Abstract
Parents are typically in charge of purchasing the food that their children eat, but little is known about how parents decide if particular foods are healthy for their children and how their beliefs about nutrition influence their children’s beliefs. In two studies, we investigated how parents of children ages 4 to 12 (N = 826) make decisions about the healthiness of foods, when presented with different representations of the same nutritional information. Providing parents with nutritional information did not influence their ratings of how healthy food items are, compared to when they are shown only pictures of the foods. Parents reported talking with their children about nutrition, believed they are the best source of information for children about nutrition, and believed their nutrition beliefs influence their child’s beliefs. Our findings highlight the role of prior knowledge in food cognition and how beliefs about foods are transmitted from parents to children.
Keywords: Parenting, numerical representations, prior knowledge, nutrition, nutrition labels
Food choices are important decisions that many parents make for their children. Although children become progressively more independent through the early school years, many children report having little control over the food they eat (Robinson, 2000). Furthermore, parents shape their children’s knowledge and habits about food (Hendy, Williams, Camise, Eckman, & Hedemann, 2009). People’s perceptions of foods influence what they decide to consume, with people eating more of a food if they think of it as healthy (Provencher, Polivy, & Herman, 2009). Therefore, parental beliefs about the healthiness of foods might influence the foods their children eat. As childhood obesity and other health concerns continue to be a public health crisis (Ebbeling, Pawlak, & Ludwig, 2002; Karnik & Kanekar, 2012), it is important to examine the factors that influence how parents make decisions about nutrition and food choices for their children.
In this paper, we focus on how parents decide which foods are healthy for their children and how they communicate nutrition information to their children. We argue that understanding how parents determine the healthiness of foods and how they communicate this information might give us some insights into how children come to think of certain foods as healthy. In two studies, we provided parents different representations of nutrition information: either no nutrition information, a traditional nutrition label, or a modified nutrition label that made the meanings of the numerical values more accessible. We explored how these different representations influenced their judgements of how healthy different foods are for their children. We also examined reports of how much parents use nutrition information to guide their purchasing decisions. In Study 2, we also examined whether parents talk to their children about nutrition and the extent to which parents think their beliefs about nutrition influence their children’s beliefs. In particular, we examined whether parents talk to their children about nutrition generally and about nutrition information on food packaging, and we considered the contexts in which these conversations take place. We also examined whether parents provided different healthiness ratings if foods were presented as for their children or for themselves. Taken together, these two studies intend to shed light on how beliefs about nutrition are transmitted from parents to children.
Parents’ decision making
When reasoning about foods, people often hold multiple categories in mind and use them to guide their decisions. Although adults most often organize foods by taxonomic categories, such as fruits or meats, they also often use categories related to the meals when the food is eaten, such as snacks or dinner (Ross & Murphy, 1999). Nguyen and Murphy (2003) found that by 4 years of age, children can classify foods into these different categories and use them to guide their inferences (such as inferences about the amount of a certain vitamin contained in a food). These different classifications of foods might be relevant, as adults who considered a certain food a snack ate more of the food than those who considered it a meal (Capaldi, Owens, & Privitera, 2006).
Parents’ decisions about their children’s food options are influenced by many factors. Noble, Stead, McDermott, and McVie (2007) found that even though mothers in the United Kingdom and Australia clearly differentiate between healthy and unhealthy food options for their children, other factors appear to influence their food-related decisions. These factors include issues related to resources (e.g., time and money) and avoiding stress during mealtimes. There is also general consensus that children have substantial influence on such decisions for a wide range of products, including food (e.g., Wilson & Wood, 2004). Children often take part in grocery shopping with their caregivers (Page, Sharp, Locksin & Sorensen, 2018). Indeed, some researchers argue that children could be “change agents” who could promote healthy food purchasing decisions on the part of their caregivers (Wingert, Zachary, Fox, Gittelsohn & Surkan, 2014). Although children clearly do influence some parental choices about food for snacks and meals, parents generally make the final choices in food selection. For this reason, we focus on a key piece of information, nutrition labels, that are required in the United States, examining the extent to which parents can and do use this information to determine what types of food might be healthy for their children to consume.
Nutrition labels are an important source of information on all packaged foods sold in the United States and many other countries (Campos, Doxey, & Hammond, 2011). These ubiquitous labels provide important information such as the serving size, total calories, and percent of daily values (usually based on a 2000 calorie diet). A review of diverse samples in different countries suggests that self-reported use of food labels when making purchases is quite high, but varies substantially across sub-groups (Campos, et al., 2011). Consumers appear to understand the importance of nutrition information, though in some cases people report using nutrition information to a greater extent than they actually do (Cowburn & Stockley, 2004; Grunert, 2010).
Nutrition labels contain information that can help consumers make more informed choices about their food consumption. Ollberding, Wolf, and Contento (2010) reported that nutrition label users appear to make healthier decisions than non-users. Labels with nutrition facts have undergone both aesthetic and content changes over time, in the hopes of conveying nutrition information in a more effective manner (George, 2014). Changes in the design have been made to highlight important information to the consumer, such as serving size, number of calories, and quantity of added sugar. For instance, the font in which calorie information is presented is now larger and bold, and the quantity of added sugars is now presented separately. These changes were implemented in order to emphasize information that could be used to make healthy choices, potentially guiding parents to choose foods with fewer calories and less sugar, and to provide their children with appropriate serving sizes.
However, even with these changes, nutrition labels rely mostly on numeric information, such as the quantity of different nutrients provided in grams. For example, a serving of yogurt may be listed as consisting of 150 grams and including 15 grams of sugar. Consuming only half a serving would imply consuming 7.5 grams of sugar. In this respect, the gram values presented on food labels need to be interpreted in light of the serving size. The raw gram values listed on the labels might not be intuitive, because people seldom encounter such values outside of the domain of nutrition and because interpreting them requires integrating two separate pieces of information (i.e., the number of grams of the specific nutrient and the number of grams in a serving). Some researchers have reported that percentage representations might be more meaningful (Moss & Case, 1999). This suggests that presenting the nutrition information as a percentage (e.g., this serving of a food item contains 15% fat) might make the information more accessible to the consumer, potentially influencing their purchasing decisions.
The form in which nutrition information is presented may influence how parents think about the food. Researchers have manipulated how nutrition information is represented and examined its effect on food choices. In one study, Adams, Hart, Gilmer, Lloyd-Richardson, and Burton (2014) showed that when given more concrete information (i.e., sugar content represented as the equivalent number of sugar cubes), participants were less likely to choose sugar-sweetened beverages than when they saw abstract information (i.e., numerical measurement units such as grams). The researchers suggested that concrete information, such as the number of sugar cubes, might be more accessible than more abstract information, such as number of grams. The findings from this study showed that modifying how nutrition information is presented to parents could influence their food-related choices.
This previous work suggests that if numerical information about nutrition is readily accessible, people may be more likely to use it in making food choices. Although sugar cubes are a concrete way to think about the amount of sugar in food, it could be difficult to find analogous concrete representations for other nutrients (such as proteins). Given that nutrition labels require proportional reasoning and integrating information about serving size with amounts of specific nutrients, we propose that one way to make this information accessible is to present nutrition information in percentages. Percentages may be more accessible to consumers because they provide proportional information directly, as a single value. In contrast, information about amounts of nutrients must be integrated with information about serving size.
At the same time, many studies suggest that people are better at processing probability information when it is presented in frequencies (e.g., 1 in 5 people) than when it is presented in percentage format (e.g., 20% of people; e.g., Gigerenzer & Hoffrage, 1995). This suggests that people may be better at interpreting information presented as raw values (15 grams out of a 100-gram serving) than as percentages (15% of the weight of the food item).
Based on these findings, an important question to consider is whether the information presented on food labels is accessible to the lay consumer. In this research, we investigated the impact of alternative ways of presenting nutrition information to consumers. Specifically, we examined how parents use information from nutrition labels and how presenting information on nutrition labels in different ways might influence their judgments of foods. Understanding these judgements is important because parents might communicate these judgments to their children. If this is the case, then parents’ conversations with their children about nutrition could influence their children’s food choices.
It is worth noting that nutrition labels already include some information presented in percentages, namely, the percent daily value. This quantity shows how much of the daily suggested intake of a nutrient is in a single serving size. These values are typically based on a 2,000-calorie daily diet. This information may be difficult for people to interpret as they have to relate this information to all the other foods they have consumed and will consume that day. Additionally, the 2,000-calorie diet on which these values are based is not the ideal diet for many people. For these reasons, in this paper we do not investigate the influence of percent daily value on healthiness judgments. Instead, we focus on how numerical representations of grams and percentages influence how people judge the healthiness of foods.
Parents influence children’s food choices
Understanding how parents make decisions about food is important because parental behavior around food, and modeling eating in particular, appears to influence children’s eating habits. Some researchers have suggested that, at least among food-secure families, parental food intake is related to child food intake (DeJesus, Gelman, Viechnicki, Appugliese, Miller, Rosenblum, & Lumeng, 2019). Furthermore, modeling eating certain foods seems to be an effective way of promoting children to eat them (Addessi, Galloway, Visalberghi, & Birch, 2005; Harper & Sanders, 1975). Thus, there appears to be a link between what parents eat and what children eat. By understanding what drives parents to purchase certain foods, we might be able to influence both their and their children’s eating habits.
