Abstract
Background
In response to the COVID-19 pandemic, Ontario issued a declaration of emergency, implementing public health interventions on March 16, 2020.
Methods
We compared cardiac catheterization procedures for ST-elevation myocardial infarction (STEMI) between January 1 and May 10, 2020 to the same time frame in 2019.
Results
From March 16 to May 10, 2020, after implementation of provincial directives, STEMI cases significantly decreased by up to 25%. The proportion of patients who achieved guideline targets for first medical contact balloon for primary percutaneous coronary intervention (PCI) decreased substantially to 28% (median, 101 minutes) for patients who presented directly to a PCI site and to 37% (median, 149 minutes) for patients transferred from a non-PCI site, compared with 2019.
Conclusions
STEMI cases across Ontario have been substantially affected during the COVID-19 pandemic.
Résumé
Introduction
En réponse à la pandémie de COVID-19, l’Ontario a déclaré l’état d’urgence et mis en place des interventions de santé publique le 16 mars 2020.
Méthodes
Nous avons comparé les procédures de cathétérisme cardiaque lors d’infarctus du myocarde avec sus-décalage du segment ST (STEMI) du 1er janvier au 10 mai 2020 à la même période en 2019.
Résultats
Du 16 mars au 10 mai 2020, après la mise en place des directives provinciales, les cas de STEMI ont connu une diminution significative pouvant atteindre jusqu’à 25 %. La proportion de patients qui ont atteint les objectifs prévus aux lignes directrices entre le premier contact médical et le ballonnet de l’intervention coronarienne percutanée (IPC) a connu une diminution considérable de 28 % (médiane, 101 minutes) pour ceux qui se présentaient directement dans un site d’IPC et de 37 % (médiane, 149 minutes) pour ceux qui étaient dirigés vers un site non-ICP, et ce, en comparaison à 2019.
Conclusions
La pandémie de COVID-19 a considérablement nui aux cas de STEMI de l’Ontario.
In response to the COVID-19 pandemic, the province of Ontario declared a state of emergency on March 16, 2020 and many public health interventions were implemented including social distancing, halting of nonessential businesses, and cancelling of elective health procedures and surgeries.1 Although ST-elevation myocardial infarction (STEMI) management requires emergent intervention and was not directly halted by these measures, the indirect effects of the pandemic on cardiac health and management might be important. Whether these interventions have affected the number of patients who present with STEMI and their treatment times is unknown.
Outcomes in patients who present with STEMI are sensitive to the timeliness of presentation (symptoms to first medical contact [FMC]) as well as the promptness of treatment (FMC to first balloon/device [FMC-balloon]). Ontario has a well developed STEMI system of care with designated care pathways (Ontario STEMI Bypass Protocol for patients calling 911 and Ontario Emergency Department STEMI Protocol for patients who present to an emergency department) and regional partnerships for primary percutaneous coronary intervention (PPCI) and pharmacoinvasive percutaneous coronary intervention (PCI) performed by 17 cardiac centres. CorHealth Ontario routinely monitors STEMI activity and provides productivity reports quarterly. In response to the changing landscape, and in consultation with provincial STEMI stakeholders and national societies, CorHealth developed a STEMI guidance document with an aim to preserve the established regional practices of PPCI or pharmacoinvasive PCI during the COVID-19 pandemic, while maintaining the safety of patients and health care workers.2,3
Brief reports from other jurisdictions affected by the COVID-19 pandemic show a substantial decrease in the number of patients who present to hospital with STEMI, delayed patient presentations, and potential delays in treatment times because of a limited capacity for regional transfers or availability of frontline health care workers.4, 5, 6 These studies were on the basis of a selected number of centres and none reported treatment times. Herein we report our observations for STEMI care during the initial few weeks after declaration of an emergency and the subsequent public health measures advising the public to stay home.
