We read with interest the modelling work of Goscé et al., ‘Modelling SARS-COV2 Spread in London: Approaches to Lift the Lockdown’, recently published in the Journal of Infection.1 This work highlights the importance of understanding transmission dynamics at a city and ‘district’ (borough) level in planning interventions to control the spread of COVID-19. The socioeconomically and demographically unequal impact of COVID-19 is well documented,2, 3, 4 and the consideration of COVID-19 transmission at a city, or even district-wide, level may not adequately reflect the uneven incidence of COVID-19. In light of our local experience, and in the context of the targeted lockdown of Leicester, the first localised city lockdown in the UK,5 we suggest a role for highly localised, community-level interventions that may not be evident in existing models.
Neither the burden of COVID-19 disease nor the pressure on existing healthcare resources have been felt equally across London, with particular strain on hospitals in the most ethnically diverse and deprived areas in the city's periphery.6 Notably, boroughs with the greatest levels of deprivation experienced the highest age-standardised mortality.7 The North Middlesex University Hospital (NMUH) in the borough of Enfield, North East London, serves a local population amongst the most deprived in England, the majority of whom are of BAME background,8 , 9 and was identified early in the surge as the second most COVID-pressured trust in the UK.6 This study examined the geographic, socioeconomic and demographic distribution of COVID-19 cases presenting to the NMUH during the pandemic peak of March and April 2020.
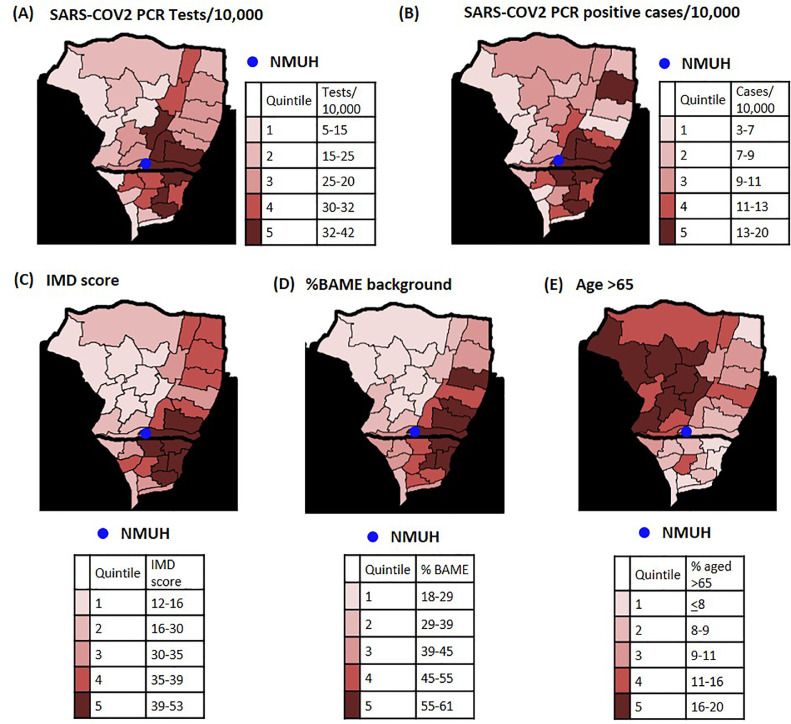
The postcodes of all patients tested for COVID-19 were retrospectively collected and used to identify the patient's ward (electoral subdivision of the borough) of residence. The incidence of symptoms consistent with the COVID-19 case definition (measured by SARS-CoV2 PCR tests on unique individuals per 10 000 ward residents) (Fig. 1 A), and the incidence of PCR-confirmed COVID-19 (measured by the number of positive SARS-CoV2 PCR results on unique individuals per 10 000 ward residents) (Fig. 1B) were mapped by ward. These maps identified that the majority of patients tested for COVID-19 and of PCR-confirmed cases were derived from a focused area immediately adjacent to the hospital (Figs. 1A & B).
Fig. 1.
Legend
(A) SARS-CoV2 PCR tests performed at NMUH per 10,000 population at a ward level. Wards with ≥5 patients tested were included
(B) SARS-CoV2 PCR positive COVID-19 cases diagnosed at NMUH per 10,000 population at a ward level. Wards with ≥ 5 cases were included
Local population structure at ward level by:
(C) Index of multiple deprivation score, 2015
(D) % of BAME background, census 2011
(E) age > 65 years, census 2011
Data from Public Health England, https://www.localhealth.org.uk/.
In all figures, wards were divided into even quintiles and then coloured by quintile. The values contained within each quintile are included in the quintile legends.
Maps generated using the Greater London Authority mapping template, https://data.london.gov.uk/dataset/excel-mapping-template-for-london-boroughs-and-wards.
