Abstract
Background
During the current global crisis unleashed by the severe acute respiratory syndrome coronavirus 2 outbreak, surgical departments have considerably reduced the amount of elective surgeries. This decrease leads to less time in the surgical room to develop and improve the surgical skills of residents. In this study, we developed a training program to obtain and maintain microsurgical skills at home, using a smartphone camera and low-cost materials, affordable for everyone.
Methods
Using a smartphone camera as a magnification device, 6 participants performed 5 exercises (coloring grids, grouping colors, unraveling of a gauze, knots with suture threads, and tower of Hanoi), both with the dominant and with the nondominant hand, for 4 weeks. We compared performance at the beginning and at the end of the training process. Each participant filled out an anonymous survey.
Results
When we compared the performance at the beginning and at the end of the training process, we found significant improvements (P = 0.05) with the dominant as well as the nondominant hand in all the exercises. All participants were satisfied or very satisfied with the definition of the objectives of the training process, material availability, the exercises performed, the choice of the time to train, and general satisfaction with the training program.
Conclusions
We developed a microsurgical skills training program to be performed at home, which can be easily reproduced. It allows residents to improve manual coordination skills and is regarded as a feasible adjunct for ongoing training for surgical residents.
Key words: COVID, Microsurgery, Neurosurgery, Pandemic, Simulation, Training
Abbreviations and Acronyms: SARS-COV-2, Severe acute respiratory syndrome coronavirus 2
Introduction
During the current global crisis unleashed by the severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) outbreak, health systems have focused their efforts on the treatment of this disease. Surgical departments have dramatically reduced the number of elective surgeries with the aim of protecting health workers and keeping the largest amount of available resources, mainly intensive health care units and mechanical breathing assisting equipment, for the treatment of patients with acute breathing symptoms caused by SARS-COV-2.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18
An example of this strategy is the recommendation sent out on March 13, 2020 by the American Committee of Surgeons to “minimize, postpone or cancel the selective programmed surgeries.”19
On the other hand, patients who do require surgery are treated by experienced surgeons, and the number of residents helping them during the procedure is reduced, with the aim of reducing the surgical time, minimizing the use of personal protection equipment, and taking care of the health of those surgeons during the learning period.7, 20
Moreover, many resident programs have chosen to reduce the amount of hours per week, organizing rotations by series of work with the goal of reducing the internal transmission of virus within the health care services, allowing backup options if any resident becomes ill or needs to be isolated.5, 6, 15, 16, 17, 21
This situation inevitably reduces time in the operating room to develop and improve surgical skills for residents.1, 22, 23 To avoid leisure time or inactivity for residents during the virus outbreak, virtual conferences and presentations with videoconference technology have been chosen to maintain academic training.6, 8, 24, 25, 26, 27, 28
Nevertheless, the question arises of whether it is possible to adapt a training program in surgical specialties in which hands-on skills are required. Because it is not possible to know the exact impact that isolation and social distancing may have on surgical practice in general, and residents under training in particular, a training program needs to be adapted to the current situation.
One of the necessary elements in microsurgical training is the surgical microscope. However, diverse and alternative means of magnification sources have been proposed to take training out of the hospital area. One of these options, which is within everyone’s reach, is the smartphone.29, 30
We introduce a model of training for acquiring and maintaining microsurgical skills at home, based on the use of simulators that have previously been described, using a smartphone camera and affordable and low-cost materials.
Methods
From March 16 to April 16, 2020, 6 participants of the program for neurosurgical residents of the Department of Neurological Surgery of Hospital “El Cruce,” Buenos Aires, Argentina performed a training skills program at home (Table 1 ).
Table 1.