Methods
Data maintained in the CorHealth Ontario Cardiac Registry were used for this analysis. The data elements are collected on a standardized STEMI Case Report Form completed by a coordinator performing chart review at each STEMI hospital and consolidated monthly. Inclusion criteria for the reports are cases with STEMI diagnosis on referral for which a coronary angiogram is performed at a hospital with PPCI capabilities as the initial procedure. Variables included in this analysis include age, sex, diabetes, hypertension, hyperlipidemia, previous myocardial infarction > 30 days, previous heart failure, previous PCI, previous coronary artery bypass surgery, chronic obstructive pulmonary disease, mode of presentation (emergency medical systems vs self), location of first presentation (direct to PCI site, transferred from non-PCI site), reperfusion type (PPCI, pharmacoinvasive PCI, rescue PCI, late PCI > 24 hours), and FMC-balloon time. Key performance indicators were percentage of STEMI cases presented directly to a PCI site achieving time ≤ 90 minutes from FMC-balloon and percentage of STEMI cases transferred from a non-PCI site achieving time ≤ 120 minutes from FMC-balloon.
For this analysis, STEMI activity across the province was compared between January 1 to May 10, 2020 and the same time period in 2019. Baseline characteristics were statistically compared across all time frames for cardiac catheterization procedures for STEMI between January 1 and May 10, 2020 to the same time frame in 2019, and, after the implementation of provincial directives, from March 16 to May 10, 2020 using a χ2 test for categorical variables and analysis of variance for continuous variables. Any differences among the 3-way time frame comparisons were further examined by performing pairwise comparisons (Table 1). The rate of the number of STEMI cases reported in biweekly periods in 2019 and 2020 were compared using a Poisson model (Fig. 1). In addition, FMC-balloon times for PPCI were assessed on a biweekly basis, coordinating with Monday to Sunday calendar weeks (Fig. 2). Times are displayed in minutes as median and 10th and 90th percentiles. The median times reported in biweekly periods in 2019 and 2020 were compared using a 2-sided Wilcoxon 2-sample test.