Children pay attention, not only to eating behavior, but also to other cues associated with foods. Children seem to pay attention to whether a food is described as palatable (Hendy & Raudenbush, 2000), whether the food is eaten by in-group members (Shutts, Kinzler, McKee, & Spelke, 2009), and whether other children like the food (DeJesus, Shutts, & Kinzler, 2018). Parental talk about foods might be a particularly useful cue, as children are more likely to eat foods that adults say are tasty (Lumeng, Cardinal, Jankowski, Kaciroti, & Gelman, 2008). However, the link between parental food talk and children’s food intake is not very clear. Parental food talk, such as talking about foods that they like or asking questions about food, does not seem to be related to children’s food intake, at least among low-income families (DeJesus et al., 2019). Further, there seem to be different styles of parental food talk, and these styles might differ among socio-demographic groups (Pesch, Harrell, Kaciroti, Rosenblum, & Lumeng, 2011).
One possible reason why research has not uncovered links between parent-child conversations about food and children’s food intake is that past research has focused on conversations about food (e.g., what parents and children like or dislike, or whether parents encourage eating certain foods and not others) and not conversations about nutrition. In one study, children who learned more about nutrition and its biological bases made healthier food choices during snack time than children who read books about exercise and eating healthily (Gripshover & Markman, 2013). So, it appears that specific information about nutrition influences food choices. Children also seem to view adults, and parents in particular, as reliable sources of information about nutrition (Nguyen, 2012; VanderBorght & Jaswal, 2009). However, little is known about how parents talk to children about nutrition.
In the current studies, we examine whether parents discuss nutrition information with their children. We also inquire about the settings in which these conversations take place. We also begin to investigate the extent to which parent’s beliefs about nutrition influence their children’s beliefs.
Current studies
In two studies, we investigated the impact of alternative ways of presenting nutrition information on parents’ judgments of the healthiness of foods, and we examined how parents discuss nutrition information with their children.
In the first study, we manipulated how nutritional values were represented: either in the traditional form of number of grams, or in a relative form of percentages by weight. We hypothesized that the relative form would be more accessible to participants, as it represents a proportion regardless of serving size. For instance, a yogurt that is 150 grams per serving with 15 grams of sugar can be represented as containing 10% sugar. We also asked parents whether they use nutrition labels to guide their decisions of which foods to purchase. With regards to the use of nutrition labels, we expected that parents would report using them more for new or unfamiliar foods than for frequently purchased and consumed foods. Lastly, we expected that most parents would rely heavily on their prior experiences and knowledge of food items when provided with only pictures of the food items and no explicit nutrition information.
Based on the findings from the first study, we conducted a follow-up study that addressed some of the limitations of the first study. First, people rarely see nutrition information in isolation. Study 2 investigated whether the results differed when participants have access to both the nutrition information and a picture of the item. Second, Study 2 also explored whether parents would rate the healthiness of food differently when the food was presented as for their child or for themselves. Finally, Study 2 also explored whether parents actually discuss nutrition with their children and the contexts in which these conversations take place.
Study 1
Method
Participants
Through Amazon’s Mechanical Turk, we recruited 496 parents who had at least one child between the ages of 4 and 12. We focused on parents of children between 4 and 12 years of age because, during these years, children eat a wide range of foods but parents still purchase the majority of the foods that they eat. We included two attention checks in the survey to make sure that participants were paying attention to the task; 115 participants were eliminated because they failed at least one of the attention checks. Of the remaining parents, 236 identified as women and 145 identified as men (one participant did not report gender). The mean age of the participants was 36.5 years (SD = 6.6, range = 23, 68). Due to an error in the survey, we did not gather race/ethnicity information. We used the MacArthur subjective socio-economic status scale to obtain participants’ ratings of their subjective socio-economic status (SES; Goodman, Adler, Kawachi, Frazier, Huang, & Colditz, 2001). The average subjective SES was 5.21, and participants used the full range of the scale (SD = 2.1, range = 0, 10). We also asked participants to rate their overall health (compared to their same age peers) using a sliding scale from 0 (not at all healthy) to 10 (very healthy). The average subjective health rating was 6.76, and participants used the full range of the scale (SD = 1.97, range = 0, 10). Due to an oversight in creating the survey, we did not ask parents about demographic information for their children (such as age and gender). The task took about 30 minutes to complete.
Design
We used a within-subjects design with three conditions: picture, grams, and percentage. Participants were informed of whether the food item was commonly eaten as a snack (e.g., fruit snacks), spread (e.g., peanut butter), breakfast (e.g., cereal), or dinner (e.g., meatloaf). We provided this category information to participants as many of the foods differed in their serving size. The information about when the food is eaten might help parents contextualize the serving size information. In the picture condition, participants viewed pictures of the food items, but no nutrition information was provided. In the grams and percentage conditions, participants were not told the identity of the food items, but they saw the nutrition information. This was a deliberate decision, as we wished to examine how participants would reason about nutrition information when they could not use their prior knowledge about the identity of the food items. In all conditions, participants were asked to judge how healthy the food item was for their children. See Figure 1.
Figure 1.
This is an example of the information that participants saw in the picture, grams and percentage conditions (respectively) for the macaroni and cheese trial. The left-most panel shows the item in the picture condition. The middle panel shows the same item in the grams condition. The right-most panel shows the same item in the percentage condition. The bottom panel shows the question that participants responded to in all conditions. The name of the child (which they provided in a previous section) was inserted where it says, “Name of Child.”
Materials and Procedure
The majority of the food items were selected from The New York Times article “Is Sushi ‘Healthy’? What About Granola? Where Americans and Nutritionists Disagree” (Quealy & Sanger-Katz, 2016). Of the 21 food items selected, 12 came from the Quealy and Sanger-Katz (2016) article (almonds, shrimp, kale, cottage cheese, ice cream, peanut butter, French fries, apple, carrots, avocado, hummus, and wheat bread). The remaining items were selected to include additional foods that might be considered unhealthy by the general public (fruit snacks, macaroni and cheese, chocolate pudding, meatloaf, hot dog, potato chips, apple pie, cereal, and popcorn). All of the included food items had nutrition label information available from the United States Food and Drug Administration. Participants made 41 total judgments (21 in the picture condition, 10 in the grams condition, and 10 in the percentage condition). The same 10 items were rated in all three conditions (almonds, shrimp, kale, cottage cheese, fruit snacks, ice cream, macaroni and cheese, peanut butter, chocolate pudding and meatloaf).
There were 11 additional items in the picture condition (hot dog, French fries, potato chips, apple pie, cereal, apple, carrots, avocado, hummus, popcorn, and wheat bread). These additional items served two purposes. First, we wanted to have some distractor items in case participants attempted to match the foods they saw in the picture conditions to the nutrition labels they saw in the grams and percentages conditions. We hoped that by having more items, this matching would be more ambiguous. Second, we wanted to pilot test some items for future studies. The ten items judged in every condition were selected so that there would be an equal number of healthy and unhealthy items.
In the picture condition, we showed participants pictures of the food items, but we did not provide any nutrition information. Images were obtained through Google images. We looked for images in which the only food displayed was the intended food item and that had a white or plain background.
In the grams condition, participants were informed whether the item was commonly eaten as a snack, breakfast, lunch or dinner, and they saw a traditional food label that showed the serving size (in grams), the number of calories, and the number of grams of fat (saturated and unsaturated), carbohydrates (sugar), and protein in one serving.
In the percentage condition, participants were given the same information as in the grams condition, but all numbers were displayed as percentages of the serving size. For example, if a food item had a serving size of 200g and contained 20g of protein, the food label in the percentage condition would show 10% protein. To direct participants to the correct interpretation of the percentage as the percent of the food, we included the following phrase “Each X gram serving is comprised of’ before presenting the percentages. However, it is worth noting that participants could have interpreted this percentage as a percent of daily value (a much more commonly displayed quantity). Number of calories and serving size in grams were displayed in the same way in the grams and percentage conditions. See Figure 1.
We presented food items to participants one at a time. Participants first viewed and rated all trials in the picture conditions because we expected these trials to be simpler to navigate. This way, all participants were familiar with the task before they saw any food labels. Always presenting the pictures first also allowed us to get participants’ ratings of the healthiness of foods before they were presented with any nutrition information. Participants were then randomly assigned to complete either the grams or the percentage condition first. Within each condition, the order in which the food items were presented was randomized. After seeing each food item (or nutrition information), we asked participants how healthy they thought the food item was for their children on a 1 (extremely unhealthy) to 6 (extremely healthy) Likert-type scale. After they rated the healthiness of the item, we asked participants to rate how a range of factors informed their judgement of healthiness on a 1 (not important at all) to 5 (extremely important) Likert-type scale. These factors included what they already knew about the food item, the number of calories, the amount of fat, the amount of carbohydrates, the amount of protein, and the serving size. For these judgements, participants could also say that they did not use the particular piece of information in judging healthiness. In the picture condition, we also asked participants to report how much they enjoyed the food item on a sliding scale with options not at all and very much as anchors.
After completing the food ratings, participants were asked to report demographic information such as subjective SES, gender, and overall health. We also asked participants to report how often they use nutrition labels when buying new foods and when buying foods that they frequently buy using a 1 (never) to 5 (always) scale. We also asked participants to report how often they use nutrition labels to determine whether a food item is healthy using a 1 (never) to 5 (always) scale. Note that all of these questions focused on parents and not on their children.
