Abstract
Introduction:
Latino men experience disproportionately high rates of diseases related to low physical activity, yet are poorly represented in physical activity intervention trials. Efforts to promote physical activity in Latina women show promising results, yet such interventions have yet to be extended to Latino men. This study tested a computer expert system-tailored, text messaging–supported physical activity intervention for underactive Spanish-speaking Latino men compared with a control group matched for contact time. Potential predictors of intervention success were also explored.
Study design:
Randomized trial. Participants were randomized to receive a Tailored Physical Activity Intervention (Intervention) or a Wellness Control Group (Control). Data were collected in 2015–2017 and analyzed 2018–2019.
Setting/participants:
Insufficiently active Latino men (N=46).
Intervention:
Intervention participants received a baseline counseling session, then received individually tailored print materials and text messages on a tapered schedule for 6 months. Controls received printed wellness materials and text messages on the same schedule.
Main outcome measures:
Primary outcome was change in weekly moderate-to-vigorous physical activity from baseline to 6 months measured by accelerometers. Self-reported moderate-to-vigorous physical activity measured by the 7-Day Physical Activity Recall Interview was a secondary outcome.
Results:
For Intervention participants, median accelerometer-measured moderate-to-vigorous physical activity increased from 10.0 minutes/week at baseline to 57.5 minutes/week at 6 months, while Control participants increased from 21.0 minutes/week at baseline to 23.0 minutes/week at 6 months (p<0.05). Similar results were found for self-reported moderate-to-vigorous physical activity. At 6 months, 47% of Intervention participants met national guidelines of 150 minutes/week versus 25% of Controls (p=0.15, not significant).
Conclusions:
Findings suggest that an individually tailored intervention can successfully increase moderate-to-vigorous physical activity in underactive Latino men. Such technology-supported interventions have potential for broad dissemination.
Trial registration:
This study is registered at www.clinicaltrials.gov NCT02512419.
INTRODUCTION
Latinos experience marked disparities in numerous conditions related to inactivity, including type 2 diabetes and obesity.1,2 Concordantly, interventions to increase physical activity (PA) have increasingly been designed and tested with Latinos in recent years. Some of these have shown significant increases in PA among Latina women,3,4 suggesting that interventions could change PA behaviors shown protect against diabetes, obesity, and other lifestyle-related conditions in this high-risk population. Latino men, however, have largely been absent from PA interventions. In a recent systematic review examining interventions to promote PA among diverse men, only one published study provided data for Latino men and there were no studies for which Latino men were exclusively the population of interest.5
This is not due to a lack of need, as Latino men also report markedly high rates of inactivity6-8 and related diseases. Compared with 26% of non-Latino white men, 40% of Latino men report never engaging in any leisure time PA9 and fewer Latinos meet PA guidelines (15.4% vs 22% for non-Latino whites).10 This disparity is not purely socioeconomic: Latino men are less physically active at every level of income, education, and employment status,9 and across U.S. regions.11 Diabetes prevalence in Latino men is approximately 50% higher than in non-Latino white men,12 and it is estimated that nearly 80% of Latino men are overweight or obese, the highest of any major demographic group.13
Although the majority of Latino men endorse the health benefits of PA,14 they have cited lack of programs in Spanish and work-related time constraints as barriers to participating in PA intervention programs.15,16 Additionally, many PA interventions for Latinos may not have appealed to Latino men as they featured walking groups, aerobic dance, and other activities that may be more appealing to Latina women.16,17 Limited formative research with Latino men suggests they may be interested in participating in PA interventions that are tailored to them.15 To prevent disease and reduce disparities among Latino men, effective, gender- and linguistically-appropriate interventions are needed to increase PA in this high-risk, underserved population.
Efficacy of a print-based Spanish language intervention to increase PA was recently shown in Latina women.18 To address the large gap in behavioral interventions for Latino men, the previous intervention was modified and tested in a small one-arm pilot trial. After 12 weeks, participants significantly increased objectively measured and self-reported PA, and retention and participant satisfaction were high.17 In follow-up interviews, intervention participants recommended program improvements including greater accountability, more contact with staff and other participants, shorter and more frequent tips, and more updates on PA opportunities.
Adopting technologies such as text messaging could be a low-cost way to improve real-time accountability and communication, and may be particularly appropriate for this population. Cell phone ownership is nearly universal in Latino adults (97%),19 and Latinos are more likely than non-Latino whites to use mobile phones for text messaging (85% vs 79%, respectively).20 Text messaging can be an effective tool for changing behaviors such as PA21; however, it is more likely to be effective when combined with more intensive educational components.22 Combining text messaging with the theory-driven, print-based intervention could therefore be an appropriate approach to increasing PA in Latino men.
The aim of the current study was to explore the potential efficacy of a multi-channel (print and text-based), theory-based, individually tailored Spanish language intervention to increase PA in Latino men through a pilot RCT. The hypothesis was that those randomly selected to receive the intervention would show significantly greater increases in objectively measured PA than those in the contact-matched control group. Changes in self-reported PA and predictors of intervention efficacy were also explored.
