Abstract
Objective:
This study examined the associations between insomnia, anxiety, and depression in college women with eating disorders (EDs).
Participants:
Six hundred and ninety female students from 28 U.S. colleges who screened positive for an ED were assessed for psychiatric comorbidities. Women were, on average, 22.12 years old, mostly White (60.1%), and undergraduates (74.3%).
Methods:
Two mediation models were tested to determine if depression and/or anxiety mediated the relationship between insomnia and ED symptomatology.
Results:
One-fifth of the sample (21.7%) reported clinically moderate and severe levels of insomnia. Both depression (B=.13, p<.001) and anxiety (B=.13, p<.001) significantly mediated the relationship between insomnia and ED psychopathology.
Conclusions:
Insomnia is relatively common in college-age women with EDs. Findings suggest that this association between ED and sleep disturbances can be explained, in part, by changes in depression and anxiety. Clinicians should consider incorporating mental health assessments for insomnia, depression, and anxiety into current ED prevention, intervention, and screening efforts on college campuses.
Keywords: anxiety, college students, depression, eating disorders, insomnia
Eating disorders (EDs) are serious mental illnesses associated with significant psychosocial impairment, clinical distress, and mortality.1,2 EDs are multifaceted and involve interactions among various genetic, behavioral, and cognitive risk and maintenance factors, including the internalization of a thin ideal of beauty,3 emotion dysregulation and distress intolerance,4,5 interpersonal dysfunction,6 and perfectionism.7,8 As such, ED presentations include various behaviors, such as dietary restraint, binge eating, purging (i.e., vomiting, laxative/diuretic abuse), and excessive exercise.9 Illness complications are further compounded by the fact that EDs are highly comorbid with a variety of psychiatric conditions, including mood, anxiety, and sleep disorders.1,2,10
Insomnia is a unique manifestation of a disruption in a person’s homoeostatic state, caused by circadian system irregularities,11 prolonged hyperarousal,12,13 and behavioral factors (e.g., poor sleep hygiene, high consumption of caffeine and/or alcohol, excessive stress)11 – all of which could exacerbate other altered homoeostatic processes, including eating. Clinical insomnia is both a risk and maintenance factor for ED psychopathology. Insomnia is associated with overall severity of ED symptoms as well as poorer quality of life and treatment outcomes.10,14,15 Past research has demonstrated that individuals with EDs endorse significantly higher levels of insomnia symptoms relative to controls. 10,16,17 Although sleep disturbances are common across the ED diagnostic spectrum,10,15 insomnia is especially prevalent in individuals with binge/purge symptomatology.18–21 The high co-occurrence of insomnia and disordered eating behaviors (ranging from 25-30% in college-age women)14 is attributed, in part, to disrupted physiological mechanisms, including fluctuations in orexin, an important hormone involved in regulating wakefulness and appetite, in cortisol, a stress hormone, and in ghrelin and leptin, hormones responsible for signaling hunger.10,14,22,23
College students are particularly vulnerable to developing both insomnia and EDs, with prevalence estimates hovering around 9.5% and 3.6-13.5%, respectively.24,25 Insomnia is highly prevalent in college women across the ED risk and diagnostic spectrum, with prevalence estimates increasing incrementally by ED risk status.14 Further, binge/purge symptomatology predicts the onset of later clinical insomnia in college samples.18,20 However, research to enhance the understanding of the associations between EDs and insomnia in college populations is needed, as it may inform screening and intervention initiatives, improve academic functioning, and reduce adverse long-term health outcomes for this vulnerable population.26–29
To date, there has been little empirical investigation into the contributing role of additional mental comorbidities to the co-occurrence of eating and sleep disorders. Considering that clinical insomnia and EDs are highly comorbid with mood and anxiety disorders,2,30 it is possible that insomnia influences ED symptomology through changes in depression and anxiety.31 Indeed, depression has been found to mediate the association between insomnia and eating pathology in outpatient and adult community samples.16,32 Anxiety, on the other hand, is predictive of insomnia in the general population30 and mediates the relationship between emotional eating and insomnia in adolescents.33 Replicating and extending these mediation models to college samples is a key next step in learning how these disorders are associated with insomnia symptomatology in college students.
