Abstract
Coronavirus disease 2019 (COVID-19) infection can involve many organs, such as central nervous system, including in relapse. We describe the case of a 64-year-old woman with microbiologically confirmed COVID-19–induced respiratory distress whose treatment resulted in a negative nasopharyngeal swab reverse transcriptase PCR (RT-PCR) result for COVID-19. However, after a few weeks, relapse occurred, as indicated by symptoms of acute meningoencephalitis. Results of COVID-19 RT-PCR testing from her cerebrospinal fluid, nasopharyngeal and tracheal aspiration specimens became positive again, but COVID-19 serum antibodies were negative. We therefore note that symptoms with neurologic involvement can be one of COVID-19's first presentations, or they can appear at relapse. Regular evaluation of patients during convalescence is therefore necessary.
Keywords: COVID-19, Encephalitis, Meningitis, Nervous system, Recurrence
Since early December 2019, coronavirus disease 2019 (COVID-19), after emerging in China, rapidly spread all over the world. The pathogen has been identified as a novel beta coronavirus and has been named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1].
Infected patients' symptoms range from asymptomatic to severe. Fever, cough and dyspnoea are the most common complaints, but involvement of other organs, including gastrointestinal, cardiac, kidney and nervous system, has also been reported [2,3]. Some patients manifest early neurologic symptoms like anosmia, ageusia, seizure, stroke and myopathy, along with mild respiratory symptoms, so new-onset neurologic manifestations can be the result of COVID-19 [4].
Here we describe the case of one definite patient with COVID-19 with pulmonary presentation that relapsed after partial recovery with central nervous system manifestation.
Case report
A 64-year-old woman sought care in the emergency department (Madaen Hospital, Tehran, Iran) on 16 February 2020 with acute progressive dyspnoea and generalized weakness. At presentation, temperature was 37.2°C, oxygen saturation 94%, respiratory rate 22 breaths per minute, heart rate 110 beat per minute and blood pressure 110/80 mm Hg. Primary laboratory test results indicated leukocytosis (white blood cell count, 13400/μl; nuclear polymorphs, 9648; lymphocytes, 2948 cells/mL; erythrocyte sedimentation rate, mm/hr; quantitative mg/l, 4+, D-dimer, >1000 ng/ml) and normal other routine laboratory tests. Medical history revealed hypertension, ischaemic heart disease and metastatic colorectal cancer from 15 months ago treated with a FOLFIRI (folinic acid, fluorouracil, irinotecan) regimen; last receipt of chemotherapy was 2 months ago.
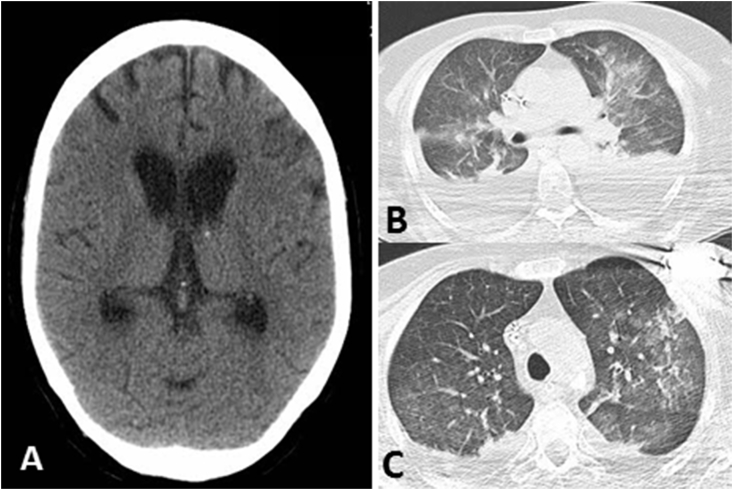
In order to address the acute dyspnoea and high D-dimer levels, pulmonary thromboembolism was suspected. Lung computed tomography (CT) was performed, revealing a pleural effusion in the lower field of both lungs, with collapse consolidation of basal segments and patchy ground-glass opacities (Fig. 1(C)). There was no evidence of pulmonary thromboembolism on angiographic images and echocardiography indicated normal pulmonary artery pressure.
Fig. 1.