Participants
| Participants | Skilled Hand | Postgraduate Year |
|---|---|---|
| 1 | Right | 1 |
| 2 | Right | 2 |
| 3 | Right | 2 |
| 4 | Right | 4 |
| 5 | Right | 4 |
| 6 | Right | 5 |
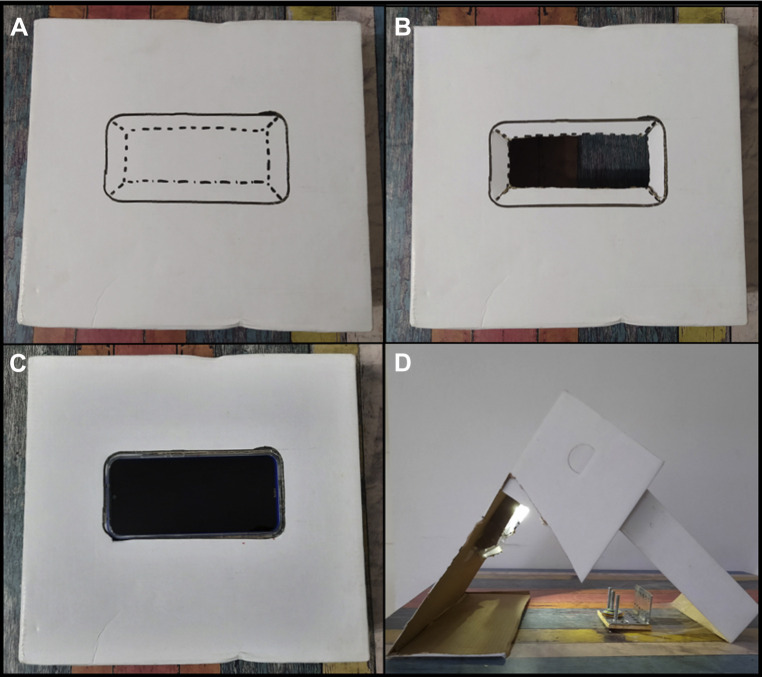
Each participant used the back camera of their smartphone as a magnification device (Redmi Note 8 [Xiaomi, Rainbow City, Beijing, China], iPhone 7, and iPhone XR (Apple, Cupertino, California, USA), with a minimum resolution of 12 megapixels, and amplification of 5×, which is compatible with the 25× objective of a surgical microscope. We used a modified shoe box as a support (Figure 1 ). This modified shoe box served not only as a support but also allowed various instruments to be passed through it from the sides (Figure 2 ).
Figure 1.
Assembly of cell phone support using a shoe box. (A) In the back surface of the box, the cell phone contour is drawn. Inside, 4 tabs are drawn (dotted lines). (B) A cut is made along the dotted lines, the rectangle disposed, and the tabs inverted to the interior of the box. (C) The cell phone is placed with the screen upward. (D) The lateral surfaces of the box are cut and the support system is ready to use.
Figure 2.
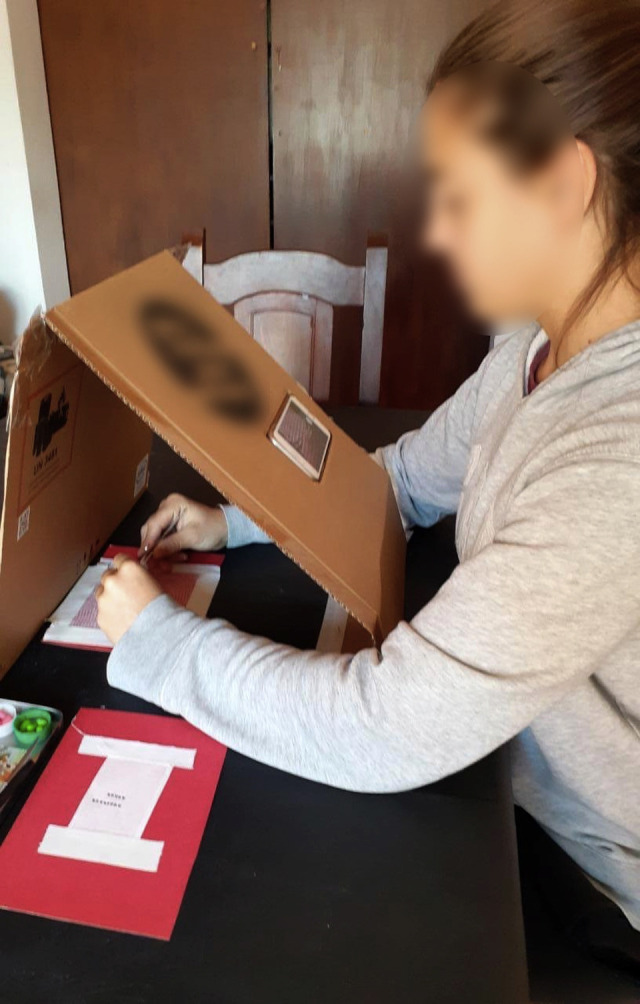
Participant training at home.
Each participant was given a set of instruments necessary to perform this program at home. Each set included microsurgical forceps (×2), scissors, surgical gauze (×5), and adhesive tape.
Before the beginning of the program, each participant had the chance to watch an explanatory video of each exercise.
Exercises
Coloring Sheets Measured in Millimeters
Aim
The aim was to exercise fine movements to improve microsurgical precision.
