Abstract
Introduction:
Adolescents who identify as a sexual or gender minority are vulnerable to multiple health disparities due to stigma-based peer harassment. Given that sexual and gender minority adolescents may be bullied for several stigmatized identities that may exacerbate health risk, it is important to examine factors that can simultaneously reduce multiple forms of targeted victimization among sexual and gender minority adolescents. This study examines whether variation in health risk across sexual and gender minority adolescents who attend schools with versus without a gay-straight alliance can be explained by lessened bias-based bullying across a broad scope of stigmatized identities and attributes.
Methods:
Data on school-based gay-straight alliances, bias-based bullying, and health risk indicators were collected from the LGBTQ National Teen Survey (n=17,112; mean age=15.57 [SD=1.27] years) and analyzed in 2019. Multiple mediation analysis was conducted using latent variable structural equation modelling.
Results:
The majority (73%) of sexual and gender minority adolescents were bullied for stigmatized identities other than those related to their gender or sexual orientation. Compared to schools without a gay-straight alliance, student reports of multiple forms of bias-based bullying (based on body weight, gender, religion, disability, gender typicality, sexual orientation) were lower at schools with gay-straight alliances, which in turn attenuated adverse health outcomes (i.e., stress, sleep problems, depression, unhealthy weight control behaviors).
Conclusions:
Sexual and gender minority adolescents experience multiple forms of bias-based bullying, which independently heighten health risk, and this study extends previous work on gay-straight alliances to highlight a wider range of potential positive contributions to adolescent health.
INTRODUCTION
Health behaviors established during adolescence set the stage for long-term health outcomes, and contribute to lifecourse health disparities.1 This is particularly salient among youth who identify as a sexual or gender minority (SGM)—who are vulnerable to multiple health disparities.2,3 As early as middle school, SGM adolescents are at heightened risk for suicidality,3 depression,3 sleep troubles,4 as well as eating disorders5—risks that have been accounted for in part by the social stigma of their sexual and gender identities.6 Comparatively little, however, is known about how mistreatment related to other stigmatized identities and attributes (e.g., based on body weight, race/ethnicity, religion, disability status) contributes to SGM adolescent health. Given the potential of schools to cultivate broad-reaching climates of acceptance that support healthy outcomes,7 the present study extends existing research to shed light on the breadth of stigma reduction associated in particular with school-based gay-straight/gender-sexuality alliances (GSAs). Specifically, the current investigation examines whether GSA presence at school contributes to lower levels of bias-based bullying across a range of stigmatized identities and attributes, and in turn attenuates adverse health outcomes (i.e., depression, sleep, stress, unhealthy weight control behaviors) among a large, diverse national sample of SGM adolescents.
Growing evidence underscores the importance of a safe and supportive school climate for the health of SGM youth.8,9 Studies of GSAs (i.e., inclusive school-based organizations that bring together SGM youth and supportive non-SGM peers to address stigma and prejudice), in particular, have documented promising health outcomes for youth, regardless of whether students are GSA members themselves. For example, Poteat and colleagues10 found that youth in Wisconsin schools with a GSA reported less smoking, drinking, and suicide attempts than those in schools without a GSA. Although all youth—regardless of sexual orientation—exhibited more positive health outcomes at schools with GSAs, the effects were particularly strong for lesbian, gay, bisexual, transgender, and questioning (LGBTQ) youth,10 and do not appear to be fleeting. Indeed, reports of alcohol use, depression, and general psychological distress are lower among LGBT young adults who attended high school with, as opposed to without, a GSA.11
Although the underlying mechanisms linking GSAs to health status have yet to be explored, increasing evidence points to a reduction in peer mistreatment. Meta-analytic data, for example, indicate that SGM-based victimization is less common in schools with a GSA than without,12 and that victimization in turn can ―get under the skin‖ in ways that compromise health,13 especially when victimization is bias-based.14 The minority stress model, in particular, suggests heightened consequences for victimization that reinforces the stigmatization of one’s identity.15 Indeed, sexuality-based bullying is more strongly associated with depression and suicidality than generalized bullying.16
However, SGM youth are also vulnerable to other forms of peer victimization beyond those targeting their sexual and gender identities. In fact, recent findings indicate that sexual minority adolescents disproportionately are targets of both weight- and disability-based harassment from peers,17 each of which independently compromises health.14,18 Despite increased recognition that adolescents may have multiple stigmatized identities,19 no research to the authors’ knowledge has examined the relative contributions of other forms of bias-based bullying on the health of SGM adolescents. Moreover, given that the co-occurrence of multiple forms of bias-based bullying can compound health risk,20,21 it is critical to understand whether mechanisms of inclusion at school may be able to reduce multiple types of targeted victimization simultaneously. In other words, SGM-related health disparities may persist without efforts to identify mechanisms that reduce, in addition to victimization targeting gender and sexual orientation, also other forms of bias-based bullying.