This study was designed to examine whether depression and anxiety mediated the relationship between insomnia and eating psychopathology in a large sample of college-age women with EDs. Based on prior research,16,32,33 we hypothesized that both depression and anxiety would mediate the relationship between insomnia and ED symptomology for the sample. Findings can help to identify new advancements in the clinical assessment, prevention, and treatment of both insomnia and EDs amongst this high-risk population.
Materials and Methods
Participants and Procedure
This study utilized baseline data from 690 participants of the Healthy Body Image (HBI) Program study, a randomized controlled trial testing the efficacy of an Internet-based, guided self-help program for college-age women with EDs at 28 U.S. universities (see earlier reports34,35 for more details on study design and data collection). Eligibility criteria for the parent trial included identifying as female, being ≥18 years, currently enrolled as a student at one of the participating universities, and screening positive for a DSM-5 clinical or subclinical ED,9 with the exception of anorexia nervosa (AN). Given the medical complications associated with this illness, all individuals who screened positive for AN were given a referral to the healthcare center at their respective institution. The Institutional Review Boards at the principal investigators’ universities approved all study procedures and materials prior to the commencement of the study. Informed consent was obtained prior to assessment completion.
Measures
All measures were self-report and completed online through Qualtrics.
Eating psychopathology.
The Eating Disorder Examination-Questionnaire (version 6.0; EDE-Q)36 is a 28-item measure that was used to measure frequency and severity of ED symptoms (i.e., vomiting, laxative/diuretic abuse, compulsive exercise, binge eating) over the last 28 days. The EDE-Q consists of four subscales – Weight Concern, Shape Concern, Eating Concern, and Restraint – as well as a Global score that measures global severity of ED symptomatology. Subscale scores are averaged to derive the EDE-Global score. If a participant reports an EDE-Q Global score above 2.3, they are considered to have a clinical ED.37 The EDE-Q demonstrates good validity and reliability in undergraduate women.38,39 In this study, Cronbach’s alpha for the EDE-Q Global score was .76.
Insomnia.
Participant’s level of insomnia symptomatology was assessed using the seven-item Insomnia Severity Index (ISI)40 measure. Items are rated on a 5-point Likert scale ranging from 0 (“not at all”) to 4 (“extremely”), with total scores ranging from 0–28. Higher scores indicate greater insomnia symptom severity, and participants that score ≥10 are considered to exhibit clinically significant levels of insomnia.40,41 Participants were categorized as either being non-clinical (scores of 0-7), or exhibiting subthreshold insomnia (8-14), moderately severe clinical insomnia (15-21), or severe clinical insomnia (22-28). The ISI demonstrates good face validity and internal consistency.42 Cronbach’s alpha for the current study was .89.
Depression.
The Patient Health Questionnaire (PHQ-9)43 is a nine-item survey that assessed participants’ level of depressive symptoms over the past two weeks. Items are rated on a 4-point scale, ranging from 0 (“not at all”) to 3 (“nearly every day”), with total scores ranging from 0–27. Higher scores correspond with greater depressive symptom severity. The PHQ-9 is considered to be a valid and reliable measure of depressive severity, with a clinical cutoff of 10 indicating moderate depression. 43,44 Since item three of the PHQ-9 assesses sleep disturbance (i.e., “trouble falling or staying asleep, or sleeping too much”), we removed this item and modified the PHQ-9 scores by totaling the remaining items to derive a total score for the resulting measure (Cronbach’s α=.87). Similar methods have been used in past ED and sleep research.35,45 Hereafter, this measure is referred to as the “modified PHQ-9.”
Anxiety.