Materials
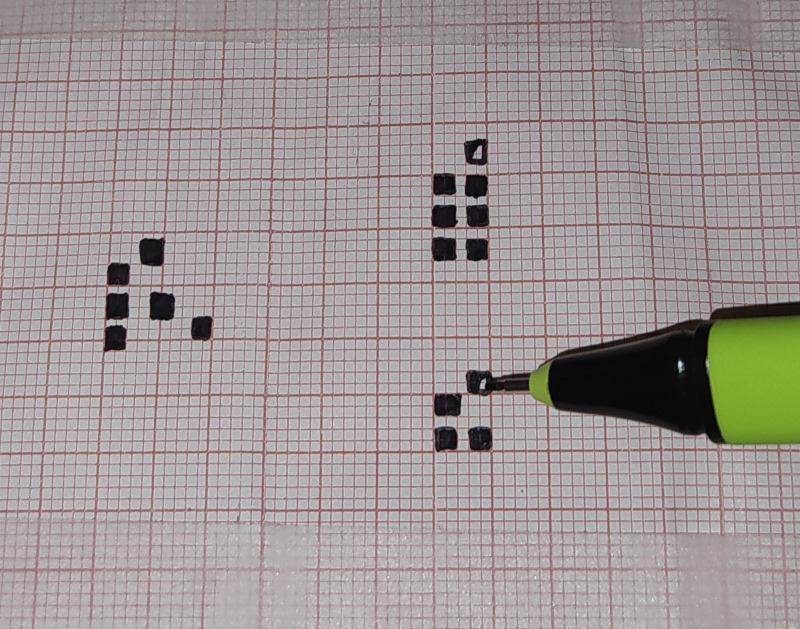
Materials included a microfiber 0.5 mm grain and a strip of electrocardiogram (ECG) paper (5×5 cm) or any paper measured in millimeters.
A 5×5 cm electrocardiogram paper was used for this exercise. The largest amount of 2×2 mm microgrids were meticulously colored in 30 seconds. Two consecutive microgrids could not be colored, and a free one had to be left among the colored ones (Figure 3).
Figure 3.
Grid coloring exercise.
Unraveling of a Gauze
Aim
The aim was to provide training in forceps movements and secure support of the hands in the microsurgical technique.
Materials
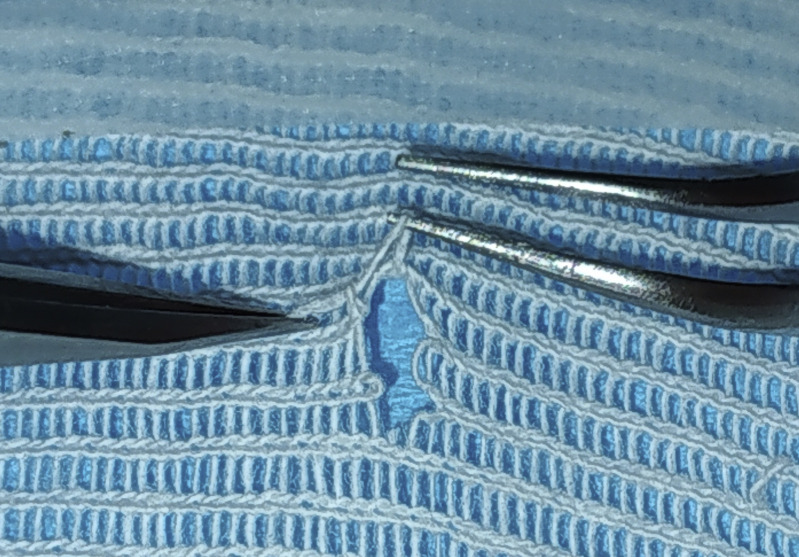
Materials included 1 surgical gauze, 1 straight and curve forceps Dumont type number 3, 5, or 7, 1 small pair of scissors or scalpel blade number 11 and an adhesive tape.
A sole layer of gauze was placed on a surface with a contrasting color to provide a better view. Gauze boundaries were fixed to the surface with adhesive tape. A thread of the weave was cut in the middle of the gauze. The edge was taken with a straight forceps and then passed to the other hand and so on, never letting the thread fall. Once the thread length was approximately 5 cm, the exercised was repeated with the nondominant hand (Figure 4 ).
Figure 4.
Unraveling of the gauze.
Knot
Aim
The aim was to exercise coordination movements required for performing microsurgical knots and also to encourage motor development of the nondominant hand.
