Abstract
Objective:
To compare healthcare utilization and costs among diabetes patients with physician, nurse practitioner (NP), or physician assistant (PA) primary care providers (PCPs).
Research Design and Methods:
Cohort study using Veterans Affairs (VA) electronic health record data to examine the relationship between PCP type and utilization and costs over 1 year in 368,481 adult, diabetes patients. Relationship between PCP type and utilization and costs in 2013 was examined with extensive adjustment for patient and facility characteristics. Emergency department and outpatient analyses used negative binomial models; hospitalizations used logistic regression. Costs were analyzed using generalized linear models.
Results:
PCPs were physicians, NPs, and PAs for 74.9% (n=276,009), 18.2% (n=67,120), and 6.9% (n=25,352) of patients respectively. Patients of NPs and PAs have lower odds of inpatient admission (OR for NP vs. physician 0.90, 95% CI=0.87, 0.93; PA vs. physician 0.92, 95% CI=0.87, 0.97), and lower emergency department use (0.67 visits on average for physicians, 95% CI=0.65, 0.68; 0.60 for NPs, 95% CI=0.58, 0.63; 0.59 for PAs, 95% CI=0.56, 0.63). This translates into NPs and PAs having approximately $500–700 less healthcare costs per patient per year (p<0.0001).
Conclusions:
Expanded use of NPs and PAs in the PCP role for some patients may be associated with notable cost savings. In our cohort, substituting care patterns and creating similar clinical situations in which they practice, NPs and PAs may have reduced costs of care by up to 150–190 million dollars in 2013.
INTRODUCTION
Most patients receive care for their diabetes in primary care settings 1, but estimates of primary care physician shortfalls range as high as 49,300 by 2030 2. Utilization of nurse practitioners (NPs) and physician assistants (PAs) as primary care providers (PCPs) has been proposed to address the shortage of PCPs and ensure access to primary care services 3.
In 2013, there were more than 88,000 PAs and 113,000 NPs employed in the United States 4. Almost a third of adults who report having a usual provider of healthcare have at least 1 visit with a PA or advanced practice nurse each year 5, and almost half of diabetes patients in the United States see an NP or PA for some part of their care 6. Approximately a third of primary care visits in both the Veterans Affairs (VA) healthcare system and community health centers are with NPs or PAs 7. Most evaluations to date, including our study of intermediate diabetes outcomes among the same study population examined in this paper, have shown that care outcomes are similar among physicians, NPs and PAs 8–11.
Although labor costs of NPs and PAs are less than those of physicians 12, there are concerns that NPs and PAs might practice in ways that increase other healthcare costs (e.g., greater reliance on specialty, hospital or emergency department care), thereby increasing total costs of care 13. For example, a recent survey found that nearly a quarter of physicians believe expanded use of NPs will be detrimental to efficiency and cost-effectiveness in healthcare in the United States 13.
Previous studies have generally found similar cost and care patterns among NPs, PAs, and physicians, although some have found differences in various care categories 9,14–19. Our study improves on common deficiencies of past studies, including inadequate case-mix adjustment, inaccurate provider type identification, ambiguous description of provider roles, and analysis of isolated segments of utilization and care costs, rather than total cost of care. Previously, we examined differences in patient healthcare costs and utilization in the sickest subset of the current cohort, those with comorbid complexity more than twice that of the average Medicare patient, and found significant cost savings among patients with NPs or PAs as PCPs 19. It has not yet been examined, however, if such cost savings generalize to a comparatively healthier population with less propensity for regular use of acute care. The aim of our study is to examine whether there are differences in total costs or in utilization of service types by whether a patient’s primary care provider is a physician, NP, or PA in a broad cohort representative of all pharmaceutically-treated diabetic patients seen in VA primary care clinics.
METHODS
This study, approved by the Institutional Review Board of the Durham VA Medical Center, utilized nationwide administrative data originating from the VA electronic health record (VA-EHR).
Data Sources and Sample Construction
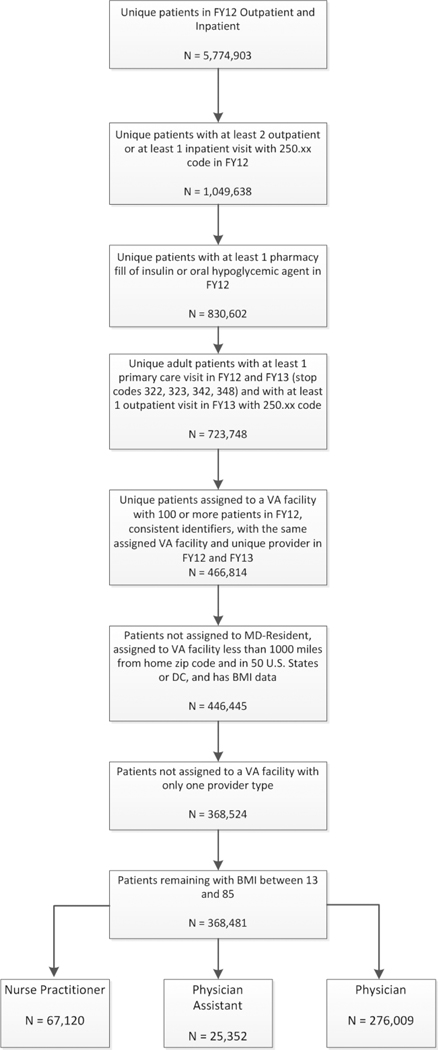
Cohort construction (Figure 1) has been previously published 10,11,19–21. In brief, this study included adult pharmaceutically-treated diabetes patients receiving primary care from the same PCP within the VA in 2012 and 2013. To be included, patients must have had a diabetes diagnosis associated with at least two VA outpatient visits and/or at least 1 VA inpatient visit and filled a prescription for insulin and/or oral hyperglycemic agents in FY 2012. Individuals also had 1 or more VA primary care visit in FY 2012 and an outpatient visit with a diabetes diagnosis in FY 2013.