METHODS
The Activo study was an RCT of a 6-month mail- and text-delivered individually tailored Spanish language PA intervention, compared with a Spanish-language wellness contact control condition. The primary outcome of interest was minutes/week of moderate-to-vigorous PA (MVPA) measured by accelerometers. Self-reported MVPA was a secondary outcome. Data were collected in 2015–2017, and analyzed in 2018–2019.
Study Population
Inclusion criteria included: self-identified as male, self-identified as Hispanic or Latino, self-reported insufficient MVPA (defined as participating in MVPA <90 minutes/week), age 18–65 years, ability to receive weekly PA-related text messages sent by the study, and willingness to be randomly assigned to either of the two study conditions.
Exclusion criteria included: unable to read or speak Spanish fluently, any medical conditions that would make unsupervised exercise unsafe as determined by the PA Readiness Questionnaire,23 verified BMI ≤45 kg/m2, hospitalization due to a psychiatric disorder in the past 3 years, and taking medication that may impair MVPA tolerance or performance (e.g., beta blockers).
Men were recruited during an 18-month period through health fairs, community organizations, and staff organizations at the university, and through media outlets including newspapers, Craigslist, Facebook, and flyers. Recruitment initially focused on the San Diego area; however, recruitment within San Diego was slower than anticipated, and a number of individuals outside the area expressed interest in the study. As broad dissemination is the ultimate goal of technology-mediated interventions, recruitment was eventually expanded to include participants outside the local geographic area to explore the potential of delivering the trial remotely through mediated channels.
Eligible men in the San Diego area attended an in-person orientation session. Interested individuals signed an informed consent document approved by the UC San Diego IRB. During this visit, participants filled out baseline questionnaires (described in Measures section), and height and weight were measured. Participants were also given an accelerometer, with instructions to wear it for 7 days.
Participants living outside the San Diego area (remote participants) completed the orientation session via telephone, then returned the informed consent forms through the mail. Participants were then sent baseline questionnaires and an accelerometer with detailed instructions to wear it for 7 days, then return it in a postage paid envelope. Anthropometric measures were not conducted among these participants.
After wearing the accelerometer for 7 days, local participants (n=31) returned to the study site and completed the 7-day PA Recall (7-day PAR) interview. After completing all baseline assessments, they were randomized to one of two study arms: (1) Tailored PA Intervention or (2) Wellness Control. Group assignment was determined using a block-permuted randomization procedure designed by the study statistician that was stratified by participants’ Transtheoretical Model Stage of Change, or level of motivational readiness, for PA. Remote participants (n=17) completed the 7-Day PAR over the phone after mailing back baseline questionnaires and accelerometers. Using the same block-permuted randomization procedure, remote participants were randomized over the phone to Tailored PA Intervention (n=7) or Wellness Control (n=10).
The PA intervention was based on the Social Cognitive Theory and Transtheoretical Model and emphasized behavioral strategies for increasing PA (e.g., goal setting, self-monitoring, problem-solving barriers, increasing social support). The intervention was adapted by bilingual (English/Spanish) and bicultural (Mexican American and Puerto Rican) study staff for Latino men from the team’s existing PA interventions for Latina women through a formative research process. First, interviews were conducted with underactive Spanish-speaking Latino men (n=10) on their PA needs and preferences. Based on these findings, the intervention was adapted and piloted in a 12-week single-arm demonstration trial with Latino men (n=10)17 followed by qualitative follow-up interviews. To confirm themes from these interviews, interviews (n=16) were conducted with a new sample of Spanish-speaking Latino men including questions about their use of cell phones and text messaging. Themes included a desire for more accountability, more information on including family members and children in PA, more information on environmental resources, and an intervention that would accommodate their busy work schedules and odd hours. Findings from the formative research process were used to inform the development of text messages and integration of themes into text and print intervention materials.
The baseline session was conducted by a PhD-level interventionist trained in motivational interviewing techniques. Participants set short-term goals, anticipated and problem solved potential barriers and were encouraged to gradually increase their activity to 150 minutes/week. Participants were given a pedometer and asked to track their number of steps, as previous studies show this can increase PA.24 Participants also received recommendations for walking/jogging routes, gyms, parks, and other places to be active near their work or home. Remote participants received all information in the mail prior to their scheduled phone call and completed goal setting via telephone.
Throughout the 6-month intervention, participants received tailored PA information in the mail weekly during Month 1, biweekly in Months 2 and 3, and monthly during Months 4–6. These mailings consisted of: (1) manuals matched to the participant’s current level of motivational readiness to change, based on the Transtheoretical Model; (2) individually tailored computerized expert system feedback reports based on the participant’s answers to monthly questionnaires (described in Measures section) that compared participants with their prior responses and with individuals who are physically active on self-efficacy for PA and cognitive and behavioral strategies associated with PA behavior change (processes of change); and (3) PA tip sheets addressing barriers to being active (such as work and family obligations). Participants also received two text messages weekly throughout the intervention: The first provided a useful/motivational tip, and the second prompted the participant to report their minutes of MVPA the previous week.