Results
We divide the results section into three parts. First, we analyzed whether participants’ healthiness ratings were influenced by the representation (picture, grams or percent). We also conducted some exploratory analyses of whether participants’ ratings differed depending on whether they were told the food was a snack or a meal and whether the food is healthy or unhealthy. Second, we analyzed participants’ reports of the information they used to guide their healthiness ratings. We explored whether the type of representation they saw influenced which information they used to guide their judgements of how healthy the food item is. Third, we present data on whether participants use nutrition labels (outside of the context of this study) to guide their purchasing decisions. If participants report not using nutrition labels, then any modification in their design would not lead to behavior changes. We also explored what factors predict use of nutrition labels. All means reported in the text are raw and not adjusted for covariates. All analyses were conducted with the statistical software R (R Core Team, 2018), using the lme4 package (Bates, Maechler, Bolker, & Walker, 2015) to fit the linear mixed-effects models. We used a Kenward-Rogers approximation for the degrees of freedom.
Effects of representation
We used linear mixed-effects regression to predict healthiness ratings for the food items. We included condition (using the picture condition as the reference group), participant age, participant gender, and participant SES as fixed effects. We also included by-subject random intercepts and by-subject random slopes for the effect of condition. We include only the 10 food items that were presented in all conditions; however, the results do not change if we include the additional 11 items presented only in the picture condition.
There was a main effect of condition, F(2, 377.02) = 10.75, p < .001. Participants rated foods as healthier when they saw the nutrition information presented in grams (M = 4.18, SD = 1.55) than when they saw only pictures of the foods (M = 3.83, SD = 1.42), F(1, 378.10) = 20.08, p < .001. Similarly, participants rated foods as healthier when they saw the nutrition information presented in percentages (M = 4.19, SD = 1.56) than when they saw only pictures of the foods, F(1, 378.10) = 21.49, p < .001. However, contrary to our prediction, there was no difference in healthiness ratings when participants saw the information in grams or percentages, F(1, 421.10) = 0.21, p = .646. See Figure 2. We also found an effect of subjective SES, such that higher SES was associated with higher healthiness ratings, F(1, 375.53) = 12.04, p < .001. There was no effect of participant age, F(1, 375.27) = 1.64, p = .201, or gender, F(1, 375.20) = 1.02, p = .313.
Figure 2.
Participants’ healthiness ratings in each of the three conditions. Higher values on the y-axis mean that participants judged the foods as more healthy. Error bars show the within-subject standard errors without adjusting for covariates. Asterisks (*) indicate that the contrast between the two conditions was significant at an alpha level of .05.
In order to investigate whether these findings changed depending on the foods being judged, we conducted several exploratory analyses. First, we divided the 10 food items judged in every condition into meal categories. When each food was presented participants were given a meal category. For these ten food items, the categories were lunch, dinner, dessert, snack or spread. We combined lunch and dinner as “meals” (kale, mac & cheese, meatloaf, and shrimp) and dessert, snacks and spreads as “snacks” (almonds, chocolate pudding, cottage cheese, fruit snacks, ice cream, peanut butter). We added meal category and its interaction with representation type to the previous model (and allowed for random slopes for these effects). When participants saw pictures of the foods (the reference condition), we found that there was an effect of meal category, such that participants rated foods typically consumed during meals (M = 4.22, SD = 1.25) as healthier than foods typically consumed as snacks (M = 3.60, SD = 1.37), χ2(1, N = 380) = 336.58, p < .001. However, this effect was qualified by an interaction with representation, such that the effect of meal category was smaller when participants saw only the nutrition information (presented as either grams or percentages), χ2(2, N = 380) = 98.05, p < .001. See Figure 3. This suggests that category information (such as when a food is typically consumed) can influence healthiness ratings.
Figure 3.
Effect of representation type on healthiness ratings when participants rated foods presented as snacks (left panel) or meals (right panel). Error bars show the within-subject standard errors without adjusting for covariates.
We also explored whether participants’ judgements depended on the healthiness of the foods. This analysis is critical, as it might also provide us with information about how accurate participants’ judgements were. To determine whether a food was healthy or not, we used information from Quealy and Sanger-Katz (2016) who had 672 nutritionists rate food items as healthy or unhealthy. We used the percentage of their respondents who categorized a given food item as healthy for this analysis (not all nutritionists rated each item, but there were about 300 ratings per item; see full results here: https://intel.morningconsult.com/public/mc/160600_topline_NYT_v2_AP.pdf). Of the 10 foods rated in all conditions, five were considered healthy (mean percent of nutritionists who categorized them as healthy = 89.2%): almonds (98%), cottage cheese (84%), kale (97%), peanut butter (82%), and shrimp (85%). Ice cream was the only food in our set that was considered unhealthy (with only 13% of nutritionists judging it as healthy). We had no information on chocolate pudding, fruit snacks, meatloaf, or macaroni and cheese, but there was consensus among our research team that these items are unhealthy, so we combined them with ice cream as “unhealthy foods.” We added healthiness category and its interaction with representation to the initial model. This model did not converge, so following recommendations by Barr, Levy, Scheepers, and Tily (2013), we removed the random intercepts. We found that, when participants saw pictures of the foods, they rated healthy foods as healthier than unhealthy foods, χ2(1, N = 380) = 2206.76), p < .001. However, this effect was qualified by an interaction with representation, χ2(1, N = 380) = 1496.61, p < .001. As can be seen in Figure 4, the difference between healthy and unhealthy foods was much smaller when participants saw only the nutrition information (regardless of whether it was presented in grams or percentages). This suggests that participants’ judgements were most accurate when they saw pictures of the food items. When they did not have access to the pictures, their ratings of healthy and unhealthy foods were more similar. Table 1 presents the mean healthiness rating for each food item in each condition.
Figure 4.
Participants’ healthiness ratings in each of the three conditions, for healthy and unhealthy foods. Higher values on the y-axis mean that participants judged the foods as healthier. Error bars show the within-subject standard errors without adjusting for covariates.
Table 1.
Mean healthiness rating by food item and condition. For study 2, we collapsed across judgements for self and judgements for child. Standard deviations are presented in parentheses.
| Study 1 | Study 2 | ||||
|---|---|---|---|---|---|
| Food Item | Picture | Grams | Percentage | Picture and Grams |
Picture and Percentage |
| Almond | 5.19 (0.79) | 4.15 (1.51) | 4.09 (1.61) | 5.25 (0.76) | 5.17 (0.71) |
| Apple | 5.56 (0.59) | NA | NA | 5.56 (0.65) | 5.55 (0.55) |
| Apple pie | 2.64 (0.97) | NA | NA | 2.50 (1.04) | 2.40 (0.91) |
| Avocado | 5.28 (0.71) | NA | NA | 5.28 (0.79) | 5.22 (0.83) |
| Baked potato | NA | NA | NA | 4.03 (0.91) | 3.89 (0.92) |
| Bread | 4.14 (0.72) | NA | NA | 3.36 (1.00) | 3.27 (0.90) |
| Bread (Wheat) | NA | NA | NA | 4.22 (0.80) | 4.12 (0.84) |
| Carrot | 5.32 (1.06) | NA | NA | 5.34 (1.07) | 5.46 (0.92) |
| Cereal | 4.03 (0.87) | NA | NA | 3.90 (1.02) | 3.96 (0.91) |
| Cheeseburger Chocolate |
NA | NA | NA | 2.89 (0.95) | 2.80 (1.05) |
| pudding | 2.79 (0.98) | 4.18 (1.56) | 4.13 (1.59) | 2.75 (0.97) | 2.62 (0.86) |
| Cottage cheese | 4.32 (0.90) | 4.19 (1.52) | 4.21 (1.51) | 4.29 (1.08) | 4.25 (0.91) |
| Egg | NA | NA | NA | 4.71 (0.79) | 4.56 (0.91) |
| Fries | 2.28 (0.97) | NA | NA | 2.20 (1.06) | 2.19 (1.05) |
| Fruit snacks | 2.52 (1.04) | 4.10 (1.60) | 4.00 (1.68) | 2.28 (1.03) | 2.42 (1.01) |
| Granola bar | NA | NA | NA | 4.05 (1.01) | 4.16 (0.92) |
| Hot dog | 2.70 (1.00) | NA | NA | 2.53 (1.04) | 2.51 (1.05) |
| Hummus | 3.99 (1.03) | NA | NA | 4.06 (1.11) | 4.02 (1.13) |
| Ice cream | 2.65 (1.00) | 4.03 (1.60) | 4.01 (1.62) | 2.53 (1.07) | 2.49 (0.91) |
| Jerky | NA | NA | NA | 3.51 (1.15) | 3.38 (1.06) |
| Kale | 5.58 (0.59) | 4.33 (1.48) | 4.47 (1.48) | 5.61 (0.61) | 5.60 (0.61) |
| Mac & cheese | 3.13 (0.97) | 4.01 (1.62) | 4.13 (1.47) | 2.90 (1.01) | 2.86 (1.01) |
| Meatloaf | 3.68 (0.88) | 4.28 (1.49) | 4.31 (1.49) | 3.66 (0.90) | 3.65 (0.82) |
| Oatmeal | NA | NA | NA | 4.74 (0.82) | 4.79 (0.68) |
| PB&J | NA | NA | NA | 3.45 (0.91) | 3.43 (0.87) |
| Peanut butter | 4.22 (0.81) | 4.04 (1.58) | 4.12 (1.54) | 4.17 (0.89) | 3.99 (0.92) |
| Popcorn | 3.77 (0.87) | NA | NA | 3.92 (0.89) | 3.86 (0.82) |
| Potato chips | 2.16 (0.94) | NA | NA | 2.04 (0.88) | 2.03 (0.81) |
| Salami | NA | NA | NA | 3.06 (1.20) | 3.03 (1.08) |
| Salmon | NA | NA | NA | 5.28 (0.84) | 5.21 (0.85) |
| Shrimp | 4.51 (0.90) | 4.47 (1.49) | 4.43 (1.49) | 4.84 (0.93) | 4.64 (0.80) |
| Yogurt | NA | NA | NA | 4.52 (0.94) | 4.50 (0.90) |
Information used
After each food item, participants were asked to report how much they used the serving size, calories, fat, protein, and carbohydrates of the food item and their prior knowledge to inform their healthiness judgements. We used a linear-mixed effects model to analyze how much participants used information of each of the six types. We included information type (with prior knowledge as the reference category), condition (with the picture condition as the reference group), participant age, participant gender, and subjective SES as fixed effects. We also included by-subject random intercepts, and two by-subject random slopes (one for the effect of information type, and one for the effect of condition).
