Abstract
Introduction:
Simulation models can improve measurement and understanding of mental health conditions in the population. Major depressive episodes are a common and leading cause of disability but are subject to substantial recall bias in survey assessments. This study illustrates the application of a simulation model to quantify the full burden of major depressive episodes on population health in the U.S.
Methods:
A compartmental model of major depressive episodes that explicitly simulates individuals’ under-reporting of past episodes was developed and calibrated to 2005–2017 National Surveys on Drug Use and Health data. Parameters for incidence of a first major depressive episode and the probability of under-reporting past episodes were estimated. Analysis was conducted from 2017 to 2019.
Results:
The model estimated that 30.1% of women (95% range: 29.0%–32.5%) and 17.4% of men (95% range: 16.7%–18.8%) have lifetime histories of a major depressive episode after adjusting for recall error. Among all adults, 13.1% (95% range: 8.1%–16.5%) of women and 6.6% (95% range: 4.0%–8.3%) of men failed to report a past major depressive episode. Under-reporting of a major depressive episode history in adults age >65 years was estimated to be 70%.
Conclusions:
Simulation models can address knowledge gaps in disease epidemiology and prevention and improve surveillance efforts. This model quantifies under-reporting of major depressive episodes and provides parameter estimates for future research. After adjusting for under-reporting, 23.9% of adults have a lifetime history of major depressive episodes, which is much higher than based on self-report alone (14.0%). Far more adults would benefit from depression prevention strategies than what survey estimates suggest.
INTRODUCTION
Mental health prevention strategies aim to reduce the incidence, recurrence, and prevalence of mental disorders, but are constrained by the lack of accurate, nationally representative surveillance assessments. Major depressive episodes (MDEs), which occur among those with major depressive disorder (MDD), bipolar disorder, and persistent depressive disorder, are leading contributors to disability worldwide.1,2 The authors’ analysis of the 2017 National Survey on Drug Use and Health (NSDUH) shows that more than 34 million adults (17.1% and 10.7% of women and men) report a lifetime history of at least one MDE,3 but the burden of MDEs on population health is likely misestimated by available survey data.
Cross-sectional surveys, including the NSDUH, assess lifetime history of psychiatric disorders retrospectively, but longitudinal studies show that assessments are prone to under-reporting.4 The Baltimore Epidemiological Catchment Area (ECA) Study found that in a 25-year period, lifetime prevalence of MDD was nearly three times greater using cumulative evaluations compared with retrospective evaluations (4.5% vs 13.1%).5 Cross-sectional surveys unexpectedly show that lifetime prevalence of MDD declines, rather than increases, with age.6 The National Comorbidity Survey–Replication showed lifetime prevalence of MDD across age groups increased as expected through age 18–44 years and dropped to 10.6% for those aged older than 60 years.7 Differential mortality and symptomatic differences in depression among older adults,8 or differences in incidence by birth cohort could explain this pattern. However, failure to recall earlier depressive episodes, particularly among older people, could result in artificial decreases in lifetime prevalence with age. Although the NSDUH provides timely cross-sectional assessments of psychopathology, it underestimates lifetime MDE prevalence by relying on retrospective reporting. Prospective cohort studies that address recall bias are costly to implement, often specific to a geographic location (e.g., Baltimore ECA), or have few data waves; even prospective studies can be subject to under-reporting.9
Simulation modeling offers an innovative methodology to fill gaps in understanding depression epidemiology and estimate its true burden on population health.10,11 Models can integrate existing information to represent processes that contribute to observed data. Other countries have documented declining lifetime depression prevalence with age, but only two simulation studies have investigated it. One microsimulation study using Australian and Dutch data addressed recall error to re-estimate lifetime depression prevalence in the population, but excluded adults aged older than 65 years who are likely to under-report.12 A Canadian discrete event simulation study investigated decreasing lifetime prevalence of MDD by age,13 but assumed a monotonically decreasing incidence function with age and zero onset before age 15 years (U.S. epidemiological data indicate the contrary14,15). To date, no simulation analysis has evaluated the impact of recall error on U.S. lifetime depression prevalence estimates.
This simulation study combines cross-sectional and prospective cohort data to address mismeasurement of a commonly occurring health condition. The model generates incidence and recall error parameters that do not yet exist in the literature and produces revised national estimates for lifetime MDE prevalence.
METHODS
Study Sample
The NSDUH is a nationally representative cross-sectional survey of the U.S. civilian non-institutionalized population, with comparable measures of MDEs from 2005 to 2017. This study used data for the adult population (approximately 36,000–44,000 respondents per year). The NSDUH defines a MDE as a period lasting ≥2 weeks during the past year (or over the lifetime) during which the respondent reports at least five of nine symptoms: (1) depressed mood, (2) diminished interest in activities, (3) changes in weight or appetite, (4) insomnia or hypersomnia, (5) psychomotor symptoms, (6) fatigue, (7) feeling worthless, (8) problems thinking, and (9) thoughts of death or suicide—at least one of which must be depressed mood or diminished interest in activities.16 Although this measurement of MDEs is based on DSM criteria,2 it does not exclude episodes due to illness, bereavement, or substance use.