Materials
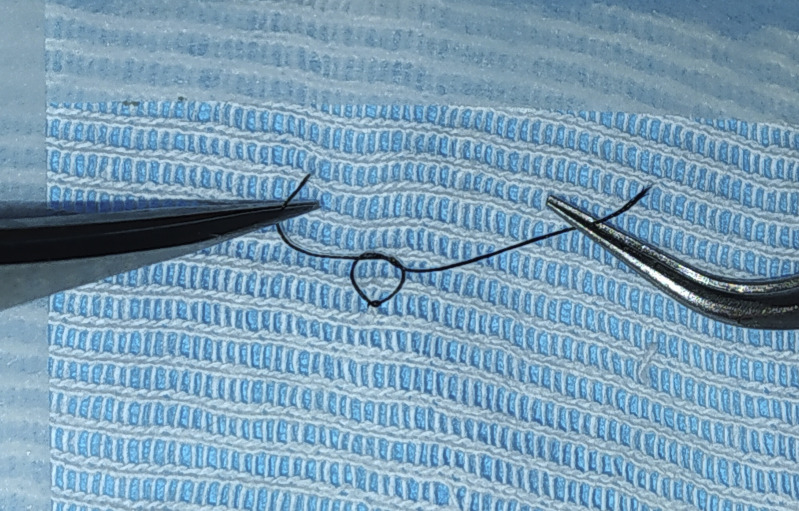
Materials included 1 surgical gauze, 2 straight and curve forceps Dumont type number 3, 5, or 7, 1 small pair of scissors or scalpel blade number 11, an adhesive tape, and a dark-colored sewing thread 100/2 thickness.
The surgical gauze was placed as described in the previous exercise. A 4-cm sewing thread piece was placed beneath 2 parallel threads of the gauze. Then, a knot was made with the sewing thread, putting together the 2 threads of the gauze. The exercise was repeated 5 times with each hand (Figure 5 ).
Figure 5.
Suturing and tying on the gauze.
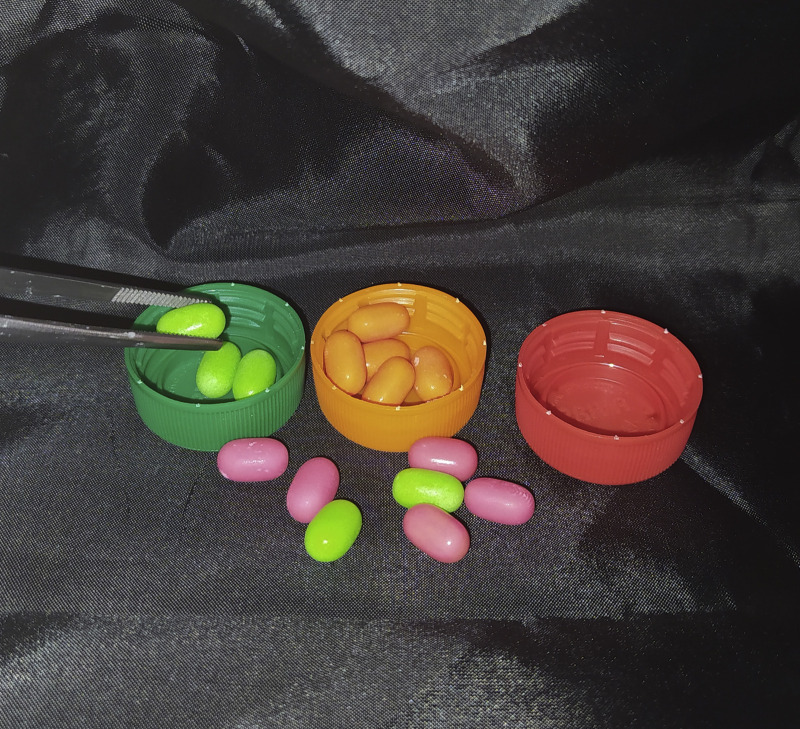
Grouping Colors
Aim
The aim was to train speed in fine movements and associative capacity.
Materials
Materials included 3 bottle lids, 15 sweet candies (such as Tic Tac [Ferrero del Ecuador S.A., Quito, Ecuador, Italy]) of 3 different colors (5 of each color), and 1 dissection forceps.
The bottle lids, which were used as the sweet candy containers, were placed in the center of the training field. Afterwards, the candies were randomly spread around the containers. Candies were grouped by color in a corresponding container in the least time possible (Figure 6 ).
Figure 6.
Associating colors.
Tower of Hanoi
Aim
The aim was to develop executive functions. Besides exercising surgical skills, this exercise evaluates the ability of planning and problem-solving activities.
Materials
Materials included 5 metallic washers increasing in size, 3 bars/screws adapted in series, 2 cm between each, on a wooden base measuring 5×10 cm and 2 straight or curved forceps Dumont type number 3, 5, or 7.
This is an exercise elaborated by the French mathematician Edouard Lucas in 1883.31, 32 It consists of 3 bars and a variable number of discs. These were placed in a decreasing way in one of the bars, forming a pyramid. The discs should be moved to form a new pyramid, using the least number of movements possible, moving 1 disc at a time and in a decreased manner (no larger disc can be placed over a smaller one).
We selected 5 metallic washers (or discs) increasing in size available at a local market, which were colored for a pleasing visual appearance (Figure 7 ).
Figure 7.
