Abstract
Purpose
The purpose of this study was to ascertain COVID-19 transmission dynamics among Latino communities nationally.
Methods
We compared predictors of COVID-19 cases and deaths between disproportionally Latino counties (≥17.8% Latino population) and all other counties through May 11, 2020. Adjusted rate ratios (aRRs) were estimated using COVID-19 cases and deaths via zero-inflated binomial regression models.
Results
COVID-19 diagnoses rates were greater in Latino counties nationally (90.9 vs. 82.0 per 100,000). In multivariable analysis, COVID-19 cases were greater in Northeastern and Midwestern Latino counties (aRR: 1.42, 95% CI: 1.11–1.84, and aRR: 1.70, 95% CI: 1.57–1.85, respectively). COVID-19 deaths were greater in Midwestern Latino counties (aRR: 1.17, 95% CI: 1.04–1.34). COVID-19 diagnoses were associated with counties with greater monolingual Spanish speakers, employment rates, heart disease deaths, less social distancing, and days since the first reported case. COVID-19 deaths were associated with household occupancy density, air pollution, employment, days since the first reported case, and age (fewer <35 yo).
Conclusions
COVID-19 risks and deaths among Latino populations differ by region. Structural factors place Latino populations and particularly monolingual Spanish speakers at elevated risk for COVID-19 acquisition.
Keywords: Latino, Hispanic, COVID-19, Disparity, Race
Introduction
The novel coronavirus disease 2019 (COVID-19) pandemic has dramatically impacted the health and well-being of millions of individuals residing in the United States (U.S.) and around the world. As of June 14, 2020, over two million people in the U.S. have been diagnosed with severe acute respiratory syndrome coronavirus [1] (SARS-CoV-2) infection and over 114,000 individuals have died from COVID-19-related complications [2]. Much of the discourse regarding disease burden has acknowledged the disparate COVID-19 diagnoses and deaths among differing populations, including ethnic and racial minorities [1,3]. This is particularly evident in the case of Latinos who comprise approximately 18% of the U.S. population in the United States and represent the nation's largest ethnic and racial minority group [4]. Latinos have been disproportionately impacted by COVID-19 [5]; as of June 8, 2020, they account for one in three (33%) of all confirmed COVID-19 cases in the United States with known ethnicity/race data, whereas half (52%) of the COVID-19 cases assessed still lacked race or ethnicity data [2]. Furthermore, Latinos have among the highest age-adjusted rates of COVID-19-associated hospitalizations at 117 per 100,000 and account for approximately one in five of all confirmed COVID-19-related deaths in the U.S. with known ethnicity/race data [6,7]. Research designed to identify the underlying drivers of SARS-CoV-2 transmission and death among the country's vast and diverse Latino populations is urgently needed.
A recent epidemiological study provided the first national assessment of the disparity in COVID-19 diagnoses and deaths among black Americans [8]. To overcome incomplete reporting of COVID-19 diagnoses and deaths by race/ethnicity, the study examined counties with a share of black Americans above the U.S. average and compared these counties to all other U.S. counties. This was shown to be a useful proxy for examining case report data and offered real-time guidance for enhancing the public health response to COVID-19 among black Americans. In the present study, we applied the same county-level approach to better understand the patterns in COVID-19 diagnoses and deaths among Latino populations nationally, including Puerto Rico. We considered the heterogeneity of the U.S. Latino population and explored whether differences in a set of core demographic variables attenuate drivers of COVID-19 diagnoses and deaths.
Methods
We assessed the differences in county-level characteristics of counties with a greater share of Latino residents than the U.S. average (≥17.8% Latino population; hereafter, disproportionately Latino counties) compared with all other counties (<17.8% Latino population). In addition, we examined the association between the proportion of Latino residents and COVID-19 cases and deaths. All data used in these analyses were from publicly available data sets. Puerto Rico was included as a single additional “county” in our analysis because Puerto Rico does not have counties as administrative units. In addition, we assessed intraregional differences based on U.S. Census statistical regions: Midwest, Northeast, South, and West [9]. Puerto Rico was excluded from the regional assessments.
Demographic data
County-level data from the U.S. Census Bureau American Community Survey 5-year [10] were collected for select demographics (county population, percentage of Latinos, percentage of the population more than the age of 65 years, percentage of the population less than the age of 35 years, percentage of the population aged less than 65 years without health insurance, occupants per room, and language spoken at home and ability to speak English). For language spoken at home, the percentages were calculated based on monolingual English, monolingual Spanish (speak Spanish at home and ability to speak English “not well” or “not at all”), and bilingual (speak Spanish at home and ability to speak English “well” or “very well”). The annual average county unemployment rates were obtained from the Bureau of Labor Statistics [11].
COVID-19 data and comorbidities
COVID-19 cases and deaths at the county-level were downloaded from USAFacts through May 11. Although more recent data were available, we chose May 11, 2020, as a cutoff date as it precedes many states' and localities' reopening of their economies, which could introduce additional bias such as increased exposure due to occupational risk or daily life activities. The rates of diagnosed diabetes among adults aged 20+ years were downloaded from the Centers for Disease Control and Prevention (CDC) Diabetes Atlas (2016) [12]. The heart disease deaths per 100,000 were accessed from CDC's Interactive Atlas of Heart Disease and Stroke for those 35 years of age and older (2016–2018) [13]. The combined rates of cerebrovascular and hypertension deaths per 100,000 were sourced from the CDC WONDER (2018) [14]. The estimates of people living with diagnosed HIV per 100,000 among adults and adolescents 13 and older were derived from the CDC ATLAS (2018) [15]. For counties with missing HIV data in Kentucky and Alaska, archived HIV data from AIDSVu.org [16] from 2015 were used, given that a state data-sharing agreement between these two states restricts the CDC from releasing comparable data.
Social/environmental data
Following Wu et al [17], we used county-level estimates of fine particulate matter (PM2.5) to assess air quality. Social distancing grades were drawn from Unacast's county measures on May 22 and were coded as A± = 1, B± = 2, C± = 3, D± = 4, and F± = 5 [18]. Higher scores were associated with poorer social distancing. The U.S. Department of Agriculture Urban–Rural Classification Scheme was used to assess urbanicity (index from 1 to 6, with 1 being the most urban) [19]. Puerto Rico was assigned an urbanicity score based on the weighted average of all municipalities.
Statistical analyses
First, we categorized counties into two groups: disproportionately Latino counties (≥17.8% of county population) and other counties (<17.8% of county population). We summarized the characteristics of counties in each group using medians and interquartile ranges. In addition, we calculated and mapped county-level COVID-19 diagnosis and death rates to assess geographic patterns for each group. Next, we analyzed the proportion of Latino residents in a county as a continuous variable and plotted the proportion of Latino residents by the rate of COVID-19 diagnoses, adjusted for days since the first infection was reported for each U.S. Census region.