Participants’ anxiety symptoms were measured using the Patient-Reported Outcomes Measurement Information System (PROMIS) Short Form v1.0 – Anxiety4a questionnaire.46 Items are rated on a 5-point Likert scale, ranging from 0 (“never”) to 4 (“always”). Scores range from 4-20 and the clinical cutoff score is considered to be ≥8.47 The PROMIS demonstrates good precision, efficiency, and internal reliability.48 In this study, Cronbach’s alpha was .90.
Analytic Strategy
Preliminary tests of skewness and kurtosis and Mahalanobis distance indicated that the data did not violate assumptions of univariate or multivariate normality. None of the study variables violated the conditions of collinearity (i.e., tolerance > .10; VIF < 10). Secondary analyses using a cross-sectional dataset were conducted. Specifically, using the Hayes model,49 two mediation analyses were performed, using bootstrapping, to determine whether the relationship between insomnia and global ED psychopathology was mediated by depression and anxiety symptoms, respectively. According to this method, in the final regression model, if the relationship between the independent and the dependent variables attenuates to non-significance after controlling for the mediating variable, then a significant mediation effect can be inferred. Additionally, in this model, an indirect effect is considered to be significant if the confidence interval does not include zero.50 All data were analyzed using SPSS 25;51 mediation analyses were conducted using PROCESS version 3.49
Results
Sample characteristics
Participants reported a mean age of 22.12 years (SD=4.84, range=18–58). They identified as White (60.1%), Black or African American (5.4%), Asian or South Asian (17.1%), American Indian or Alaska Native (0.4%), Native Hawaiian or Pacific Islander (0.1%), multi-racial (7.7%), and other (6.7%). Nearly one-fifth of the sample identified as Hispanic (17.4%). Most participants were either undergraduate (74.3%) or graduate students (24.8%). Mean body mass index was 25.70 kg/m2 (SD=6.00). The distribution of insomnia symptomatology (M=9.47, SD=6.34) was as follows: non-clinical insomnia (42.3%), subthreshold insomnia (35.1%), clinically moderately severe insomnia (16.5%), and clinically severe insomnia (5.2%). The current sample reported relatively high scores on the EDE-Q Global (M=3.57; SD=1.10), and moderate scores on the modified PHQ-9 (M=9.74; SD=5.45) and the PROMIS (M=11.18; SD=4.22).
Mediation models
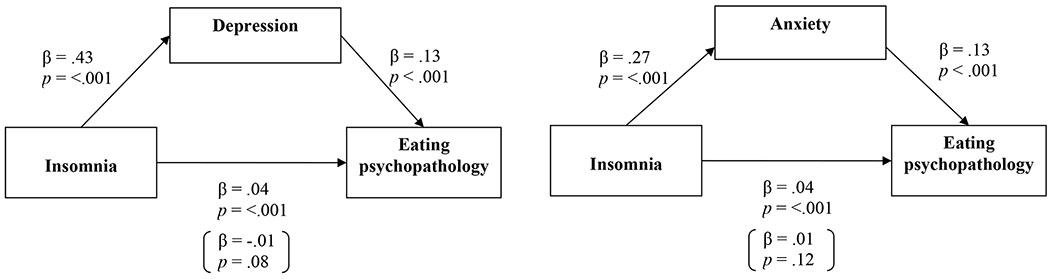
The overall mediation model – whereby insomnia symptom severity was modeled to contribute to ED psychopathology through depression – was significant, F(2, 680) = 190.31, p < .001, and accounted for 35.9% of the variance in ED psychopathology (See Figure 1). This model, conducted with 5,000 bootstraps, yielded a mean bootstrap estimate of the indirect effect of .05 (SE = .005). Because the 95% confidence interval did not include zero (0.05 – 0.06), we concluded that the indirect effect of depression on the association between insomnia and ED psychopathology was significant. In other words, insomnia was associated with greater depressive symptom severity, which in turn, was associated with global ED symptom severity for the sample.