Table 1.
Baseline characteristics of cardiac catheterization procedures for STEMI
| January 1 to May 10, 2019 | January 1 to March 15, 2020 | March 16 to May 10, 2020 | P | ||||
|---|---|---|---|---|---|---|---|
| STEMI patients |
2513 |
1397 |
824 |
||||
| Mean age (SD) | 63.6 (12.6) |
% | 63.9 (12.5) |
% | 63.5 (12.5) |
% | 0.770 |
| n | n | n | |||||
| Female sex | 680 | 27.1 | 406 | 29.1 | 225 | 27.3 | 0.392 |
| Diabetes | 559 | 22.2 | 307 | 22 | 177 | 21.5 | 0.898 |
| Hypertension | 1285 | 51.1 | 696 | 49.8 | 399 | 48.4 | 0.370 |
| Hyperlipidemia | 1050 | 41.8 | 537 | 38.4 | 311 | 37.7 | 0.039 |
| Previous MI | 296 | 11.8 | 116 | 8.3 | 65 | 7.9 | < 0.001 |
| Previous CHF | 61 | 2.4 | 30 | 2.1 | 11 | 1.3 | 0.173 |
| Previous PCI | 330 | 13.1 | 174 | 12.5 | 98 | 11.9 | 0.613 |
| Previous CABG | 101 | 4 | 47 | 3.4 | 25 | 3 | 0.336 |
| COPD | 101 | 4 | 61 | 4.4 | 19 | 2.3 | 0.038 |
| EMS presentation | 1468 | 58.4 | 845 | 60.5 | 564 | 68.5 | < 0.0001 |
| Symptom onset to FMC > 12 hours | 60 (1551) | 3.7 | 33 (834) | 3.8 | 13 (520) | 2.4 | 0.326 |
| Total PCI | 2141 | 85.2 | 1176 | 84.2 | 722 | 87.6 | 0.084 |
| PPCI | 1843 | 73.3 | 990 | 70.9 | 622 | 75.5 | 0.051 |
| Pharmacoinvasive PCI | 146 | 5.8 | 87 | 6.2 | 38 | 4.6 | 0.275 |
| Rescue PCI | 53 | 2.1 | 36 | 2.6 | 19 | 2.3 | 0.643 |
| Late PCI (> 24 hours) | 99 | 3.9 | 63 | 4.5 | 43 | 5.2 | 0.272 |
| Cardiac catheterization only | 372 | 14.8 | 221 | 15.8 | 102 | 12.4 | 0.084 |
CABG, coronary artery bypass surgery; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; EMS, emergency medical systems; FMC, first medical contact; MI, myocardial infarction; PCI, percutaneous coronary intervention; PPCI, primary percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
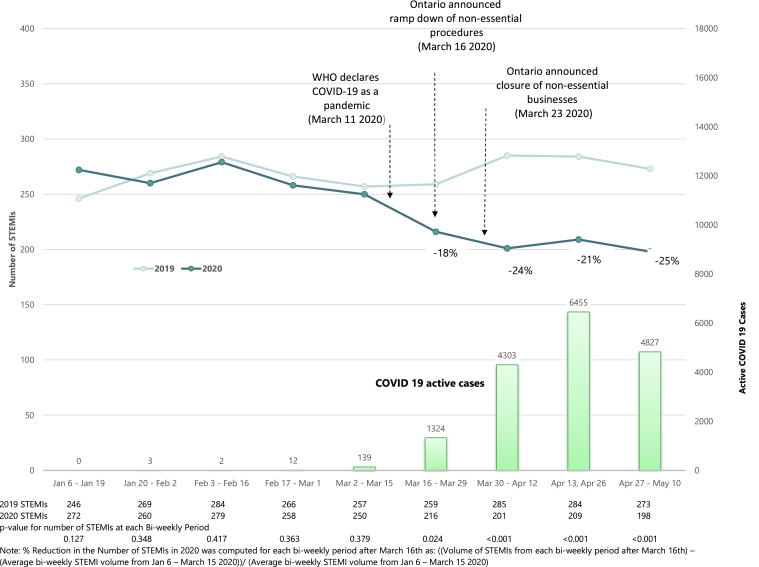
Figure 1.
ST-elevation myocardial infarction (STEMI) activation across Ontario: line chart showing number of STEMI activations every 2 weeks between January and May, 2019 and 2020. Bar chart shows number of active COVID-19 cases reported across Ontario. WHO, World Health Organization. Data from COVID-19 in Canada (https://art-bd.shinyapps.io/covid19canada).
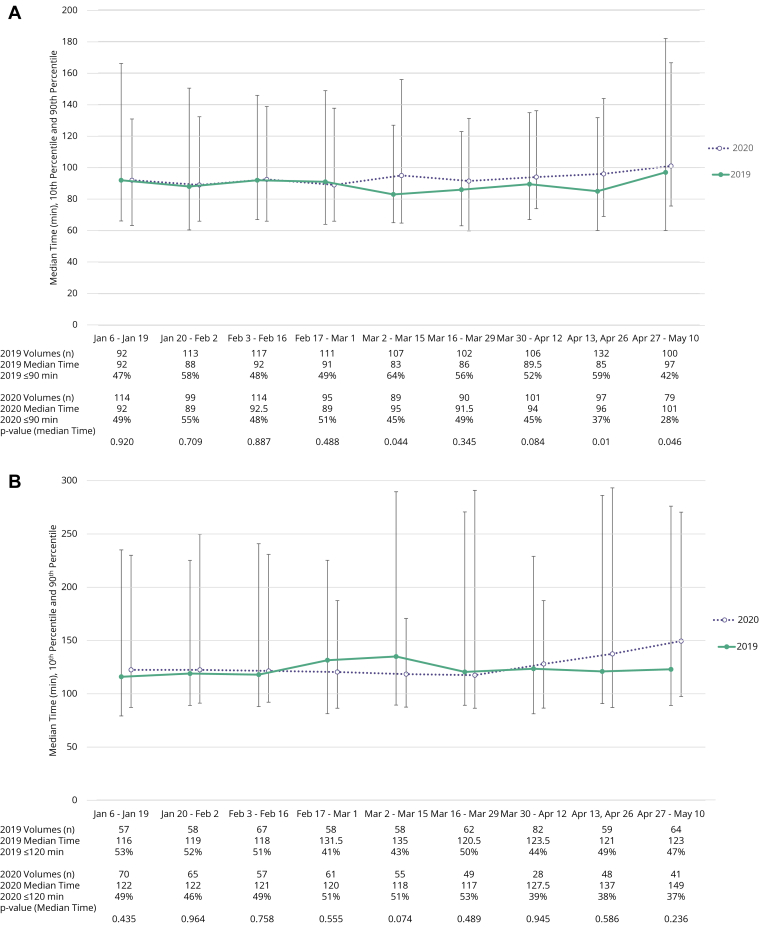
Figure 2.