To address this significant gap in research, the current study explores how health risk varies across SGM adolescents who attend schools with versus without a GSA, and whether such variation is related to experiences of bias-based bullying. Extending previous studies linking GSAs to less LGBTQ bullying,12 multiple forms of bias-based bullying (i.e., based on body weight, gender, race/ethnicity, religion, disability, gender typicality, sexual orientation) are assessed, each of which is expected to contribute uniquely to adolescents’ health outcomes. Presuming that the social acceptance fostered by GSAs might spill over to cultivate a broadly inclusive school climate, GSA presence at school is expected to be associated with lower levels of each type of bias-based bullying, and in turn attenuate health risk among SGM adolescents (i.e., lower levels of depression, sleep problems, stress, and unhealthy weight control behaviors). Along with assessing links between GSAs and depression, which have been examined previously,11,22 the present study focuses on additional health indicators of sleep (i.e., difficulty falling asleep), weight control behaviors, and stress, which are relevant to both short- and long- term adolescent health.23–25
METHODS
Study Sample
Data for this study came from a large national web-based survey of SGM adolescents (LGBTQ National Teen Survey).26 All participants (aged 13–17 years) were currently living in the U.S., spoke English, and identified as LGBTQ. A total of 29,291 adolescents began the survey. The final analytic sample (n=17,112) excluded those who screened ineligible (e.g., outside the age range; n=8,985), completed <10% of the survey (n=3,006), or were flagged in post-hoc mischievous responder’s sensitivity analyses.26
The University of Connecticut’s IRB approved the study. Participants were recruited in partnership with the Human Rights Campaign (HRC) through social media outlets (Facebook, Twitter, Instagram, Snapchat, Reddit), HRC’s network of community partners, and with assistance of social influencers in the LGBTQ community. Adolescents interested in the survey began after reading information about the study’s purpose and procedures, and after accepting the study conditions and giving assent (a waiver of parental consent was obtained from the IRB). To compensate for participation, adolescents could choose to enter a raffle for a random drawing of gift cards and were offered HRC wristbands. Data were collected online from April to December in 2017, and analyzed in 2019. Additional information describing the details of data collection, screening procedures, recruitment, and sample composition are reported elsewhere.26
Measures
Several demographic variables were controlled for in the current analyses, along with relevant covariates, including disability status, BMI, and disclosure of SGM identity to classmates (i.e., ―“outness”). Participants reported their sex at birth (male/female), in addition to their current gender identity (male/female/transgender male/transgender female/non- binary/genderqueer/something else). Gender identity was dichotomized as cisgender (i.e., youth who reported a natal sex at birth concordant with their gender identity; e.g., a male assigned at birth who identified as a cisgender male) or transgender (i.e., youth who reported a natal sex at birth discordant with their gender identity; e.g., a male assigned at birth who identified as transgender or non-binary).26 To assess sexual orientation, participants selected from a series of response options: gay or lesbian, bisexual, straight, queer, pansexual, asexual, questioning, and other (e.g., demisexual). Ethnicity was self-reported and represented by four dummy variables (African American, Latino, Asian, other ethnicity) using white students (the largest ethnic group in the sample) as the reference group. Participant age and parental level of education were also included in the analyses.
Additionally, the analyses controlled for self-reported disability status (0=no disability, 1=disability), as well as BMI percentile, which was determined using the Centers for Disease Control growth charts based on height, weight, age, and sex (i.e., participants’ self-reported sex assigned at birth). Finally, outness to classmates was assessed by asking participants how many classmates currently they think know of their sexual orientation. A binary indicator was created to compare students reporting that no (17%) versus at least one (83%) classmate know of their sexual orientation.
Participants self-reported whether or not their school had a GSA (0=no, 1=yes).
To assess experiences of bias-based bullying, adolescents were asked how often on a 5-point scale (0=never to 4=very often) they are teased or treated badly by other students at school for each of the following reasons: body weight, gender, race/ethnicity, sexuality, religion, disability, and gender typicality.