To assess whether the observed associations between the proportion of Latino residents and COVID-19 cases and deaths were confounded by other factors, we conducted a multivariate analysis using Bayesian hierarchical models. We fit zero-inflated negative binomial models with logarithmic link functions separately to COVID-19 cases and deaths using integrated nested Laplace approximations.[20] All models included the proportion of the population that is Latino as a continuous variable, the county population as an offset and included a spatially structured state-level random effect.[21] We first estimated an unadjusted rate ratio for the proportion of the population that is Latino before fitting a model that only controlled for the proportion of population that is younger than 35 years. Finally, we present a fully adjusted model that includes all other county-level characteristics (see Table 1 for the characteristics) and an interaction term for the region by proportion of Latino residents to estimate the adjusted rate ratios for each region. To control for potential temporal confounding, each model also included a variable representing the number of days since the first case of COVID-19 was reported in each county. We presented the adjusted rate ratios of COVID-19 cases and deaths, comparing the observed third quartile to the observed first quartile of each variable. Rate ratios greater than one indicate that the higher levels of a given characteristic were associated with higher rates of COVID-19 cases or deaths. All analyses were performed using R 3.5.0. and Bayesian hierarchical models were fit using the INLA package (www.r-inla.org).
Table 1.
Distribution of the demographics, chronic diseases, social/environmental factors, and COVID-19 diagnoses and deaths in disproportionally Latino counties (≥17.8% of the total population) and in all other counties (<17.8% of the total population)
| Characteristic | Pct. Latinx <17.8% (n = 2700) | Pct. Latinx ≥17.8% (n = 443) |
|---|---|---|
| Demographics | ||
| Population | 25,461 (11,080, 64,100) | 29,189 (9284, 176,325) |
| % Latino | 3.3 (1.9, 6.2) | 30.9 (22.9, 47.9) |
| % black | 2.2 (0.7, 11.2) | 2.9 (0.9, 8.0) |
| % white | 91.0 (77.6, 95.5) | 82.3 (73.4, 89.3) |
| % over 65 y old | 18.3 (16.0, 21.0) | 15.3 (13.2, 18.7) |
| % under 35 y old | 42.2 (39.2, 45.1) | 47.1 (43.1, 50.9) |
| % unemployed | 4.2 (3.4, 5.4) | 4.0 (3.3, 5.0) |
| % uninsured | 10.5 (7.2, 14.5) | 16.2 (11.6, 21.3) |
| % occupancy > 1 per room | 1.7 (1.2, 2.5) | 3 .9 (2.8, 5.7) |
| % monolingual (English) | 47.9 (31.8, 66.9) | 28.2 (18.7, 37.9) |
| % monolingual (Spanish) | 8.4 (2.2, 16.5) | 15.1 (9.5, 21.5) |
| % bilingual | 39.8 (25.8, 51.4) | 55.4 (49.0, 59.9) |
| % Mexican | 0.5 (0.1, 1.2) | 6.5 (3.9, 10.5) |
| % Cuban | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.1) |