Trends in ST-elevation myocardial infarction (STEMI) metrics in 2-week intervals between January and May, 2020 are shown using medians (with 10th and 90thpercentiles). (A) Time from first medical contact to balloon (FMC-balloon) for patients who presented to percutaneous coronary intervention sites. (B) FMC-balloon for patients transferred from non-percutaneous coronary intervention sites. Number of cases and percentage of patients who met target FMC-balloon are listed below each plot.
Results
Between January 1 and May 10, 2020, there were 2221 STEMI cases reported to CorHealth, compared with 2513 cases during the same time frame in 2019 (Table 1). There were no differences observed in baseline characteristics of age and sex. Compared with 2019 or the first 3 months of 2020 there were fewer patients with hyperlipidemia, previous myocardial infarction, and chronic obstructive pulmonary disease and an approximate 8% increase in patients who presented using emergency medical systems after March 16, 2020. There were no changes observed in the proportion of patients referred for cardiac catheterization who presented > 12 hours after symptom onset. Most (more than 70%) of STEMI cases continued to be treated with PPCI.
A sustained and significant reduction in STEMI cases of up to 25% was observed after March 16, 2020 (Fig. 1). The decrease in STEMI volumes also correlated with an increase in reported active COVID-19 cases (Fig. 1). Starting in the week of March 16, 2020, the proportion of patients who achieved FMC-balloon benchmarks for PPCI decreased substantially to 28% (FMC-balloon ≤ 90 minutes) for patients who presented directly to a PCI site and to 37% (FMC-balloon ≤ 120 minutes) for patients transferred from a non-PCI site (Fig. 2). The corresponding biweekly median times significantly increased to 101 minutes for the direct to PCI site group and nonsignificantly increased to 149 minutes for patients transferred from a non-PCI site, compared with 2019.
Discussion
Our early observations for STEMI care during COVID-19 across Ontario show a substantial and sustained decrease in cardiac catheterization procedures for STEMI over several weeks starting mid-March, 2020. This coincided temporally with the Ontario government-directed public health interventions and direction to stay home. Although the most STEMI patients continued to receive primary PCI, a decrease in key performance metrics was noted especially in patients being transferred from non-PCI sites. An increase in cardiac catheterization lab procedures for patients with symptom onset to FMC > 12 hours was not observed.
Recent reports have noted a decrease in number of STEMI presentations during the COVID-19 pandemic. Combining 9 US centres with volumes > 100 PPCIs per year, Garcia et al. noted a 38% reduction in STEMI activations post COVID-19 compared with the immediate previous 14 months.5 In a smaller single-centre study from Hong Kong, Tam et al. noted reduced daily emergency room attendance after COVID-19 including a decrease in STEMI patients.4 In these studies, STEMI patients tended to have longer symptom onset to FMC time outside of the window for revascularization. Possible explanations provided for the decrease in STEMI activations include: (1) intense public health messaging to stay home leading to less short-term physical activity and less stressful work environments for many; (2) patients’ fear of contracting disease in a hospital environment resulting in delays in presentation or out-of-hospital death; and (3) delayed presentations (> 12 hours) resulting in decisions to not pursue emergency catheter-based therapies. The magnitude of reduction in STEMI procedures in our experience was not as large as others and in our analysis we were not able to determine if similar reasons are true in Ontario. It is an area of ongoing analysis to determine if there were a greater number of out-of-hospital cardiac deaths potentially due to untreated STEMI and if the short-term outcomes for treated STEMI patients were affected because of delays in presentation. CorHealth data only includes STEMI patients who have a cardiac catheterization procedure. Therefore, we could not determine the number of STEMI patients who presented to non-PCI hospitals and were not referred for cardiac catheterization.