Figure 1.
Cohort Construction
The VA facility most frequently visited for primary care in FY 2012 was considered the patient’s “home” facility, and facilities were retained in the sample if they had at least two professions of PCPs practicing and treated at least 100 eligible diabetic patients. The provider most visited within the home facility was considered the patient’s PCP, and we retained only patients with consistent PCP assignment from FY 2012 to 2013, using the same rules for PCP assignment in FY 2013.
Provider Type/Profession
The exposure of interest was the profession of the patient’s PCP (i.e., physician, NP, or PA), determined based on the provider’s profession code in administrative data.
Outcomes
We examined the association between provider type and the following health care utilization outcomes, determined a priori and occurring in FY 2013: 1) any VA-purchased or provided inpatient hospitalization; 2) number of days with VA-purchased or provided emergency department (ED) visits; 3) VA primary care visits; 4) VA endocrinology visits; 5) VA non-endocrinology specialty care visits. Cost outcomes, also determined a priori, included VA-provided and VA-purchased inpatient, outpatient, pharmacy, and total healthcare expenditures. We took a VA-payer perspective and included the cost of all care either provided by or paid for by VA. Post-hoc, we examined inpatient visits and emergency department visits attributed to ambulatory care sensitive conditions (ACSC), as defined by AHRQ22, to better understand how the nature of inpatient visits may differ by provider type. As a sensitivity analysis to ensure adequate exposure to one’s primary provider, we examined these outcomes on the subgroup of patients who had at least two visits to their assigned PCP. As a secondary analysis, we examined outcomes among the subgroup of diabetic patients managing 3 or more chronic conditions 23.
Utilization outcomes were compiled from Medical SAS datasets that summarize care provided by VA and fee-basis files with information on care paid for by VA but occurring outside the VA healthcare system. Type/location of outpatient care are based on VA clinic stop codes. Non-ED outpatient utilization included only VA-provided care; both VA-provided and VA-paid ED visits were combined to include emergency care.
Outpatient expenditures were calculated from the VA Health Economics Resource Center (HERC) Outpatient Average Cost Data,24 which assigns expenditures based on type of clinic and procedure codes, and fee basis files that contain expenditures for all VA-purchased care incurred in non-VA facilities. Similarly, inpatient expenditures were calculated from the HERC Inpatient Average Cost Data, which calculates expenditures per admission based on age, gender, discharge disposition, bed section, length of stay, and Medicare diagnostic-related group weights, as well as fee basis files, which include all VA-purchased inpatient care in non-VA facilities. Pharmaceutical expenditures were calculated from the Managerial Cost Accounting (MCA) System National Data Extracts Pharmacy file and include the cost of all drugs dispensed by the VA. Total expenditures summed inpatient, outpatient (including emergency department), and pharmacy expenditures.
Statistical Analysis
All statistical analyses used SAS version 9.4 (SAS Institute Inc., Cary, NC). The association between provider type and utilization and cost outcomes were examined via multivariable regression techniques described below. Each model had the same patient- and facility-level covariates, which included demographic characteristics, social complexity measures, health status, access to services, and primary care facility characteristics, as shown in Table 1. All covariates were centered such that the estimates can be interpreted as the effect of provider type holding other covariates constant at their mean values. All patient-level variables were obtained from VA-EHR data from FY-2012.
Table 1:
Characteristics of VA Patients with Diabetes by Primary Care Provider1 Type Assigned In Cost and Utilization Sample
| Category | Nurse Practitioner n=67,120 | Physician Assistant n=25,352 | Physician n=276,009 | Total n=368,481 |
|---|---|---|---|---|
| PATIENT-LEVEL FACTORS | ||||
| Male N (%) | 63739 ( 95.0) | 24636 ( 97.2) | 267828 ( 97.0) | 356203 ( 96.7) |
| Age Mean (SD) | 65.2(10.2) | 65.5(10.1) | 65.2(10.0) | 65.2(10.0) |
| Age Group N (%) | ||||
| Less Than 40 | 718 ( 1.1) | 256 ( 1.0) | 2486 ( 0.9) | 3460 ( 0.9) |
| 40 to Less Than 65 | 34108 ( 50.8) | 12628 ( 49.8) | 141839 ( 51.4) | 188575 ( 51.2) |
| 65 to Less Than 80 | 25867 ( 38.5) | 9989 ( 39.4) | 106050 ( 38.4) | 141906 ( 38.5) |
| 80 and Over | 6427 ( 9.6) | 2479 ( 9.8) | 25634 ( 9.3) | 34540 ( 9.4) |
| Race N (%) | ||||