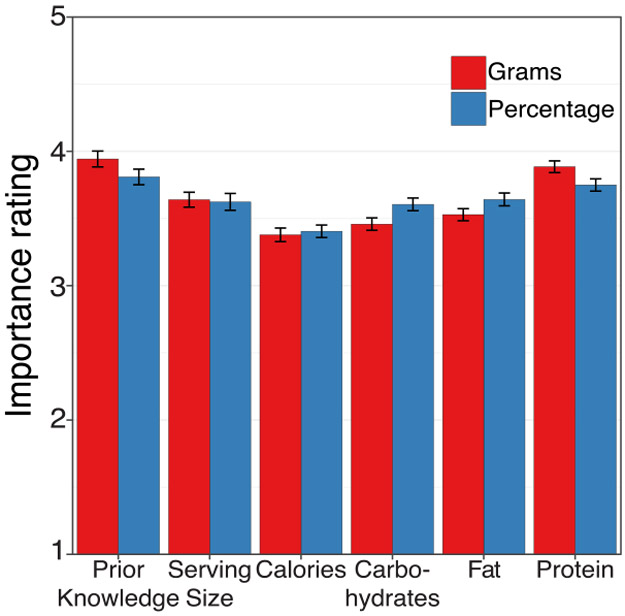
We found a main effect of representation, χ2(2, N = 380) = 98.72, p < .001. Participants reported using more information when they judged healthiness based on nutrition information presented in grams (M = 3.77, SD = 1.17) than when they judged based on pictures alone (M = 3.70, SD = 1.28), t(366.7) = 3.53, p < .001. Participants also reported using more information when they judged healthiness based on nutrition information presented in percentages (M = 3.79, SD = 1.16) than when they judged based on pictures alone, t(368.1) = 4.26, p < .001. These effects were expected, because participants had no access to any nutrition information in the picture condition and could only use their prior knowledge. We also found an effect of category type, χ2(5, N = 380) = 223.65, p < .001. Participants reported using prior knowledge about the food items (M = 4.07, SD = 1.07) more than the serving size (M = 3.62, SD = 1.21; t(377.5) = −11.90, p < .001), calories (M = 3.73, SD = 1.22; t(380) = −10.62, p < .001), fat (M = 3.73, SD = 1.23; t(382.7) = −9.33, p < .001), carbohydrates (M = 3.68, SD = 1.26; t(384.5) = −9.78, p < .001), or protein (M = 3.60, SD = 1.29; t(385.7) = −11.20, p < .001). We also found an interaction between category type and representation, χ2(10, N = 380) = 374.36, p < .001. As seen in Figure 5, participants used nutrition information less and prior knowledge more in the picture condition. There were no differences between the grams and the percentage conditions. No other effects were significant.
Figure 5.
Participants’ reports of how much they used prior knowledge, serving size, calories, carbohydrates, fat and protein to inform their healthiness ratings for all three conditions. Higher values on the y-axis mean that participants used the information more. Error bars show the within-subject standard error.
Predictors of nutrition label use
To analyze whether participants reported using nutrition labels when buying foods, we used a linear-mixed effects model. We included whether participants were reporting about buying a new food product (versus a product they frequently buy), their rating of how often they used nutrition labels to determine healthiness (mean centered), the interaction of product type (i.e., new vs. frequently bought) and self-reported nutrition label use, participant age, participant gender and subjective socio-economic status as fixed effects. We included by-subject random intercepts and by-subject random slopes for the effect of frequent versus new items. This model did not converge, so we removed the by-subject random intercepts.
Participants were more likely to use nutrition labels when buying new products (M = 3.47, SD = 1.12) than when buying products they frequently consume (M = 2.93, SD = 1.21), t(370) = 8.95, p < .001. Furthermore, participants who reported using nutrition labels more when considering a food item’s healthiness also reported using nutrition labels more frequently than those who said they used nutrition labels less when considering a food item’s healthiness, t(367) = 25.47, p < .001. The interactions between using nutrition labels to determine healthiness and using nutrition labels for new items was not significant, t(370) = 1.27, p = .203. Participants with higher subjective socio-economic status reported using nutrition labels more frequently, t(367) = 2.98, p = .003. There was no effect of participant age, t(367) = 0.56, p = .579, or gender, t(367) = 0.54, p = .589.
Discussion
One of the main goals of Study 1 was to examine how the same information presented in different representations might affect parents’ ratings of food. We did not find evidence for our hypothesis that presenting nutrition information as percentages (instead of grams) would influence participants’ ratings of how healthy foods are. We did find that when participants had only nutrition information and no identifying information about what the food was, their healthiness ratings did not vary very much between food items. On the other hand, when participants had only identifying information (i.e., a picture of the food) but no explicit nutrition information, their judgements seemed to follow those of experts. In line with this finding, we also found that participants reported relying on their prior knowledge about the food items more than on any other source of information about healthiness, particularly when they saw pictures of the items.
Our results also suggest that even some conceptual information, specifically, a label that the food is eaten as a snack or as part of a meal, leads to changes in ratings of how healthy a food is for children. However, given that we did not manipulate this factor, it could be due to the snack foods used in this study being less healthy than the “meal” foods.
We found that participants reported using nutrition labels when buying new food products. However, parents reported not using nutrition labels when buying products that they frequently consume. For frequently consumed food items, parents might simply use their prior experience and knowledge about the food items to judge healthiness. This might mean that nutrition labels in food packaging might be a useful way to create impressions of how healthy a new food item is but might be less effective at shifting impressions of how healthy a particular food is, once those impressions have been formed.
In Study 1, we showed participants either a picture of the food item or the nutrition information, along with information about the food’s category (e.g., snack, breakfast food, etc.), but without information about the food’s identity. Therefore, we were unable to assess whether presenting different forms of nutrition information influences judgments of healthiness when the participants know the identity of the food item. We investigated this question in Study 2. In Study 2, we also asked participants to report whether they discuss nutrition information with their children.
Study 2
In Study 2, we examined whether different presentations of food labels influence judgments of healthiness when participants know the identities of the food items. As in Study 1, we asked participants to determine whether food items were healthy for their child between the ages of 4 and 12.
One open question is whether parents’ judgements of how healthy foods are for their children differ from their judgements of how healthy the same foods are for themselves. Parents may have different beliefs about what foods are healthy for their children and what foods are healthy for themselves or adults more generally. Parents might believe that children’s nutritional needs are different from those of adults; for example, they might believe that children need more fat or more protein in their diets than adults do. We explored this issue by randomly assigning participants to either make decisions for themselves or for their children.
We also wished to know more about the contexts within which parents discuss nutrition information with their children. To that end, in Study 2 we also included questions requesting information about whether and when participants discuss nutrition information with their children, and about participants’ beliefs about the value of different information sources for learning about nutrition.
Method
Participants
We recruited 501 parents with children between the ages of 4 and 12 through Amazon’s Mechanical Turk. None of them had participated in Study 1. We included one attention check to ensure that participants paid attention to the items; 40 participants did not pass the attention check and so were removed from the sample. Sixteen participants were removed because they did not report having children in the desired age range. Of the remaining 445 participants, 147 identified as men, 297 identified as women, and one did not report gender. Participants’ age ranged from 22 to 65 (M = 36.8, SD = 7.4). Of the 445 participants, 345 identified as white, 44 as Asian or Asian American, 26 as Black or African American, 17 as Hispanic or LatinX, 7 as Native American or American Indian, and 6 as bi- or multi-racial. Participants’ subjective socioeconomic status ranged from 0 to 10 (M = 5.3, SD = 2.2). Participants’ subjective health ranged from 1 to 10 (M = 6.70, SD = 2.00). The mean age of the participants’ children was 7.9 years (SD = 2.6 years). Two hundred and thirty-two participants reported that their child was a boy, 211 reported that their child was a girl, and 2 did not report the gender of their child.
We also asked participants to respond to the question, “How much responsibility do you have for grocery shopping in your family?” They answered using a sliding scale from 0 (never do it) to 100 (always do it). On average, participants were on the upper end of the scale (M = 86.79, SD = 18.90, range = 2, 100). We asked a similar question about their responsibility for preparing foods for their family, and participants were again at the upper end of the scale (M = 81.60, SD = 23.22, range = 0, 100).
Design
We used a 2 (representation: grams, percentages) x 2 (target: for child, for self) between-groups design. Participants rated the healthiness of 32 food items. All participants saw a picture of the food item and a nutrition label for that item side by side. Participants were randomly assigned to rate how healthy the food items were either for themselves or for their children. Participants were also randomly assigned to see the nutrition information in grams or percentages.