Figure 1.
Models testing mediation of the insomnia-ED psychopathology association through depression and anxiety (N=690). Values in parentheses represent the standardized association between insomnia and ED psychopathology after controlling for depression and/or anxiety.
A second mediation model was conducted whereby anxiety was modeled to mediate the association between global ED psychopathology and insomnia symptom severity (See Figure 1). The overall model was significant, F(2, 681) = 116.29, p < .001, and accounted for 25.5% of the variance in ED psychopathology. This model, conducted with 5,000 bootstraps, yielded a mean bootstrap estimate of the indirect effect of .03 (SE = .004). Because the 95% confidence interval did not include zero (0.03 – 0.04), we concluded that the indirect effect of anxiety on the association between insomnia and ED psychopathology was significant. Similarly, insomnia was associated with greater anxiety symptom severity, which in turn, was associated with greater global ED psychopathology for the sample.
Discussion
This study examined the prevalence of clinical insomnia in a large sample of college women with EDs, and whether depression and anxiety mediated the association between insomnia and EDs for this group. Findings revealed that one in five college women with EDs endorsed insomnia symptomatology that was clinically moderate or severe, similar to past ED research.14 As hypothesized, both depression and anxiety independently mediated the association between insomnia symptom severity and EDs, suggesting that insomnia symptoms per se may not directly exacerbate ED symptoms, but that they may do so through indirect pathways. These findings both confirm and extend past research on community samples16 and adolescents,33 suggesting that similar relationships apply for college women with EDs. Although many studies have demonstrated a robust link between depression, sleep disturbances, and EDs,10,15 the present study provides evidence that depressive symptoms, separate from the effects of sleep, significantly mediate the association between insomnia and ED symptoms. Furthermore, these findings illustrate how anxiety and insomnia symptoms can influence one another to increase ED symptom severity.
This is one of the first studies to assess for the associations between insomnia and comorbid mental illnesses among a large, geographically diverse sample of college women with EDs. However, there are a number of limitations. First, the data are based on self-report rather than objective, physiological measures. However, due to the logistic limitations imposed by the parent trial (e.g., study was deployed across 28 universities and designed to test Internet-based, technological advancements in ED treatment), self-report measures were the most accessible, efficient, and scalable means of obtaining data on college women with EDs in an anonymous, minimally invasive manner. Furthermore, these measures have strong psychometric support for use in clinical and research settings to assess for various mental health outcomes (i.e., sleep disturbance, eating psychopathology, depression, anxiety). Next, data were cross-sectional and thus causality cannot be inferred; longitudinal exploration into the nature of the relationship between EDs, insomnia, depression, and anxiety, as well as additional transdiagnostic constructs that affect both insomnia and EDs (e.g., emotion dysregulation, weight status)52,53 for college women is warranted. Last, future research should replicate these findings with other populations, including non-female students with EDs, and should examine whether these mediation models hold in a sample of college students without EDs.
Findings illustrate the complex interplay between sleep, eating, mood, and anxiety disorders and highlight these relationships within college women with EDs. Health professionals treating college students presenting with EDs should comprehensively assess for common comorbidities, such as depression, anxiety, and insomnia. For patients with both EDs and insomnia symptoms, targeting depression and anxiety early in treatment may have the added benefit of attenuating the impact of insomnia on eating psychopathology for this group.
Both sleep disorders and EDs place a significant economic burden upon college campuses.54,55 Although many universities offer mental health services through school-funded counseling centers, many college students are unable or unwilling to seek care due to a series of societal (e.g., stigma), institutional (e.g., understaffed and underfunded counseling centers), and personal barriers (e.g., denial of issue).54 Considering this high-cost and the barriers associated with seeking and receiving care, early prevention and psychoeducation may be key to curbing the adverse consequences of sleep disorders and EDs.56
In the current study, a sizeable group of college-age women with EDs reported clinically moderate and severe insomnia symptomatology, and this relationship was mediated by depressive and anxiety symptoms. These results underscore the importance of considering comorbidities when addressing the impact of insomnia and EDs in college women, and offer additional insights into the complex relationships among these common psychological conditions.1,2 Health professionals should consider incorporating insomnia, depression, and anxiety screenings into ED assessment, prevention, and intervention efforts on college campuses.
