S.L. Social inequalities in neighborhood visual walkability: Using street view imagery and deep learning technologies to facilitate healthy city planning. Sustainable Cities and Society. 2019;50 doi: 10.1016/J.Scs.2019.101605. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.