(A) Brain computed tomographic (CT) scan revealed mild senile cortical atrophy. (B) Second lung CT scan revealed increase in plural effusion amount and ground-glass opacities. (C) First lung CT scan revealed bilateral pleural with collapse consolidation of basal segments and patchy ground-glass opacities.
Respiratory specimen by nasopharyngeal swab was tested for COVID-19 by qualitative real-time PCR (RT-PCR) (QiaSymphony; Qiagen, Hilden, Germany) was positive. Then the patient was treated with intravenous ceftriaxone and clindamycin. In addition, she received hydroxychloroquine (200 mg gavage twice daily) and lopinavir/ritonavir (400/100 mg gavage twice daily). She underwent regular swabs every week. Aligned with her partial recovery, the result of third nasopharyngeal swab RT-PCR for COVID-19 became negative, but she was still hospitalized. After 21 days, her consciousness suddenly decreased, and she again experienced respiratory distress. Therapy was empirically begun with intravenous meropenem, vancomycin, ampicillin, acyclovir and steroids. Neurologic evaluations found no evidence of focal neurologic deficit, meningismus or mild cortical atrophy on axial brain CT (Fig. 1(A)).
Lumbar puncture was performed, and analysis of the cerebrospinal fluid (CSF) had a 1920/mm3 cell count with 90% polymorphs, marked hypoglycorrhachia (glucose was 10 mg/dl with simultaneous blood glucose of 162 mg/dl) and elevated protein (94.8 g/l). There was no bacterial growth after 48 hours of incubation, and PCR result for Herpesviridae was negative. Second chest CT scan revealed diffuse alveolar infiltration in both lungs with bilateral pleural effusion (Fig. 1(B)), and tracheal aspiration culture led to growth of Klebsiella pneumoniae which was extremely drug resistant.
The patient continued to receive treatment for bacterial meningitis and ventilator-associated pneumonia; colistin provided intravenously was added. Eventually nasopharynx, tracheal aspiration and CSF specimens were tested again for COVID-19—and incredibly, all results were positive (Table 1). At that time, COVID-19 antibodies (IgM and IgG) were negative by the recombinant immunoblot assay technique. These positive PCR results were obtained on 9 April 2020, about 21 days after the negative result of the nasopharyngeal RT-PCR testing, which, in combination with antibody results, indicated definite respiratory infection relapse and a simultaneous central nervous system involvement with COVID-19.
Table 1.
Timeline of COVID-19 RT-PCR results
| Specimen | Date | PCR result |
|---|---|---|
| Nasopharyngeal swab | 16 February 2020 | Positive |
| Nasopharyngeal swab | 23 February 2020 | Weakly positive |
| Nasopharyngeal swab | 1 March 2020 | Negative |
| Nasopharyngeal swab | 8 March 2020 | Negative |
| Nasopharyngeal swab | 22 March 2020 | Positive |
| Tracheal aspiration | 22 March 2020 | Positive |
| Cerebrospinal fluid | 22 March 2020 | Positive |
COVID-19, coronavirus disease 2019; RT-PCR = reverse transcriptase PCR.
Discussion
COVID-19 is a Betacoronavirus that bind to angiotensin-converting enzyme 2 (ACE2) to enter the cell. ACE2 is present in several multiple human organs, including the nervous system, so SARS-CoV-2, which causes upper respiratory tract disease, can infect neural cells and result in a different neurologic appearance such as encephalitis [[5], [6], [7], [8]]. Some of the patients had fever and positive PCR test result after their hospital discharge. This might be due to the biological characteristics of COVID-19, or it might even be related to the reinfection [9].
Moriguchi et al. [10] reported a case of meningoencephalitis associated with SARS-CoV-2 in which specific COVID-19 RNA was detected in a CSF sample but not in the sample taken by nasopharyngeal swab. Also, brain magnetic resonance imaging revealed abnormal signal-changing of the temporal lobe, suggesting encephalitis. Our patient had meningitis/encephalitis with a CSF pattern completely consistent with bacterial meningitis, but with negative culture results for bacterial pathogens and a positive CSF sample PCR result indicating SARS-CoV-2. In our literature review, CSF analysis of reported encephalitis/meningitis cases resulted in mild lymphocytic pleocytosis [[11], [12], [13]]. Because our patient was receiving antimicrobial treatment, the negative CSF culture result for bacterial growth is not conclusive. As a study limitation, bacterial PCR analysis of CSF was not performed, so we cannot absolutely map the pattern of CSF results onto COVID-19. Chen et al. [14] reported a confirmed case of COVID-19 in a patient whose oropharyngeal swab test for SARS-CoV-2 became positive again after two sequentially negative results. The probability of a false-negative result may increase with an oropharyngeal or nasopharyngeal swab test alone, or it can be affected by such things as operator experience, sampling site and virus load of the specimen.