The ECA study followed a 1981 baseline cohort of 3,481 adult household residents in East Baltimore and repeated assessments in 1982, 1993–1996, and 2004–2005. Participants provided information about depressive episodes based on the question: During that year, was there ever a time when you were feeling sad, depressed, or blue, and had some of these other problems like [list of DSM criteria for MDD]?14
Model Overview
Figure 1 shows the model structure. The compartmental model has stocks (boxes) for depressive states and transition probabilities governing the flow (arrows) of individuals moving across them. The model includes three possible MDE states. In this study, “past-year MDE” (black) refers to individuals with a MDE within the past 12 months, including a first or recurrent episode. “Former MDE” refers to individuals who report a lifetime history of at least one MDE but no episode within the past year (gray). “Never MDE” refers to those who report no lifetime history of a MDE (white). This model explicitly includes a “recall error” state for people who report no lifetime history of MDEs, but who are former MDE.
Figure 1.
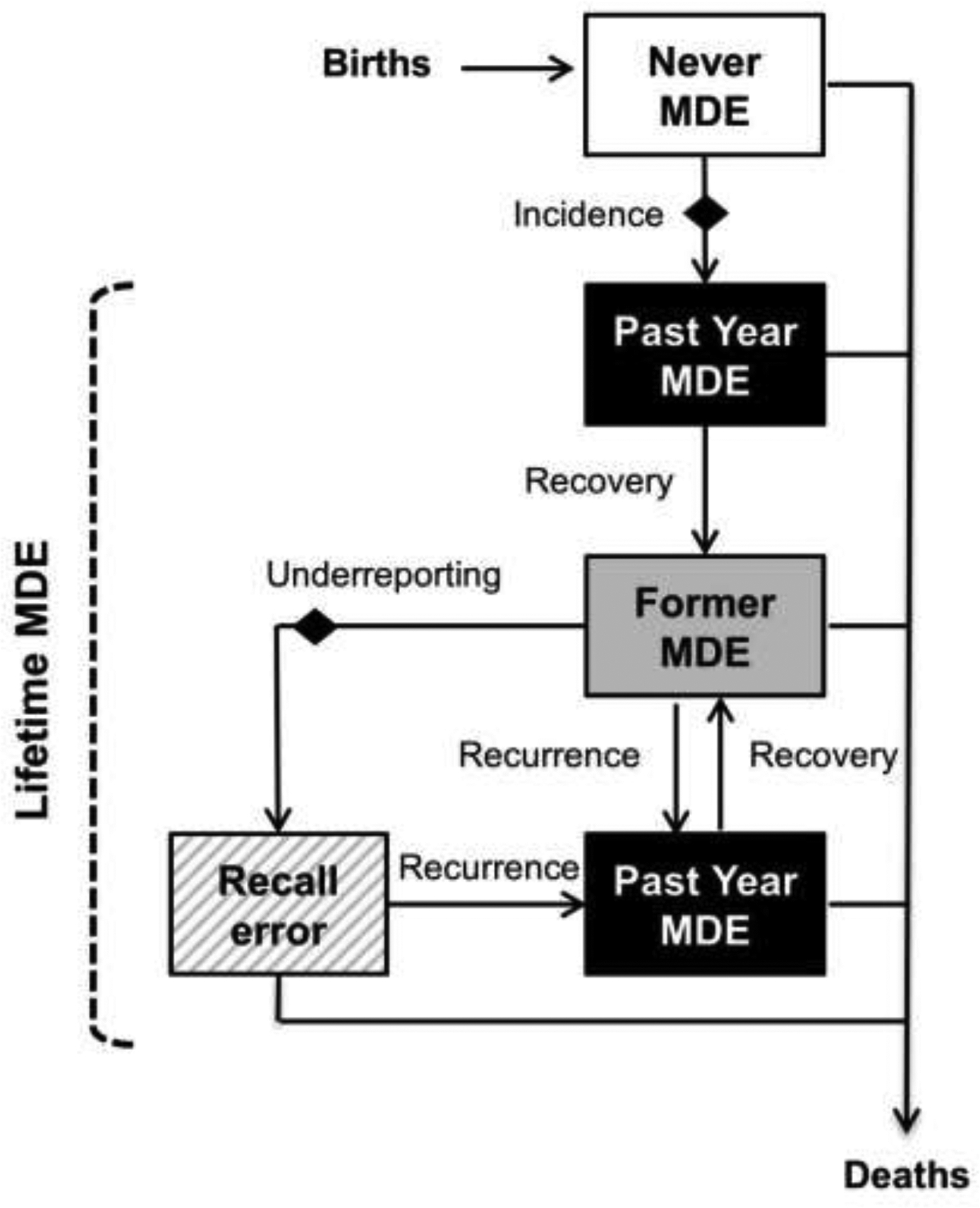
Model diagram of depressive states and transitions.
MDE, major depressive episode; Diamond, annual probabilities estimated during model calibration; Never MDE, individuals with no lifetime history of MDEs; Past year MDE, individuals with a past year MDE; Former MDE, individuals with lifetime history of at least one MDE but no MDEs in the past; Recall error, individuals who report no lifetime history of MDEs but are modeled as former MDE.