| % Dominican | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) |
| Chronic disease | ||
| % diabetes | 10.0 (7.9, 12.7) | 9.0 (6.9, 11.2) |
| Heart disease death rate | 347.0 (300.8, 408.5) | 326.4 (284.5, 376.6) |
| Cerebrovascular and hypertension death rate | 68.5 (51.5, 90.4) | 59.0 (42.9, 81.5) |
| HIV infection rate | 91.5 (39.6, 187.0) | 136.8 (64.4, 249.7) |
| Social environment | ||
| Urbanicity score | 5.0 (4.0, 6.0) | 5.0 (3.0, 6.0) |
| PM2.5 | 6.4 (4.6, 7.7) | 5.8 (4.3, 7.1) |
| Social distancing score | 4.0 (3.0, 5.0) | 4.0 (3.0, 5.0) |
| Days since first case | 46.0 (38.0, 52.0) | 46.0 (34.0, 56.0) |
| COVID-19 | ||
| COVID-19 diagnosis rate (per 100,000) | 82.0 (34.1, 198.5) | 90.9 [35.1, 262.7) |
| COVID-19 death rate (per 100,000) | 0.0 (0.0, 7.3) | 1.3 (0.0, 7.6) |
| COVID-19 death rate (cases >200, n = 566) | 13.8 (6.3, 31.5) | 9.3 (3.6, 26.2) |
PM2.5 = fine particulate matter in the air.
Results
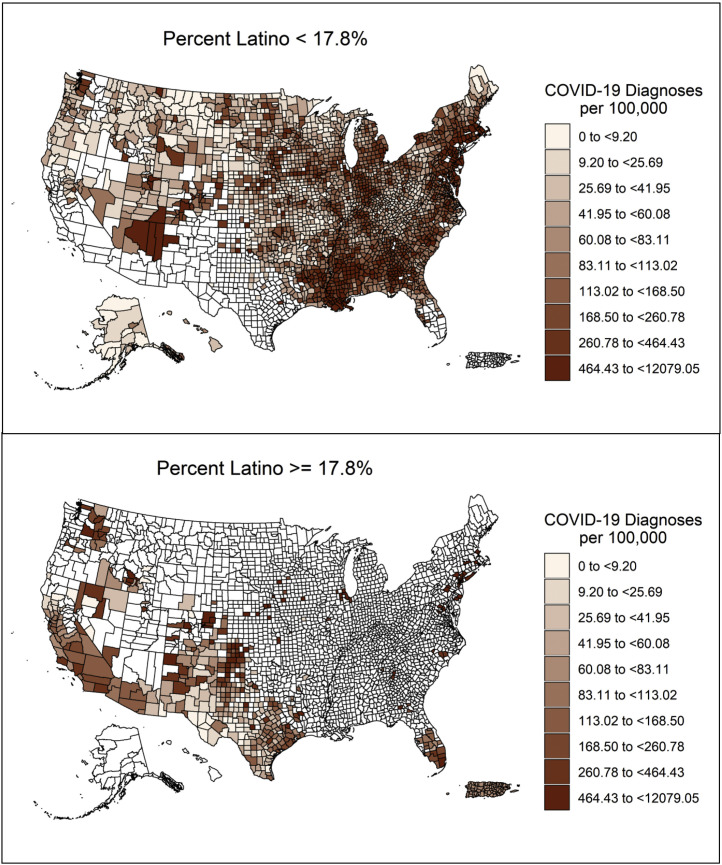
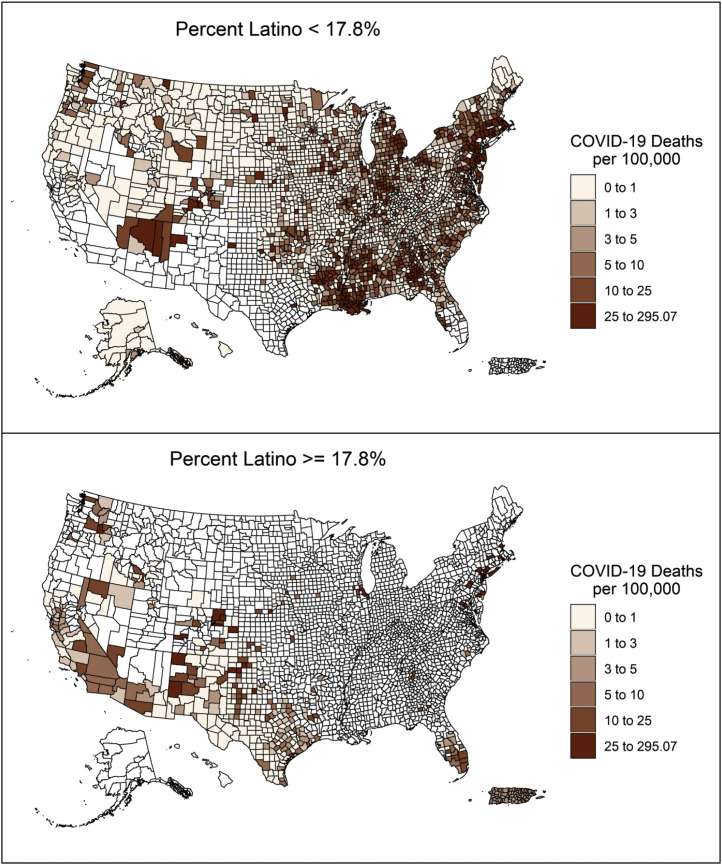
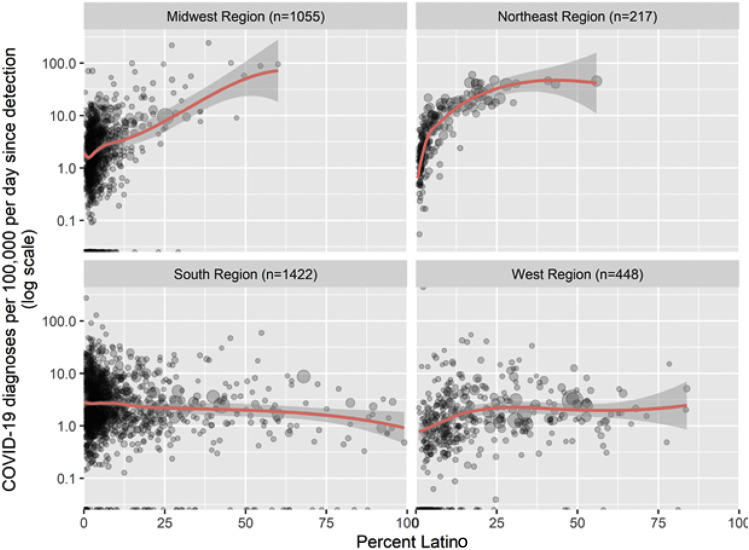
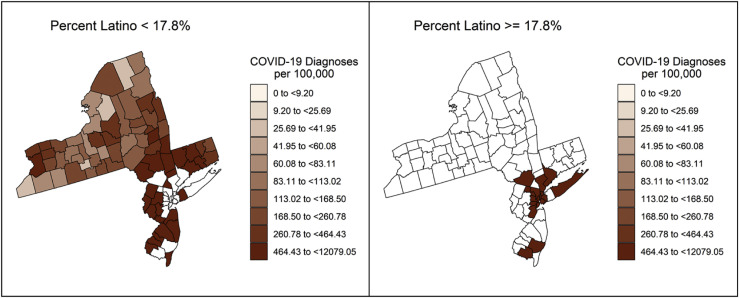
Fourteen percent of U.S. counties (443/3143) are disproportionately Latino. As of May 11, there were 700,169 COVID-19 cases (Fig. 1 ) and 42,674 COVID-19 deaths (Fig. 2 ) in disproportionately Latino counties. Up to 91.2% of disproportionately Latino counties (404/443) reported a case of COVID-19 and 54.4% (241/443) reported a death versus 92% (2484/2700) and 49.4% (1335/2700) in all other counties. COVID-19 cases increased with the proportion of Latino residents, particularly in the Midwestern and Northeastern counties (Fig. 3). Considering the major concentration of the epidemic during the period for the data used in this analysis, we have also included Fig. 1, Fig. 2 with the rates of COVID-19 diagnosis and deaths in disproportionally Latino counties in New York, New Jersey, and Connecticut.
Fig. 1.
Rates of COVID-19 diagnosis in disproportionally Latino (≥17.8% of population) and all other counties (<17.8% of population) as of May 11, 2020. Puerto Rico was included as a single data point.
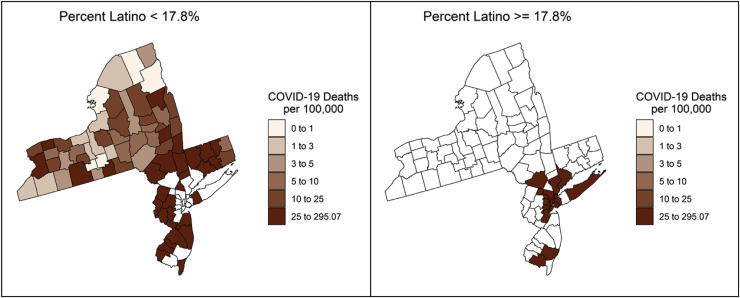
Fig. 2.
Rates of COVID-19 deaths in disproportionally Latino (≥17.8% of population) and all other counties (<17.8% of population) as of May 11, 2020. Puerto Rico was included as a single data point.
Fig. 3.
COVID-19 cases per 100,000 population (adjusted per day since detection) by proportion of Latino residents in the Northeast, Midwest, West, and South of the United States as of May 11, 2020.
Fig. 1.
Rates of COVID-19 diagnosis in disproportionally Latino (≥17.8% of population) and all other counties (<17.8% of population) in New York, New Jersey, and Connecticut as of May 11, 2020. As of May 11, 38.2% (509,763/1,334,088) of all COVID-19 cases were in New York, New Jersey, or Connecticut.
Fig. 2.