The increase in treatment times from FMC for patients who received PPCI is concerning but not unexpected. Meeting performance indicators for timely reperfusion in patients with STEMI is highly dependent on tight alignments of rapid diagnosis and rapid transfers between STEMI providers. In a well organized STEMI system, longer treatment times for PPCI are generally associated with ambiguity in patient clinical presentation (eg, atypical symptoms) or diagnostic findings (eg, complex electrocardiograms). Timely availability of transport services and health care personnel at the sending and receiving hospitals might have been an issue. It is possible that safety measures aimed to protect the patient and health care workers might have negatively affected timely delivery of PPCI. These safety measures include newly implemented screening protocols at every step of the patient encounter as well as donning of personal protective equipment by health care workers. In addition, symptoms of dyspnea and chest pain related to possible presence of COVID-19 might have further delayed definitive STEMI diagnosis and activation. Most concerning is that the lower proportion of patients who achieved performance indices are noted in the setting of reduced STEMI volumes. This suggests, that although the province of Ontario did not experience a significant limitation in intensive care unit beds due to COVID-19 (between March and May 2020) and hospital systems were not directed to limit essential activity, there was an observed reduction in the performance of the Ontario STEMI system to provide timely care.7 Whether this is a temporary phenomenon related to initial challenges of implementation and accommodation to new processes that will improve over time remains to be seen.
Despite increasing COVID-19 activity across the province more than 70% of STEMI procedures across Ontario were for PPCI. Some groups have proposed a move to a routine fibrinolytic-based reperfusion strategy during the pandemic.8,9 A pharmacoinvasive strategy as reported in the Strategic Reperfusion Early after Myocardial Infarction (STREAM) study, might be an alternative to PPCI when timeline metrics cannot be met, especially during the COVID-19 pandemic.10
Although increased risks of intracranial bleed have been a concern with this strategy, recent real world data from the Vital Heart Response Strategy Alberta, Canada has shown that a pharmacoinvasive strategy was associated with improved clinical outcomes (including core lab ST-segment resolution) compared with PPCI with similar intracranial and major bleeding rates, when half-dose in elderly patients was incorporated.11 Fibrinolysis time of 30 minutes might be a more achievable mode of reperfusion with fewer personnel and allows more time for further evaluation of patient status and testing for COVID-19. Additionally, transfer for a less emergent cardiac catheterization procedure further protects cardiac catheterization laboratory staff from inadvertent exposure and risks. In addition to the STEMI guidance document,2 CorHealth informed provincial emergency departments of the need to be adequately prepared including consideration of a pharmacoinvasive approach during this pandemic and future waves of COVID-19.12 However, challenges of routine fibrinolysis administration include ability to rapidly ramp up local supplies, ability of emergency departments to rapidly switch practice, and ongoing need for rescue PCI. Additionally, specific concerns related to administration of fibrinolysis during the COVID-19 pandemic include atypical STEMI presentations and reports of a myocarditis-like syndrome that mimics STEMI and possible increased risks of fibrinolysis.13 The recently organized North American COVID-19 ST-Segment-Elevation Myocardial Infarction (NACMI) registry will provide further insight into these clinical presentations and outcomes.14 Previous observational studies have shown that every 10-minute treatment delay in PPCI leads to an additional 3.3 deaths among 100 PPCI-treated patients for FMC-balloon times ranging from 60 to 180 minutes.15 Although the proportion of patients who received PPCI within 90 minutes decreased substantially in the direct to PCI centre group, the actual increase in median times was < 10 minutes. However, the increase in median FMC-balloon time for the transferred patients increased by more than 20 minutes. Ongoing surveillance and monitoring are needed because it is not clear at this time that the processes that contributed to increased FMC-balloon time would not also adversely affect door to needle time. Nevertheless, a pharmacoinvasive strategy might need to be reconsidered regardless of COVID-19 prevalence, for patients who present at hospitals across Ontario without PPCI capabilities, where substantial PPCI treatment delays are expected.16
Limitations
CorHealth relies on cardiac hospitals to provide timely data for reporting purposes. During the COVID-19 pandemic many hospitals report reduction of staff as well as reallocation to essential services. Although it is possible that data entry might be delayed, surveys of hospitals did not highlight any concerns with workload for data entry for this analysis. We did not observe changes in the proportion of STEMI patients who presented late after symptom onset. This might be related to several factors including uncertainty and inconsistencies in defining symptom onset (ie, when symptoms started vs when they were severe enough to seek medical attention), differences in coding of patients as STEMI or non-STEMI on the referral form, and patients not being referred for cardiac catheterization. However, the coding practices have remained unchanged over the past several years. Mortality data were not available for this cohort but will be the focus of further analysis.