Participants in the intervention arm received regularly scheduled phone calls from a Spanish-speaking Latino interventionists during the initial 3 months of the study: after 1 week (to ensure proper pedometer use and receipt of text messages), after 1 month (20 to 30–minute call to review progress and set new goals), and after 2 and 3 months (addressing text messaging engagement).
Participants in the Wellness Control Group received publicly available Spanish-language print materials from the National Heart Lung and Blood Institute on promotion of heart-healthy behaviors for Latinos via mail and SMS text messaging. Print-based materials included booklets on health topics other than PA (e.g., cholesterol) and health tip sheets (e.g., insomnia, stress management, and nutrition) mailed to participants on the same schedule as the PA intervention arm. Participants also received two text messages weekly throughout the study containing health and wellness tips unrelated to PA, and received phone calls on the same schedule verifying receipt of text messages and answering any questions.
Measures
Questionnaires were administered at baseline to measure demographic information, acculturation (Brief Acculturation Scale), and adult health literacy (Short Test of Functional Health Literacy in Adults).25
MVPA at baseline and 6 months was measured by accelerometer (ActiGraph 3X+). Accelerometers measure movement and intensity of PA and have been validated with heart rate telemetry26 and total energy expenditure.27 Participants wore the accelerometer on their left hip for 7 days. Consistent with previous studies, valid wear time was classified as 5 days of ≥600 minutes of wear time each day or ≥3,000 minutes of wear time over 4 days.28 Accelerometer data were processed using the ActiLife software using a cut point of 1,952 and ≥10 minutes/bout to establish the minimum threshold for MVPA.
Activity was also measured via self-report using the 7-Day PAR interview.29-34 The 7-Day PAR is an interviewer-administered instrument that provides an estimate of weekly minutes and intensity of PA. Strategies for increasing accuracy of recall are incorporated, and all domains of PA (e.g., leisure, transportation, and occupational) are evaluated. To help participants distinguish between PA intensities in their recollection of PA, San Diego–based participants walked on a treadmill for 10 minutes at a moderate intensity pace (approximately 3–4 miles per hour, determined by rating of perceived exertion) immediately before completing the 7-Day PAR at baseline and again at follow-up. Owing to logistical limitations, this was not done for the remote participants. The 7-Day PAR has been widely used and consistently demonstrated acceptable reliability, internal consistency, and concurrent validity with objective measures of activity.29-33 The 7-Day PAR is valid to deliver by phone, sensitive to changes in MVPA over time,30,31 and has good test–retest reliability among Latino participants.34 To avoid bias, study staff conducting the 7-Day PAR, and all other measures, were blinded to study condition.
Three measures specific to PA behavior change were administered at baseline and then on a monthly basis throughout the study to help generate the tailored expert system feedback reports for the PA intervention group participants. These included the 4-item Stages of Change measure, the 40-item Processes of Change measure, and PA self-efficacy. Each of these have shown good reliability and validity.35-37
Statistical Analysis
As a preliminary step, between-group differences in baseline variables, including sociodemographics, acculturation, and baseline minutes/week of MVPA were examined using t-tests (for continuous variables), chi-square tests (for categorical variables), and non-parametric tests as appropriate. Using correlation analysis, potential confounders were identified (e.g., demographic characteristics). A variable was considered a confounder if it was correlated with both the outcome and predictor (group assignment) at a modest p<0.10 level. Confounders were included as covariates in subsequent models.
Unadjusted weekly minutes of MVPA at baseline and follow-up were presented by arm for both subjectively reported MVPA and objectively measured outcomes. As MVPA data were skewed and attempts to transform toward normality were unsuccessful (e.g., skewness still significant), medians and interquartile ranges are presented as measures of central tendency and spread. Finally, Spearman rank correlations were used to examine associations between self-reported and objectively measured minutes/week of MVPA at baseline and follow-up. Spearman correlations are less subject to potential outlying values. Assuming moderate effect sizes, N=60 was determined adequate to detect significant between-group differences.
To examine potential intervention effects on the primary outcome (weekly minutes of MVPA at 6 months), a series of quantile regression models were used, which estimate effects on median outcomes (as opposed to mean outcomes), and are thus ideal in pilot studies where the outcomes are subject to a high degree of variability and skewness. Models regressed outcome at 6 months (self-reported and objectively measured minutes/week of MVPA in separate models) on treatment assigned, baseline value of the outcome, as well as confounders identified a priori. Models of objectively measured MVPA additionally controlled for ActiGraph wear time. Model estimates were based on a likelihood/quasi-likelihood approach to estimation and thus made use of all available data without directly imputing missing outcomes.
As a subsequent step, the proportion of participants who reported meeting national guidelines for MVPA38 (defined as ≥150 minutes/week of MVPA measured by the 7-Day PAR) was examined. Both unadjusted and adjusted differences between groups were examined (using chi-square analyses for the former and logistic regression for the latter).