Acknowledgments
The authors would like to thank all participating universities, research participants, and study staff for their time and dedication to this trial, without whom this work would not be possible. We would also like to thank Drs. Andrea Kass Graham, Dawn Eichen, Corinna Jacobi, and Megan Jones Bell for their contributions to this grant. This research was supported by funding from the National Institutes of Health (NIH), R01 MH100455, K08 MH120341, T32 HL007456, and T32 HL130357.
Footnotes
Declaration of Interest
The authors have no financial or non-financial interests to disclose at this time.
References
- 1.Klump KL, Bulik CM, Kaye WH, Treasure J, Tyson E. Academy for eating disorders position paper: Eating disorders are serious mental illnesses. Int J Eat Disord. 2009; 42(2): 97–103. [DOI] [PubMed] [Google Scholar]
- 2.Schaumberg K, Welch E, Breithaupt L, et al. The science behind the academy for eating disorders’ nine truths about eating disorders. Eur Eat Disord Rev. 2017; 25: 432–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Striegel-Moore RH, Bulik CM. Risk factors for eating disorders. Am Psychol. 2007; 62(3): 181–198. [DOI] [PubMed] [Google Scholar]
- 4.Harrison A, Sullivan S, Tchanturia K, Treasure J. Emotional functioning in eating disorders: Attentional bias, emotion recognition and emotion regulation. Psychol Med. 2010; 40: 1887–1897. [DOI] [PubMed] [Google Scholar]
- 5.Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. J Consult and Clin Psych. 2001; 69(6): 1061–1065. [DOI] [PubMed] [Google Scholar]
- 6.Monterubio GE, Fitzsimmons-Craft EE, Wilfley DE. Interpersonal dysfunction as a risk factor for eating disorders. In: Wade T, ed. Encyclopedia of feeding and eating disorders. Springer; Singapore; 2017. [Google Scholar]
- 7.Bardone-Cone AM, Wonderlich SA, Frost RO, et al. Perfectionism and eating disorders: Current status and future directions. Clin Psychol Rev. 2007; 27: 384–405. [DOI] [PubMed] [Google Scholar]
- 8.Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behav Res Ther. 2003; 41: 509–528. [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 10.Allison KC, Spaeth A, Hopkins CM. Sleep and eating disorders. Curr Psychiatry Rep. 2016; 18: 92. [DOI] [PubMed] [Google Scholar]
- 11.Reeve K, Bailes B. Insomnia in adults: etiology and management. J for Nurse Practitioners - JNP. 2010; 6: 53–60. [Google Scholar]
- 12.Roth T Insomnia: definition, prevalence, etiology, and consequences. JCSM. 2007; 3: S7–S10. [PMC free article] [PubMed] [Google Scholar]
- 13.Levenson JC, Kay DB, Buysse DJ. The pathophysiology of insomnia. Chest. 2015; 147(4): 1179–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aspen V, Weisman H, Vannucci A, et al. Psychiatric co-morbidity in women presenting across the continuum of disordered eating. Eat Behav. 2014; 15: 686–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lundgren JD, O’Reardon JP, Allison KC, Spresser CD. Sleep and quality of life in eating disorders. In Verster JC, Pandi-Perumal SR, Streiner DL, eds. Sleep and quality of life in clinical medicine. Totowa, NJ: Humana Press; 2008. [Google Scholar]
- 16.Kenny TE, Van Wijk M, Singleton C, Carter JC. An examination of the relationship between binge eating disorder and insomnia symptoms. Eur Eat Disord Rev. 2018; 26: 186–196. [DOI] [PubMed] [Google Scholar]
- 17.Tromp MDP, Donners AAMT, Garssen J, Verster JC. Sleep, eating disorder symptoms, and daytime functioning. Nat Sci Sleep. 2016; 8: 35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bos SC, Soares MJ, Marques M, et al. Disordered eating behaviors and sleep disturbances. Eat Behav. 2013; 14: 192–198. [DOI] [PubMed] [Google Scholar]