| White | 48530 ( 72.3) | 18939 ( 74.7) | 192958 ( 69.9) | 260427 ( 70.7) |
| Black | 11673 ( 17.4) | 3934 ( 15.5) | 53694 ( 19.5) | 69301 ( 18.8) |
| Native Hawaiian | 605 ( 0.9) | 228 ( 0.9) | 3184 ( 1.2) | 4017 ( 1.1) |
| American Indian | 472 ( 0.7) | 193 ( 0.8) | 1927 ( 0.7) | 2592 ( 0.7) |
| Asian | 290 ( 0.4) | 77 ( 0.3) | 1552 ( 0.6) | 1919 ( 0.5) |
| Unknown or Missing | 5550 ( 8.3) | 1981 ( 7.8) | 22694 ( 8.2) | 30225 ( 8.2) |
| Hispanic N (%) | 2556 ( 3.8) | 913 ( 3.6) | 13247 ( 4.8) | 16716 ( 4.5) |
| Marital Status N (%) | ||||
| Currently Married | 39781 ( 59.3) | 15630 ( 61.7) | 164741 ( 59.7) | 220152 ( 59.7) |
| Previously Married | 19468 ( 29.0) | 7173 ( 28.3) | 79935 ( 29.0) | 106576 ( 28.9) |
| Never Married | 7651 ( 11.4) | 2493 ( 9.8) | 30540 ( 11.1) | 40684 ( 11.0) |
| Unknown Marital Status | 220 ( 0.3) | 56 ( 0.2) | 793 ( 0.3) | 1069 ( 0.3) |
| Homeless at Any Time During Year N (%) | 1248 ( 1.9) | 365 ( 1.4) | 5065 ( 1.8) | 6678 ( 1.8) |
| Copay Status N (%) | ||||
| No Copay Due to Disability | 35091 ( 52.3) | 13341 ( 52.6) | 152246 ( 55.2) | 200678 ( 54.5) |
| No Copay Due to Low Income | 17847 ( 26.6) | 6568 ( 25.9) | 72570 ( 26.3) | 96985 ( 26.3) |
| Must Pay Copay | 13031 ( 19.4) | 5105 ( 20.1) | 47447 ( 17.2) | 65583 ( 17.8) |
| Copay Status Unknown | 1151 ( 1.7) | 338 ( 1.3) | 3746 ( 1.4) | 5235 ( 1.4) |
| Mental Health Diagnoses N (%) | ||||
| Mood Disorder | 2857 ( 4.3) | 1013 ( 4.0) | 12715 ( 4.6) | 16585 ( 4.5) |
| Post-Traumatic Stress Disorder | 9365 ( 14.0) | 3410 ( 13.5) | 39732 ( 14.4) | 52507 ( 14.2) |
| Dementia | 1826 ( 2.7) | 736 ( 2.9) | 8712 ( 3.2) | 11274 ( 3.1) |
| Substance Abuse | 5268 ( 7.8) | 1656 ( 6.5) | 21453 ( 7.8) | 28377 ( 7.7) |
| Other Mental Health Diagnosis | 10917 ( 16.3) | 3903 ( 15.4) | 44696 ( 16.2) | 59516 ( 16.2) |
| DCG Risk Score Mean (SD) | 0.9(1.2) | 0.9(1.2) | 1.0(1.4) | 1.0(1.3) |
| Diagnostic Cost Group (DCG) Score Category N (%) | ||||
| Less Than or Equal to 0.5 | 34768 ( 51.8) | 13464 ( 53.1) | 136895 ( 49.6) | 185127 ( 50.2) |
| Greater Than 0.5 to 1 | 11693 ( 17.4) | 4143 ( 16.3) | 46508 ( 16.9) | 62344 ( 16.9) |
| Greater Than 1 to 1.5 | 8648 ( 12.9) | 3205 ( 12.6) | 35701 ( 12.9) | 47554 ( 12.9) |
| Greater Than 1.5 to 2 | 4431 ( 6.6) | 1725 ( 6.8) | 20064 ( 7.3) | 26220 ( 7.1) |
| Greater Than 2 | 7580 ( 11.3) | 2815 ( 11.1) | 36841 ( 13.3) | 47236 ( 12.8) |
| Distance to Assigned Facility Mean (SD) | 19.2(35.1) | 21.2(39.0) | 20.3(39.1) | 20.2(38.4) |
| Distance from VHA Primary Care Clinic N (%) | ||||
| Less Than 5 Miles | 17008 ( 25.3) | 6049 ( 23.9) | 62535 ( 22.7) | 85592 ( 23.2) |
| 5 to Less Than 25 Miles | 33650 ( 50.1) | 12320 ( 48.6) | 143986 ( 52.2) | 189956 ( 51.6) |
| 25 to Less Than 50 Miles | 10873 ( 16.2) | 4752 ( 18.7) | 45931 ( 16.6) | 61556 ( 16.7) |
| 50 Miles and Over | 4830 ( 7.2) | 2088 ( 8.2) | 21752 ( 7.9) | 28670 ( 7.8) |
| Missing | 759 ( 1.1) | 143 ( 0.6) | 1805 ( 0.7) | 2707 ( 0.7) |
| Body Mass Index (BMI) Category N (%) | ||||
| 13 to Less Than 18.5 | 126 ( 0.2) | 43 ( 0.2) | 653 ( 0.2) | 822 ( 0.2) |
| 18.5 to Less Than 25 | 6020 ( 9.0) | 2202 ( 8.7) | 25742 ( 9.3) | 33964 ( 9.2) |
| 25 to Less Than 30 | 19517 ( 29.1) | 7406 ( 29.2) | 80879 ( 29.3) | 107802 ( 29.3) |
| 30 to Less Than 35 | 21329 ( 31.8) | 8124 ( 32.0) | 86356 ( 31.3) | 115809 ( 31.4) |
| 35 to Less Than 40 | 12085 ( 18.0) | 4535 ( 17.9) | 49845 ( 18.1) | 66465 ( 18.0) |
| 40 to 85 | 8043 ( 12.0) | 3042 ( 12.0) | 32534 ( 11.8) | 43619 ( 11.8) |
| Baseline Body Mass Index (BMI) Mean (SD) | 32.5(6.4) | 32.5(6.4) | 32.4(6.5) | 32.5(6.5) |
| Baseline HgBA1C Mean (SD) | 7.6(1.5) | 7.6(1.4) | 7.6(1.5) | 7.6(1.5) |
| Baseline Systolic Blood Pressure Mean (SD) | 132.9(13.0) | 132.8(12.9) | 133.1(13.2) | 133.1(13.2) |
| Baseline LDL Cholesterol Mean (SD) | 87.2(29.9) | 87.0(29.7) | 85.8(29.6) | 86.1(29.6) |
| % Visits PCP Seen Mean (SD) | 77.0(25.1) | 77.9(24.7) | 75.3(25.8) | 75.8(25.6) |
| More Than 1 Visit with Assigned PCP N (%) | 54220 ( 80.8) | 20791 ( 82.0) | 215247 ( 78.0) | 290258 ( 78.8) |
| 3 or More Chronic Conditions N (%) | 56089 ( 83.6) | 20996 ( 82.8) | 232168 ( 84.1) | 309253 ( 83.9) |
| FACILITY-LEVEL FACTORS | ||||
| Endocrinology Referral Capacity2 N (%) | 27788 ( 41.4) | 11110 ( 43.8) | 152237 ( 55.2) | 191135 ( 51.9) |
| Rural Urban Commuting Area Status N (%) | ||||
| Metropolitan Area Core | 50114 ( 74.7) | 17040 ( 67.2) | 214034 ( 77.5) | 281188 ( 76.3) |
| Metropolitan Area Core - Remaining Levels | 5692 ( 8.5) | 4158 ( 16.4) | 33704 ( 12.2) | 43554 ( 11.8) |
| Micropolitan Area Core | 8232 ( 12.3) | 3332 ( 13.1) | 21494 ( 7.8) | 33058 ( 9.0) |
| Small Town or Rural | 3082 ( 4.6) | 822 ( 3.2) | 6777 ( 2.5) | 10681 ( 2.9) |
| STATE-LEVEL FACTORS | ||||
| Region N (%) | ||||
| South | 19260 ( 28.7) | 9631 ( 38.0) | 122345 ( 44.3) | 151236 ( 41.0) |