Using a series of quantile regression models, potential baseline predictors of success were explored, including sociodemographic variables and nativity among those randomized to the intervention condition. Interest was in exploring predictors of PA adoption for those receiving the intervention condition. Correlation analysis was used as a preliminary step to reduce the risk of multicollinearity (namely, no two variables with correlations >0.75 were included in the multivariate model. Should this case arise, the decision was made to include the stronger correlate of study outcome). The goal was to identify potential characteristics of participants who reported greater minutes/week of MVPA at end of treatment controlling for baseline. Given the limitations of sample size, this was exploratory and estimates of effect (with CIs) were of interest (as opposed to statistical hypothesis testing).
All analyses were carried out in Stata/SE, version 15.1 and α set a priori at 0.05. Analyses were conducted on the intention-to-treat sample. Estimates were based on likelihood approaches and thus made use of all available data without directly imputing missing outcomes.
RESULTS
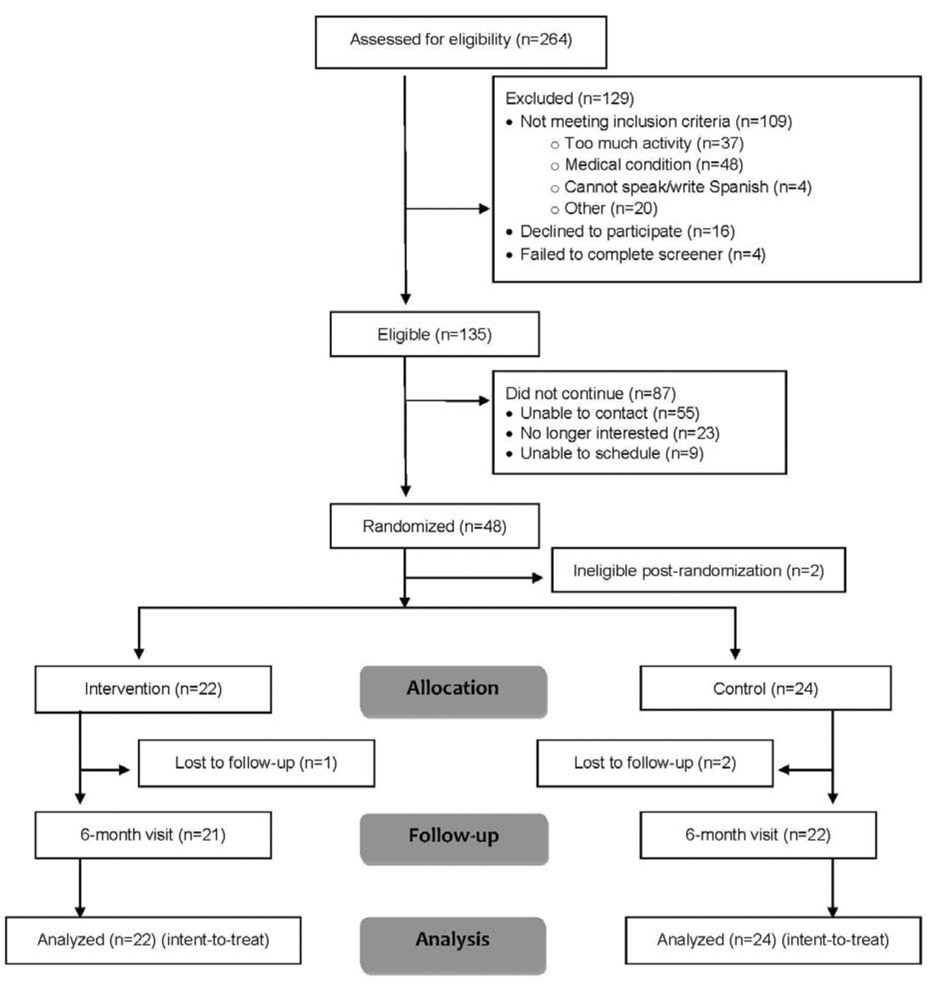
Study participants were 46 men randomized to Intervention (n=22) and Control (n=24) groups (CONSORT diagram, Figure 1). Participants were recruited in 2015–2016, with follow-up visits extending into 2017. Two participants never started and thus were removed from subsequent analyses. Participants were aged 43.04 (SD=10.67) years, and 87% identified as Mexican or Mexican American. The majority had at least some college education (57%), were employed at least part time (87%), were first-generation Americans (85%), and spoke more Spanish than English in the home (70%). There were no significant between-group differences in demographic characteristics or baseline PA (p>0.05 for all). All participants had valid objectively measured MVPA at baseline, and 30 (65%) had valid data at 6 months. In addition, all participants had valid self-reported PA at baseline and 85% had valid data at follow-up. A full description of the sample is presented in Table 1.
Figure 1.
CONSORT diagram.
Table 1.