Materials
We showed participants pictures of food items, one at a time, accompanied by nutrition labels. Participants were told whether the food is typically consumed as a snack, breakfast, lunch, or dinner. The nutrition labels presenting the information in grams or percentages were the same as in the previous study. Similar to Study 1, participants reported whether they were familiar with the food item, and how much they (or their children, if they were rating for their children) enjoyed it. Participants then rated the healthiness of the food item using the same scale as in Study 1. Instead of judging how much participants used each piece of information after every judgement, participants gave one rating at the end of the study indicating the importance they placed on prior knowledge, serving size, calories, fat, carbohydrates, and protein when determining how healthy a food is.
We also asked participants several questions that tapped into how they talk with their children about nutrition. Participants were asked to report whether they talk with their children about nutrition and nutrition information in food packaging. Participants also rated how important it is for them that their child has a good understanding of which foods are healthy for them using a 5-point scale that ranged from 1 (not at all important) to 5 (extremely important). We also asked participants where they think their child should learn about nutrition (from parents, other family members, teachers, doctors, nutrition tables, TV shows, advertisements, or online searches). For this item, participants could choose as many options as they wanted and could also write in any other source of information. We also asked participants to report how they think their children learned about nutrition, using the same set of options. Participants also reported which of those sources would be the best source of nutrition information for their children.
Using a 7-point scale, ranging from far too little to far too much, participants rated how much they thought their own ideas about nutrition influenced the food that their child eats. We also asked participants to report when they talk with their children about nutrition and when they talk about nutrition labels on food packages (at mealtimes, at restaurants, at the grocery story, or at any other time). Participants rated how knowledgeable they thought their children were about nutrition when compared to other children in the same age range using a 5-point scale, ranging from not knowledgeable to extremely knowledgeable. Finally, participants were asked how much of the responsibility for grocery shopping and how much of the responsibility for preparing food they have in their family.
Procedure
Participants completed a short screener to determine whether they were eligible for the study. Then, they read an online consent form prior to beginning the study. Participants first provided information about the age and gender of their child, and they then completed the healthiness rating task, followed by questions about how they talk about nutrition with their children. Finally, they provided other demographic information.
Results
This section has the same general structure as the results of Study 1. First, we analyze whether participants’ healthiness ratings were influenced by the representation and whether they were judging foods for themselves or their children. We also conduct similar exploratory analyses of whether participants’ ratings differed depending on meal category and food healthiness. Second, we analyze participants’ reports of the information they used to guide their healthiness ratings. We explore whether participants use different information if they are making decisions for themselves or their children, and if the information used varied depending on the numerical representation. Third, we present data on whether participants use nutrition labels. Finally, we have argued that parents’ reasoning in the domain of nutrition influences their children’s reasoning. However, this is only possible if parents discuss nutrition information with their children. The last section of results explores whether participants talk with their children about nutrition and nutrition labels. All means reported in the text are raw means (unadjusted for covariates). All analyses were conducted with the statistical software R (R Core Team, 2018), using the lme4 package (Bates, Maechler, Bolker, & Walker, 2015) to fit the linear mixed-effects models. We used a Kenward-Rogers approximation for the degrees of freedom.
Effects of representation on healthiness ratings
We used a linear mixed-effects model to predict participants’ healthiness ratings. We included whether participants were making decisions for themselves or for their children, whether they saw the nutrition information in grams or percentages, child age, child gender, participant age, participant gender and subjective SES as predictors. We also included the interactions between making decisions for self or child and representation type, decision for self or child and child age, and decision for self or child and parent age.
We found that participants who judged how healthy food items were for their children (M = 3.91, SD = 1.39) rated items as healthier than participants who judged how healthy food items were for themselves (M = 3.75, SD = 1.42), χ2 (1, N = 435) = 19.87, p < .001. As in Study 1, we did not find that participants differed in their healthiness judgements depending on whether they saw the nutrition information in grams (M = 3.86, SD = 1.42) or percentages (M = 3,81, SD = 1.39), χ2 (1, N = 435) = 0.22, p = .637. Representation also did not interact with whether participants were making decision for themselves or their children, χ2 (1, N = 435) = 2.43, p = . 119. As in Study 1, we found that participants with higher subjective SES rated foods as healthier than those with lower subjective SES, χ2 (1, N = 435) = 11.65, p = .001. Einlike Study 1, we found that participants who identified as women judged foods as healthier than those who identified as men, χ2 (1, N = 435) = 7.44, p = .006. No other effects were significant.
As in Study 1, we examined whether the meal category influenced healthiness ratings. We categorized foods as “meals” (baked potato, cereal, cheeseburger, egg, French fries, hotdog, kale, macaroni and cheese, meatloaf, oatmeal, peanut butter and jelly sandwich, salmon, shrimp, white bread, wheat bread, and yogurt) and “snacks” (almonds, apple, apple pie, avocado, carrots, chocolate pudding, cottage cheese, fruit snacks, granola bar, hummus, ice cream, jerky, peanut butter, popcorn, potato chip, and salami). We included meal category and its interaction with representation type and whether participants were making decisions for themselves or for their children in the previous model. As in Study 1, there was an effect of meal category, such that participants rated foods typically consumed during main meals (M = 3.90, SD = 1.32) as healthier than foods typically consumed as snacks (M = 3.77, SD = 1.48), χ2(1, N = 435) = 30.53, p < .001. However, there were no interactions with numerical representation, χ2(1, N = 435) = 0.06, p = .804, or making decisions for self or child, χ2(1, N = 435) = 0.77, p = .382, and no three-way interaction, χ2(1, N = 435) = 0.35, p = .555. This suggests category information (such as when a food is typically consumed) can influence healthiness ratings.
We also explored whether participants’ judgements depended on the healthiness of the foods. Of the 32 foods rated, 14 were considered healthy (mean percent of nutritionists who categorized them as healthy = 89%): almonds (98%), apple (99%), avocado (95%), baked potato (72%), carrot (99%), cottage cheese (84%), egg (96%), hummus (91%), kale (97%), oatmeal (97%), peanut butter (82%), popcorn (61%), shrimp (85%) and whole wheat bread (90%). On the other hand, 7 were considered unhealthy (mean percent of nutritionists who categorized them as healthy = 20.6%): cheeseburger (28%), French fries (5%), granola bar (28%), ice cream (13%), jerky (23%), white bread (15%), and yogurt (32%). The remaining foods were categorized as healthy (salmon) or unhealthy (apple pie, cereal, chocolate pudding, fruit snacks, hotdog, macaroni and cheese, meatloaf, peanut butter and jelly sandwich, potato chips, and salami) based on consensus among the research team. We added healthiness category and its interaction with representation and decisions for self or child to the initial model. As in Study 1, participants rated healthy foods as healthier than unhealthy foods, χ2(1, N = 435) = 3591.76, p < .001. None of the interactions were significant. Table 1 presents the mean healthiness rating for each food item in each condition.
Both Study 1 and Study 2 showed that parents relied on prior knowledge to make their healthiness decisions. In Study 1, we found that there was a difference between having a picture or the nutrition label for the item. However, we do not know whether having both the picture and the nutrition information is different from having only the picture. It is possible that participants in Study 2 simply did not pay attention to the nutrition information because they had access to the pictures and relied on their prior knowledge. To consider whether this was the case, we tested whether the ratings of participants in Study 2 differed from those of participants in Study 1 when they were rating only pictures. Because participants in Study 1 rated all of the pictures first, we were not concerned about exposure to the other conditions. We restricted our analysis to the ten food items that were used in all conditions of Study 1, and we used a linear-mixed effects model predicting healthiness ratings from experimental condition, participant age, participant gender, and subjective SES. We did not include child age or child gender, as we did not have this information for Study 1.
We did not find an effect of condition, χ2 (2, N = 600) = 2.78, p = .249. This suggests that participants who had access to the picture and the nutrition information rated foods similarly to participants who saw only the picture. Participants who identified as women rated foods as healthier than those who identified as men, χ2 (1, N = 600) = 4.08, p = .043. Participants with higher subjective SES also rated foods as healthier than those with lower subjective SES, χ2 (2, N = 600) = 19.19, p < .001.
In order to see whether participants’ judgements were accurate, we compared their ratings to the percentage of nutritionists from Quealy and Sanger-Katz (2016) who considered the foods healthy. For this analysis, we included all of the foods in Study 1 (picture condition) and 2 that were rated in Quealy and Sanger-Katz (2016). We predicted healthiness ratings from the percentage of nutritionists who considered the food healthy, representation condition (picture only, picture and grams, or picture and percentage), their interaction, participant age, participant gender, and subjective SES. We also included by-subject random intercepts and by-subject random slopes for the effect of percentage of nutritionists. The results of this model are presented in Figure 6. As seen in the figure, participants’ ratings were predicted by the nutritionists’ ratings, χ2 (1, N = 600) = 2518.74, p < .001. As the percent of nutritionists who considered the food as healthy increased, participants’ healthiness ratings also increased. However, the figure also highlights that participants’ ratings do not match perfectly nutritionists’ ratings. Participants judged very unhealthy foods as healthier than did nutritionists, and healthy foods as less healthy. This suggests that overall, parents consider food as somewhat healthy or very healthy, with most ratings being above the midpoint. Parents also do not seem to rate many foods as extremely or very unhealthy. We did not find a significant interaction between nutritionists’ ratings and representation type, χ2 (2, N = 600) = 5.94, p = .051.
Figure 6.
Participants’ healthiness ratings (on the y-axis) compared to the percentage of nutritionists in Quealy and Sanger-Katz (2016) who categorized the food as healthy (on the x-axis). The different lines show the picture condition from Study 1, and the picture and grams and picture and percentage conditions from Study 2 (for participants making decisions for their children). Error bands show the within-subject standard errors. The dotted line is the relation if participants’ judgements perfectly matched the nutritionists’ judgements. The points are each rating the participants provided. The points are jittered to minimize overlap.