Tower of Hanoi exercise.
Training Program
The exercises are performed once a day, 3 times a week during an initial period of 4 weeks. It has been suggested that the training should be performed as the first activity of the day.
The participant must record their time with a chronometer and film their practice for a subsequent control with a designated tutor.
Participants were given auto examination papers to record the time and the achievements reached by each participant (see Appendix A).
Series of Exercises To Be Performed First with the Dominant Hand and Then with the Nondominant One
-
1)
Coloring the grid
-
2)
Grouping colors
-
3)
Unraveling of the gauze
-
4)
Knots
-
5)
Tower of Hanoi
This sequence of exercises was repeated in the subsequent training activities during the 4 weeks that the program lasted.
Once the participants finished the exercises, they anonymously filled out a form (satisfaction survey) to show if they considered these exercises useful in keeping their skills active and improving them (see Appendix B).
Data and videos from the training sessions were gathered during the first training (baseline) and last training (final).
We compared skill performance in 5 exercises at the beginning and at the end of the training process in 6 participants. The ongoing variables were the time to conclude an exercise or the amount of tasks performed. A Wilcoxon test was used to compare our matches at the beginning and at the end of the process. The test was performed with SPSS version 25 (IBM Corp., Armonk, New York, USA).
Results
Six residents concluded the 12 repetitions of training. When comparing performance at the beginning and at the end of the training process (exercise 1 vs. exercise 12), we found significant improvements (P = 0.05) with the dominant hand as well as with the nondominant hand (Supplementary Table 1).
When the anonymous surveys filled out by the participants were evaluated, all reported being satisfied or very satisfied with the definition of the goals of the training process, the availability of materials, the exercises performed, the choice of the time to train, and in general, they reported satisfaction with the training program as a whole (Table 2 ).
Table 2.
Satisfaction Survey
| Evaluation Parameters | Very Unsatisfied | Unsatisfied | Neutral | Satisfied | Very Satisfied |
|---|---|---|---|---|---|
| Definition of training objectives | 3 | 3 | |||
| Materials availability | 6 | ||||
| Exercises performed | 2 | 4 | |||
| Possibility to choose the moment to train | 1 | 5 | |||
| Overall satisfaction | 2 | 6 |
Discussion
During this time of social isolation, restriction of learning activities, and limitation of surgical procedures with the aim of reducing the SARS-COV-2 transmission, protecting health workers, and optimizing the use of institutional resources for the treatment of this disease, there is a need to create alternative solutions that allow us, together with health care activities, to continue with training programs in surgical specialties, because the main element that we seek to develop is not the innate talent of a surgeon but the ongoing training process.8, 33 Although simulation training should be an integral part of every neurosurgical training program, the pandemic exacerbates that need.
Because during this current situation residents will spend an uncertain amount of time out of the operating room, home training is required. There are existing training models, such as that described by Belykh and Byvaltsev,34 but using a portable microscope. In our case, not all residents could afford a microscope, and therefore, it was necessary to look for alternative sources of magnification that allow us to compensate for the lack of microscope during training.
Top-range smartphones with high-resolution cameras may be used as alternatives.
In 2014, Kim et al.30 described the first training with these alternative methods of magnification. In that study, the participants performed vascular anastomosis in synthetic 2-mm vessels using 8-0 sutures and a smartphone as a source of magnification. Huotarinen et al.29 also use smartphones to train in fields with greater magnification, but unlike Kim et al., who use a support arm to keep the smartphone stable, Huotarinen et al. attached it to a coffee cup.
With the objective of using the smartphone screen to perform the exercises, and to avoid the use of direct vision, we decided to adapt a shoe box as a support for the smartphone while performing exercises within it.
The main limitation of the smartphone as a source of magnification is the lack of stereoscopic vision that a surgical microscope provides.
However, the lack of stereopsis has been compensated for by proprioception. For instance, the lack of depth has been replaced through the contact of the 2 forceps, or a forceps and some other element of the exercise. This strategy allowed participants to improve significantly the time of exercise completion after an initial adaptation period. It has been previously shown that microsurgical performance under two-dimensional visualization is possible but requires more time and may be not so effective, compared with a three-dimensional visualization.35, 36
Because two-dimensional visualization of a smartphone resembles the view obtained during laparoscopic procedures, several investigators have encouraged its use as an image source for training in laparoscopic skills.37, 38
There are previous reports of using smartphones as magnification devices for microsurgical training.29, 30 Based on these reports, we developed a training program using materials easily found at home, with the aim of maintaining progress of training residents.
During the COVID outbreak, many surgical departments have considerably reduced the number of procedures that they perform. This reduction could lead to a negative impact on trainees. Like other investigators, we believe that surgical simulators could mitigate the effects of COVID in formation of residents.39, 40, 41, 42, 43
The outcome, in our experience, shows a significant improvement with both hands in manual skills performance, after training (i.e., all participants improved, regardless of their previous level of skill).