Baseline Characteristics of the Study Sample, N=46
| Characteristics | Intervention N=22 |
Control N=24 |
|---|---|---|
| Age, years, mean (SD) | 44.2 (10.3) | 42.0 (11.0) |
| Ethnicity, Mexican descent, n (%) | 20 (90.9) | 20 (83.3) |
| Employment | ||
| Unemployed | 2 (9.1) | 4 (16.7) |
| Full time | 14 (63.6) | 15 (62.5) |
| Part time | 6 (27.3) | 5 (20.8) |
| Education, at least some college, n (%) | 10 (45.5) | 16 (66.7) |
| Marital, married/living with partner, n (%) | 16 (72.6) | 15 (62.5) |
| Nativity, n (%) | ||
| First generation | 18 (81.8) | 21 (87.5) |
| Second generation | 4 (8.2) | 2 (8.5) |
| Third generation | 0 (0) | 1 (4.2) |
| Language spoken in the home, n (%) | ||
| Only Spanish | 7 (31.8) | 12 (50.0) |
| Spanish more than English | 9 (40.9) | 4 (16.7) |
| Both equally | 5 (22.7) | 7 (29.2) |
| English more thanSpanish | 1 (4.5) | 1 (4.2) |
| Language read, n (%) | ||
| Only Spanish | 4 (18.2) | 2 (8.3) |
| Spanish more thanEnglish | 8 (36.4) | 10 (41.7) |
| Both equally | 8 (36.4) | 8 (36.4) |
| English more thanSpanish | 2 (9.1) | 2 (9.1) |
| Stofhla Score,a mean (SD) | 34.57 (1.91) | 33.58 (3.53) |
| BMI, mean (SD) | 29.83 (4.83) | 29.67 (4.83) |
Stofhla = short test of functional health literacy in adults.
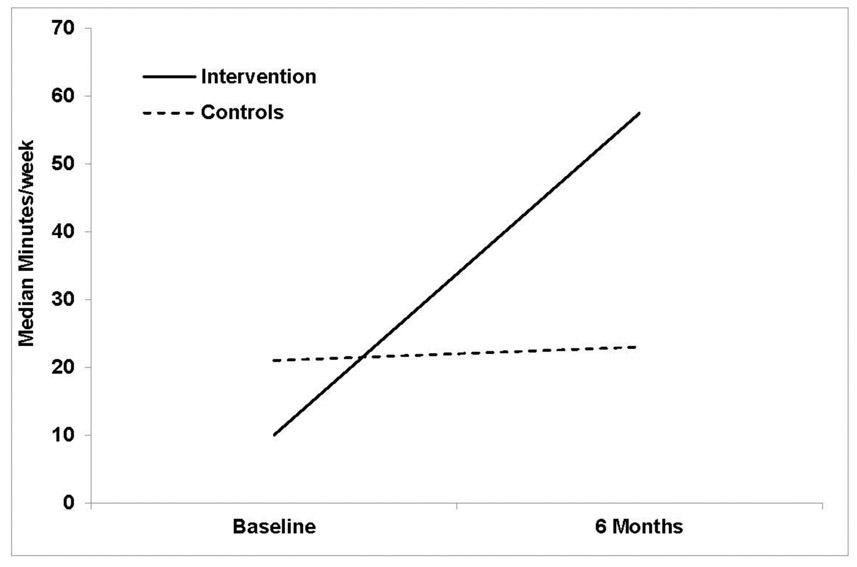
For ActiGraph-measured MVPA, the median increased from 10.00 minutes/week (IQR=0–42.50) to 57.50 minutes/week (IQR=18.50–104.50) among Intervention participants and from 21.00 minutes/week (IQR=0–59) to 23.00 minutes/week (IQR=0–76.25) among Controls. At baseline, median wear time was 13.9 hours/day at baseline and 13.5 hours/day at follow-up with no significant difference between conditions (p>0.05). Quantile regression indicated a significant between-group difference in median objectively measured MVPA at 6 months (b=37.52 [18.01], p=0.04), suggesting a difference in median minutes/week of MVPA at 6 months between Intervention and Control to be 38 minutes. Correlations between self-reported and objectively measured MVPA were borderline significant at baseline (rho=0.28, p=0.07) and significant at 6 months (rho=0.49, p=0.01).
Intervention dose was assessed by evaluating the number of questionnaires returned (zero to six), intervention calls completed (zero to three), and percentage of materials participants reported reading. Adjusting for baseline MVPA, there was a trend toward greater accelerometer-measured MVPA in those returning more questionnaires (b=20.60 [19.66]), for those completing more intervention calls (b=13.38 [18.99]), and for those who reported reading more of the mailed materials (b=12.37 [66.70]).