Marked socioeconomic inequality has previously been identified in the borough, with stark geographic disparities in average income, life expectancy and housing quality between wards.10 Given the association of socioeconomic status and COVID-19 risk,7 borough wards were categorised by index of multiple deprivation score (IMD) 2015 and mapped (Fig. 1C), demonstrating that the areas that experienced a particularly high incidence of COVID-19 were those with the highest deprivation scores. Consistent with this geographic association, 42.97% (627/1459) of the PCR-confirmed COVID-19 patient were resident in the most deprived wards (categorised as IMD decile 1 or 2). Patients living in these wards were also significantly more likely to return a positive SARS-CoV2 PCR result than those from less deprived parts of the borough: 41.47% (260/627) of SARS-CoV2 PCR tests performed on people living in wards in IMD deciles 1&2 returned positive PCR results, compared to 30.55% (11/36) of tests performed on patients resident in the least deprived wards (IMD deciles 9&10), p 0.01, Chi-squared test.
The socioeconomic unevenness of the borough wards is mirrored in the ethnic diversity of their inhabitants, with the majority of the borough's black, Asian and ethnic minority (BAME) residents living in the most deprived, most COVID-19 affected, areas (Fig. 1D). In order to explore the impact of ethnicity within our patient population, patients were grouped as of either BAME background or white European background according to their self-reported ethnicity at hospital registration or excluded if no ethnicity was documented. Consistent with national-level observations regarding the increased risk of COVID-19 in BAME patients,2 , 4 50.39% of BAME patients tested were SARS-CoV2 PCR positive, compared to 37.79% of white European patients (p < 0.0001, Fischer's exact test).
At the time this study was undertaken, only patients being admitted to hospital who met the Public Health England clinical case definition were eligible for SARS-CoV2 PCR testing. As NMUH has the only emergency department in the borough, this study likely captures the majority of local residents with severe COVID-19 symptoms during the study period but the absolute number of cases cannot be determined. In light of this it is noteworthy that the most COVID-19 affected wards were those with the youngest populations (Fig. 1E), a factor typically associated with less severe COVID-19 disease,3 suggesting a potent role for socioeconomic and demographic factors beyond age in COVID-19 risk in our local population.
This study highlights the impact of socioeconomic and demographic factors on COVID-19 risk, and that these factors can be highly geographically localised. As the response to COVID-19 evolves from the national to local, resources need to be effectively, and equitably, targeted. The disparate demographic and socioeconomic structure of each city, and even borough, will likely necessitate differing approaches to limit the spread of the disease: the COVID-19 response must be embedded in local context.
The highly focused distribution of COVID-19 in our local area raises the possibility that specific community-level interventions may be useful in reducing COVID-19 transmission. Modelling will play a vital role in designing future interventions against COVID-19. Consideration of the possible merits of public health approaches against COVID-19 at city, and even borough, -wide level may mask substantial local disparities in its incidence, and therefore not identify the benefit of targeted measures to limit the spread of COVID-19. These models must use highly localised data, incorporating socioeconomic and demographic factors, to better reflect our local, and other national,2 , 4 , 7 observations regarding the unequal distribution of COVID-19. It is imperative that future models are able to reflect the unequal burden of COVID-19 in order to facilitate better resource allocation in the ongoing response.
Declaration of Competing Interest
None.
References
- 1.Goscé L., Phillips P.A., Spinola P., Gupta D.R.K., Abubakar P.I. Modelling SARS-COV2 spread in London: approaches to lift the lockdown. J Infect. 2020;81(2):260–265. doi: 10.1016/j.jinf.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aldridge R.W., Lewer D., Katikireddi S.V., Mathur R., Pathak N., Burns R. Black, Asian and minority ethnic groups in England are at increased risk of death from COVID-19: indirect standardisation of NHS mortality data. Wellcome Open Res. 2020;5:88. doi: 10.12688/wellcomeopenres.15922.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ICNARCReports [Internet]. [Cited 2020 May 6]. Available from: https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports.
- 4.Coronavirus (COVID-19) related deaths by ethnic group, England and Wales - Office for National Statistics [Internet]. [cited2020. Available from:https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronavirusrelateddeathsbyethnicgroupenglandandwales/2march2020to10april2020.
- 5.Plans for managing the coronavirus (COVID-19) outbreak in Leicester [Internet]. GOV.UK. [cited2020]. Available from: https://www.gov.uk/government/speeches/local-action-to-tackle-coronavirus.
- 6.April 2020 GB. Revealed: the hospitals facing most pressure to meet coronavirus demand [Internet]. Health Serv J 2020. [citedAvailable from: https://www.hsj.co.uk/quality-and-performance/revealed-the-hospitals-facing-most-pressure-to-meet-coronavirus-demand/7027354.article.
- 7.Deaths involving COVID-19 by local area and socioeconomic deprivation - Office for National Statistics [Internet]. [cited2020. Available from:https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand17april.
- 8.State of the Borough | Haringey Council [Internet]. [cited2020Available from:https://www.haringey.gov.uk/local-democracy/about-council/state-of-the-borough.
- 9.Borough and wards profiles • Enfield Council [Internet]. [cited2020. Available from:https://new.enfield.gov.uk/services/your-council/borough-and-wards-profiles/.
- 10.Enfield Poverty and Inequality Commission Archives [Internet].Smith Institute. [cited2020]. Available from:http://www.smith-institute.org.uk/book-author/enfield-poverty-and-inequality-commission/.