The model simulates all individuals in the never MDE state at age 0 years based on U.S. Census Bureau estimates for 2005–2017.17 As individuals age, they may have a first MDE according to age-specific MDD incidence rates from the ECA study.18 The ECA study found bimodal MDD incidence distributions; incidence peaked around age 30 years, with a smaller peak around age 45 years for females, and similar peaks at ages 40 and 55 for males.18 As the ECA study did not include incidence rates for females aged <22 years and males aged <29 years, this model estimated probabilities of a first MDE for age 12–21 years in females and 12–28 years in males during calibration.
Following a first MDE, individuals can recover into the former MDE state. Annual recovery probabilities are treated as identical for males and females, and as constant across all ages. Recovery and recurrence transition probabilities were calculated based on data from the ECA study.14 Likelihood of recovering from an episode is the same regardless of whether individuals are in a first or subsequent episode, based on evidence showing no significant difference in rates of recovery by number of prior episodes.19
As those with past year MDE are included in lifetime prevalence estimates, under-reporting was only estimated among the former MDE group. Former MDE individuals can shift into the “recall error” state based on calibrated estimates for the annual probability of under-reporting past episodes. This study assumed no inaccuracies due to over-reporting of MDEs, as mental illnesses are significantly under-reported compared with other conditions.20,21 Like the former MDE group, the recall error group can have a recurrent MDE.
Finally, individuals across all states exit the model based on age, birth cohort, and year-specific death probabilities. The model applied an elevated risk of death to all ages among those with MDE histories.22 All surviving individuals exit the model by death at age 99 years. Female and male individuals were modeled separately.23 Analysis was conducted in R, version 3.1.3 from 2016 to 2019.24
Analysis
The model is calibrated to reproduce NSDUH depression patterns by age and sex, fitting individuals in the “recall error” state as part of the never MDE population. Cubic natural splines were used to estimate age-specific probabilities of a first MDE for females aged 12–21 years and males aged 12–28 years. No MDEs occur prior to age 12 years, because data suggest that only 0.50%–0.75% of children show signs of depression by age 11 years.25 Finally, under-reporting was estimated for each of five age groups to align with NSDUH data. Because NSDUH top-codes all ages >65 years, the same probabilities were estimated for the entire age 65–99 years category. The model assumes zero probability of past MDE under-reporting for ages <18 years.
The impact of three parameters, recovery, recurrence, and relative risk of mortality among people with a history of MDE, were assessed on two main outcomes: (1) the proportion of the adult population that fails to recall past histories of MDEs and (2) lifetime MDE prevalence. These parameters are assessed using Latin hypercube sampling.26,27 Ranges representing 95% of values generated from this approach are reported (Appendix).
RESULTS
Probabilities of first lifetime MDE are shown (Figure 2). Calibrated estimates show higher risk of a first episode at younger ages with peaks at age 18 years among females (0.047) and at age 16 years among males (0.014). Among youth and young adults, extrapolated probabilities of MDE onset were substantially lower for males than for females.
Figure 2.
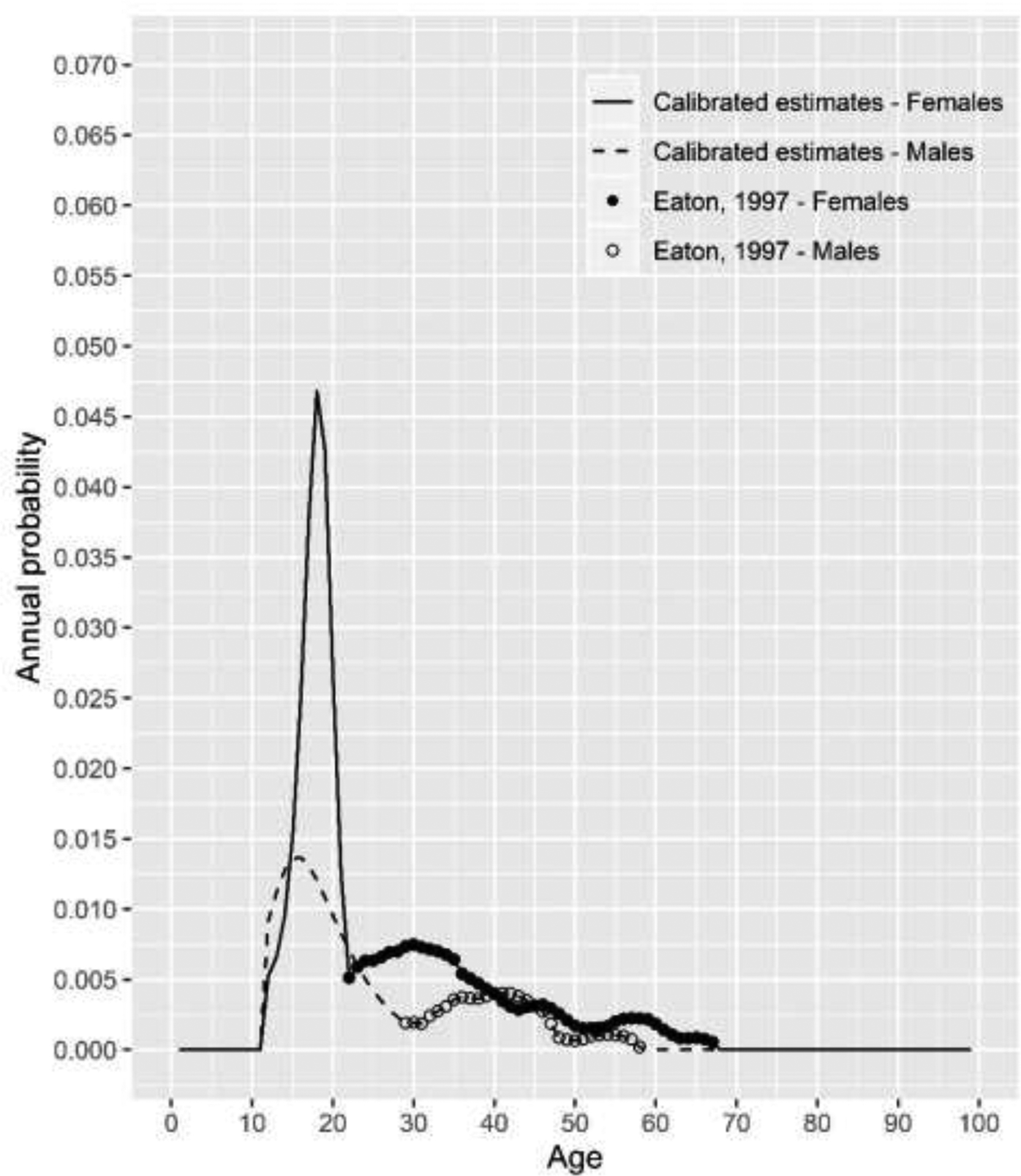
Annual probability of first major depressive episode.