- 19.Kim KR, Jung YC, Shin MY, Namkoong K, Kim JK, Lee JH. Sleep disturbance in women with eating disorder: Prevalence and clinical characteristics. Psychiatry Res. 2010; 176: 88–90. [DOI] [PubMed] [Google Scholar]
- 20.Soares MJ, Macedo A, Bos SC, et al. Sleep disturbances, body mass index and eating behaviour in undergraduate students. J Sleep Res. 2011; 20: 479–486. [DOI] [PubMed] [Google Scholar]
- 21.Trace SE, Thornton LM, Runfola CD, Lichtenstein P, Pedersen NL, Bulik CM. Sleep problems are associated with binge eating in women. Int J Eat Disord. 2012; 45(5): 669–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coutinho WF, Moreira RO, Spagnol C, Appolinario JC. Does binge eating disorder alter cortisol secretion in obese women? Eat Behav. 2007; 8(1): 59–64. [DOI] [PubMed] [Google Scholar]
- 23.Lauer CJ, Krieg JC. Sleep in eating disorders. Sleep Med Rev. 2004; 8: 109–118. [DOI] [PubMed] [Google Scholar]
- 24.Eisenberg D, Nicklett EJ, Roeder K, Kirz NE. Eating disorder symptoms among college students: Prevalence, persistence, correlates, and treatment-seeking. J Am Coll Heal. 2011; 59(8): 700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor DJ, Bramoweth AD, Grieser EA, Tatum JI, Roane BM. Epidemiology of insomnia in college students: Relationship with mental health, quality of life, and substance use difficulties. Behav Ther. 2013; 44: 339–348. [DOI] [PubMed] [Google Scholar]
- 26.Beiter R, Nash R, McCrady M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord. 2015; 173: 90–96. [DOI] [PubMed] [Google Scholar]
- 27.Pedrelli P, Nyer M, Yeung A, Zulauf C, Wilens T. College students: mental health problems and treatment considerations. Acad Psychiatry. 2015; 39(5): 503–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Trockel MT, Barnes MD, Egget DL. Health-related variables and academic performance among first-year college students: Implications for sleep and other behaviors. J Am Coll Heal. 2000; 49(3): 125–131. [DOI] [PubMed] [Google Scholar]
- 29.Yanover T, Thompson JK. Eating problems, body image disturbances, and academic achievement: Preliminary evaluation of the eating and body image disturbances academic interference scale. Int J Eat Disord. 2008; 41: 184–187. [DOI] [PubMed] [Google Scholar]
- 30.Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008; 64: 443–449. [DOI] [PubMed] [Google Scholar]
- 31.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. SLEEP. 2013; 36(7): 1059–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lombardo C, Battagliese G, Venezia C, Salvemini V. Persistence of poor sleep predicts the severity of the clinical condition after 6 months of standard treatment in patients with eating disorders. Eat Behav. 2015; 18: 16–19. [DOI] [PubMed] [Google Scholar]
- 33.Nguyen-Rodriguez ST, McClain AD, Spruijt-Metz D. Anxiety mediates the relationship between sleep onset latency and emotional eating in minority children. Eat Behav. 2010; 11: 297–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fitzsimmons-Craft EE, Firebaugh ML, Graham AK, et al. State-wide university implementation of an online platform for eating disorders screening and intervention. Psyc Serv. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goel NJ, Sadeh-Sharvit S, Flatt RE, et al. Correlates of suicidal ideation in college women with eating disorders. Int J Eat Disord. 2018; 51(6): 579–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fairburn CG. Cognitive behavior therapy and eating disorders. New York, NY: Guilford Press; 2008. [Google Scholar]