| Midwest | 18805 ( 28.0) | 6792 ( 26.8) | 65784 ( 23.8) | 91381 ( 24.8) |
| Northeast | 14814 ( 22.1) | 5810 ( 22.9) | 40896 ( 14.8) | 61520 ( 16.7) |
| West | 14241 ( 21.2) | 3119 ( 12.3) | 46984 ( 17.0) | 64344 ( 17.5) |
Data for patient-level variables are from the Veterans Administration electronic health record files. Other data sources are described in the Methods section.
Primary care provider (PCP) is assigned as the physician, NP, or PA seen most during FY 2012 and 2013.
Endocrinology referral capacity is defined as either present (endocrinology or other diabetes mellitus specialty clinics provided 500 or more visits to cohort patients in FY12) or absent (fewer than 500 visits to cohort patients).
Demographic characteristics included: gender; age; race; and ethnicity. Social complexity measures included: marital status; homelessness and, mental health diagnoses. Body Mass Index (BMI) was calculated based on height and weight information in the VA-EHR. Global health status was estimated using the prospective diagnostic cost group [DCG] score calculated by the VA, a validated measure of medical complexity in the VA population. 25,26 DCG is normed so that the average Medicare patient has a score equal to 1.27 Access measures included patient-level covariates, co-pay status and travel distance to the VA, and facility-level covariates: availability of specialized diabetes services at the VA; rurality of the VA based on the ZIP code version of the Rural Urban Community Area codes;28 and region of the United States. To account for potential differences in continuity of care, we also included a variable representing the proportion of visits to the patient’s assigned PCP. Since our previous work found that PCP assignment was not associated with state scope of practice regulations, we did not include a variable for scope of practice.20
Logistic regression models, fit using generalized estimating equations (GEEs) with empirical sandwich standard errors and exchangeable working correlation to account for provider-level clustering, were fit to a dichotomous indicators of hospitalization, ACSC-related hospitalization, and ACSC-related ED visits during FY 2013. For each count utilization outcome, we assessed whether a Poisson or negative binomial regression model provided better fit and whether a zero-inflated model was warranted using Akaike Information Criterion (AIC). For VA endocrinology visits, a marginalized zero-inflated negative binomial model with a provider-level random effect was utilized29,30 via SAS PROC NLMIXED; for all others, a standard negative binomial regression was fit via GEEs with empirical sandwich standard errors and exchangeable working correlation to account for provider-level clustering (SAS PROC GENMOD).
Similarly, for the health care expenditure outcomes, we assessed the proportion of zero values to determine whether a 2-part model may be needed31. Inpatient expenditures contained a large proportion of zero values and were therefore examined using a marginalized 2-part model with a log-skew-normal distribution and provider-level random effect 32–34, which provided the best fit as determined by AIC. Outpatient, pharmacy, and total expenditures were fit using generalized linear models. After specification testing35, each were fit using a log link with variance proportional to the standard deviation. Models were fit using GEEs, and empirical sandwich standard errors coupled with an exchangeable working correlation to account for provider-level clustering and potential overdispersion (using SAS PROC GENMOD).
To interpret model results, we set a priori thresholds for clinical significance of model-estimated differences at 0.3% for probability of inpatient admission and ACSC ED visit, 5% for number of ED visits, and 10% for each outpatient utilization type. Any difference in per-person annual health care costs was considered meaningful a priori due to the potential cumulative effect to the healthcare system.
RESULTS
The sample included 368,481 patients from 568 VA facilities. PCPs were physicians, NPs, and PAs for 74.9% (n=276,009), 18.2% (n=67,120), and 6.9% (n=25,352) of patients respectively, and patients saw their identified PCP on 75.8% of their primary care visits. The majority of patients (78.8%) had at least two visits to their assigned PCP (n=290,258).
Patient characteristics (Table 1) were similar across PCP profession, with NPs slightly more likely to see female patients and physicians slightly more likely to see black patients. Notably, DCG scores did not differ by provider type. Larger differences were seen in facility and regional characteristics (Table 1). Physician PCPs were more common in facilities with endocrine referral capacities, in core metropolitan areas, and in the South. NP and PA PCPs were more prevalent in the Northeast.