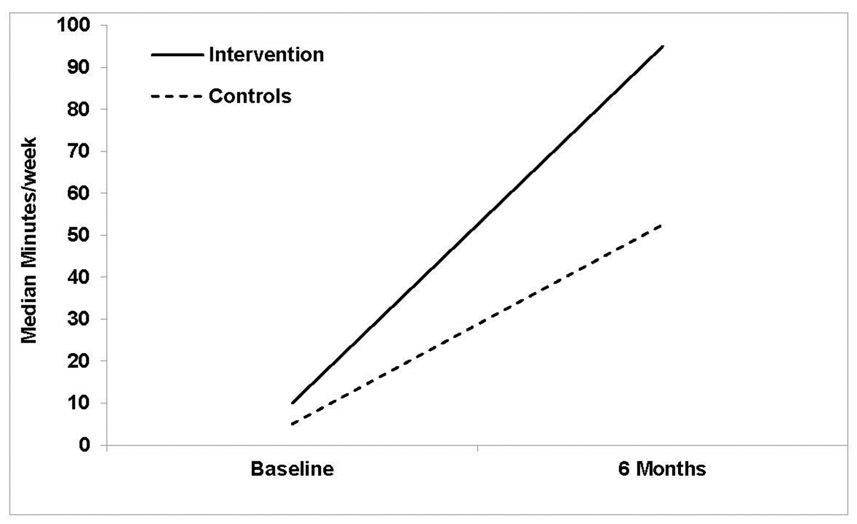
At baseline, median self-reported MVPA was 10.00 minutes/week for Intervention participants (IQR=0–45) and 5.00 minutes/week for controls (IQR=0–43.75). At 6-month follow-up, these increased to 95.00 minutes/week (IQR=15–180) among Intervention participants and 52.50 minutes/week among Controls (IQR=16.25–298.50). These data are presented in Figure 2. Although not significant, there was a trend favoring Intervention participants in minutes/week of MVPA at 6 months controlling for baseline, with a difference in median minutes/week of 42.36 between Intervention and Control (p=0.10). There were no significant differences at baseline or 6 months between face-to-face and remote participants in MVPA measured by accelerometers or self-report (p>0.19 for all).
Figure 2.
Unadjusted between group differences in (A) accelerometer-measured MVPA by group and time point; and (B) self-reported MVPA by group and time point.
MVPA, moderate to vigorous physical activity.
Fourteen participants (36%) of the aggregate sample met national guidelines for self-reported PA at 6 months (47% of Intervention participants vs 25% of Controls, χ2=2.12, p=0.15). Logistic regression models showed an OR of 2.70 (95% CI=0.70, 10.47) for meeting national guidelines in intervention versus control participants.
Models of ActiGraph-measured MVPA at 6 months suggested that, among patients in the intervention group, a greater increased was observed for first-generation participants than second-generation participants (b=113.15, 95% CI=7.96, 234.26). This generation effect was also found for self-reported MVPA at 6 months, controlling for baseline (b=176.19, 95% CI=12.38, 340.01).
Furthermore, those who were married or living with their partner had lower accelerometer-measured MVPA at 6 months compared with those who were single (b= −83.88, 95% CI= −146.72, −21.03). Point estimates did not suggest effects of age, health literacy, BMI, employment or reading language preference on success in the Intervention.
DISCUSSION
Findings from the current study support the preliminary efficacy of Spanish language PA interventions delivered via individually tailored self-help materials and text messages for Latino men. Participants in the intervention group achieved significantly greater increases in MVPA than the control group over a 6-month period. This was seen for both objectively measured and self-reported MVPA (38 and 42 minutes more than controls, respectively), and appeared to increase with intervention dose received. Although the sample size was smaller than planned, the effect size was larger than anticipated, thus findings were still statistically significant. Such increases are similar to those found in prior print- and Internet-based interventions for Latina women (mean differences of 41 and 50 minutes/week at 6 months with similar controls, p<0.01, respectively).4,18 Significant correlations between self-report and accelerometer-recorded MVPA were also found in both studies.
As for predictors of treatment effect, first generation immigrants and single men seemed to benefit more from the intervention than their more acculturated or partnered counterparts. The hypothesis is that individuals who read more in Spanish may have fewer appropriate PA resources/programs and thus found this Spanish language program particularly helpful and relevant to their needs, compared to those who read more in English and thus already had plenty of PA information options available. Single individuals may have had fewer competing demands for their time and thus could participate more fully in the program. Similar results have been found in weight loss studies.39 Thus, future studies may need to take relationship status into consideration when intervening on health behaviors. Recent findings for Latino men have highlighted the importance of family dynamics, social support (spouse, children), and their relationship to accountability for the initiation and maintenance of PA.16
Limitations
Study limitations include the short length (6 months) of the intervention and small sample size (N=46), which limited the feasibility of subanalyses. The study sample comprised primarily first-generation, educated (57% at least some college) Latino men, and thus findings may not generalize to the larger population. Moreover, the study focused on MVPA and may not fully capture physically active work, which may be more prominent in Latino men. For remote participants, anthropometric measures were not collected and PA recall interviews occurred by phone. However, this allowed the authors to determine that the intervention could be disseminated to a larger audience without requiring face-to-face visits. Additional strengths of the study include the understudied, high-risk population, RCT design, both objective and self-report measures of MVPA, and high retention rate (93.5%). The high retention rate in this study may be due to a number of strategies, including offering flexible times for study visits (early morning, evening, weekends), visits and check-in calls were made by the same bilingual, bicultural staff who built rapport with participants, and staff used multiple modes of communication (text, letter, phone) to contact participants who missed study appointments.