Information used
Participants were asked to report how important serving size, calories, fat, protein, and carbohydrates of the food item and their prior knowledge were when judging the healthiness of food items. We used a linear-mixed effects model to analyze how much participants used each of the six types of information. The model included whether participants were making decisions for themselves or for their children, whether they saw the nutrition information in grams or percentages, information type (six levels, with prior knowledge as the reference category), child age, child gender, participant age, participant gender, and subjective SES as fixed effects. We included the interaction between information type and representation type (grams or percentages) and the interaction between information type and decision for self or for child. We also included by-subject random intercepts and by-subject random slopes for the effect of category.
We did not find a main effect of judging for self or for child, Wald χ2 (1, N = 435) = 0.69, p = .407, or an interaction with information type, Wald χ2 (5, N = 435) = 6.29, p = .279. However, there was a significant interaction of information type and number representation, Wald χ2 (5, N = 435) = 13.20, p = .022. The difference between the importance placed on prior knowledge and the importance placed on carbohydrates was smaller among those who saw the nutrition information in percentages than among those who saw the nutrition information presented in grams, t(432) = 2.36, p = .019. As seen in Figure 7, participants in the percentage condition said that prior knowledge was less important and carbohydrates were more important than participants in the grams condition. There were also significant overall effects of information type, Wald χ2 (5, N = 435) = 93.38, p < .001, but no overall effect of number representation, Wald χ2 (1, N = 435) = 2.94, p = .087. As seen in Figure 7, with the exception of protein, participants rated all type of information as less important than prior knowledge, but participants’ greater reliance on prior knowledge was reduced when the nutrition information was presented in percentages. Additionally, participants who identified as women rated information sources as more important than those who identified as men, Wald χ2 (1, N = 435) 6.63, p = .010. Participants with higher subjective SES also rated information sources as more important than those with lower subjective SES, Wald χ2 (1, N = 435) = 12.44, p < .001. Taken together, the findings suggest that when nutrition information was expressed in percentages, participants drew on that information more than when it was expressed in grams.
Figure 7.
Importance ratings for the 6 types of nutrition information by representation condition. Higher values on the y-axis mean that participants rated that piece of information as more important. Error bars show the within-subjects standard error without adjusting for covariates.
Use of nutrition labels
We asked participants to report how often they used nutrition labels when buying food products they frequently consume and when buying new products on a 5-point scale ranging from 1 (never) to 5 (always). As in Study 1, we used a linear-mixed effects model to predict whether participants used food labels when buying products. We included whether participants were reporting about buying a new product (versus a product they frequently buy), their rating of how often they use nutrition labels to determine healthiness (mean centered), the interaction of these factors, participant gender, participant age, child gender, child age, and subjective SES as fixed effects. We included by-subject random intercepts and by-subject random slopes for the effect of frequent versus new items. However, this model did not converge, so we removed the random intercepts.
As in Study 1, we found that participants were more likely to use nutrition labels for new products (M = 3.73, SD = 1.01) than for products they frequently bought (M = 2.94, SD = 1.23), t(427.06) = 13.64, p < .001. Again, we found that participants who reported using nutrition labels to determine how healthy a food item is reported using nutrition labels more often, t(422.08) = 22.38, p < .001. As in Study 1, we did not find an interaction of these factors, t(427.44) = 0.28, p = .782. Participants with higher subjective socio-economic status reported using food labels more frequently, t(420.59) = 4.68, p < .001, and those who identified as women (M = 3.38, SD = 1.23) reported using food labels more than those who identified as men (M = 3.23, SD = 1.13), t(422.52) = 2.11, p = .035. No other effects were significant.
Parent-child nutrition talk
Most participants reported that it was either extremely or very important for them that their child knows about nutrition (n = 366, 82%). In line with this finding, we found that the majority of participants (95.7%) said that they talk with their child about nutrition. Most often, participants said that they talk about nutrition during mealtime at home (n = 420, 94%) or at restaurants (n = 123, 28%). Many participants also said that they discuss nutrition at the grocery store (n = 299, 67%). Some of the write-in answers included: when they are eating something “bad” for them (n = 3), when growing or preparing food (n = 5), when planning meals (n = 2), when the child asked questions (n = 4), when watching food-related media or advertisements (n = 2), at home not during meal times (n = 2), in the car (n = 2), and randomly when the topic arises (n = 6). Participants reported that their children should learn about nutrition from parents (n = 435, 98%), teachers (n = 292, 66%), other family members (n = 245, 55%), online searches (n = 81, 18%), TV shows aimed at children (n = 170, 38%), nutrition labels (n = 240, 54%), advertisements (n = 76, 17%), and doctors (n = 329, 74%). However, the majority of the participants (n = 318, 71%) said that parents are the best source of information for their children’s learning about nutrition.
Many participants also reported talking with their children about nutrition information on food packaging (60%). We used logistic regression to explore whether participants who had older children were more likely to say that they talked with their children about food labels, and we included participant age, participant gender, child gender, and subjective SES as covariates. We found that the age of the child was a significant, positive predictor of participants’ reporting that they talk with their children about food labels, t(429) = 5.29, p < .001. Additionally, participants with higher subjective SES were more likely to talk with their children about nutrition labels, t(429) = 3.75, p < .001. We did not find that participant age, t(429) = −1.67, p = .091, participant gender, t(429) = −0.33, p = .738, or child gender, t(429) = 1.25, p = .210, predicted whether participants talked with their children about nutrition labels. Most participants said that they discuss nutrition labels at home around mealtime (n = 135, 30%) or at the grocery store (n = 118, 26%).
When participants were asked to rate how knowledgeable their children were about nutrition (compared to other children their age) on a 5-point scale, they rated their children as moderately knowledgeable (M = 3.17, SD = 0.86). We attempted to predict participants’ ratings of how knowledgeable their children were about nutrition from child age, child gender, participant gender, participant age, subjective SES, and whether their participants said they talk with their children about nutrition and about food labels. We found that participants who self-reported talking to their children about nutrition and nutrition labels more specifically reported that their children were more knowledgeable about nutrition, t(427) = 3,90, p < .001 for nutrition; t(427) = 6.19, p < .001 for nutrition labels. We also found that as subjective SES increased parents rated that their children knew more about nutrition, t(427) = 4.14, p < .001. In these analyses, the age of the child was not a significant predictor of their nutrition knowledge, t(427) = 0.98, p = .327, presumably because we had asked participants to rate their children in relation to same age peers. There were no effects of child gender, t(427) = 1.68, p = .093, participant gender, t(427) = 1.28, p = .202, or participant age, t(432) = −1.70, p = .090.
We also asked participants to rate, on a 7-point scale, how much their own beliefs about nutrition influenced what their children eat. Participants on average said their beliefs about nutrition had a moderate influence on what their children eat (M = 4.37, SD = 1.19). We investigated whether these scores varied depending on the child’s age, child’s gender, participant’s age, participant’s gender, participant’s subjective SES, how much of the responsibility of preparing food and grocery shopping the participant had, and whether the participant said they talk with their child about nutrition and about nutrition labels. Participants who reported that they talk with their children about nutrition labels more strongly agreed that their own beliefs about nutrition influence what their child eats than participants who reported that they do not talk with their children about food labels, t(425) = 4.07, p < .001. Participants with higher subjective SES thought their own beliefs influenced their child’s beliefs more than those with lower subjective SES, t(425) = 2.45, p = .015. Participants who identified as women thought their beliefs influenced their child’s beliefs more than those who identified as men, t(425) = 2.19, p = .029. None of the other predictors were significant.
Discussion
As in Study 1, we did not find that participants’ judgements about the healthiness of food items differed when the information was presented in grams or percentages. However, we also found that participants’ judgements about healthiness when they saw a picture and the nutrition information of the food item did not differ from when they saw only a picture. Indeed, participants reported that prior knowledge was the most important piece of information they used when rating the food items. This suggests that when they recognized the item that was pictured, they may have ignored or paid less attention to the nutrition information presented with the picture. Participants not attending to the food labels of items they recognize is in line with our finding that participants report not using food labels when purchasing foods they consume frequently. Additionally, we found that participants who rated foods for their children gave higher healthiness ratings than those who rated foods for themselves.
Participants reported talking with their children about nutrition, and they reported that these conversations typically occur around mealtime or at the grocery store. Although participants reported that children learn about nutrition from a variety of sources, most considered themselves to be the best source of information about nutrition for their children. Fewer participants reported talking with their children about nutrition information found on food packaging, and whether they did so was related to how much they thought their children knew about nutrition.
General Discussion
In two studies, we investigated how parents use nutrition information when rating the healthiness of foods, and whether the form that this information takes (i.e., whether it is presented in grams vs. in percentages) affects their ratings. Study 1 showed that when parents only had access to nutrition information, their ratings of the healthiness of foods did not differ between healthy and unhealthy foods or between foods in different meal categories. Study 2 showed that, in general, when parents rated foods for their child they rated them as healthier than when they rated food for themselves. When considering data from both studies, we found that parents made similar judgements when they saw pictures of the foods accompanied by nutrition information than when they saw only the pictures. This suggests that parents are more likely to use food labels when they do not know a lot about the items, such as when purchasing a new food product. However, once they are familiar with a particular food product, parents appear less attentive to the nutrition labels. This result is important, as it suggests that there are significant challenges to getting parents to attend to food labels if they are already familiar with particular food items. Future research should explore how parents report gaining knowledge about the healthiness of foods more generally and whether their knowledge about nutrition and food healthiness is accurate.