Table 2 presents covariate-adjusted model estimated proportions and counts of each type of utilization per patient by PCP type, and Table 3 presents estimated odds ratios (ORs) and incidence density ratios (IDRs). Patients of NPs and PAs were less likely than those of physicians to incur a hospitalization (NP vs. physician OR=0.90, 95% CI=0.87–0.93; PA vs. physician OR=0.92, 95% CI=0.87–0.97), while no difference was seen between NPs and PAs. Specifically, an estimated 12.7% of physician patients (95% CI=12.5–12.9), 11.5% of NP patients (95% CI=11.2–11.9), and 11.7% of PA patients (95% CI=11.2–12.3) incurred hospitalizations in FY 2013. Patients of NPs and PAs were less likely than those of physicians to incur an ACSC-related hospitalization as well (NP vs. physician OR=0.90, 95% CI=0.86–0.94; PA vs. physician OR=0.91, 95% CI=0.86–0.97), and again no difference was observed between NPs and PAs. 12.2% of inpatient admissions were ACSC-related; ACSC-related hospitalizations were experienced by an estimated 11.1% of physician patients (95% CI=10.9–11.3), 10.2% of NP patients (95% CI=9.8–10.5), and 10.2% of PA patients (95% CI=9.7–10.8). Patients of physicians also visited the ED more frequently in the year (0.67 visits on average for physicians, 95% CI=0.65–0.68; 0.60 for NPs, 95% CI=0.58–0.63; 0.59 for PAs, 95% CI=0.56– 0.63). Fewer than 1.5% of patients incurred ACSC-related ED visits, regardless of provider type, and differences among provider type were less notable. No clinically meaningful differences were observed for number of primary care visits, endocrinology or non-endocrinology specialty visits.
Table 2.
Covariate-adjusted model estimated proportions or counts of utilization per patient by PCP type in FY 2013
| Outcome | Nurse Practitioners | Physician Assistants | Physicians |
|---|---|---|---|
| Estimated Proportion with… (95% Confidence Interval) | |||
| Any inpatient visit | 0.115 (0.112, 0.119) | 0.117 (0.112, 0.123) | 0.127 (0.125, 0.129) |
| Any ambulatory care sensitive condition inpatient visit | 0.102 (0.097, 0.105) | 0.102 (0.097, 0.108) | 0.111 (0.109, 0.113) |
| Any ambulatory care sensitive condition emergency department visit | 0.012 (0.011, 0.013) | 0.012 (0.010, 0.014) | 0.013 (0.013, 0.014) |
| Estimated Mean Number of Days with… (95% Confidence Interval) | |||
| An emergency department visit | 0.60 (0.58, 0.63) | 0.59 (0.56, 0.63) | 0.67 (0.65, 0.68) |
| A VA primary care visit | 3.10 (3.04, 3.15) | 3.27 (3.17, 3.37) | 2.93 (2.90, 2.96) |
| A VA non-endocrinology specialty care visit | 2.25 (2.18, 2.31) | 2.15 (2.05, 2.25) | 2.27 (2.24, 2.30) |
| A VA endocrinology visit | 0.25 (0.24, 0.25) | 0.26 (0.23, 0.28) | 0.26 (0.25, 0.28) |
Table 3.
Covariate-adjusted model estimated differences in FY 2013 patient utilization by PCP type.
| Outcome | Nurse Practitioners vs. Physicians | Physician Assistants vs. Physicians | Nurse Practitioners vs. Physician Assistants |
|---|---|---|---|
| Estimated Odds Ratio (95% Confidence Interval) | |||
| Any inpatient visit | 0.90 (0.87, 0.93) | 0.92 (0.87, 0.97) | 0.98 (0.92, 1.04) |
| Any ambulatory care sensitive condition inpatient visit | 0.90 (0.86, 0.94) | 0.91 (0.86, 0.97) | 0.99 (0.92, 1.06) |
| Any ambulatory care sensitive condition emergency department visit | 0.91 (0.83, 0.99) | 0.90 (0.78, 1.04) | 1.01 (0.86, 1.18) |
| Estimated Incidence Density Ratio (95% Confidence Interval) | |||
| Days with emergency department visits | 0.91 (0.87, 0.94) | 0.89 (0.84, 0.94) | 1.02 (0.96, 1.09) |
| Days with VA primary care visits | 1.06 (1.04, 1.08) | 1.12 (1.08, 1.15) | 0.95 (0.91, 0.98) |
| Days with VA non-endocrinology specialty care visits | 0.99 (0.96, 1.02) | 0.95 (0.90, 0.995) | 1.04 (0.99, 1.10) |
| Days with VA endocrinology visits | 1.07 (1.00, 1.13) | 1.04 (0.94, 1.14) | 1.02 (0.92, 1.01) |
Table 4 presents covariate-adjusted model-estimated annual per-patient medical expenditures in FY 2013 by PCP type, as well as the mean ratio of expenditures for comparison across provider types. Patients of physicians incurred greater inpatient, outpatient, pharmacy, and total overall expenditures compared to patients of NPs or PAs, while patients of NPs vs. PAs had nearly identical mean per-patient expenditures in all categories. Specifically, patients of NPs and PAs incurred 8% (95% CI=4%−11%) and 11% (95% CI=6%−16%), respectively, lower inpatient expenditures than patients of physicians, translating to a mean per-patient annual difference of $264 and $370, respectively, in inpatient expenditures. Of slightly less magnitude, patients of PAs and NPs incurred 5–6% lower annual per-patient pharmacy expenditures than physicians (NPs 95% CI=3%−9%; PAs 95% CI=2%−9%) than patients of physicians, translating to a mean per-patient annual difference of approximately $100 in pharmaceutical expenditures. Smaller differences were seen in outpatient expenditures by provider type: patients of NPs incurred 3% lower outpatient expenditures in the year (95% CI=1%−4%) and patients of PAs incurred 4% lower outpatient expenditures (95% CI=1%−7%) compared to patients of physicians. The cumulative effect led to a reduction in total per-patient healthcare expenditures for patients of NPs and PAs compared to those of physicians. Overall, patients of NPs incurred 5% lower expenditures compared to those of physicians (95% CI=3%−7%), while patients of PAs incurred 6% lower (95% CI=3%−9%). This translated to a difference of $563 and $696 in per-patient annual total health care expenditures, respectively.