Four health risk outcome variables were assessed: self-reported depression, sleep problems, unhealthy weight control behaviors, and stress. To assess depression, ten items were adapted from Kutcher’s Adolescent Depression Scale27 (mean=1.35, SD=0.75, α=0.90). Sleep problems were assessed by asking participants to indicate how often they had trouble getting to sleep (mean=2.15, SD=1.19; scale: 0 [never] to 4 [always]), and stress was assessed by self-reported average level of stress (mean=6.47, SD=1.96) using a scale of 1 (not at all stressed) to 10 (very stressed).28 Nine items from Project EAT (a longitudinal cohort study examining eating and activity behaviors in ethnically and socioeconomically diverse young people)29 were used to measure unhealthy weight control behaviors (e.g., vomiting, using laxatives, smoking) that adolescents engaged in during the past year on a scale of 0 (never) to 3 (on a regular basis) (mean=0.50, SD=0.48, α=0.79).
Statistical Analysis
Latent variable structural equation modeling was used to test the relations among the study constructs in Mplus, version 8.0. Full information maximum likelihood estimation methods were used for missing data. Confirmatory factor analysis was conducted to evaluate factorial validity of the latent health risk construct before building the structural equation model. Following recommended procedures,30 all ―“a” paths (i.e., each type of bias-based bullying on GSA) and ―“b” paths (i.e., health risk on each type of bias-based bullying) were estimated simultaneously, while accounting for covariates. The Model Constraint command was used to estimate the indirect effect of GSAs on health risk through each type of bias-based bullying (c’).
RESULTS
Table 1 summarizes sample demographic characteristics. Sixty-three percent of adolescents reported attending schools with a GSA. In addition to the means and SDs, intercorrelations among the continuously modelled variables are depicted in Table 2. Although the indicators of bias-based bullying all capture targeted victimization, they were only slightly to moderately correlated (range=0.13–0.55), suggesting that they are related, but distinct, constructs. The intercorrelations also revealed each type of bias-based bullying to be associated with the health risk indicators.
Table 1.
Sample Demographics (N=17,112)
| Variable | n (%) | Mean | SD |
|---|---|---|---|
| Age, range | 13.00–17.00 | 15.57 | 1.27 |
| BMI percentile, range | 0.00–99.90 | 65.50 | 30.49 |
| Sex | |||
| Male | 4,739 (27.7) | ||
| Female | 12,373 (72.3) | ||
| Ethnicity | |||
| White | 10,225 (61.9) | ||
| African American | 952 (5.8) | ||
| Latino | 1,877 (11.4) | ||
| Asian | 677 (4.1) | ||
| Other | 2,797 (16.8) | ||
| Gender identity | |||
| Cisgender | 11,475 (67.1) | ||
| Transgender | 5,637 (32.9) | ||
| Sexual orientation | |||
| Gay or Lesbian | 6,401 (37.4) | ||
| Bisexual | 5,970 (34.9) | ||
| Straight | 279 (1.6) | ||
| Pansexual | 2,256 (13.2) | ||
| Queer | 699 (4.1) | ||
| Asexual | 725 (4.2) | ||
| Questioning | 424 (2.5) | ||
| Other | 358 (2.1) |
Table 2.
Means, SDs, and Intercorrelations Among Continuously Modelled Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Weight-based bullying | - | |||||||||||||
| 2. Gender-based bullying |
0.29 *** |
- | ||||||||||||
| 3. Race/ethnicity-based bullying |
0.23 *** |
0.19 *** |
- | |||||||||||
| 4. Religion-based bullying |
0.23 *** |
0.26 *** |
0.20 *** |