Rates of COVID-19 deaths in disproportionally Latino (≥17.8% of population) and all other counties (<17.8% of population) in New York, New Jersey, and Connecticut as of May 11, 2020. As of May 11, 49.1% (39,038/79,448) of all COVID-19 deaths were in New York, New Jersey, or Connecticut.
Differences in COVID-19 cases by region are replicated in the bivariate analyses comparing disproportionately Latino counties with all other counties (Table 1). Across regions, disproportionately Latino counties comprised people younger than those in other counties, were more likely to lack health insurance, had a greater number of persons per room in a household, had fewer monolingual English-speaking Latino residents, and had a greater proportion of monolingual Spanish-speaking or bilingual (Table 1; disaggregation by region in Table 1 can be found in Supplemental Table 1). There were no major differences in the underlying health conditions or social distancing scores and varying associations by region for other variables.
In Table 2 , the multivariate model examining predictors of both COVID-19 cases and associated mortality are presented. In the Northeast and Midwest regions, the rate of COVID-19 cases was higher in counties with a higher proportion of Latinos (third quartile compared with first quartile; aRR: 1.42, 95% CI: 1.11–1.84 and aRR: 1.70, 95% CI: 1.57–1.85, respectively) after adjusting for sociodemographic characteristics, comorbidities, and socioeconomic determinants. In addition, higher rates of COVID-19 cases were associated with a greater proportion of black residents (aRR: 1.11, 95% CI: 1.03–1.19), fewer white residents (aRR: 0.76, 95% CI: 0.67–0.85), and less unemployment (aRR: 0.86, 95% CI: 0.81–0.91). Similarly, higher rates of COVID-19 cases were associated with a greater proportion of monolingual Spanish speakers (aRR: 1.28, 95% CI: 1.16–1.42), higher heart disease death rates (aRR: 1.07, 95% CI: 1.01–1.14), and less social distancing (aRR: 0.72, 95% CI: 0.64–0.81) after controlling for all other factors (including the proportion of Latinos). In addition, higher rates of COVID-19 cases were associated with the number of days since the first case was diagnosed (aRR: 1.90, 95% CI: 1.80–2.01), indicating that similar demographics and comorbidities tend to have about 1.9 times as many cases at 52 days (third quartile) after COVID-19 was detected in the county compared with 37 days (first quartile) after COVID-19 was detected.
Table 2.
Rate ratios (third vs. first quartile) of demographics, chronic disease, social/environmental factors, for COVID-19 diagnoses and deaths
| Characteristic | COVID-19 cases | COVID-19 deaths | ||
|---|---|---|---|---|
| Unadjusted model | Q1 | Q3 | RR (95% CI) | RR (95% CI) |
| % Latino | 2.112 | 9.563 | 1.280 (1.239, 1.324) | 1.103 (1.054, 1.154) |
| Adjusted for age only | Q1 | Q3 | aRR (95% CI) | aRR (95% CI) |
| % Latino | 2.112 | 9.563 | 1.171 (1.131, 1.213) | 1.052 (1.002, 1.105) |
| % under 35 y old | 39.514 | 46.08 | 1.390 (1.315, 1.468) | 1.226 (1.131, 1.330) |
| Full adjusted model | Q1 | Q3 | aRR (95% CI) | aRR (95% CI) |
| % Latino: Northeast | 2.112 | 9.563 | 1.424 (1.113, 1.841) | 1.315 (0.930, 1.890) |
| % Latino: Midwest | 2.112 | 9.563 | 1.701 (1.570, 1.849) | 1.173 (1.037, 1.336) |
| % Latino: South | 2.112 | 9.563 | 1.024 (0.866, 1.212) | 0.986 (0.759, 1.283) |
| % Latino: West | 2.112 | 9.563 | 1.084 (0.909, 1.295) | 1.002 (0.761, 1.322) |
| Demographics | ||||
| % black | 0.7 | 10.2 | 1.107 (1.034, 1.185) | 1.204 (1.075, 1.349) |
| % white | 76.6 | 95.1 | 0.755 (0.674, 0.846) | 0.853 (0.700, 1.041) |
| % under 35 years old | 39.514 | 46.08 | 0.996 (0.940, 1.057) | 0.860 (0.787, 0.941) |
| % unemployed | 3.367 | 5.367 | 0.859 (0.814, 0.907) | 0.882 (0.803, 0.969) |
| % uninsured | 7.53 | 15.505 | 0.986 (0.906, 1.073) | 1.014 (0.877, 1.175) |
| % occupancy > 1 per room | 1.234 | 2.875 | 0.999 (0.955, 1.046) | 1.127 (1.042, 1.217) |
| % monolingual (English) | 28.552 | 63.576 | 0.862 (0.689, 1.068) | 1.146 (0.706, 1.922) |
| % monolingual (Spanish) | 3.115 | 17.512 | 1.284 (1.158, 1.419) | 1.078 (0.867, 1.356) |
| % bilingual | 28.262 | 53.81 | 0.972 (0.823, 1.139) | 1.172 (0.821, 1.712) |
| Chronic disease | ||||
| % diabetes | 7.8 | 12.5 | 1.019 (0.968, 1.074) | 1.003 (0.922, 1.092) |
| Heart disease death rate | 297.45 | 402.85 | 1.069 (1.005, 1.138) | 1.015 (0.917, 1.123) |
| Cerebrovascular/hypertension death rate | 50.1 | 89.386 | 1.007 (0.977, 1.033) | 1.043 (0.994, 1.080) |
| HIV infection rate | 40.8 | 198.05 | 0.987 (0.945, 1.032) | 0.987 (0.925, 1.055) |
| Social environment | ||||
| Urbanicity score | 3 | 6 | 1.085 (0.987, 1.192) | 1.079 (0.928, 1.254) |
| PM2.5 | 4.58 | 7.625 | 1.028 (0.918, 1.151) | 1.230 (1.028, 1.471) |
| Social distancing score | 3 | 5 | 0.720 (0.643, 0.806) | 0.866 (0.720, 1.040) |
| Days since first case | 37 | 52 | 1.901 (1.801, 2.007) | 2.082 (1.858, 2.340) |
All ratios compare the value of the third quartile (Q3) with the value of first quartile (Q1) for each variable in each row.
Urbanicity: 1 = urban, 6 = rural.
Social distancing score is a grade: A = 1, B = 2, C = 3, D = 4, F = 5.
Days since the first case is temporality variable based on the following citation: Geographic Differences in COVID-19 Cases, Deaths, and Incidence—United States, February 12–April 7, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:465–471. DOI: http://dx.doi.org/10.15585/mmwr.mm6915e4 icon.
Data as of May 11, 2020.