Our patient had a positive PCR result for SARS-CoV-2 21 days after a negative result. This positive result was confirmed by using three separate samples from nasopharynx, tracheal aspiration and CSF. To differentiate reinfection from recurrence of the disease, specific antibody testing was performed, and both COVID-19 IgM and IgG were negative. These results suggest the possibility of disease recurrence with a negative antibody test result, although our results may be related to the medical history of our patient, as well as the immunosuppression due to malignancy and chemotherapy. Although no leukocytopenia or lymphopenia was present, as a result of the lack of accurate information about the patient's humoral status, we cannot make a correct judgement about her immune condition.
Conclusion
To our knowledge, ours is the first study to report relapse of COVID-19 with meningoencephalitis manifestation. So it should be mentioned that neurologic symptoms as well as respiratory symptoms, may be the first presentation of COVID-19 and in pandemic period, we should be kept this expectancy in our mind, to avoid delayed diagnosis or misdiagnosis. Also given the possibility of a second positive SARS-CoV-2 RNA result in patients whose condition has improved and to prevent further transmission, regular evaluation of patients during convalescence seems necessary.
Conflict of interest
None declared.
Acknowledgements
The authors express their appreciation to members of the department of infectious disease, Shahid Beheshti University of Medical Sciences.
References
- 1.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karimi N., Razavi A.S., Rouhani N. Frequent convulsive seizures in an adult patient with COVID-19: a case report. Iran Red Crescent Med J. 2020 [Google Scholar]
- 3.Chen L., Liu H.G., Liu W., Liu J., Liu K., Shang J. [Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia] Zhonghua Jie He He Hu Xi Za Zhi. 2020 doi: 10.3760/cma.j.issn.1001-0939.2020.0005. [DOI] [PubMed] [Google Scholar]
- 4.Pleasure S.J., Green A.J., Josephson S.A. The spectrum of neurologic disease in the severe acute respiratory syndrome coronavirus 2 pandemic infection. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1065. [DOI] [PubMed] [Google Scholar]
- 5.Sanders J.M., Monogue M.L., Jodlowski T.Z., Cutrell J.B. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020 doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 6.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:1–9. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steardo L., Steardo L., Jr., Zorec R., Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol (Oxf) 2020;229 doi: 10.1111/apha.13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharifi-Razavi A., Karimi N., Rouhani N. COVID-19 and intracerebral haemorrhage: causative or coincidental? New Microbes New Infect. 2020;35:100669. doi: 10.1016/j.nmni.2020.100669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou L., Liu K., Liu H.G. Cause analysis and treatment strategies of ‘recurrence’ with novel coronavirus pneumonia (COVID-19) patients after discharge from hospital. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:281–284. doi: 10.3760/cma.j.cn112147-20200229-00219. [DOI] [PubMed] [Google Scholar]
- 10.Moriguchi T., Harii N., Goto J., Harada D., Sugawara H., Takamino J. A first case of meningitis/encephalitis associated with SARS-coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong P.F., Craik S., Newman P., Makan A., Srinivasan K., Crawford E. Lessons of the month 1: a case of rhombencephalitis as a rare complication of acute COVID-19 infection. Clin Med (Lond) 2020;20:293–294. doi: 10.7861/clinmed.2020-0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernard-Valnet R., Pizzarotti B., Anichini A. Two patients with acute meningo-encephalitis concomitant to SARS-CoV-2 infection. medRxiv. 2020 doi: 10.1111/ene.14298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duong L., Xu P., Liu A. Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in downtown Los Angeles, 2020 Apr 17 (comment) Brain Behav Immun. 2020;87:33. doi: 10.1016/j.bbi.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen D., Xu W., Lei Z., Huang Z., Liu J., Gao Z. Recurrence of positive SARS-CoV-2 RNA in COVID-19: a case report. Int J Infect Dis. 2020;93:297–299. doi: 10.1016/j.bbi.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]