Latino men are often not well represented in clinical trials, despite recent NIH program announcements focused on minority men. Past researchers have faced challenges to recruiting Latino men and this study was no different.40 Based on previous experience recruiting Latina women, initial recruitment efforts for this study used diverse approaches, such as community events, partnering with local leaders and churches, and posting advertisements on Latino newspapers and Craigslist. However, among this population of Latino men, non-face-to-face recruitment strategies were more effective and yielded the majority of participants. However, though recruitment was difficult, Latino men had higher retention rates and satisfaction compared to previous studies with Latina women.3,4 Future research should continue to identify strategies to recruit and engage Latino men. Although some flexibility may be required to facilitate Latino male research participation, their voices will be critical to developing effective interventions and addressing existing health disparities.
It is hypothesized that intervention components contributed to differences in PA between the Intervention Group and Controls by addressing participant calls for accountability (via phone calls, texting), more information on including family members and children in PA and environmental resources (in self-help print materials), and accommodation of busy work schedules and odd hours (in all three distance-based approaches). However, the multiple component nature of this intervention makes it difficult to determine the individual influences of the various features. Multiphase optimization strategies could help tease out added benefits of text messaging and further streamline the intervention for cost effectiveness prior to large-scale dissemination and implementation.
Finally, given national data supporting smartphone access in Latino men8 and their apparent willingness to receive/interact with phone-based PA intervention strategies in the current study, future steps will involve transferring the program to smartphone application for increased convenience and ease of use.
CONCLUSIONS
The poor chronic disease profile for U.S. Latino men, coupled with few Spanish PA interventions, necessitates research that can produce practice-relevant evidence leading to effective PA programs for this population. These results show feasibility and good potential efficacy of an expert system tailored print intervention paired with text messaging, including delivering the intervention remotely via non-face-to-face mediated channels, and objective measurement. The ongoing challenge is to establish maintenance that will contribute to a sustained healthy lifestyle and reduced health disparities.
ACKNOWLEDGMENTS
This work was supported by the National Institute of Nursing Research and NIH (R21NR014911). The study sponsor had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication. The study was approved by the IRB at the University of California, San Diego on October 23, 2014 (IRB #141174).
Footnotes
The main findings from this study were presented at the 2018 Annual Meeting for the Society of Behavioral Medicine.
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Umpierrez GE, Gonzalez A, Umpierrez D, Pimentel D. Diabetes mellitus in the Hispanic/Latino population: an increasing health care challenge in the United States. Am J Med Sci. 2007;334(4):274–282. 10.1097/maj.0b013e3180a6efe3. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011-2012. NCHS Data Brief 2013;(131):1–8. www.ncbi.nlm.nih.gov/pubmed/24152742 Accessed March 11, 2020. [PubMed] [Google Scholar]
- 3.Marcus BH, Dunsiger SI, Pekmezi D, et al. Twelve-month physical activity outcomes in Latinas in the Seamos Saludables Trial. Am J Prev Med. 2015;48(2):179–182. 10.1016/j.amepre.2014.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marcus BH, Hartman SJ, Larsen BA, et al. Pasos Hacia La Salud: a randomized controlled trial of an internet-delivered physical activity intervention for Latinas. Int J Behav Nutr Phys Act. 2016;13:62 10.1186/s12966-016-0385-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Griffith DM, Bergner EM, Cornish EK, McQueen CM. Physical activity interventions with African American or Latino men: a systematic review. Am J Mens Health. 2018;12(4):1102–1117. 10.1177/1557988318763647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White M, Shoemaker ML, Park S, et al. Prevalence of modifiable cancer risk factors among U.S. adults aged 18–44 years. Am J Prev Med. 2017;53(3 suppl 1):S14–S20. 10.1016/j.amepre.2017.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arredondo EM, Sotres-Alvarez D, Stoutenberg M, et al. Physical activity levels in U.S. Latino/Hispanic adults: results from the Hispanic Community Health Study/Study of Latinos. Am J Prev Med. 2016;50(4):500–508. 10.1016/j.amepre.2015.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. National Health Interview Survey, 2017. Age-adjusted percent distributions (with standard errors) of participation in leisure-time aerobic and muscle-strengthening activities that meet the 2008 federal physical activity guidelines among adults aged 18 and over, by selected characteristics: United States, 2017. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2017_SHS_Table_A-14.pdf Published 2017. Accessed March 11, 2020.