Q1 = first quartile; Q3 = third quartile; RR = rate ratio; aRR = adjusted rate ratio; % = percentage; PM2.5 = fine particulate matter in the air.
After controlling for all potential confounders, COVID-19 deaths were associated with the proportion of Latino residents in the Midwest region (aRR: 1.17, 95% CI: 1.04–1.34) and in counties with crowded living conditions (aRR: 1.13, 95% CI: 1.04–1.22) or elevated air pollution (aRR: 1.23, 95% CI: 1.03–1.47). COVID-19 death rates were lower among counties with a higher proportion of persons aged 35 years or younger (aRR: 0.86, 95% CI: 0.79–0.94) or a higher level of unemployment (aRR: 0.88, 95% CI: 0.80–0.97).
Discussion
To our knowledge, this is the first nationwide analysis of Latino-specific COVID-19 diagnoses and deaths in the U.S., including Puerto Rico. We found that the COVID-19 pandemic disproportionately impacts Latinos. Latino counties only account for 11% of counties in the Northeast, 4% of counties in the Midwest, and 33% of counties in the West. Nonetheless, they comprise a disparate proportion of COVID-19 cases in each region with 63.4% of cases and 66.1% of deaths in the Northeast, 31.9% of cases and 22.6% of deaths in the Midwest, and 75.4% of cases and 73.7% of deaths in the in the West. Our analyses provide a timely proxy for assessing the impact of COVID-19 on Latino communities and affirm the importance of Latino tailored prevention, care, and focused efforts to meet the needs of Latino individuals and communities.
Nationally, COVID-19 diagnoses and deaths increased with the proportion of Latinos residing within a given county. This relationship varied by geographic region, however, and declined in the South. The high burden of COVID-19 among black Americans across the country and in the South specifically may counter-balance Latino disparities and may help explain why the disparity seen in other regions among Latinos was not found in the South. Furthermore, undocumented immigrants, who are also disproportionately represented in the South [22], are less likely to both seek primary care and have hospital admissions relative to documented Latino immigrants [23,24].
COVID-19 deaths increased with the proportion of Latino residents in the Midwest only. A likely explanation for this finding is that most meat and poultry processing facilities in the United States are in the Midwest and colocated with COVID-19 outbreaks [25]. Various reports have found that a large number of Latino migrants are hired to work in the meatpacking industry and that COVID-19 outbreaks and deaths have been rising in meatpacking plants [26]. Exercising his authority under the Defense Production Act, in April 2020, President Trump issued an executive order that designated meatpacking workers as “essential workers”, thereby forcing many plants to reopen despite the ongoing transmission of COVID-19 in the plants and surrounding communities [27]. Since that time, there have been documented increases in COVID-19 deaths in meatpacking plants; those deaths may be reflected in our data.
Our findings suggest that occupational exposure plays an important role in Latino COVID-19 cases and deaths. Up to 59% of the Latino community in the United States is aged less than 35 years compared with 46% of the total population [10]. Relative to other racial and ethnic groups, Latinos are disproportionately young and overrepresented in a segment of the workforce that experiences ongoing occupational exposure. In addition to meatpacking plants, most of the Latino community is employed in factories or in other service-based industries that have been deemed “essential” in recent months [25,26]. Furthermore, counties with a high proportion of monolingual Spanish speakers were more likely to have higher rates of COVID-19 cases (compared with counties with fewer monolingual Spanish speakers), but not more likely to have increased COVID-19 death rates. Again, monolingual Spanish speakers are more likely to be occupationally exposed through involvement in factory or “service industry” jobs, but they are also more likely to be healthier, younger, and undocumented, thereby providing insight into the observed rates of greater Latino COVID-19 cases and no deaths in this analysis [24,26,28].
COVID-19 testing access for Latinos warrants mention. In general, COVID-19 testing has prioritized older populations with clinical indications for testing or those with underlying health conditions [29,30]. Migrants, who are likely to be monolingual, may be less likely to get tested. Those who are tested are likely to be sick and, thus, have clinical indications for testing.
Historically, Latinos have experienced patterns of decreased access to health care because of lack of insurance, inadequate insurance coverage, and fear of deportation [31,32]. Furthermore, recent policies that have deterred immigrants from receiving federal safety net assistance may influence decisions to seek testing or care even when needed [33]. Given this, it is likely that immigrants would have more undiagnosed cases than other groups and would be under-reported in official case counts. Additional barriers to testing among Latinos may include provider bias and less access to culturally appropriate health care services [34,35].
As with the previous analysis of COVID-19 among black Americans, the social determinants of health such as housing, employment, and working conditions were better predictors of Latino COVID-19 cases and deaths than underlying health conditions (except heart disease). Disproportionately Latino counties had a greater proportion of individuals residing in densely populated households, which was associated with COVID-19 cases. Employment was slightly lower in disproportionally Latino counties when compared with other counties, which was associated with lower COVID-19 cases and death rates after controlling for other variables. These findings might be ascribed to the fact that most Latinos continued working during this period, were not working from home, and many jobs held by Latino populations place them at greater risk exposure to COVID-19 [36]. Taken together, these findings suggest that a sole focus on individual-level factors such as risk behaviors is inadequate for implementing an effective national public health response to COVID-19 prevention and control within Latino communities.
Our analyses have limitations. First, as valuable as our analyses are in highlighting communities that are at a higher risk for COVID-19 acquisition and death, our study is an ecological analysis. Associations at the county level do not necessarily reflect associations at the individual level. The COVID-19 analytical methods we used, however, have been rigorously reviewed and published in another COVID-19 analysis [8] and others have used county-level data to assess COVID-19 impacts in racial minority communities [[37], [38], [39]]. Another limitation is the COVID-19 data itself. Some have criticized existing COVID-19 surveillance data as inaccurate, but these same publicly available data are also used by the Centers for Disease Control and Prevention to compile COVID-19 reports and issue public health recommendations [40]. Our analyses likely underestimated COVID-19 cases in disproportionately Latino counties because Latino communities, particularly those in low-income areas, are less likely to have access to COVID-19 testing [41,42], and some Latinos fear accessing health care due to their immigration status. Moreover, the COVID-19 surveillance systems have inadequately captured race and ethnicity data which are important to describe the heterogeneity in the Latino population. Third, owing to data limitations, we included Puerto Rico as one county, which constrained our ability to characterize the nuances in the island's epidemic. Fourth, our results were subject to a specific date and time, and consequently, statistically significant associations may weaken or strengthen as the pandemic grows.