Notes: Solid line = Females ages 12–21 years calibrated model estimates; Dashed line = Males ages 12–28 years calibrated model estimates; Black dots = incidence probabilities for female age at onset of major depressive disorder (MDD) in the Baltimore Epidemiological Catchment Area (ECA) Study; Circles = incidence probabilities for male age at onset of MDD in the Baltimore ECA Study.
The calibrated model estimated zero probability of under-reporting past MDEs for both males and females aged 18–25 years (Figure 3). The estimated proportion of former MDE individuals who did not report their past episodes was higher for females (15.2%) than for males (10.5%) for those aged 26–34 years and similar for ages 35–49 years (10.1% vs 8.8%) and 50–64 years (12.0% vs 12.7%). Probabilities of under-reporting were dramatically higher for those aged ≥65 years, with 92.3% and 71.9% of former MDE females and males not reporting their histories of MDEs according to the model.
Figure 3.
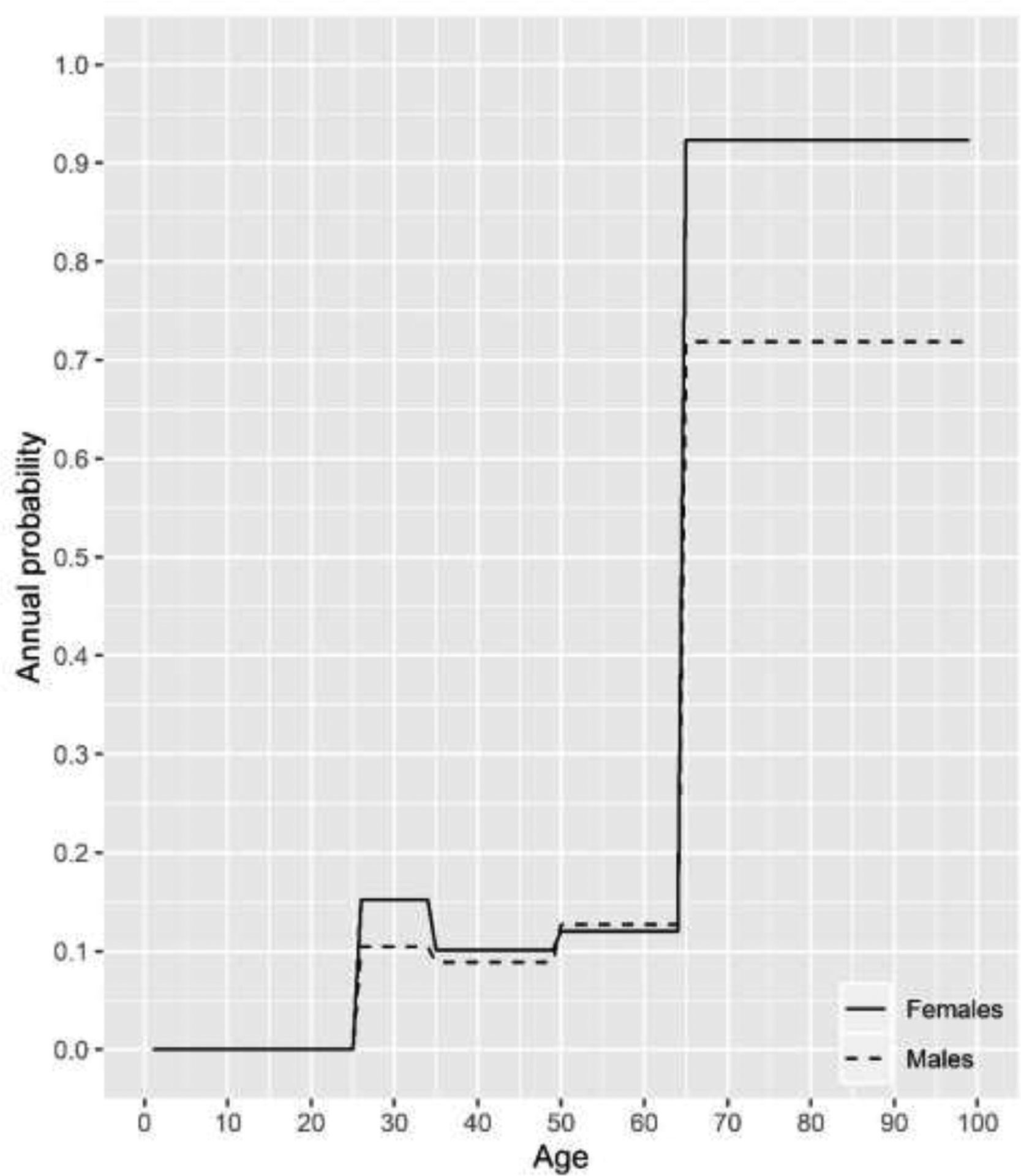
Past major depressive episode under-reporting probabilities by age.