- | ||||||||||
| 5. Disability-based bullying |
0.23 *** |
0.28 *** |
0.13 *** |
0.22 *** |
- | |||||||||
| 6. Gender typicality-based bullying |
0.33 *** |
0.45 *** |
0.19 *** |
0.23 *** |
0.23 *** |
- | ||||||||
| 7. Sexuality-based bullying |
0.39 *** |
0.43 *** |
0.21 *** |
0.27 *** |
0.24 *** |
0.55 *** |
- | |||||||
| 8. Depression |
0.33 *** |
0.33 *** |
0.17 *** |
0.17 *** |
0.26 *** |
0.27 *** |
0.30 *** |
- | ||||||
| 9. Sleep problems |
0.22 *** |
0.22 *** |
0.11 *** |
0.13 *** |
0.17 *** |
0.19 *** |
0.19 *** |
0.52 *** |
- | |||||
| 10. Stress |
0.21 *** |
0.23 *** |
0.09 *** |
0.13 *** |
0.16 *** |
0.18 *** |
0.20 *** |
0.50 *** |
0.28 *** |
- | ||||
| 11. Unhealthy weight control behaviors |
0.38 *** |
0.29 *** |
0.17 *** |
0.18 *** |
0.20 *** |
0.24 *** |
0.28 *** |
0.47 *** |
0.29 *** |
0.25 *** |
- | |||
| 12. BMI percentile |
0.24 *** |
0.05 *** |
0.04 *** |
0.02 * |
0.03 ** |
‒0.01 | 0.02* |
0.10 *** |
0.07 *** |
0.04 *** |
0.20 *** |
- | ||
| 13. Parental level of |
‒0.12 *** |
‒0.03 *** |
‒0.09 *** |
‒0.01 | ‒0.01 |
‒0.08 *** |
‒0.10 *** |
‒0.14 *** |
‒0.08 *** |
‒0.02 |
‒0.14 *** |
‒0.11 *** |
- | |
| 14. Age |
‒0.03 ** |
‒0.07 *** |
‒0.02 * |
‒0.02 * |
‒0.02 | ‒0.02 |
‒0.07 *** |
‒0.07 *** |
‒0.11 *** |
0.02* | ‒0.01 |
‒0.04 *** |
‒0.03 ** |
- |
| Mean | 1.16 | 1.01 | 0.55 | 0.52 | 0.35 | 1.45 | 1.52 | 1.35 | 2.15 | 6.47 | 0.50 | 65.50 | 4.19 | 15.57 |
| SD | 1.21 | 1.20 | 0.95 | 0.97 | 0.85 | 1.32 | 1.28 | 0.75 | 1.19 | 1.96 | 0.48 | 30.49 | 1.59 | 1.27 |
Note: Boldface indicates statistical significance (
p<0.001
p<0.01
p<0.05).
Across the present sample of SGM adolescents, 91% reported at least one experience of bias- based bullying—more than double estimates in predominantly non-SGM samples (36%–40%).14 Moreover, 73% reported experiences of bias-based bullying other than those related to their gender or sexual identities (e.g., based on disability, race/ethnicity, religion, body weight). Table 3 presents the rates of each type of bias-based bullying, broken down by ethnicity and sex. Bullying based on sexual orientation (68%), gender typicality (63%), and weight (57%) were most common, with more than half of the sample reporting at least one instance of each of the aforementioned, followed by gender-based (48%), race/ethnicity-based (30%), religious-based (27%), and disability-based (17%) bullying. Bullying based on race/ethnicity was reported as less common among white students, and bullying based on gender was reported less frequently among male students.
Table 3.
Percent of Adolescents Reporting at Least One Instance of Each Type of Bias-based Bullying
| Bias-based bullying | Total sample (%) | White (%) | African American (%) | Latino/a (%) | Asian (%) | Other ethnic (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | ||
| Weight-based | 57 | 58 | 53 | 49 | 53 | 60 | 56 | 43 | 54 | 63 | 55 |
| Gender-based | 48 | 58 | 23 | 40 | 22 | 56 | 21 | 50 | 26 | 61 | 27 |
| Race/Ethnicity-based | 30 | 14 | 15 | 57 | 62 | 63 | 52 | 77 | 66 | 59 | 55 |
| Sexuality-based | 68 | 68 | 76 | 47 | 74 | 66 | 71 | 52 | 65 | 67 | 74 |
| Religious-based | 27 | 28 | 23 | 22 | 19 | 27 | 16 | 28 | 21 | 31 | 25 |
| Disability-based | 17 | 19 | 11 | 12 | 9 | 16 | 6 | 12 | 11 | 24 | 11 |
| Gender typicality-based | 63 | 59 | 76 | 57 | 82 | 60 | 75 | 52 | 71 | 61 | 73 |
Note: “Other ethnic” refers to adolescents who self-reported an ethnic group other than the four pan-ethnic groups.