- 37.Mond JM, Hay PJ, Rodgers B, et al. Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Beh Res Th. 2004; 42(5): 551–567 [DOI] [PubMed] [Google Scholar]
- 38.Luce KH, Crowther JH, Pole M. Eating disorder examination questionnaire (EDE-Q): Norms for undergraduate women. Int J Eat Disord. 2008; 41: 273–276. [DOI] [PubMed] [Google Scholar]
- 39.Rose JS, Vaewsorn A, Rosselli-Navarra F, et al. Test-retest reliability of the eating disorder examination-questionnaire (EDE-Q) in a college sample. J Eat Disord. 2013; 1: 42–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001; 2(4): 297–307. [DOI] [PubMed] [Google Scholar]
- 41.Morin CM, Colecchi C, Stone J, Sood RM, Brink D. Behavioral and pharmacological therapies for late-life insomnia: A randomized controlled trial. J Am Med Assoc. 1999; 281: 991–999. [DOI] [PubMed] [Google Scholar]
- 42.Smith MT, Wegener ST. Measures of sleep: The insomnia severity index, medical outcomes study (MOS) sleep scale, Pittsburgh sleep diary (PSD), and Pittsburgh sleep quality index (PSQI). Arthritis Rheum. 2003; 49(5S): S184–S196. [Google Scholar]
- 43.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psyc Annals. 2002; 32(9): 509–515. [Google Scholar]
- 44.Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009; 114: 163–173. [DOI] [PubMed] [Google Scholar]
- 45.Trockel M, Karlin BE, Taylor CB, Brown GK, Manber R. Effects of cognitive behavioral therapy for insomnia on suicidal ideation in veterans. SLEEP. 2015; 38(2): 259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS): Depression, anxiety, and anger. Assessment. 2011; 18(3): 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kroenke K, Yu Z, Wu J, Kean J, Monahan PO. Operating characteristics of PROMIS four-item depression and anxiety scales in primary care patients with chronic pain. Pain Med. 2014; 15(11): 1892–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010; 63(11): 1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hayes A Introduction to mediation, moderation, and conditional process analysis. 2nd ed. New York, NY: Guilford Press; 2017. [Google Scholar]
- 50.Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychol Sci. 2007; 18(3): 233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Corp IBM. IBM SPSS Statistics for Windows, Version 25.0. 2017. Armonk, NY: IBM Corp. [Google Scholar]
- 52.Kauffman BY, Bakhshaie J, Lam H, Alfano C, Zvolensky MJ. Insomnia and eating expectancies among college students: the role of emotion dysregulation. Cogn Behav Ther. 2018; 47(6): 470–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yeh S- SS, Brown RF. Disordered eating partly mediates the relationship between poor sleep quality and high body mass index. Eat Behav. 2014; 15: 291–297. [DOI] [PubMed] [Google Scholar]
- 54.Kass AE, Balantekin KN, Fitzsimmons-Craft EE, Jacobi C, Wilfley DE, Taylor CB. The economic case for digital interventions for eating disorders among United States college students. Int J Eat Disord. 2017; 50: 250–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Prichard JR, Hartmann ME. Follow-up to Hartmann & Prichard: Should universities invest in promoting healthy sleep? A question of academic and economic significance. Sleep Heal. In press. [DOI] [PubMed] [Google Scholar]
- 56.Trockel M, Manber R, Chang V, Thurston A, Taylor CB. An e-mail delivered CBT for sleep-health program for college students: Effects on sleep quality and depression symptoms. J Clin Sleep Med. 2011; 7(3): 276–281. [DOI] [PMC free article] [PubMed] [Google Scholar]