The record of activities in the sheet provided allowed the participant not only to be self-examined but also to be objectively assessed by a “blind” tutor. The tutor was asked not only to evaluate the rate of improvement in the participants’ skills but also to give positive feedback regarding the skills to maintain and those to improve with further training.
Each participant filled out an anonymous survey when they finished the training program. All participants reported being satisfied with the program and with the opportunity to perform microsurgical training at home with affordable materials. One of the items that caused greatest satisfaction was the chance to choose the time of day to perform the training program. Regarding the affordable and easily found materials used, all participants agreed that the program allowed them to continue to improve their skills and hand–eye coordination when surgical activity is severely limited. Moreover, many participants mentioned that using materials similar to those used in regular surgical practice could be of greater benefit; however, the cost increase would negatively affect accessibility of such training. The exercises using surgical gauze were considered most similar to normal surgical practice.
Special attention should be given to the exercise named tower of Hanoi, which allowed participants not only to improve their performance with both hands but also to improve on planning the next movement to achieve the goal of the exercise with the least amount of movements and time possible. Consequently, the exercise stimulates not only manual performance but also cognitive activity. This exercise was the only one that showed a better performance with the nondominant compared with the dominant hand. We believe that this result may be because the movement of the forceps in this exercise was widely developed by the surgeon’s nondominant hand.
All participants believe that the training program had a positive impact on their professional practice, because it allowed them to obtain skills, improve coordination, and make delicate movements with better precision in a controlled environment.
Conclusions
We introduced a microsurgical practice program to be performed at home, which makes it easily reproducible. It also allowed participants to improve their manual coordination skills, making it a feasible adjunct for the ongoing training of surgical residents.
Acknowledgments
We are grateful to Rodrigez Storani, María Laura, and Enrique Martins for their selfless help.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Appendix B. Satisfaction SurveyPlease indicate your level of satisfaction
| Parameters for Evaluation | Very Unsatisfied | Unsatisfied | Neutral | Satisfied | Very Satisfied |
|---|---|---|---|---|---|
| Definition of objectives | |||||
| Materials availability | |||||
| Exercises performed | |||||
| Possibility to choose the moment to practice | |||||
| Overall satisfaction |
-
–
Have you enjoyed the Home Training Programme?
-
–
Do you have any opinion about using easily available materials?
-
–
Do you think training should be performed with similar materials that you would find in your daily practice? Or believe that the skills acquired depend more on the exercise performed than on the materials?
-
–
Which exercise do you consider to be more similar to your daily practice?
-
–
Do you think that the training will improve your professional practice? If your answer is positive, please detail.
-
–
If you have any comments write them down:
- Thanks for your participation!
Supplementary Table 1.
Comparison of Performance at the Beginning and at the End of TrainingHand Stage Median Interquartile Range P Value Grid coloring in 30 seconds∗ Left Initial 4.0 3.0 5.3 0.042 Final 5.5 4.4 7.3 Right Initial 6.5 3.5 7.6 0.027 Final 8.8 7.6 10.3 Associating colors† Left Initial 45.5 42.3 63.3 0.028 Final 28.5 27.0 34.3 Right Initial 46.5 41.0 61.0 0.028 Final 29.0 24.3 32.7 Unraveling of the gauze† Left Initial 298.5 213.8 741.8 0.028 Final 262.5 112.8 339.3 Right Initial 370.0 230.3 608.3 0.028 Final 206.0 106.5 304.8 Knots† Left Initial 223.0 114.5 468.0 0.028 Final 94.5 61.8 125.0 Right Initial 122.0 98.3 295.5 0.028 Final 63.5 48.0 194.0 Tower of Hanoi† Left Initial 193.5 178.0 254.8 0.028 Final 108.0 96.5 151.0 Right Initial 232.5 164.0 350.3 0.028 Final 100.5 87.5 144.0 ∗Variable: number of colored squares in 30 seconds.†Variable: time in seconds.