To evaluate factorial validity for the health risk latent variable, confirmatory factor analysis was conducted first. Multiple fit indices suggested a good measurement model (χ2[2]=6.34, p=0.04; standardized root mean square residual=0.01; comparative fit index=0.99; Tucker-Lewis index=0.99; root mean square error of approximation [RMSEA]=0.01; RMSEA CI=0.00, 0.03). The mediation model in turn showed acceptable fit (χ2[91]=3,695.60, p<0.001; standardized root mean square residual=0.03; RMSEA=0.05; RMSEA CI=0.047, 0.049), with all factor loadings >0.50. As shown in Figure 1, after accounting for the covariates (i.e., sex, gender, sexual orientation, ethnicity, disability status, BMI, parental level of education, age, outness to classmates), presence of a GSA at school was associated with less weight- (β= −0.07, p<.001), gender- (β = −0.02, p=0.019), religion- (β = −0.08, p<0.001), disability- (β = −0.03, p<0.001), gender typicality– (β = −0.06, p<0.001), and sexuality-based (β = −0.09, p<0.001) bullying. Additionally, each type of bias-based bullying was positively related to health risk (weight: β =0.21, p<0.001; gender: β=0.05, p=0.001; race/ethnicity: β=0.05, p<0.001; religion: β=0.03, p=0.001; disability: β=0.04, p=0.016; gender typicality: β=0.10, p<0.001; sexuality: β=0.15, p<0.001). The total effect of GSA on health risk was significant, such that presence of a GSA at school was related to reduced health risk (β= −0.06, p<0.001). Tests of indirect effects revealed significant indirect paths from GSA presence to health risk for each type of bias-based bullying (weight: b= −0.019, p<0.001; gender: b= −0.001, p=0.051; religion: b= −0.004, p=0.003; disability: b= −0.002, p=0.042; gender typicality: b= −0.008, p<0.001; sexuality: b= −0.018, p<0.001), with the exception of race/ethnicity (for which the “a” path‖ was non-significant). Thus, the association between GSAs and reduced health risk can be partially accounted for by lower levels of multiple forms of bias-based bullying.
Figure 1. Standardized coefficients for model testing mediation of gay-straight alliance (GSA) presence, bias-based bullying and health risk.
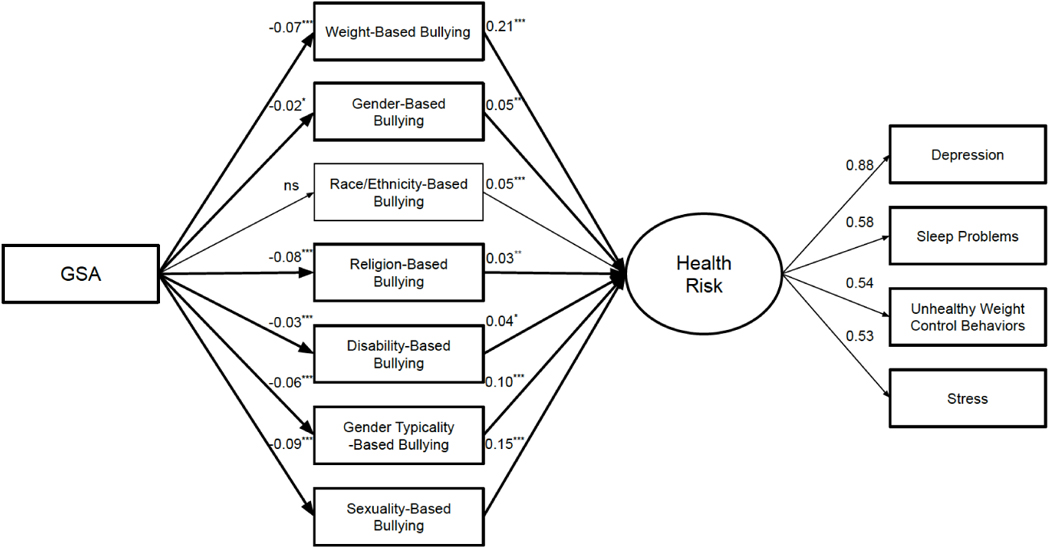
Note: Bolded lines indicate significant indirect effects. All paths control for sex, gender, sexual orientation, ethnicity, disability status, BMI, parental level of education, age, and outness to classmates. χ2(91)=3695.60, p<0.001; SRMR=0.03; RMSEA=0.05; RMSEA CI=0.047–0.049. ***p<0.001; **p<0.01; *p<0.05.
DISCUSSION
The current findings extend prior research on GSAs to highlight a wider range of potential positive contributions to adolescent health. Expanding the breadth of health effects beyond mental health22 and substance use,10 the results show how GSAs also contribute to lower levels of stress, sleep problems, and unhealthy weight control behaviors among SGM youth, and shed light on potential mechanisms underlying such associations. Specifically, in addition to reductions in LGBTQ-related victimization from peers at school, the present findings indicate that GSAs are related to reductions in bullying across a broad scope of other stigmatized identities and attributes, such as weight, religion, and disability. This is important not only because SGM youth may possess multiple stigmatized identities for which they are bullied, but also because each type of bias-based bullying was found to be a unique health risk factor, even after accounting for relevant covariates (i.e., participants’ age, sex, ethnicity, gender identity, sexual identity, disability status, parental level of education, BMI, and outness to classmates).