Notes: Solid line = Females; Dashed line = Males; model estimates calibrated for age groups 18–25, 26–34, 35–49, 50–64, and ≥65 years. Annual probabilities for individuals age <18 years fixed at zero.
Figure 4 shows estimated lifetime MDE prevalence by age group and sex in 2017. Past-year MDE prevalence ranged from 8%–10% of females and 4%–6% of males aged >25 years, and was 16.5% and 9.8% for female and male young adults aged 18–25 years. The recall-corrected model estimated that 30.1% of females and 17.4% of males had a lifetime history of MDEs. The proportion of the population with a lifetime history of MDEs increased with age until peaking in those aged 50–64 years, where 33.2% of females and 19.4% of males had a history of a MDE in their lifetimes, then decreased for those aged ≥65 years to 31.2% and 16.9%, respectively. Thereafter, the oldest age group (≥65 years) shows slightly lower lifetime MDE prevalence compared with younger adults, due to differential mortality. During sensitivity analysis, 95% of estimates for lifetime MDE prevalence fell between 29.0% and 32.5% among females and between 16.7% and 18.8% among males (Appendix Figure 3).
Figure 4.
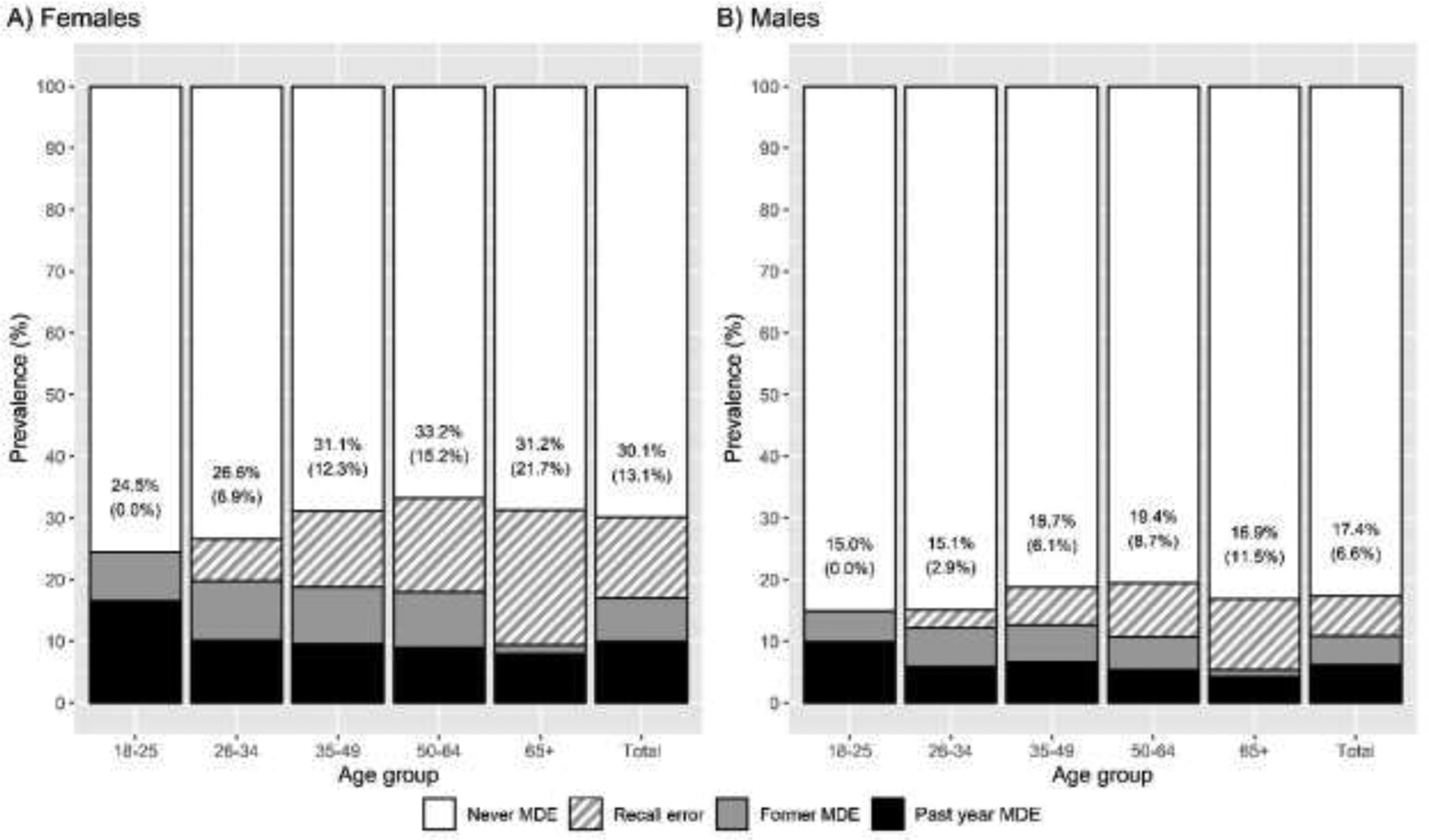
Adult lifetime MDE prevalence by age group with recall error adjustment, 2017.