Table 4.
Covariate adjusted model estimated annual per-patient medical expenditures in FY 2013 by PCP type and percentage difference by PCP type.
| Outcome | Nurse Practitioners | Physician Assistants | Physicians |
|---|---|---|---|
| Estimated Annual Expenditures | |||
| Inpatient | $3209 (3098, 3321) | $3103 (2934, 3272) | $3473 (3408, 3537) |
| Outpatient | $6451 (6348, 6556) | $6367 (6192, 6548) | $6623 (6567, 6680) |
| Pharmacy | $1740 (1698, 1783) | $1757 (1699, 1817) | $1853 (1827, 1878) |
| Total Overall | $11,224 (11013, 11440) | $11,091 (10766, 11426) | $11,787 (11673, 11903) |
| Estimated Mean Ratio for Difference in Expenditures (95% Confidence Interval) | |||
| Nurse Practitioners vs. Physicians | Physician Assistants vs. Physicians | Nurse Practitioners vs. Physician Assistants | |
| Inpatient | 0.92 (0.89, 0.96) | 0.89 (0.84, 0.94) | 1.03 (0.97, 1.10) |
| Outpatient | 0.97 (0.96, 0.99) | 0.96 (0.93, 0.99) | 1.01 (0.98, 1.05) |
| Pharmacy | 0.94 (0.91, 0.97) | 0.95 (0.91, 0.98) | 0.99 (0.95, 1.03) |
| Total Overall | 0.95 (0.93, 0.97) | 0.94 (0.91, 0.97) | 1.01 (0.98, 1.05) |
In the sensitivity analysis among patients with at least 2 visits in FY 12 to their assigned PCP, overall utilization and costs were slightly higher for all provider types (Appendix Tables 1–3); the relative differences among providers were essentially unchanged.
Multiple Chronic Conditions Subgroup Analysis
The subsample with 3 or more chronic conditions included 309,256 patients, or 83.9% of the original sample, reflecting the complex comorbidity burden facing this population. Mean per-patient expenditures were slightly higher compared to the overall sample, but relative differences in all outcomes were consistent with the main analysis.
DISCUSSION
Our results found meaningfully higher total care costs for patients with physician PCPs, driven by higher hospitalizations, although ED visits and pharmacy costs also contributed. Limitations withstanding, projecting $540-$694 lower yearly expenditures for patients of PAs and NPs to the 276,009 patients in our sample cared for by physicians, substituting care patterns and productivity expectations used by VA NPs and PAs could have reduced costs of care for primary care patients with diabetes by 150–190 million dollars in 2013.
Our findings are consistent with other research showing similar or lower resource use by NPs/PAs, compared to physicians, or when NPs and/or PAs are included in the care team 15,17,19,36–38, and suggests our previous work generalizes more broadly into primary care practices 19. Because we analyzed total cost of care in a population of all pharmaceutically-treated diabetic patients, our results directly address the long-standing question of whether care by NPs and PAs, who are less expensive to employ than physicians, might cost health systems more in the long run due to resource use in excess of that of physicians in other categories of costs (i.e., office visits, laboratory services, prescription medications, referrals, ED use, hospital admissions). In fact, in our study they cost the health system considerably less, even before accounting for their lower salaries.
Our study was not designed to provide insight into the reasons for more ED visits and hospitalizations in patients with physician PCPs, but we can suggest some possible causes based on existing literature. It is possible that the greater use of primary care visits by PA and NP patients may have helped to avoid costly ED and inpatient use, although the difference for NPs, at 6% more visits than physicians, did not meet our a priori clinical significance level of 10%. Physicians in VA primary care manage panels that are about 15% larger than those of NPs and PAs 17, and this might explain why physician patients had fewer office visits per year than NP and PA patients. Some past research has found that clinicians with higher patient loads had more emergent visits 39, but this finding has been inconsistent 40. It is possible that lower patient loads might make it easier for patients to reach their PCP and have a discussion about whether an ED visit is necessary. It is also possible that patients of physicians used more acute services and experienced higher total costs than patients of NPs and PAs because they are sicker in some way that our extensive statistical adjustment for medical and social complexity did not account for.
A strength of our study is that it can be interpreted with reference to our previous work on the same cohort, in which we found relatively minor differences in characteristics of patients across provider types 20 and no clinically-meaningful differences in adjusted intermediate quality of care outcomes 10. Our work on a smaller and more medically complex cohort found similar results on care quality, health resource utilization, and total costs of care 19. Another strength is that the VA’s well-developed electronic health record system supports extensive adjustment for case-mix differences as well as accurate identification of provider type, a feature not found in many commonly-used data sources, where work of NPs and PAs is often obscured behind incident-to billing practices or distorted due to physician–centric sampling strategies.41
Past comparative effectiveness research on care costs has often been limited by inadequate descriptions of the context of care, so that it is difficult to discern the actual role of the NPs or PAs 18. In contrast, the VA PACT model of care is well-described and the role of NPs and PAs is clearly identifiable as that of a PCP, rather than as a supplement to physician care 42. Therefore, the NPs and PAs that we studied are working in a relatively uniform care model in a PCP role that is comparable to their physician counterparts. Other strengths of our study include its nationwide scope and large sample size. Our study is the first to report on total cost of care for primary care patients of PAs.