The present results provide novel insights that underscore school-based bullying—especially victimization targeting personal attributes and identities—as a significant health concern. In particular, depression, stress, sleep trouble, and unhealthy weight control behaviors were found to be elevated among SGM adolescents who experienced more frequent bias-based bullying. Moreover, these associations were persistent across each form of targeted peer mistreatment. Although more negative outcomes have been documented for youth experiencing multiple, as opposed to one, type of bias-based bullying,21 the present investigation is among the first to examine the relative contributions of bullying based on multiple specific identities and attributes to adolescent health. Comparison across standardized coefficients revealed that weight-based bullying was most strongly linked to adverse health (followed by sexuality-based bullying). The high degree of perceived controllability surrounding body weight31 may intensify feelings of self-blame following weight-based mistreatment in ways that tax physical and psychological health.32 Given that the health consequences of weight-based victimization in adolescence persist into adulthood,18 and that sexual minority youth are disproportionately targeted,17 it will be important for future studies to examine how weight-based mistreatment may contribute to lifecourse SGM health disparities.2,3
The present study shows that the documented social challenges facing SGM youth go beyond those tied to their sexual and gender identities. In fact, the majority of adolescents in the current sample (73%) were bullied for identities and attributes unrelated to their gender or sexual orientation. Specifically, more than half of the SGM youth in the sample reported experiencing weight-based bullying, and almost a third were victimized because of their race/ethnicity and religious affiliation. Thus, rather than adhering to a one-size-fits-all approach by considering bias-based bullying related to a single social identity (e.g., sexual orientation or disability or religion), it is critical to recognize that adolescents may experience multiple forms of targeted harassment that each independently exacerbate health risk. As such, identifying mechanisms to increase inclusion and acceptance overall (as opposed to targeting specific groups) may be a more comprehensive and effective approach to reducing the multiple forms of bias-based bullying that SGM youth face.
Supporting recent calls for schools to take proactive steps to promote inclusion,7 the present findings highlight GSAs in particular as a potential mechanism of stigma reduction across a wide range of social identities that place youth at risk for bullying. More work is needed to determine the nature of this relationship, including potential reasons why GSAs may reduce multiple forms of bias-based bullying. One possible explanation is a “diffusion of inclusion” effect, where schoolwide acceptance of SGM youth through GSAs fosters a broadly inclusive school climate that spills over to increase acceptance of those possessing other stigmatized identities or attributes (e.g., high body weight). Support for GSAs affecting the overall school climate comes from studies showing that all students—regardless of sexual orientation—are better adjusted in schools with, versus without, GSAs.10
Limitations
Several study limitations should be noted. First, this investigation is cross-sectional, and therefore causation cannot be inferred. In addition, there may be fundamental differences between schools with and without GSAs that contribute to health risk that were not assessed in this study. For example, evidence suggests that GSAs are more common in schools with a greater proportion of students from higher socioeconomic backgrounds,10 who are at a health advantage.33 Future multilevel studies that take into account school- (e.g., anti-bullying policies) and community-level (e.g., political orientation) differences could help tease apart GSA effects from other contextual characteristics. Second, GSA membership was not assessed, only GSA presence at school. Investigating whether individual differences in GSA involvement (e.g., membership duration, engagement), offer additional health benefits beyond GSA presence will be important to examine in future research.
Additionally, despite a large, diverse sample of SGM adolescents, the current findings cannot be generalized to those who do not utilize or have access to online networks where HRC advertised the study. Also, as gender identity was dichotomized because of the complexity of the analytic models, the authors were unable to disentangle nuances in the associations between GSAs and bias-based bullying across diverse gender minorities—particularly non-binary or genderqueer youth, who may not self-identify as transgender but were classified as such in this paper. Finally, all measures in this study were self-reported by adolescents. Thus, it will be important to replicate the current findings with objective assessments, such as peer nominations of victimization and physiological assessment of health indices (e.g., actigraphy to measure sleep, cortisol levels to capture stress). Furthermore, BMI was calculated based on self-reported data (height, weight, age, sex assigned at birth), and given increasing discussion regarding BMI guidelines that are gender inclusive,34 future research should be cognizant of changes for measurement of BMI among transgender youth if new guidelines emerge.