Notes: Distribution of the adult population with past year MDE (black), former MDE (gray), former MDE with recall error (diagonal hatching pattern), and never MDE (white). Numbers represent the percent of individuals with lifetime MDE histories. Numbers in parentheses represent the percent of individuals with recall error who fail to report lifetime MDEs.
MDE, major depressive episode.
The model estimated 13.1% of women and 6.6% of men failed to report their MDE histories. Individuals who failed to report their past MDEs represented an increasing share of those with MDE histories with each successive age category; this proportion is lowest for age 26–34 years when 6.9% of females and 2.9% of males make up this group, and highest for ages ≥65 years at 21.7% of females and 11.5% of males. People who failed to report their past episodes made up more than two thirds of those with MDE histories at age ≥65 years. Sensitivity analysis showed that 95% of values for the proportion of adults that under-report a past episode ranged from 8.1% to 16.5% for females and 4.0% to 8.3% for males (Appendix Figure 3).
DISCUSSION
This simulation model quantifies the impact of recall error on lifetime MDE prevalence in the U.S. This study finds that 23.9% of adults have histories of MDEs, which is considerably higher than estimates that do not adjust for under-reporting; more than 40% of adults with MDE histories failed to report them in cross-sectional surveys. The findings corroborate simulation studies from other countries that show lifetime prevalence of depression is dramatically higher than indicated by retrospective analyses.12,28 The recall-corrected estimates also show the expected pattern of increasing lifetime prevalence with age, with a minor decrease in the oldest age group that can attributed to differential mortality.
Strengths of the model include its structural simplicity, its remarkably close fit with survey data, and its integration of epidemiological information. This simple yet comprehensive simulation model derives parameters for MDE onset, recovery, and recurrence from the nation’s longest-running psychiatric epidemiologic prospective cohort study.29 Sensitivity analysis suggests that even with considerable uncertainty surrounding adults under-reporting past episodes, lifetime MDE prevalence estimates fall within narrow ranges.
The probability of having a first MDE is much higher during adolescence than adulthood. By extrapolating probabilities to younger ages, while anchoring the MDE prevalence in the model to observed values for adults aged 18 years or older, the model estimates plausible incidence data that could not otherwise be obtained through survey data. Youth and adult measures for depression are not directly comparable, nor are they generally used within the same surveys.8
These incidence estimates are consistent with other studies that show depressive symptoms increase during adolescence, and that sex differences in depression onset widen throughout this life stage.25
Limitations
Alternative concepts might explain lower lifetime MDE prevalence among adults aged 65 years and older besides recall error. Older adults may interpret prior depressive symptoms more positively.30 Older adults are less likely to endorse depressive symptoms, and their symptoms are more likely to be categorized as “minor” depression.31 Their high levels of under-reporting are driven in part by the fact that a greater proportion of their past MDEs might have occurred in the more distant past. Finally, differential mortality reduces prevalence at older ages; even a modest hazard ratio has a larger impact on elderly individuals than younger age groups. However, differential mortality does not explain unchanging patterns of lifetime MDE prevalence during ages 25–64 years when recall error still occurs.
The lifetime MDE prevalence estimates shown here may not reflect expected prevalence in the future due to potential cohort effects as well as population aging. Recent NSDUH data suggest that MDE incidence may be rising over time among young adults (Appendix).32 Earlier birth cohorts may have lower rates of depression compared to recent birth cohorts. More recent cohorts may also have greater mental health awareness, making them more likely to report symptoms. This highlights the need for additional research on cohort patterns of MDEs to better understand changes over time. Models can be extended to consider variations in risk by cohort and explore the impact of such variations on morbidity and mortality. Finally, because the U.S. population is aging and recall error increases with age, this will further underestimate the true burden of MDEs.
The parameters used in this study come from literature on MDD, but some MDEs also occur among those with bipolar disorder and persistent depressive disorder. The calibrated incidence probabilities are also higher than those reported for MDD in part because some MDEs are excluded by MDD criteria. Although it is not possible to disaggregate MDEs by type of disorder in the NSDUH, as MDD is nearly ten times more common than bipolar disorder, such episodes overwhelmingly are represented by people with this condition. Recurrence rates may differ between those with and without recall error, but without published evidence on this topic to parameterize them differently, the model treats them as equal.