Despite study strengths, there are limitations and considerations. Our study examined costs from the VA payer perspective, so it is possible that we missed some utilization and costs paid by patients or other insurers. There is little reason to suspect that this non-VA payer use varies by provider type after adjusting for facility-level variations, such as rurality and access measures. Our patient population is predominantly male and has more social, economic, and health challenges compared to the general US population. However, it is reasonable to suppose that NP and PA care for less complex patients would be at least as efficient as it is for complex veterans. VA is an integrated system with salaried employees, so it is possible that patterns may be different in fee for service and non-integrated settings. However, wider use of population-based health management and related incentives (e.g., accountable care organizations) extends the generalizability of findings. Our study does not account for the time that physicians spend consulting with NPs and PAs. Data from other sources, however, suggests that the time spent consulting is minimal 43. Since our study did not include savings that the VA accrues due to lower salaries of NPs and PAs (considering their lower patient loads), we may present an underestimate of the net financial benefits to VA of using PAs and NPs. However, we also did not account for per-patient labor costs and provider panel size, which differs by provider profession. Additionally, length of follow-up was modest at 1 year, and we did not examine long-term effects of practice patterns. We also analyzed only patients with a consistent PCP over two years, and thus our results may not generalize to patients with more fragmented primary care. Finally, although we controlled for many potential patient- and facility-level confounders, we lacked access to many provider-level characteristics, such as overall panel size and time spent in clinic. The observational nature of this study may not account for unmeasured confounders in practice pressures, performance expectations or patient populations between physicians, NPs and PAs.
We found that use of NPs and PAs as primary care providers for veterans with diabetes was associated with lower odds of all cause and ambulatory care sensitive hospital admission, fewer emergency department visits, and lower total costs of care over a 1 year period. Our previous analyses found equivalent intermediate clinical outcomes for patients of NPs, PAs, and physicians. Combined, these findings suggest that expanded use of NPs and PAs in the primary care role may be able to yield substantial cost savings while maintaining quality of care 10,11.
Supplementary Material
Acknowledgments:
This study was funded/sponsored by the Health Services Research & Development (HSR&D) Service of the United States Department of Veterans Affairs (IIR 13-063). The work was supported by the Center of Innovation for Health Services Research in Primary Care (CIN 13-410) at the Durham Veterans Affairs Medical Center. No authors report conflicts of interest. The views expressed in this article are those of the authors and do not reflect the position or policy of the Department of Veterans Affairs, United States government, or Duke University. Drs. Jackson and Smith take responsibility for study design, access to data, and publication.
REFERENCES
- 1.Rothman AA, Wagner EH. Chronic illness management: what is the role of primary care? Ann Intern Med. 2003;138(3):256–261. [DOI] [PubMed] [Google Scholar]
- 2.Association of American Medical Colleges. 2018 Update: The Complexities of Physician Supply and Demand: Projections from 2014 to 2025. 2018; https://aamc-black.global.ssl.fastly.net/production/media/filer_public/85/d7/85d7b689-f417-4ef0-97fb-ecc129836829/aamc_2018_workforce_projections_update_april_11_2018.pdf.
- 3.Auerbach DI, Chen PG, Friedberg MW, et al. Nurse-Managed Health Centers And Patient-Centered Medical Homes Could Mitigate Expected Primary Care Physician Shortage. Health Affairs. 2013;32(11):1933–1941. [DOI] [PubMed] [Google Scholar]
- 4.Hooker RS, Brock DM, Cook ML. Characteristics of nurse practitioners and physician assistants in the United States. Journal of the American Association of Nurse Practitioners. 2016;28(1):39–46. [DOI] [PubMed] [Google Scholar]
- 5.Everett CM, Morgan P, Jackson GL. Primary care physician assistant and advance practice nurses roles: Patient healthcare utilization, unmet need, and satisfaction. Healthcare. 2016;4(4):327–333. [DOI] [PubMed] [Google Scholar]
- 6.Druss BG, Marcus SC, Olfson M, Tanielian T, Pincus HA. Trends in care by nonphysician clinicians in the United States. N Engl J Med. 2003;348(2):130–137. [DOI] [PubMed] [Google Scholar]
- 7.Morgan PA, Abbott DH, McNeil RB, Fisher DA. Characteristics of primary care office visits to nurse practitioners, physician assistants and physicians in United States Veterans Health Administration facilities, 2005 to 2010: a retrospective cross-sectional analysis. Hum Resour Health. 2012;10(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang Y, Long Q, Jackson SL, et al. Nurse Practitioners, Physician Assistants, and Physicians Are Comparable in Managing the First Five Years of Diabetes. Am J Med. 2018;131(3):276–283.e272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 2018;7:CD001271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jackson GL, Smith VA, Edelman D, et al. Intermediate Diabetes Outcomes in Patients Managed by Physicians, Nurse Practitioners, or Physician Assistants: A Cohort Study. Ann Intern Med. 2018;169(12):825–835. [DOI] [PubMed] [Google Scholar]
- 11.Everett CM, Morgan P, Smith VA, et al. Primary care provider type: Are there differences in patients’ intermediate diabetes outcomes? JAAPA. 2019;32(6):36–42. [DOI] [PubMed] [Google Scholar]
- 12.Roblin DW, Howard DH, Becker ER, Kathleen Adams E, Roberts MH. Use of midlevel practitioners to achieve labor cost savings in the primary care practice of an MCO. Health Serv Res. 2004;39(3):607–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donelan K, DesRoches CM, Dittus RS, Buerhaus P. Perspectives of physicians and nurse practitioners on primary care practice. N Engl J Med. 2013;368(20):1898–1906. [DOI] [PubMed] [Google Scholar]