Conclusions
We have demonstrated the heterogeneity in COVID-19 infection and death among Latinos in the U.S. These findings call for focused and energetic policy and programmatic responses. Even where Latinos and other racial/minority groups share similar structural barriers, the same policy responses may not be equally effective. For example, health care access is a critical starting point for responding to COVID-19 and all states need to expand Medicaid to achieve a more sustainable public financing system for health care. Most Latinos in the United States are citizens and would benefit from access in all states to Medicaid for persons with income up to 138% of poverty (i.e., Medicaid expansion population). Nonetheless, a range of federal and state policies create barriers to health insurance coverage both for immigrants and families of immigrants. This includes the five-year waiting period for access to Medicaid and the Children's Health Insurance Program (CHIP) for qualified noncitizens, the newly implemented public charge rule, and the exclusion from Medicaid and CHIP of undocumented immigrants. Too many Latinos are left behind in accessing public health insurance programs, they tend to have jobs that are less likely to offer employer sponsored insurance, and the mainstream health system is often unwelcoming, confusing, and inaccessible to them. Thus, alternative approaches are needed to provide prevention and care services in addition to expanding Medicaid and CHIP. This includes expanding the financing for health centers and other culturally and linguistically appropriate programs that are not subject to these eligibility restrictions.
From a programmatic perspective, timely assessments and interventions for infection control and prevention can address the intersection of occupational risk and employment in some Latino communities. Surveillance systems are called to capture data about race and ethnicity, not only for laboratory purposes, but also for hospitalizations and death certificates. Finally, these findings and recommendations should be considered alongside the different experiences of Latino communities across states, counties, and Puerto Rico. Grassroots strategies and community knowledge would strengthen the effectiveness of efforts to respond to COVID-19 and should be fully integrated in the response to the COVID-19 pandemic.
Conflicts of interest
The authors have no conflict of interest to disclose.
Acknowledgment
Authors' contributions: Each author made substantial contributions to all phases of article development and revision; contributed to study, analysis, and article plans; interpreted data; and approved the final version before submission. C. E. Rodriguez-Diaz, V. Guilamo-Ramos, G. Millett, and P. S. Sullivan conceptualized the project. E. Hall conducted main analyses. C. E. Rodriguez-Diaz, V. Guilamo-Ramos, G. Millett, L. Mena, B. Honermann, and J. S. Crowley drafted original and revised versions of the article. G. J. Prado, M. Marzan-Rodriguez, and C. Beyrer provided substantial revisions and feedback. C. E. Rodriguez-Diaz confirms full access to all aspects of the research and writing process and takes final responsibility for the article.
Appendix
Supplemental Table 1.
Distribution of the demographics, chronic diseases, social/environmental factors, and COVID-19 diagnoses and deaths in disproportionally Latino counties (≥17.8% of the total population) and in all other counties (<17.5% of the total population) by U.S. region
| Characteristic | Northeast |
Midwest |
South |
West |
||||
|---|---|---|---|---|---|---|---|---|
| Proportion Latinx < 17.8% proportion Latinx ≥17.8% |
Proportion Latinx < 17.8% proportion Latinx ≥17.8% |
Proportion Latinx < 17.8 % proportion Latinx ≥17.8% |
Proportion Latinx f 17.8% proportion Latinx≥17.8% |
|||||
| (n = 194) | (n = 23) | (n = 1018) | (n = 37) | (n = 1186) | (n = 236) | (n = 302) | (n = 146) | |
| Demographics | ||||||||
| Population | 82,769 (44,978; 185,973) | 789,034 (471,258; 9,554,19) | 19,729 (8198; 45,079) | 19,620 (4823;36,467) | 26,833 (14,324; 63,208) | 21,350 (7211; 74,659) | 15,929 (6161; 57,188) | 50,866 (14,895; 245,617) |
| % Latino | 2.9 (1.6, 5.3) | 22.7 (19.7, 27.0) | 2.7 (1.7, 4.6) | 25.2 (21.3, 33.1) | 3.6 (2.0, 6.5) | 31.1 (23.0, 52.9) | 6.8 (3.7, 10.5) | 33.7 (25.2, 48.0) |
| % black | 25 (1.0 5.3) | 11.4 (9.2, 18.8) | 0.9 (0.4, 2.3) | 2.3 (0.8, 4.7) | 11.8 (3.0, 30.5) | 4.6 (1.5, 9.8) | 0.6 (0.2, 1.0) | 1.4 (06, 2.7) |
| % white | 91.9 (87.9, 95.8) | 66.6 (55.7, 74.2) | 94.8 (90.9, 96.6) | 87.7 (80.4, 89.9) | 79.4 (63.4, 91.6) | 83.3 (75.0, 89.5) | 91.2 (85 5, 94.5) | 82.3 (74.1, 88.8) |
| % over 65 y old | 18.5 (16.8, 20.7) | 14.8 (13.6, 16.1) | 18.9 (16.7, 21.5) | 14.5 (12.9, 17.3) | 17.7 (15.6, 20.1) | 15.4 (12.9, 19.1) | 19.1 (14.3, 24.0) | 15.4 (131, 18.9) |
| % under 35 y old | 40.9 (38.0, 43.1) | 45.0 (43.7, 47.1) | 41.9 (39.3, 44.5) | 47.7 (45.2, 51.0) | 42.8 (39.8, 45.7) | 47.4 (42.8, 51.0) | 41.7 (36.1, 47.2) | 46.7 (43.2, 50.7) |
| % unemployed | 5.0 (4.0, 6.3) | 4.2 (3.5, 5.0) | 3.9 (3.2, 5.0) | 3.3 (2.4, 4.2) | 4.4 (3.6, 5.5) | 3.7 (3.2, 4.4) | 4.4 (3.3, 5.9) | 4.9 (3.9, 6.3) |
| % uninsured | 6.6 (5.2, 8.3) | 8.5 (6.5, 11.4) | 8.1 (6.2, 11.1) | 12.8 (8.9, 15.5) | 13.3 (10.1, 16.4) | 20.4 (17.2, 23.6) | 11.5 (8.8, 16.0) | 11.8 (9.4, 14.5) |
| % occupancy > 1 per room | 1.3 (1.0, 1.7) | 3.7 (2.5, 5.1) | 1.4 (1.0, 2.0) | 3.2 (2.3, 3.9) | 2.0 (1.4, 2.8) | 4.0 (3.0, 5.6) | 2.4 (1.5, 3.4) | 4.3 (2.9, 6.1) |