Because public-use NSDUH data do not disaggregate their oldest age group, under-reporting parameters were estimated for all individuals in this group. In the absence of reliable age-specific depression mortality rates, a single relative risk of mortality point estimate for all individuals with MDE histories was applied.
The incidence, recovery, and recurrence rates were derived them from a cohort study conducted in East Baltimore that may not be representative of the U.S. population.29 This simple compartmental model does not track individual trajectories of episodes because it simulates aggregate-level patterns. Recovery and recurrence rates do not depend on number, duration, or time since prior episode; they are net population rates that do not vary by age, as U.S. age-specific data on recovery or recurrence from MDEs are not available. Sensitivity analyses revealed that varying these parameters did not change inferences drawn from the model: Recall error leads to severe underestimation of lifetime MDE prevalence based on survey data.
CONCLUSIONS
This study demonstrates the application of a novel methodology to address mismeasurement of health histories that can advance population health research. Few simulation models have been implemented for mental health system planning, and fewer still for depression.33 Computational models can guide the design of such systems, but unless the scope of the underlying health problem is measured accurately, the population health impact of prevention interventions will also be misestimated. Modeling methods can reconcile implausible information with other epidemiological data to better characterize the needs of patient populations. These findings show that preventing MDEs would benefit a much larger segment of the population—and that far more episodes occur at younger ages—than what surveys indicate. The sex- and age-specific estimates of MDE incidence produced by the model can facilitate research on strategies that aim to prevent MDE onset across the life course, especially during adolescence and young adulthood.
Interested researchers can explore this model at github.com/jamietam/dep-model-AJPM/. Users can: (1) download calibrated MDE incidence rates, (2) simulate the impact of MDE prevention strategies, (3) reconcile irregular or misreported health data with other data sources through calibration, or (4) simulate other health conditions that are often subject to under-reporting.
By correcting for under-reporting in the general U.S. population, the full impact of mental health promotion efforts can be measured. Accurate lifetime MDE prevalence estimates account for those who may still be experiencing subclinical or residual effects associated with their past episode that impair functioning.34 Assessments of lifetime prevalence for chronic physical conditions, such as heart disease, identify individuals at risk for additional events (myocardial infarction) for whom maintenance treatment and clinical monitoring are important. Individuals with a history of MDEs have increased risk for a recurrent episode, but without correcting for under-reporting, surveys would fail to identify individuals who might benefit from mental health programs. Under-reporting is also a source of discrepancy in comparisons of self-reported depressive symptoms and clinical diagnoses.21 However, relying on reports of clinical diagnosis would still substantially underestimate the burden of depression because approximately 37% of adults with MDEs do not receive any treatment for them.35
Planning for the healthcare needs of complex populations such as those with MDEs requires models that are sufficiently detailed yet simple and flexible enough to implement. Although this analysis focuses on lifetime prevalence, the model estimates past-year MDE prevalence as well and can be used for other studies; it is already being applied to study intervention strategies for a special subpopulation—smokers with comorbid major depression.36 Substance use disorders, which often co-occur with MDEs, are difficult to measure and would benefit from the application of methods such as those presented here. When existing health data are irregular or insufficient, modeling methods can address such gaps and more accurately represent population health impact.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the National Institute of Drug Abuse of the NIH under award number F31DA041083 during which time JT was at the University of Michigan. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
JT directed this study, conceived of and developed the model, and wrote the first draft of the manuscript. BM, KZ, and RM contributed substantively to the model conceptualization and to drafts and revisions of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 3.Center for Behavioral Health Statistics, Quality Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health (NSDUH). Rockville, MD: Center for Behavioral Health Statistics; 2017. [Google Scholar]
- 4.Patten SB, Williams JV, Lavorato DH, Bulloch AG, D’Arcy C, Streiner DL. Recall of recent and more remote depressive episodes in a prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2012;47(5):691–696. 10.1007/s00127-011-0385-5. [DOI] [PubMed] [Google Scholar]
- 5.Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, Mojtabai R. Accuracy of reports of lifetime mental and physical disorders: results from the Baltimore Epidemiological Catchment Area study. JAMA Psychiatry. 2014;71(3):273–280. 10.1001/jamapsychiatry.2013.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Patricia B, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 8.Mezuk B, Eaton WW. Approaches to measuring multi-dimensional constructs across the life course: operationalizing depression over the lifespan In: Walford G, Tucker E, Viswanathan M, eds. The SAGE Handbook of Measurement. London, UK: SAGE, Inc; 2010:239–264. 10.4135/9781446268230.n13. [DOI] [Google Scholar]
- 9.Hassan E Recall bias can be a threat to retrospective and prospective research designs. Internet Journal of Epidemiology. 2005;3(2):1–7. https://print.ispub.com/api/0/ispub-article/13060. Accessed April 3, 2020. [Google Scholar]
- 10.Homer JB, Hirsch GB. System dynamics modeling for public health: background and opportunities. Am J Public Health. 2006;96(3):453–458. 10.2105/ajph.2005.062059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galea S, Riddle M, Kaplan GA. Causal thinking and complex system approaches in epidemiology. Int J Epidemiol. 2010;39(1):97–106. 10.1093/ije/dyp296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kruijshaar ME, Barendregt J, Vos T, de Graaf R, Spijker J, Andrews G. Lifetime prevalence estimates of major depression: an indirect estimation method and a quantification of recall bias. Eur J Epidemiol. 2005;20(1):103–111. 10.1007/s10654-004-1009-0. [DOI] [PubMed] [Google Scholar]
- 13.Patten SB, Gordon-Brown L, Meadows G. Simulation studies of age-specific lifetime major depression prevalence. BMC Psychiatry. 2010;10:85 10.1186/1471-244x-10-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eaton WW, Shao H, Nestadt G, Lee BH, Bienvenu OJ, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry. 2008;65(5):513–520. 10.1001/archpsyc.65.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Breslau J, Gilman SE, Stein BD, Ruder T, Gmelin T, Miller E. Sex differences in recent first-onset depression in an epidemiological sample of adolescents. Transl Psychiatry. 2017;7(5):e1139 10.1038/tp.2017.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration. 2017. National Survey on Drug Use and Health - Public Use File Codebook. Rockville, MD: Substance Abuse and Mental Health Services Administration; October 23, 2018. [Google Scholar]
- 17.U.S. Census Bureau. 2014. National Population Projections Datasets. www.census.gov/data/datasets/2014/demo/popproj/2014-popproj.html. Published 2014. Accessed October 15, 2016.