Nutrition labels and food cognition
These findings add to a growing body of work on people’s judgments of the healthiness of foods, and on the sources of information people use to make such judgments. Our finding that people base their judgments on prior knowledge about the foods, rather than on nutrition labels, is in line with past research showing that even children as young as 3 can successfully categorize foods as “healthy” or “junky” (Nguyen & Murphy, 2003; Nguyen, 2007). By adulthood, people have years of experience with familiar foods, and they have well-established views about which foods are healthy. People’s views about the physical and emotional consequences of eating healthy and unhealthy foods increase in precision and elaborateness over development (e.g., Wellman & Johnson, 1982; Raman, 2014); however, their judgments about the healthiness of foods are largely accurate, even in early childhood. In the present studies, it appears that parents’ judgements resemble those of nutritionists, with the caveat that parents rarely rated foods as very unhealthy.
The finding that parents do not modify their healthiness judgements very much when they have only nutrition information was surprising. This might mean that parents do not know how to interpret nutrition labels. The idea that parents might not know how to interpret nutrition labels is in line with research suggesting that many young adults have an inadequate understanding of nutrition labels (Sharf, Sela, Zentner, Shoob, Shai, & Stein-Zamir, 2012). Parents generally viewed foods as healthy, and this was even more prevalent when there was no picture of the food item. If this finding holds up in future studies, it may have profound implications for the idea that nutrition labels should be present for all foods in all settings. Previous work suggests that people are more likely to overeat snacks deemed to be healthy (Provencher, Polivy, & Herman, 2009). If placing a nutrition label on an unfamiliar but unhealthy food leads parents to perceive such foods as healthier, these labels may paradoxically lead to an increase in the consumption of unhealthy foods.
Our studies add to previous findings that nutrition label use may be lower than self-report studies suggest (Cowburn & Stockley, 2004), as people use such labels mainly for unfamiliar products. Prior work suggests that nutrition knowledge promotes the use of nutrition labels (Miller & Cassady, 2015), but our findings indicate that people might not use labels accurately or might discount the information they provide for familiar foods. It is worth pointing out that parents in both of our studies indicated that they used nutrition information found on labels, such as calories, fat and protein. However, their judgements did not change when the information was not present. This might indicate that parents might think that they are using the information, but they might only be using their prior knowledge about how much protein or fat a food has.
Our data do not support the idea that nutrition information presented in percentages was more accessible to participants than comparable information presented in grams. Only one finding suggested that percentage information was more accessible; namely, parents rated the importance of information about carbohydrates as higher when they had encountered that information in percentages. At the same time, however, there was no evidence that parents judged the healthiness of foods differently when nutrition information was presented in percentages vs. in grams, suggesting that any practical impact of such differences in representation is limited. Overall, effects of number representation were small and not consistently observed.
Transmission of beliefs about nutrition
This study provides insight into how parents communicate nutrition information to their children. Most parents in Study 2 reported talking with their children about nutrition in general, and some reported specifically talking about nutrition labels. This type of talk might be important, as parents who reported talking with their children about nutrition thought that their children were more knowledgeable about nutrition than parents who did not report engaging in these talks. From the current study, it is not clear if children know more about nutrition because their parents talk with them about it, or if parents are more likely to talk about nutrition if they perceive their child as knowing a lot about nutrition. Future work should attempt to investigate the directionality of this relation.
One clear finding was that parents endorse that their children may obtain nutrition information from many sources, but most believe that they themselves are the best source of information. This is encouraging, as when parents lack self-efficacy for teaching children about a particular topic, they are more likely to withdraw from teaching opportunities (Grolnick, Benjet, Kurowski, & Apostoleris, 1997). Our studies suggest that in the domain of nutrition, parents might feel confident in talking to their children.
Although most parents in our study reported talking with their children about nutrition, other observational research suggests that parents and children rarely talk about nutrition when making food purchasing decisions. For example, O’Dougherty, Story and Stang (2006) observed parent-child interaction around purchasing decisions in supermarkets and found that nutritional considerations were raised in only 3% of interactions. Some other, more vague comments about potential food purchases might also conceivably have been based on nutritional aspects of the products (e.g., “you don’t want that stuff’, about candy)—but on the whole, the frequency of discussions about nutrition in supermarket interactions was very low. The authors did not report whether the nutrition information that was discussed in these interactions was based on prior knowledge or on nutrition labels.
The low frequency of discussions about nutrition in supermarkets and grocery stores might be related to the foods that families purchase. The bulk of the items that families purchase are likely foods with which they are familiar. Both of our studies show that parents often do not use nutrition labels when purchasing familiar foods. If families purchase only familiar foods, they might not check nutrition labels much and might discuss them with their children even less. Additionally, many foods that are considered healthy, such as fruits and vegetables, often do not have nutrition labels. This might also limit opportunities for parents to discuss nutrition information with their children.
These findings highlight the need for research addressing when and where parents do talk about nutrition with their children, as such interactions are likely influence children’s thinking in this domain. The influence of parents can be seen in the fact that young children report preferring to learn about the healthiness of foods from parents and teachers, rather than from cartoons or from other children (Nguyen, 2012). Future research should investigate parent-child interactions around food choices, both in naturalistic and experimental settings, in order to identify contextual features that trigger discussions of nutrition and to examine the kinds of nutrition information that parents and children discuss. Future research should also explore how parent-child discussions about nutrition relate to food choices.
Researchers should also examine the effects of socio-demographic factors on parents’ conversations and interactions with their children relating to nutrition.. We found that mothers, to a greater extent than fathers, thought their beliefs about nutrition influenced their children’s beliefs. This was the case, even after controlling for self-rated responsibility for preparing foods and grocery shopping and whether they said they talked to their child about nutrition and nutrition labels. Therefore, it could be that mothers are more likely to discuss nutrition during mealtimes than fathers, or that mothers are more likely to prepare foods or grocery shop with their children.
We also found that parents who rated their subjective socio-economic status higher rated foods as healthier, overall, than parents who rated their subjective socio-economic status as lower. We did not predict this relation a priori, and we are therefore cautious in interpreting it. However, this finding highlights the need for further research on how socio-demographic factors influence people’s evaluations of foods, as well as research on whether such evaluations are observed in parent-child talk about nutrition.
Limitations
Our studies have a several important limitations. First, the nutrition information we provided was limited, even when pictures were provided along with the labels in Study 2. Second, the information presented in our study was restricted to serving size, calories, and quantities of key nutrients such as carbohydrates, fat, and protein. We chose to present only a few nutrition facts in order to have a more straightforward manipulation, but this does mean that our food labels were simplified. We also only asked parents about these broad categories. It is possible that parents’ ratings would have been different if we had posed the questions differently. For example, parents might have responded differently if we had asked how much their judgements were determined by the amount of sugar (a more specific term) than the amount of carbohydrates (a broader term). Third, the percentage information that we included was different from the percentage information that is normally presented on nutrition labels, which is percent of daily value based on a 2000 calorie diet. This may have been confusing. Although we attempted to provide enough information to guide parents to the intended interpretation of these percentages, we do not have any information that would help us determine whether parents did in fact interpret the percentages as we intended. Future studies should examine whether presenting parents with grams or percent of daily values leads to differences in their healthiness judgements. Fourth, we did not include information about how the food items might be prepared, about the other items being consumed along with the food items that day or week, or about the overall quantity being consumed. These are all key issues to consider when thinking about the healthiness of meals more generally. Finally, we did not obtain information about actual parent-child conversations, but simply asked parents to report on whether they talk with their children about nutrition. It is possible that parents actually talk less to their children than they reported.
Conclusions
Our studies suggest that most parents talk with their children about nutrition, and many parents talk with them about nutrition labels. Many of these conversations happen around mealtimes or at the grocery store. Parents who reported talking with their children about nutrition labels also perceived their children to be more knowledgeable about nutrition compared to parents who did not report talking to their children about nutrition labels. However, parents do not seem to use nutrition labels when they are making decisions about familiar foods. Instead, nutrition labels seem to be used primarily when considering the purchase of new food items. We found that parents’ judgements based on pictures alone (and therefore, only on prior knowledge) differed from those made when they had access to nutrition information alone. However, parents’ judgements when they had access to nutrition information and pictures of the items did not differ substantially from their judgements based on pictures alone. In sum, parents regularly make food choices for their children. Parents consider the nutritional content of foods, both when evaluating the healthiness of foods and in communicating with their children about those evaluations. However, parents do not always draw on nutrition information from labels, even when that information is available to them.
Highlights.