Conclusions
The COVID-19 pandemic and corresponding public health measures have had a significant effect on STEMI care across Ontario. Cardiac catheterization lab procedures for STEMI have been reduced. The proportion of patients who meet reperfusion treatment goals for PPCI has decreased. Long-term consequences of these observations should be considered.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: The research reported has adhered to the relevant ethical guidelines.
See page 683 for disclosure information.
References
- 1.Ministry of Heath Ontario. http://www.health.gov.on.ca Available at:
- 2.CorHealth Ontario Cardiac Guidance Documents. https://www.corhealthontario.ca/resources-for-healthcare-planners-&-providers/covid19/guidance Available at:
- 3.Wood D.A., Sathananthan J., Gin K. Precautions and procedures for coronary and structural cardiac interventions during the COVID-19 pandemic: guidance from Canadian Association of Interventional Cardiology. Can J Cardiol. 2020;36:780-3. doi: 10.1016/j.cjca.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tam C.F., Cheung K.S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Filippo O., D’Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during covid-19 outbreak in northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Critical Care Services Ontario CCSO COVID-19 Updates. https://criticalcareontario.com/covid19-updates Available at:
- 8.Daniels M.J., Cohen M.G., Bavry A.A., Kumbhani D.J. Reperfusion of STEMI in the COVID-19 era-business as usual? Circulation. 2020;141:1948–1950. doi: 10.1161/CIRCULATIONAHA.120.047122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bainey K.R., Bates E.R., Armstrong P.W. STEMI care and COVID-19: the value proposition of pharmacoinvasive therapy Circ Cardiovasc. Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006834. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong P.W., Gershlick A.H., Goldstein P. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2013;368:1379–1387. doi: 10.1056/NEJMoa1301092. [DOI] [PubMed] [Google Scholar]
- 11.Bainey K.R., Armstrong P.W., Zheng Y. Pharmacoinvasive strategy versus primary percutaneous coronary intervention in ST-elevation myocardial infarction in clinical practice: insights from the Vital Heart Response Registry. Circ Cardiovasc Interv. 2019;12 doi: 10.1161/CIRCINTERVENTIONS.119.008059. [DOI] [PubMed] [Google Scholar]
- 12.CorHealth Ontario. https://www.corhealthontario.ca/resources-for-healthcare-planners-&-providers/covid19/cardiac Available at:
- 13.Bangalore S., Yatskar L., Harari R. ST-segment elevation in patients with COVID-19—a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dehghani P., Davidson L.J., Grines C.L. North American COVID-19 ST-Segment-Elevation Myocardial Infarction (NACMI) registry: rationale, design, and implications. Am Heart J. 2020;227:11–18. doi: 10.1016/j.ahj.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong G.C., Welsford M., Ainsworth C. 2019 Canadian Cardiovascular Society/Canadian Association of Interventional Cardiology guidelines on the acute management of ST-elevation myocardial infarction: focused update on regionalization and reperfusion. Can J Cardiol. 2019;35:107–132. doi: 10.1016/j.cjca.2018.11.031. [DOI] [PubMed] [Google Scholar]
- 16.Mercuri M., Welsford M., Schwalm J.D. Providing optimal regional care for ST-segment elevation myocardial infarction: a prospective cohort study of patients in the Hamilton Niagara Haldimand Brant Local Health Integration Network. CMAJ Open. 2015;3:E1–7. doi: 10.9778/cmajo.20140035. [DOI] [PMC free article] [PubMed] [Google Scholar]