- 18.Eaton WW, Anthony JC, Gallo J, et al. Natural history of diagnostic interview schedule / DSM-IV major depression: the Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry. 1997;54(11):993–999. 10.1001/archpsyc.1997.01830230023003. [DOI] [PubMed] [Google Scholar]
- 19.Solomon DA, Keller MB, Leon AC, et al. Recovery from major depression: a 10-year prospective follow-up across multiple episodes. Arch Gen Psychiatry. 1997;54(11):1001–1006. 10.1001/archpsyc.1997.01830230033005. [DOI] [PubMed] [Google Scholar]
- 20.Bharadwaj P, Pai MM, Suziedelyte A. Mental health stigma. Econ Lett. 2017;159:57–60. 10.1016/j.econlet.2017.06.028. [DOI] [Google Scholar]
- 21.Eaton WW, Neufeld K, Chen L-S, Cai G. A comparison of self-report and clinical diagnostic interviews for depression: diagnostic interview schedule and schedules for clinical assessment in neuropsychiatry in the Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry. 2000;57(3):217–222. 10.1001/archpsyc.57.3.217. [DOI] [PubMed] [Google Scholar]
- 22.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the Global Burden of Disease Study 2010. PLoS Med. 2013;10(11):e1001547 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. [Google Scholar]
- 25.National Collaborating Centre for Mental Health. National Institute for Health and Clinical Excellence: Guidance Depression in Children and Young People: Identification and Management in Primary, Community and Secondary Care. Leicester, UK: The British Psychological Society, The Royal College of Psychiatrists; 2005. [PubMed] [Google Scholar]
- 26.McKay MD, Beckman RJ, Conover WJ. A comparison of three methods for selecting values of input variables in the analysis of output from a computer code. Technometrics. 1979;21(2):239–245. 10.1080/00401706.1979.10489755. [DOI] [Google Scholar]
- 27.Chalom A, de Prado PIKL. pse: Parameter Space Exploration with Latin Hypercubes. R package version 0.4.5. http://CRAN.R-project.org/package=pse. Published 2016.
- 28.Moffitt TE, Caspi A, Taylor A, et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40(6):899–909. 10.1017/s0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eaton WW, Kalaydjian A, Scharfstein DO, Mezuk B, Ding Y. Prevalence and incidence of depressive disorder: the Baltimore ECA follow-up, 1981–2004. Acta Psychiatr Scand. 2007;116(3):182–188. 10.1111/j.1600-0447.2007.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carstensen LL, Turan B, Scheibe S, et al. Emotional experience improves with age: evidence based on over 10 years of experience sampling. Psychol Aging. 2011;26(1):21–33. 10.1037/a0021285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Penninx BH, Geerlings SW, Deeg DH, van Eijk JM, van Tilburg W, Beekman AF. Minor and major depression and the risk of death in older persons. Arch Gen Psychiatry. 1999;56(10):889–895. 10.1001/archpsyc.56.10.889. [DOI] [PubMed] [Google Scholar]
- 32.Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Abnorm Psychol. 2019;128(3):185–199. 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- 33.Long KM, Meadows GN. Simulation modelling in mental health: a systematic review. J Simul. 2018;12(1):76–85. 10.1057/s41273-017-0062-0. [DOI] [Google Scholar]
- 34.Kelly KM, Mezuk B. Predictors of remission from generalized anxiety disorder and major depressive disorder. J Affect Disord. 2017;208:467–474. 10.1016/j.jad.2016.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Institute of Mental Health. Major Depression. www.nimh.nih.gov/health/statistics/major-depression.shtml. Published 2017. Accessed May 7, 2018.
- 36.Tam J. Smoking and Mental Illness Co-morbidity: Implications for Mortality Outcomes and Treatment Interventions [Doctoral Dissertation]. Ann Arbor, MI: Health Services Organization and Policy, University of Michigan; 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