| % monolingual (English) | 52.8 (39.8, 61.8) | 19.4 (15.7, 23.7) | 56.0 (38.7, 73.1) | 18.3 (13.8, 23.6) | 38.5 (25.3, 55.2) | 28.9 (19.1, 37.6) | 58.2 (403, 72.1) | 31.7 (24.3, 42.0) |
| % monolingual (Spanish) | 6.9 (3.4, 12.1) | 20.8 (17.9, 24.8) | 5.8 (0.7, 13.2) | 21.5 (15.8, 25.1) | 12.2 (4.5, 20.3) | 14.4 (8.9, 20.3) | 6.2 (2.0, 11.7) | 14.5 (8.3, 20.1) |
| % bilingual | 39.4 (31.6, 47.4) | 58.6 (56.4, 59.2) | 34.1 (20.2, 47.1) | 59.3 (54.2, 62.9) | 45.6 (32.8, 55.4) | 56.3 (50.4, 60.7) | 33.7 (21.1, 45.9) | 52.2 (45.9, 56.8) |
| % Mexican | 0.1 (0.0, 0.3) | 1.4 (0.5, 2.0) | 0.3 (0.1, 0.9) | 8.9 (6.7, 11.6) | 0.7 (0.2, 1.5) | 6.0 (4.0, 9.5) | 0.9 (0.2, 2.0) | 7.3 (4.7, 11.6) |
| % Cuban | 0.0 (0.0, 0.0) | 0.1 (0.1, 0.3) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.1) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.1) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) |
| % Dominican | 0.1 (0.0, 0.2) | 2.3 (1.3, 3.5) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) |
| Chronic disease | ||||||||
| % diabetes | 8.6 (7.3, 10.1) | 9.2 (7.6, 10.1) | 9.1 (72, 11.1) | 9.1 (8.0, 10.1) | 12.1 (9.9, 14.6) | 9.4 (7.0, 12.4) | 7.5 (6.0, 9.1) | 8.4 (6.7, 104) |
| Heart disease death rate | 327.0 (290.9, 357.4) | 305.6 (285.5, 341.8) | 329.6 (291.1, 371.9) | 299.5 (270.8, 335.2) | 398.8 (340.4, 460.6) | 358.2 (315.7, 400 3) | 288.6 (253.2, 321.6) | 289 9 (254.5, 330.1) |
| Cerebrovascular and hypertension death rate | 58.1 (47.7, 69.1) | 43.4 (40.1, 47.4) | 70.0 (52.9, 96.7) | 59.9 (42.9, 119.3) | 70.1 (53.4, 88.2) | 64.3 (48.1, 89.9) | 63.5 (43.7, 101.0) | 52.9 (42.5, 70.4) |
| HIV infection rate | 104.5 (60.5, 210.6) | 491.6 (292.4, 815.0) | 50.3 (0.0, 89.8) | 0.0 (0.0, 81.6) | 1689 (94.1, 308.4) | 142.4 (64.2, 250 6) | 44.2 (0.0, 106.7) | 129.8 (81.8, 209.2) |
| Social Environment | ||||||||
| Urbanicity score | 4.0 (3.0, 5.0) | 2.0 (1.0, 2.5) | 5.0 (4.0, 6.0) | 5.0 (5.0, 6.0) | 5.0 (3.0, 6.0) | 5.0 (3.0, 6.0) | 6.0 (4.0, 6.0) | 5.0 (3.0, 6.0) |
| PM2.5 | 5.3 (4.2, 6.9) | 7.9 (6.7, 8.6) | 5.4 (4.1, 6.9) | 4.8 (4.5, 6.3) | 7.4 (6.5, 8.0) | 6.4 (5.2, 7.2) | 2.8 (2.2, 3.7) | 3.9 (3.1, 5.9) |
| Social distancing score | 4.0 (4.0, 5.0) | 4.0 (4.0, 5.0) | 4.0 (3.0, 5.0) | 4.0 (3.0, 4.0) | 4.0 (4.0, 5.0) | 4.0 (3.0, 5.0) | 4.0 (3.0, 4.0) | 4.0 (3.0, 4.0) |
| COVID-19 | ||||||||
| Days since first case | 53.0 (47.2, 58.0) | 63.0 (60.0, 66.0) | 43.0 (31.0, 50.0) | 36.0 (27.0, 45.0) | 47.0 (41.0, 52.0) | 43.5 (26.0, 51.0) | 45.0 (13.0, 54.0) | 50.0 (42.0, 60.0) |
| COVID-19 diagnosis rate (per 100,000) | 161.3 (69.7, 405.7) | 1910.2 (1384.4, 2527.9) | 65.0 (24 5139.4) | 545.5 (229 4, 1864.4) | 109 4 (50.0, 251.1) | 64.3 (26.6, 157.4) | 33.2 (8.0, 84.0) | 86.9 (44.1, 206.3) |
| COVID-19 death rate (per 100,000) | 6.4 (1.6, 30.5) | 1110 (83.8, 156.2) | 0.0 (0.0, 4.6) | 0.0 (0.0, 16.9) | 2.5 (0.0, 9.8) | 0.0 (0.0, 4.8) | 0.0 (0.0, 1.1) | 1.7 (0.0, 6.7) |
| COVID-19 death rate (cases >200) | 34.6 (15.6, 57.7) | 111.0 (83.8, 156.2) | 11.5 (6.3, 26.0) | 16.9 (9.3, 24.9) | 10.0 (5.3, 24.5) | 5.3 (2.8, 12.4) | 6.5 (4.0, 14.6) | 6.6 (2.7, 14.5) |
Urbanicity: 1 = urban, 6 = rural.
Social distancing score is a grade: A = 1, B = 2, C = 3, D = 4, F = 5.
Days since the first case is temporality variable based on the following citation: Geographic Differences in COVID-19 Cases, Deaths, and Incidence—United States, February 12–April 7, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:465–471. DOI: https://doi.org/10.15585/mmwr.mm6915e4external icon.
Data as of May 11, 2020.
Pct. = percentage; PM2.5 = fine particulate matter in the air.
References
- 1.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2478–2480. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control, Prevention Coronavirus Disease 2019 (COVID-19) in the U.S. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- 3.Raifman M.A., Raifman J.R. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Census Bureau American community survey 1-year estimates. 2018. https://data.census.gov/cedsci/table?t=Hispanic%20or%20Latino&tid=ACSDP1Y2018.DP05&hidePreview=false
- 5.Holtgrave D.R., Barranco M.A., Tesoriero J.M., Blog D.S., Rosenberg E.S. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Ann Epidemiol. 2020;48:9–14. doi: 10.1016/j.annepidem.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Weekly updates by select demographic and geographic characteristics. 2020. https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/
- 7.Centers for Disease Control, Prevention COVIDView: a weekly surveillance summary of U.S. COVID-19 activity. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
- 8.Millett G.A., Jones A.T., Benkeser D. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Census Bureau Census regions and divisions of the United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf
- 10.United States Census Bureau American community survey 5-year United States Census Bureau. 2018. https://data.census.gov/cedsci/
- 11.Bureau of Labor Statistics Local area unemployment statistics. 2019. https://www.bls.gov/lau
- 12.Centers for Disease Control, Prevention Diabetes Atlas. https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html
- 13.Centers for Disease Control, Prevention Interactive atlas of heart disease and stroke. https://nccd.cdc.gov/DHDSPAtlas/Default.aspx
- 14.Centers for Disease Control, Prevention CDC Wonder 2018. https://wonder.cdc.gov/ucd-icd10.html
- 15.Centers for Disease Control, Prevention. CDC NCHHSTP AtlasPlus [online data portal]. https://www.cdc.gov/nchhstp/atlas/index.htm Accessed May 22, 2020.