We investigated how parents decide if particular foods are healthy for their children
Parents of children (ages 4-12) rated the healthiness of foods
Parents rated healthiness primarily based on prior knowledge
Numerical representations (percentages vs. grams) did not affect healthiness ratings
Parents reported talking with children about nutrition and nutrition labels
Acknowledgements:
This research was supported by seed funding from the University of Wisconsin School of Human Ecology Center for Child and Family Well-Being and by a core grant to the Waisman Center from the National Institute of Child Health and Human Development (NICHD) (U54 HD090256). David Menendez was supported by the Institute of Education Sciences, U.S. Department of Education, through Award #R305B150003 to the University of Wisconsin-Madison. The opinions expressed are those of the authors and do not represent views of the U.S. Department of Education. We are grateful for contributions from Leah Szymborski and Porter Pavalko to the design of the stimuli.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams JM, Hart W, Gilmer L, Lloyd-Richardson EE, & Burton KA (2014). Concrete images of the sugar content in sugar-sweetened beverages reduces attraction to and selection of these beverages. Appetite, 83, 10–18. doi: 10.1016/j.appet.2014.07.027 [DOI] [PubMed] [Google Scholar]
- Addessi E, Galloway AT, Visalberghi E, & Birch LL (2005). Specific social influences on the acceptance of novel foods in 2–5-year-old children. Appetite, 45, 264–271. doi: 10.1016/j.appet.2005.07.007 [DOI] [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B, & Walker S (2015). Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software, 67(1), 1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Barr DJ, Levy R, Scheepers C, & Tily HJ (2013). Random effects structure for confirmatory hypothesis testing: Keep it maximal. Journal of Memory and Language, 68, 255–278. doi: 10.1016/j.jml.2012.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos S, Doxey J, & Hammond D (2011). Nutrition labels on pre-packaged foods: a systematic review. Public Health Nutrition, 14, 1496–1506. doi: 10.1017/s1368980010003290 [DOI] [PubMed] [Google Scholar]
- Capaldi ED, Owens JQ, & Privitera GJ (2006). Isocaloric meal and snack foods differentially affect eating behavior. Appetite, 46(2), 117–123. doi: 10.1016/j.appet.2005.10.008 [DOI] [PubMed] [Google Scholar]
- Cowburn G, and Stockley L (2004). Consumer understanding and use of labeling: a systematic review. Public Health Nutrition, 8, 21–28. doi: 10.1079/phn2005666 [DOI] [PubMed] [Google Scholar]
- DeJesus JM, Gelman SA, Viechnicki GB, Appugliese DP, Miller AL, Rosenblum KL, & Lumeng JC (2018). An investigation of maternal food intake and maternal food talk as predictors of child food intake. Appetite, 127, 356–363. doi: 10.1016/j.appet.2018.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeJesus JM, Shutts K, & Kinzler KD (2018). Mere social knowledge impacts children's consumption and categorization of foods. Developmental Science, 21, e12627. doi: 10.1111/desc.12627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebbeling CB, Pawlak DB, & Ludwig DS (2002). Childhood obesity: public-health crisis, common sense cure. The Lancet, 360, 473–482. doi: 10.1016/s0140-6736(02)09678-2 [DOI] [PubMed] [Google Scholar]
- George J (2014, February 24). Big changes to food labels gets thumbs up from dieticians. Philadelphia Business Journal, Retrieved from: https://www.bizjournals.com/philadelphia/blog/health-care/2014/02/food-labels.html [Google Scholar]
- Gigerenzer G, & Hoffrage U (1995). How to improve Bayesian reasoning without instruction: Frequency formats. Psychological Review, 102, 684–704. doi: 10.1037/0033-295X.102.4.684 [DOI] [Google Scholar]
- Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, & Colditz GA (2001). Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics, 108, E31. doi: 10.1542/peds.108.2.e31 [DOI] [PubMed] [Google Scholar]
- Gripshover SJ, & Markman EM (2013). Teaching young children a theory of nutrition: Conceptual change and the potential for increased vegetable consumption. Psychological Science, 24, 1541–1553. doi: 10.1177/0956797612474827 [DOI] [PubMed] [Google Scholar]
- Grolnick WS, Benjet C, Kurowski CO, & Apostoleris NH (1997). Predictors of parent involvement in children's schooling. Journal of Educational Psychology, 89, 538–548. doi: 10.1037//0022-0663.89.3.538 [DOI] [Google Scholar]
- Grunert KG (2010). Nutrition knowledge, and use and understanding of nutrition information on food labels among consumers in the UK. Appetite, 55, 177–189. doi: 10.1016/j.appet.2010.05.045 [DOI] [PubMed] [Google Scholar]
- Harper LV, & Sanders KM (1975). The effect of adults' eating on young children's acceptance of unfamiliar foods. Journal of Experimental Child Psychology, 20, 206–214. doi: 10.1016/0022-0965(75)90098-3 [DOI] [Google Scholar]
- Hendy HM, & Raudenbush B (2000). Effectiveness of teacher modeling to encourage food acceptance in preschool children. Appetite, 34, 61–76. doi: 10.1006/appe.1999.0286 [DOI] [PubMed] [Google Scholar]
- Hendy HM, Williams KE, Camise TS, Eckman N, & Hedemann A (2009). The Parent Mealtime Action Scale (PMAS). Development and association with children's diet and weight. Appetite, 52, 328–339. doi: 10.1016/j.appet.2008.11.003 [DOI] [PubMed] [Google Scholar]
- Karnik S, & Kanekar A (2012). Childhood obesity: a global public health crisis. International Journal of Preventative Medicine, 3, 1–7. doi: 10.1201/b18227-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumeng JC, Cardinal TM, Jankowski M, Kaciroti N, & Gelman SA (2008). Children's use of adult testimony to guide food selection. Appetite, 51, 302–310. doi: 10.1016/j.appet.2008.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LMS, & Cassady DL (2015). The effects of nutrition knowledge on food label use. A review of the literature. Appetite, 92, 207–216. doi: 10.1016/j.appet.2015.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss J, & Case R (1999). Developing children's understanding of the rational numbers: A new model and an experimental curriculum. Journal for Research in Mathematics Education, 30, 122–147. [Google Scholar]
- Nguyen SP (2007). An apple a day keeps the doctor away: Children's evaluative categories of food. Appetite, 48, 114–118. doi: 10.1016/j.appet.2006.06.001 [DOI] [PubMed] [Google Scholar]
- Nguyen SP (2012). The role of external sources of information in children's evaluative food categories. Infant and Child Development, 21, 216–235. doi: 10.1002/icd.745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen SP, & Murphy GL (2003). An apple is more than just a fruit: Cross-classification in children's concepts. Child development, 74(6), 1783–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble G, Stead M, Jones S, McDermott L, & McVie D (2007). The paradoxical food buying behaviour of parents: Insights from the UK and Australia. British Food Journal, 109, 387–398. doi: 10.1108/0070700710746795 [DOI] [Google Scholar]
- O’Dougherty M, Story M, & Stang J (2006). Observations of parent-child co-shoppers in supermarkets: children’s involvement in food selections, parental yielding, and refusal strategies. Journal of Nutrition Education and Behavior, 38(3), 183–188. [DOI] [PubMed] [Google Scholar]
- Ollberding NJ, Wolf RL, & Contento I (2011). Food label use and its relation to dietary intake among US adults. Journal of the American Dietetic Association, 111 S47–S51. doi: 10.1016/j.jada.2011.03.009 [DOI] [PubMed] [Google Scholar]
- Page B, Sharp A, Lockshin L, & Sorensen H (2018). Parents and children in supermarkets: Incidence and influence. Journal of Retailing and Consumer Services, 40, 31–39. [Google Scholar]
- Pesch MH, Harrell KJ, Kaciroti N, Rosenblum KL, & Lumeng JC (2011). Maternal styles of talking about child feeding across sociodemographic groups. Journal of the American Dietetic Association, 111, 1861–1867. doi: 10.1016/j.jada.2011.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provencher V, Polivy J, & Herman CP (2009). Perceived healthiness of food. If it's healthy, you can eat more!. Appetite, 52, 340–344. doi: 10.1016/j.appet.2008.11.005 [DOI] [PubMed] [Google Scholar]
- Quealy K & Sanger-Katz M (2016). Is Sushi ‘Healthy’? What About Granola? Where Americans and Nutritionists Disagree. The New York Times; Retrieved from https://nyti.ms/2jUmdOG [Google Scholar]
- R Core Team (2018). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: URL https://www.R-project.org/. [Google Scholar]
- Raman L (2014). Children's and adults' understanding of the impact of nutrition on biological and psychological processes. British Journal of Developmental Psychology, 32, 78–93. doi: 10.1111/bjdp.12024 [DOI] [PubMed] [Google Scholar]
- Robinson S (2000). Children's perceptions of who controls their food. Journal of Human Nutrition and Dietetics, 13, 163–171. doi: 10.1046/j.1365-277x.2000.00229.x [DOI] [PubMed] [Google Scholar]
- Ross BH, & Murphy GL (1999). Food for thought: Cross-classification and category organization in a complex real-world domain. Cognitive Psychology, 38, 495–553. [DOI] [PubMed] [Google Scholar]
- Sharf M, Sela R, Zentner G, Shoob H, Shai I, & Stein-Zamir C (2012). Figuring out food labels. Young adults’ understanding of nutritional information presented on food labels is inadequate. Appetite, 58, 531–534. doi: 10.1016/j.appet.2011.12.010 [DOI] [PubMed] [Google Scholar]
- Shutts K, Kinzler KD, McKee CB, & Spelke ES (2009). Social information guides infants' selection of foods. Journal of Cognition and Development, 10, 1–17. doi: 10.1080/15248370902966636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderBorght M, & Jaswal VK (2009). Who knows best? Preschoolers sometimes prefer child informants over adult informants. Infant and Child Development: An International Journal of Research and Practice, 18, 61–71. doi: 10.1002/icd.591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellman HM, & Johnson CN (1982). Children's understanding of food and its functions: A preliminary study of the development of concepts of nutrition. Journal of Applied Developmental Psychology, 3, 135–148. [Google Scholar]
- Wilson G, & Wood K (2004). The influence of children on parental purchases during supermarket shopping. International Journal of Consumer Studies, 28, 329–336. [Google Scholar]
- Wingert K, Zachary DA, Fox M, Gittelsohn J, & Surkan PJ (2014). Child as change agent. The potential of children to increase healthy food purchasing. Appetite, 81, 330–336. [DOI] [PubMed] [Google Scholar]