CONCLUSIONS
The current study highlights that the social challenges negatively affecting the health of SGM adolescents extend beyond those related to their sexual and gender identities. In considering approaches to mitigate health risk, increased attention is needed toward the wide range of bias- based bullying experienced by SGM adolescents. Given the breadth of stigma reduction across multiple social identities, school-based GSAs represent a promising avenue to support healthy outcomes for SGM youth.
ACKNOWLEDGMENTS
This research uses data from the LGBTQ Teen Study, designed by Ryan J. Watson and Rebecca M. Puhl in collaboration with the Human Rights Campaign, and supported by the Office for Vice President of Research at the University of Connecticut. The authors acknowledge the intensive efforts of Ellen Kahn, Gabe Murchison, and Liam Miranda in their support, conceptualization, and management related to the LGBTQ Teen Study.
This project was supported by the Research Excellent Program of the Office of the Vice President for Research at the University of Connecticut. Ryan J. Watson was also supported by a National Institute on Drug Abuse grant (K01DA047918). Any interpretations and opinions expressed herein are solely those of the authors and may not reflect those of the NIH.
LML conceived of the current study, participated in analysis and interpretation of the data, and helped to draft the manuscript. RMP conceived of the current study, participated in analysis and interpretation of the data, helped to draft the manuscript, and was a principal investigator on the larger project from which the present analyses were conducted. RJW conceived of the current study, participated in analysis and interpretation of the data, helped to draft the manuscript, and was a principal investigator on the larger project from which the present analyses were conducted. All authors read and approved the final manuscript.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–2478. 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hafeez H, Zeshan M, Tahir MA, Jahan N, Naveed S. Health care disparities among lesbian, gay, bisexual, and transgender youth: a literature review. Cureus. 2017;9(4):e1184. 10.7759/cureus.1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marshal MP, Dietz LJ, Friedman MS, et al. Suicidality and depression disparities between sexual minority and heterosexual youth: a meta-analytic review. J Adolesc Health. 2011;49(2):115–123. 10.1016/j.jadohealth.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang Y, Li P, Lai Z, et al. Role of sleep quality in mediating the relationship between sexual minority status and suicidal behavior among Chinese adolescents. Psychol Res Behav Manag. 2018;11:607–615. 10.2147/prbm.s186586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Connolly MD, Zervos MJ, Barone CJ, Johnson CC, Joseph CLM. The mental health of transgender youth: advances in understanding. J Adolesc Health. 2016;59(5):489–495. 10.1016/j.jadohealth.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 6.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. 10.2105/ajph.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Juvonen J, Lessard LM, Rastogi R, Schacter HL, Smith DS. Promoting social inclusion in educational settings: challenges and opportunities. Educ Psychol. 2019;54(4):250–270. 10.1080/00461520.2019.1655645. [DOI] [Google Scholar]
- 8.Hatzenbuehler ML, Birkett M, Van Wagenen A, Meyer IH. Protective school climates and reduced risk for suicide ideation in sexual minority youths. Am J Public Health. 2013;104(2):279–286. 10.2105/ajph.2013.301508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sandfort TGM, Bos HMW, Collier KL, Metselaar M. School environment and the mental health of sexual minority youths: a study among Dutch young adolescents. Am J Public Health. 2010;100(9):1696–1700. 10.2105/ajph.2009.183095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poteat VP, Sinclair KO, DiGiovanni CD, Koenig BW, Russell ST. Gay–straight alliances are associated with student health: a multischool comparison of LGBTQ and heterosexual youth. J Res Adolesc. 2013;23(2):319–330. 10.1111/j.1532-7795.2012.00832.x. [DOI] [Google Scholar]
- 11.Heck NC, Flentje A, Cochran BN. Offsetting risks: high school gay-straight alliances and lesbian, gay, bisexual, and transgender (LGBT) youth. Psychol Sex Orientat Gend Divers. 2013;1(S):81–90. 10.1037/2329-0382.1.s.81. [DOI] [Google Scholar]