- 16.Valdiserri R.O., Sullivan P.S. Data visualization promotes sound public health practice: the AIDSvu example. AIDS Educ Prev. 2018;30(1):26–34. doi: 10.1521/aeap.2018.30.1.26. [DOI] [PubMed] [Google Scholar]
- 17.Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. Exposure to air pollution and COVID-19 mortality in the United States: a nationwide cross-sectional study. medRxiv. 2020 doi: 10.1101/2020.04.05.20054502. Submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Unacast social distancing scoreboard-- Counties. https://www.unacast.com/covid19/social-distancing-scoreboard
- 19.United States Department of Agriculture Rural-Urban Continuum Codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx
- 20.Rue H., Martino S., Chopin N. Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. J R Stat Soc Ser B (Statistical Methodology) 2009;71(2):319–392. [Google Scholar]
- 21.Besag J., York J., Mollié A. Bayesian image restoration, with two applications in spatial statistics. Ann Inst Stat Math. 1991;43(1):1–20. [Google Scholar]
- 22.Pew Research Center’s Hispanic Trends Project Portrait of unauthorized immigrants in the United States. 2009. https://www.pewresearch.org/hispanic/2009/04/14/a-portrait-of-unauthorized-immigrants-in-the-united-states/
- 23.Berk M.L., Schur C.L., Chavez L.R., Frankel M. Health care use among undocumented Latino immigrants. Health Aff (Millwood) 2000;19(4):51–64. doi: 10.1377/hlthaff.19.4.51. [DOI] [PubMed] [Google Scholar]
- 24.Vargas Bustamante A., Chen J., Rodriguez H.P., Rizzo J.A., Ortega A.N. Use of preventive care services among Latino subgroups. Am J Prev Med. 2010;38(6):610–619. doi: 10.1016/j.amepre.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 25.Dyal J.W., Grant M.P., Broadwater K. COVID-19 among workers in meat and poultry processing facilities ― 19 states, April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(18) doi: 10.15585/mmwr.mm6918e3. [DOI] [PubMed] [Google Scholar]
- 26.Waltenburg M.A. Update: COVID-19 among workers in meat and poultry processing facilities ― United States, April–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:887–892. doi: 10.15585/mmwr.mm6927e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The White House Executive order on delegating authority under the DPA with respect to food supply chain resources during the national emergency caused by the outbreak of COVID-19. The White House. https://www.whitehouse.gov/presidential-actions/executive-order-delegating-authority-dpa-respect-food-supply-chain-resources-national-emergency-caused-outbreak-covid-19/
- 28.McClure E.S., Vasudevan P., Bailey Z., Patel S., Robinson W.R. Racial capitalism within public health: how occupational settings drive COVID-19 disparities. Am J Epidemiol. 2020:kwaa126. doi: 10.1093/aje/kwaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Philly C.B.S. Coronavirus philadelphia: positive tests higher in poorer neighborhoods despite six times more testing in higher-income neighborhoods, researcher says. 2020. https://philadelphia.cbslocal.com/2020/04/06/coronavirus-philadelphia-positive-tests-higher-in-poorer-neighborhoods-despite-six-times-more-testing-in-higher-income-neighborhoods-researcher-says/
- 30.Bilal U., Barber S., Diez-Roux A.V. Spatial INequities in COVID-19 outcomes in three US Cities. medRxiv. 2020 [Google Scholar]
- 31.Ornelas I.J., Yamanis T.J., Ruiz R.A. The health of undocumented latinx immigrants: what we know and future directions. Annu Rev Public Health. 2020;41(1):289–308. doi: 10.1146/annurev-publhealth-040119-094211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rhodes S.D., Mann L., Simán F.M. The impact of local immigration enforcement policies on the health of immigrant Hispanics/Latinos in the United States. Am J Public Health. 2015;105(2):329–337. doi: 10.2105/AJPH.2014.302218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perreira K.M., Pedroza J.M. Policies of exclusion: implications for the health of immigrants and their children. Annu Rev Public Health. 2019;40(1):147–166. doi: 10.1146/annurev-publhealth-040218-044115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hall W.J., Chapman M.V., Lee K.M. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60–e76. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Velasco-Mondragon E., Jimenez A., Palladino-Davis A.G., Davis D., Escamilla-Cejudo J.A. Hispanic health in the USA: a scoping review of the literature. Public Health Rev. 2016;37(1):31. doi: 10.1186/s40985-016-0043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.US Department of Labor Job flexibilities and work schedules -2017-2018. Data from the American Time Use Survey. https://www.bls.gov/news.release/pdf/flex2.pdf
- 37.McGrath J., Kessler J., Cook A. Coronavirus is decimating racially diverse communities large and small. Third Way Report. 2020. https://www.thirdway.org/memo/coronavirus-is-decimating-racially-diverse-communities-large-and-small
- 38.McKinsey, Company Black Americans face disproportionate share of disruption from coronavirus. https://www.mckinsey.com/featured-insights/coronavirus-leading-through-the-crisis/charting-the-path-to-the-next-normal/black-americans-face-disproportionate-share-of-disruption-from-coronavirus
- 39.The Commonwealth Fund COVID-19 more prevalent, deadlier in U.S. counties with higher black populations. 2020. [DOI]
- 40.Centers for Disease Control, Prevention Coronavirus Disease 2019 (COVID-19): cases & deaths by County. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/county-map.html
- 41.Schmitt-Grohé S., Teoh K., Uribe M. National Bureau of Economic Research; Washington, DC: 2020. Covid-19: testing inequality in New York City; p. w27019. [Google Scholar]
- 42.In large texas cities, access to coronavirus testing may depend on where you live. NPR.org. https://www.npr.org/sections/health-shots/2020/05/27/862215848/across-texas-black-and-hispanic-neighborhoods-have-fewer-coronavirus-testing-sit