- 9.Neighbors CJ, Marquez DX, Marcus BH. Leisure-time physical activity disparities among Hispanic subgroups in the United States. Am J Public Health. 2008;98(8):1460–1464. 10.2105/ajph.2006.096982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics. Health, United States, 2018. Hyattsville, MD: National Center for Health Statistics; 2019. www.cdc.gov/nchs/data/hus/hus18.pdf. Accessed March 11, 2020. [Google Scholar]
- 11.Sohn EK, Porch T, Hill S, Thorpe RJ. Geography, race/ethnicity, and physical activity among men in the United States. Am J Mens Health. 2017;11(4):1019–1027. 10.1177/1557988316689498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat 10. 2012;(252):1–207. www.ncbi.nlm.nih.gov/pubmed/22834228. [PubMed] [Google Scholar]
- 13.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mathieu RA, Powell-Wiley TM, Ayers CR, et al. Physical activity participation, health perceptions, and cardiovascular disease mortality in a multiethnic population: the Dallas Heart Study. Am Heart J. 2012;163(6):1037–1040. 10.1016/j.ahj.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez J, Powell J, Agne A, Scarinci I, Cherrington A. A focus group study of Mexican immigrant men’s perceptions of weight and lifestyle. Public Health Nurs. 2012;29(6):490–498. 10.1111/j.1525-1446.2012.01026.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Valdez LA, Morrill KE, Griffith DM, Lindberg NM, Hooker SP, Garcia DO. Mexican origin Hispanic men’s perspectives of physical activity–related health behaviors. Am J Mens Health. 2019;13(1): 1557988319834112 10.1177/1557988319834112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larsen BA, Dunsiger S, Hartman S, et al. Activo: assessing the feasibility of designing and implementing a physical activity intervention for Latino Men. Int J Mens Health. 2014;13(1):60–71. 10.3149/jmh.1301.60. [DOI] [Google Scholar]
- 18.Marcus BH, Dunsiger SI, Pekmezi DW, et al. The Seamos Saludables Study: a randomized controlled physical activity trial of Latinas. Am J Prev Med. 2013;45(5):598–605. 10.1016/j.amepre.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pew Research Center. Demographics of mobile device ownership and adoption in the United States, www.pewinternet.org/fact-sheet/mobile/. Published 2019. Accessed March 11, 2020.
- 20.Duggan M Cell Phone Activities 2012. https://www.pewresearch.org/internet/2012/11/25/additional-demographic-analysis-2/. Published 2012.
- 21.Fanning J, Mullen SP, McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J Med Internet Res. 2012;14(6):e161 10.2196/jmir.2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lau PWC, Lau EY, Wong DP, Ransdell L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res. 2011;13(3):e48 10.2196/jmir.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas S, Reading J, Shephard R. Revision of the physical activity readiness questionnaire (PAR-Q). Can J Sport Sci. 1992;17(4):338–345. https://psycnet.apa.org/record/1993-24047-001. [PubMed] [Google Scholar]
- 24.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–2304. 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 25.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537–541. 10.1007/bf02640361. [DOI] [PubMed] [Google Scholar]
- 26.Janz KF. Validation of the CSA accelerometer for assessing children’s physical activity. Med Sci Sport Exerc. 1994;26(3):369–375. 10.1249/00005768-199403000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Melanson EL, Freedson PS. Validity of the Computer Science and Applications, Inc. (CSA) activity monitor. Med Sci Sport Exerc. 1995;27(6):934–940. 10.1249/00005768-199506000-00021. [DOI] [PubMed] [Google Scholar]
- 28.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, Mcdowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 29.Prince SA, Adamo KB, Hamel M, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-day PAR. Med Sci Sport Exerc. 2003;35(5):801–809. 10.1249/01.mss.0000064941.43869.4e. [DOI] [PubMed] [Google Scholar]
- 31.Leenders NY, Sherman WM, Nagaraja HN, Kien CL. Evaluation of methods to assess physical activity in free-living conditions. Med Sci Sport Exerc. 2001;33(7):1233–1240. 10.1097/00005768-200107000-00024. [DOI] [PubMed] [Google Scholar]
- 32.Dunn AL, Garcia ME, Marcus BH, Kampert JB, Kohl HW, Blair SN. Six-month physical activity and fitness changes in Project Active, a randomized trial. Med Sci Sport Exerc. 1998;30(7):1076–1083. 10.1097/00005768-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281(4):327–334. https://doi.org/10-1001/pubs.jama-issn-0098-7484-281-4-joc80889. [DOI] [PubMed] [Google Scholar]
- 34.Rauh MJD, Hovell MF, Hofstetter CR, Sallis JF, Gleghorn A. Reliability and validity of self-reported physical activity in Latinos. Int J Epidemiol. 1992;21(5):966–971. 10.1093/ije/21.5.966. [DOI] [PubMed] [Google Scholar]
- 35.Bock BC, Marcus BH, Pinto BM, Forsyth LH. Maintenance of physical activity following an individualized motivationally tailored intervention. Ann Behav Med. 2001;23(2):79–87. 10.1207/s15324796abm2302_2. [DOI] [PubMed] [Google Scholar]
- 36.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–66. 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 37.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992;11(6):386–395. 10.1037/0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 38.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schoeppe S, Vandelanotte C, Rebar AL, Hayman M, Duncan MJ, Alley SJ. Do singles or couples live healthier lifestyles? Trends in Queensland between 2005–2014. PLoS One. 2018;13(2):e0192584 10.1371/journal.pone.0192584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ayala GX, San Diego Prevention Research Center Team. Effects of a promotor-based intervention to promote physical activity: Familias Sanas y Activas. Am J Public Health. 2011;101(12):2261–2268. 10.2105/ajph.2011.300273. [DOI] [PMC free article] [PubMed] [Google Scholar]