Appendix A. Self-Assessment FormComplete this form at the end of your daily training sessionSession Training __ of 12.
| Left Hand | Right Hand | |
|---|---|---|
| Microgrids colored within 30 seconds | ||
| Order color pills (time to complete the exercise in seconds) | ||
| Time to complete Unraveling of the gauze (time to complete the exercise in seconds) | ||
| Knots on surgical gauze (time to complete the exercise in seconds) | ||
| Tower of Hanoi (time to complete the exercise in seconds) |
References
- 1.Ahmed N., Devitt K.S., Keshet I., et al. A systematic review of the effects of resident duty hour restrictions in surgery: Impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;259:1041–1053. doi: 10.1097/SLA.0000000000000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Capkin S., Cavit A., Kaleli T. Microsurgery training with smartphone [Mikrochirurgische Übungen mit Smartphone als Vergrößerungshilfe] Handchir Mikrochir Plast Chir. 2018;50:443–445. doi: 10.1055/a-0661-6015. [DOI] [PubMed] [Google Scholar]
- 3.Carter B.S., Chiocca E. Editorial. COVID-19 and academic neurosurgery. J Neurosurg. 2020;133:8–9. doi: 10.3171/2020.4.JNS201013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi B.D. Editorial. A neurosurgery resident’s response to COVID-19: anything but routine. J Neurosurg. 2020;133:16–17. doi: 10.3171/2020.4.JNS201028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chowdhry S.A., Spetzler R.F. Genealogy of training in vascular neurosurgery. Neurosurg. 2014;741:198–203. doi: 10.1227/NEU.0000000000000225. [DOI] [PubMed] [Google Scholar]
- 6.Demirseren M.E., Tosa Y., Hosaka Y. Microsurgical training with surgical gauze: the first step. J Reconstr Microsurg. 2003;19:385–386. doi: 10.1055/s-2003-42634. [DOI] [PubMed] [Google Scholar]
- 7.Eichberg D.G., Shah A.H., Luther E.M., et al. Letter: Academic Neurosurgery Department Response to COVID-19 Pandemic: The University of Miami/Jackson Memorial Hospital Model. Neurosurgery. 2020;87:E63–E65. doi: 10.1093/neuros/nyaa118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ericsson K.A. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79:70–81. doi: 10.1097/00001888-200410001-00022. [DOI] [PubMed] [Google Scholar]
- 9.Gallo G., Trompetto M. The Effects of COVID-19 on academic activities and surgical education in Italy. J Invest Surg. 2020;33:687–689. doi: 10.1080/08941939.2020.1748147. [DOI] [PubMed] [Google Scholar]
- 10.Gunasagaran J., Rasid R.J., Mappiare S., Devarajooh C., Ahmad T.S. Microgrids: A model for basic microsurgery skills training. Malay Orthop J. 2018;122:37–41. doi: 10.5704/MOJ.1807.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu Y.J., Zhang J.M., Chen Z.P. Experiences of practicing surgical neuro-oncology during the COVID-19 pandemic. J Neurooncol. 2020;148:199–200. doi: 10.1007/s11060-020-03489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien) 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kairys J.C., McGuire K., Crawford A.G., Yeo C.J. Cumulative operative experience is decreasing during general surgery residency: A worrisome trend for surgical trainees? J Am Coll Surg. 2008;206:804–813. doi: 10.1016/j.jamcollsurg.2007.12.055. [DOI] [PubMed] [Google Scholar]
- 14.Lee Z., Chyi Yeu D., Ang B., Ng W., Seow W. Editorial. COVID-19 and its impact on neurosurgery: Our early experience in Singapore. JNeurosurg. 2020;33:24–25. doi: 10.3171/2020.4.JNS201026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Limbrick D.D., Jr., Dacey R.G., Jr. Simulation in neurosurgery: Possibilities and practicalities: foreword. Neurosurgery. 2013;73:1–3. doi: 10.1227/NEU.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 16.Potts J.R. Residency and Fellowship Program Accreditation: Effects of the novel Coronavirus (COVID-19) pandemic. J Am Coll Surg. 2020;230:1094–1097. doi: 10.1016/j.jamcollsurg.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323:2131–2132. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 18.Suri A., Patra D.P., Meena R.K. Simulation in neurosurgery: Past, present, and future. Neurol India. 2016;643:387–395. doi: 10.4103/0028-3886.181556. [DOI] [PubMed] [Google Scholar]
- 19.Bambakidis N.C., Tomei K.L. Editorial: Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg. 2020;133:10–11. doi: 10.3171/2020.3.JNS20965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crosby D.L., Sharma A. Insights on Otolaryngology Residency Training during the COVID-19 Pandemic. Otolaryngol Head Neck Surg. 2020;163:38–41. doi: 10.1177/0194599820922502. [DOI] [PubMed] [Google Scholar]
- 21.Bath J., Lawrence P. Why we need open simulation to train surgeons in an era of work-hour restrictions. Vascular. 2011;19:175–177. doi: 10.1258/vasc.2011.oa0284. [DOI] [PubMed] [Google Scholar]