- 14.Martin-Misener R, Harbman P, Donald F, et al. Cost-effectiveness of nurse practitioners in primary and specialised ambulatory care: systematic review. BMJ Open. 2015;5(6):e007167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu H, Robbins M, Mehrotra A, et al. The Impact of Using Mid-level Providers in Face-to-Face Primary Care on Health Care Utilization. Med Care. 2017;55(1):12–18. [DOI] [PubMed] [Google Scholar]
- 16.Kurtzman ET, Barnow BS. A Comparison of Nurse Practitioners, Physician Assistants, and Primary Care Physicians’ Patterns of Practice and Quality of Care in Health Centers. Med Care. 2017;55(6):615–622. [DOI] [PubMed] [Google Scholar]
- 17.Virani SS, Akeroyd JM, Ramsey DJ, et al. Health Care Resource Utilization for Outpatient Cardiovascular Disease and Diabetes Care Delivery Among Advanced Practice Providers and Physician Providers in Primary Care. Population health management. 2018;21(3):209–216. [DOI] [PubMed] [Google Scholar]
- 18.Martinez-Gonzalez NA, Rosemann T, Djalali S, Huber-Geismann F, Tandjung R. Task-Shifting From Physicians to Nurses in Primary Care and its Impact on Resource Utilization: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Med Care Res Rev. 2015;72(4):395–418. [DOI] [PubMed] [Google Scholar]
- 19.Morgan PA, Smith VA, Berkowitz TSZ, et al. Impact Of Physicians, Nurse Practitioners, And Physician Assistants On Utilization And Costs For Complex Patients. Health Aff (Millwood). 2019;38(6):1028–1036. [DOI] [PubMed] [Google Scholar]
- 20.Morgan P, Everett CM, Smith VA, et al. Factors Associated With Having a Physician, Nurse Practitioner, or Physician Assistant as Primary Care Provider for Veterans With Diabetes Mellitus. Inquiry. 2017;54:46958017712762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Everett CM, Morgan P, Smith VA, et al. Interpersonal continuity of primary care of veterans with diabetes: a cohort study using electronic health record data. BMC family practice. 2018;19(1):132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prevention Quality Indicators Technical Specifications, Version 4.5, AHRQ. 2014; http://www.qualityindicators.ahrq.gov/Archive/PQI_TechSpec_V45.aspx, 2018.
- 23.J Yoon CA. Technical Report 33: Comparing the measurement of chronic conditions in ICD-9-CM and ICD-10-CM in VA patients, FY2014-FY2016. In. Washington D.C: Department of Veterans Affairs; 2017. [Google Scholar]
- 24.Wagner TH, Chen S, Barnett PG. Using average cost methods to estimate encounter-level costs for medical-surgical stays in the VA. Medical Care Research and Review. 2003;60(3_suppl):15S–36S. [DOI] [PubMed] [Google Scholar]
- 25.Maciejewski ML, Liu CF, Derleth A, McDonell M, Anderson S, Fihn SD. The performance of administrative and self-reported measures for risk adjustment of Veterans Affairs expenditures. Health Serv Res. 2005;40(3):887–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ellis RP, Ash A. Refinements to the Diagnostic Cost Group (DCG) model. Inquiry. 1995;32(4):418–429. [PubMed] [Google Scholar]
- 27.Ash A, Porell F, Gruenberg L, Sawitz E, Beiser A. Adjusting Medicare capitation payments using prior hospitalization data. Health Care Financ Rev. 1989;10(4):17–29. [PMC free article] [PubMed] [Google Scholar]
- 28.U.S. Department of Agriculture. 2010 Rural-Urban Commuting Area (RUCA) Codes. 2010; http://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation.aspx. Accessed August 13, 2016.
- 29.Preisser JS, Das K, Long DL, Divaris K. Marginalized zero‐inflated negative binomial regression with application to dental caries. Statistics in medicine. 2016;35(10):1722–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leann Long D, Preisser JS, Herring AH, Golin CE. A marginalized zero‐inflated Poisson regression model with random effects. Journal of the Royal Statistical Society: Series C (Applied Statistics). 2015;64(5):815–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith VA, Neelon B, Maciejewski ML, Preisser JS. Two parts are better than one: modeling marginal means of semicontinuous data. Health Services and Outcomes Research Methodology. 2017;17(3–4):198–218. [Google Scholar]
- 32.Smith VA, Preisser JS, Neelon B, Maciejewski ML. A marginalized two‐part model for semicontinuous data. Statistics in medicine. 2014;33(28):4891–4903. [DOI] [PubMed] [Google Scholar]
- 33.Smith VA, Neelon B, Preisser JS, Maciejewski ML. A marginalized two-part model for longitudinal semicontinuous data. Statistical methods in medical research. 2017;26(4):1949–1968. [DOI] [PubMed] [Google Scholar]
- 34.Smith VA, Maciejewski ML, Olsen MK. Modeling semicontinuous longitudinal expenditures: a practical guide. Health services research. 2018;53:3125–3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? Journal of health economics. 2001;20(4):461–494. [DOI] [PubMed] [Google Scholar]
- 36.Morgan PA, Shah ND, Kaufman JS, Albanese MA. Impact of physician assistant care on office visit resource use in the United States. Health Serv Res. 2008;43(5 Pt 2):1906–1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mafi JN, Wee CC, Davis RB, Landon BE. Comparing Use of Low-Value Health Care Services Among U.S. Advanced Practice Clinicians and Physicians. Ann Intern Med. 2016;165(4):237–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martinez-Gonzalez NA, Djalali S, Tandjung R, et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res. 2014;14:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lowe RA, Localio AR, Schwarz DF, et al. Association between primary care practice characteristics and emergency department use in a medicaid managed care organization. Med Care. 2005;43(8):792–800. [DOI] [PubMed] [Google Scholar]
- 40.Huntley A, Lasserson D, Wye L, et al. Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open. 2014;4(5):e004746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morgan P, Strand J, Ostbye T, Albanese M. Missing in Action: Care by physician assistants and nurse practitioners in national health surveys. Health Services Research. 2007;42(5):2022–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19(7):e263–272. [PubMed] [Google Scholar]
- 43.Fletcher CE, Copeland LA, Lowery JC, Reeves PJ. Nurse practitioners as primary care providers within the VA. Military Medicine. 2011;176(7):791–797. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.