- 12.Marx RA, Kettrey HH. Gay-straight alliances are associated with lower levels of school- based victimization of LGBTQ+ youth: a systematic review and meta-analysis. J Youth Adolesc. 2016;45(7):1269–1282. 10.1007/s10964-016-0501-7. [DOI] [PubMed] [Google Scholar]
- 13.Gini G, Pozzoli T. Association between bullying and psychosomatic problems: a meta- analysis. Pediatrics. 2009;123(3):1059–1065. 10.1542/peds.2008-1215. [DOI] [PubMed] [Google Scholar]
- 14.Russell ST, Sinclair KO, Poteat VP, Koenig BW. Adolescent health and harassment based on discriminatory bias. Am J Public Health. 2012;102(3):493–495. 10.2105/ajph.2011.300430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patrick DL, Bell JF, Huang JY, Lazarakis NC, Edwards TC. Bullying and quality of life in youths perceived as gay, lesbian, or bisexual in Washington state, 2010. Am J Public Health. 2013;103(7):1255–1261. 10.2105/ajph.2012.301101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bucchianeri MM, Gower AL, McMorris BJ, Eisenberg ME. Youth experiences with multiple types of prejudice-based harassment. J Adolesc. 2016;51:68–75. 10.1016/j.adolescence.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 18.Puhl RM, Wall MM, Chen C, Bryn Austin S, Eisenberg ME, Neumark-Sztainer D. Experiences of weight teasing in adolescence and weight-related outcomes in adulthood: a 15-year longitudinal study. Prev Med. 2017;100:173–179. 10.1016/j.ypmed.2017.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghavami N, Peplau LA. Urban middle school students’ stereotypes at the intersection of sexual orientation, ethnicity, and gender. Child Dev. 2018;89(3):881–896. 10.1111/cdev.12763. [DOI] [PubMed] [Google Scholar]
- 20.Garnett BR, Masyn KE, Austin SB, Miller M, Williams DR, Viswanath K. The intersectionality of discrimination attributes and bullying among youth: an applied latent class analysis. J Youth Adolesc. 2014;43(8):1225–1239. 10.1007/s10964-013-0073-8. [DOI] [PubMed] [Google Scholar]
- 21.Mulvey KL, Hoffman AJ, Gönültaş S, Hope EC, Cooper SM. Understanding experiences with bullying and bias-based bullying: what matters and for whom? Psychol Violence. 2018;8(6):702–711. 10.1037/vio0000206. [DOI] [Google Scholar]
- 22.Toomey RB, Ryan C, Diaz RM, Russell ST. High school gay–straight alliances (GSAs) and young adult well-being: an examination of GSA presence, participation, and perceived effectiveness. Appl Dev Sci. 2011;15(4):175–185. 10.1080/10888691.2011.607378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014;18(1):75–87. 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: findings from a 10-year longitudinal study. J Am Diet Assoc. 2011;111(7):1004–1011. 10.1016/j.jada.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eiland L, Romeo RD. Stress and the developing adolescent brain. Neuroscience. 2013;249:162–171. 10.1016/j.neuroscience.2012.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watson RJ, Wheldon CW, Puhl RM. Evidence of diverse identities in a large national sample of sexual and gender minority adolescents. J Res Adolesc. 2020;30(S2):431–442. 10.1111/jora.12488. [DOI] [PubMed] [Google Scholar]
- 27.LeBlanc JC, Almudevar A, Brooks SJ, Kutcher S. Screening for adolescent depression: comparison of the Kutcher Adolescent Depression Scale with the Beck Depression Inventory. J Child Adolesc Psychopharmacol. 2002;12(2):113–126. 10.1089/104454602760219153. [DOI] [PubMed] [Google Scholar]
- 28.Wadden TA, Foster GD. Weight and Lifestyle Inventory (WALI). Obesity (Silver Spring). 2006;14(suppl 3):99S–118S. 10.1038/oby.2006.289. [DOI] [PubMed] [Google Scholar]
- 29.Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J Obes. 2002;26(1):123–131. 10.1038/sj.ijo.0801853. [DOI] [PubMed] [Google Scholar]
- 30.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 31.Martin SB, Rhea DJ, Greenleaf CA, Judd DE, Chambliss HO. Weight control beliefs, body shape attitudes, and physical activity among adolescents. J Sch Health. 2011;81(5):244–250. 10.1111/j.1746-1561.2011.00585.x. [DOI] [PubMed] [Google Scholar]
- 32.Graham S, Juvonen J. Self-blame and peer victimization in middle school: an attributional analysis. Dev Psychol. 1998;34(3):587–599. 10.1037/0012-1649.34.3.587. [DOI] [PubMed] [Google Scholar]
- 33.Hanson MD, Chen E. Socioeconomic status and health behaviors in adolescence: a review of the literature. J Behav Med. 2007;30(3):263–285. 10.1007/s10865-007-9098-3. [DOI] [PubMed] [Google Scholar]
- 34.Kidd KM, Sequeira GM, Dhar CP, Montano GT, Witchel SF, Rofey D. Gendered body mass index percentile charts and transgender youth: making the case to change charts. Transgend Health. 2019;4(1):297–299. 10.1089/trgh.2019.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]