- 22.Burke J.F., Chan A.K., Mummaneni V., et al. Letter: The Coronavirus Disease 2019 global pandemic: A neurosurgical treatment algorithm. Neurosurg. 2020;87:E50–E56. doi: 10.1093/neuros/nyaa116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karuna T. Learning microvascular anastomosis in low socioeconomic vascular models during residency. Cureus. 2017;9:e1199. doi: 10.7759/cureus.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis E.E., Taylor L.J., Hermsen J.L., McCarthy D.P., Fiedler A.G. Cardiothoracic education in the time of COVID-19: How I teach It. Ann Thorac Surg. 2020;110:362–363. doi: 10.1016/j.athoracsur.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ortiz P.A. Teaching in the time of COVID-19. Biochem Mol Biol Educ. 2020;48:201. doi: 10.1002/bmb.21348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perin A., Servadei F., DiMeco F., Hub and Spoke’ Lombardy Neurosurgery Group May we deliver neuro-oncology in difficult times (e.g. COVID-19)? J Neurooncol. 2020;148:203–205. doi: 10.1007/s11060-020-03496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mak S.T., Yuen H.K. Oculoplastic surgery practice during the COVID-19 novel coronavirus pandemic: experience sharing from Hong Kong. Orbit. 2020;39:316–318. doi: 10.1080/01676830.2020.1754435. [DOI] [PubMed] [Google Scholar]
- 28.Tomlinson S.B., Hendricks B.K., Cohen-Gadol A.A. Editorial. Innovations in neurosurgical education during the COVID-19 pandemic: is it time to reexamine our neurosurgical training models? J Neurosurg. 2020;133:14–15. doi: 10.3171/2020.4.JNS201012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huotarinen A., Niemelä M., Jahromi B.R. An easy, efficient and mobile way for training microsurgical skills during busy life of neurosurgical residency and resource challenged environment. World Neurosurg. 2017;107:358–361. doi: 10.1016/j.wneu.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 30.Kim D.M., Kang J.W., Kim J.K., Youn I., Park J.W. Microsurgery training using a smartphone. Microsurgery. 2015;35:500–501. doi: 10.1002/micr.22369. [DOI] [PubMed] [Google Scholar]
- 31.Simon H.A. The functional equivalence of problem solving skill. Cogn Psychol. 1975;7:268–288. [Google Scholar]
- 32.Welsh M.C., Huizinga M. The development and preliminary validation of the Tower of Hanoi-revised. Assessment. 2001;8:167–176. doi: 10.1177/107319110100800205. [DOI] [PubMed] [Google Scholar]
- 33.Ericsson K.A., Krampe R.T., Tesch-Romer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;100:363–406. [Google Scholar]
- 34.Belykh E., Byvaltsev V. Off-the-job microsurgical training on dry models: Siberian experience. World Neurosurg. 2014;82:20–24. doi: 10.1016/j.wneu.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 35.Belykh E., George L., Zhao X., et al. Microvascular anastomosis under 3D exoscope or endoscope magnification: A proof-of-concept study. Surg Neurol Int. 2018;9:115. doi: 10.4103/sni.sni_36_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wehr F., Held J. Stereoscopic versus monoscopic displays: Learning fine manual dexterity skills using a microsurgical task simulator. Appl Ergon. 2019;77:40–49. doi: 10.1016/j.apergo.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 37.Oti A.T., Galvão L.N., Pessoa T.C.P., et al. Development of a laparoscopic training model using a smartphone. Rev Col Bras Cir. 2017;44:471–475. doi: 10.1590/0100-69912017005008. [DOI] [PubMed] [Google Scholar]
- 38.Pérez Escamirosa F., Ordorica Flores R., Minor Martínez A. Construction and validation of a low-cost surgical trainer based on iPhone technology for training laparoscopic skills. Surg Laparosc Endosc Percutan Tech. 2015;25:e78–e82. doi: 10.1097/SLE.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 39.Amparore D., Claps F., Cacciamani G.E., et al. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol Nefrol. 2020;72:505–509. doi: 10.23736/S0393-2249.20.03868-0. [DOI] [PubMed] [Google Scholar]
- 40.Ehrlich H., McKenney M., ElkbuliWe A. Asked the experts: Virtual learning in surgical education during the COVID-19 pandemic-shaping the future of surgical education and training. World J Surg. 2020;44:2053–2055. doi: 10.1007/s00268-020-05574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fuller S., Vaporciyan A., Dearani J.A., Stulak J.M., Romano J.C. COVID-19 disruption in cardiothoracic surgical training: An opportunity to enhance education. Ann Thorac Surg. 2020 doi: 10.1016/j.athoracsur.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28:e456–e464. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shafi A.M.A., Atieh A.E., Harky A., Sheikh A.M., Awad W.I. Impact of COVID-19 on cardiac surgical training: Our experience in the United Kingdom. J Card Surg. 2020;35:1954–1957. doi: 10.1111/jocs.14693. [DOI] [PMC free article] [PubMed] [Google Scholar]