Abstract
In older adults, we determined (1) the association of perceived sleep quality with stress-coping behaviors (drinking alcohol, smoking tobacco, medication/drug use, overeating, prayer, exercise, social support, and treatment from a health professional) and (2) whether coping behavior mediated the relationship of perceived sleep quality with depression. Data came from the US Health and Retirement Study 2008–2010 (n = 1174). Using logistic regression, poor perceived sleep quality was associated with medication/drug use (odds ratio = 2.9; 95% confidence interval = 1.4–6.0) and overeating (odds ratio = 1.6; 95% confidence interval = 1.1–2.5). However, using structural equation modeling, coping behavior did not mediate the relationship of perceived sleep quality with depression symptomatology (p = 0.14).
Keywords: coping, depression, older person, sleep, stress
Introduction
Sleep plays a critical role in maintaining physical and mental health. This is particularly true among older adults, since maintaining sleep quality is increasingly challenging in later life, in terms of both sleep duration and quality (Landry et al., 2015). For example, among Americans aged 55 or older, 7–15 percent report rarely or never feeling rested when waking up in the morning (Foley et al., 1995) and 15 percent report frequently feeling sleepy during the day (Chasens et al., 2007). Daytime sleepiness among older adults increases risk of mortality, cardiovascular disease, and depressive symptoms (Jaussent et al., 2011; Newman et al., 2000); however, underlying pathways linking sleep quality to mental and physical health outcomes are poorly understood. Identifying mechanisms by which poor sleep quality influences mental and physical health may help identify novel intervention targets.
Coping behavior is one potential mediating pathway linking sleep quality and health. Coping behavior refers to the wide range of strategies that persons engage in when confronted with stressful life events (Cousson-Gélie et al., 2010). As outlined by Lazarus and Folkman (1984), coping behavior involves the perception of events, the appraisal of those events as stressful, and an individual’s behavior in response to those stressful events. Experimental evidence in animals and humans suggests that poor sleep quality—both restricted and disturbed sleep—increases the probability that daily life events (e.g. interpersonal relationships, job-related responsibilities) will be perceived as stressors, as opposed to benign occurrences (Meerlo et al., 2008). For example, in humans, exposure to temporary sleep deprivation and continuous arousals during sleep is associated with greater plasma concentrations of cortisol (Späth-Schwalbe et al., 1991), a hormone well-known for its role in the physical and psychological stress response (Stalder and Kirschbaum, 2013).
In addition, poor sleep quality has been associated with engaging in specific health behaviors to cope with stress. For example, in Japan, adults with sleep disorders reported smoking and drinking alcohol in response to stress more often than those without sleep disorders (Otsuka et al., 2017). Related work indicates that poor sleep quality may also increase misuse of medications and overeating as stress-coping behaviors (Albert et al., 2017; Benedict et al., 2012). In other words, poor sleep quality may increase both the probability that daily life events are perceived to be stressful and the likelihood individuals engage in “unhealthy” coping behaviors (e.g. substance use, overeating) in response to those stressful events. In addition, poor sleep quality may inhibit use of “healthy” stress-coping behaviors (e.g. seeking help from a medical professional (Unützer and Park, 2012), social support (Wade and Kendler, 2000), physical activity (Ströhle, 2008)). However, empirical evidence examining whether sleep quality is associated with specific coping behaviors is limited.
Building on this research, we sought to examine the association of perceived sleep quality with coping behaviors (drinking alcohol, smoking tobacco, drug/medication use, overeating, prayer, exercise, social support, and treatment from a health professional) in a nationally representative sample of older adults in the United States. In addition, we aimed to determine whether coping behavior mediated the association between perceived sleep quality and depression. We hypothesized that those with poor perceived sleep quality would be more likely to engage in coping behaviors considered detrimental to health over the long term (i.e. drinking alcohol, smoking tobacco, drug/medication use and overeating) and less likely to engage in coping behaviors considered beneficial to health over the long term (i.e. seeking professional help, social support, prayer and exercise). We also hypothesized that the relationship between perceived sleep quality and depression would be mediated by coping behaviors.
Materials and methods
Sample
This study included data from the 2008 and 2010 waves of the Health and Retirement Study (HRS), a longitudinal study that biennially collects demographic, socioeconomic, and health information on a representative sample of non-institutionalized US adults aged >50 years (Sonnega et al., 2014). Among the 15,840 individuals who participated in the 2008 wave, a random sub-sample (n = 1380) completed an experimental module designed to assess eight coping behaviors, described below. For this study, the analysis sample was limited to those who also participated in the HRS 2010 wave (n = 1225).
Of those eligible, 1174 (95.8%) had non-missing data for perceived sleep quality, depression measures, and covariates of interest. The analytic sample was 56 percent female, 79 percent non-Hispanic White, 63 percent married, with a mean age of 67 years. In addition, 16 percent had less than a high school degree, 7 percent were below the federal poverty threshold, and the mean number of medical comorbidities was 2.
HRS was approved by the University of Michigan Institutional Review Board, and all participants provided informed consent.
Measures
Sleep quality.
Perceived sleep quality was assessed in 2008. Participants were asked, “How often do you feel really rested when you wake up in the morning?” Based on the distribution of responses to this item, we grouped respondents into three categories: (1) most of the time or always (reference group), (2) sometimes rested, and (3) rarely or never rested. Prior studies have used restless sleep as a proxy for sleep quality when there is a lack of other sleep domains available (Burgard and Ailshire, 2009; Leggett et al., 2016).
Coping behavior.
In 2008, HRS included a module that assessed coping behavior within a random sub-sample of study participants (Mezuk et al., 2017). Adapted from questions originally used in the National Survey of Black Americans (Jackson and Gurin, 1987), the module included eight coping behaviors: drinking alcohol, drug or medication use, overeating, smoking, exercise, prayer, social support, and professional help. First, it asked respondents to think about “things you are most likely to do after having what you think is a stressful event or day” (emphasis in original). Next, it asked, “How often do you use [behavior] to help make it easier to bear?” with responses coded using a 5-point Likert-type scale ranging from never to very often.
In this study, the Likert-type scoring was used to dichotomize coping behaviors based on the degree to which an individual depended on each behavior in response to stress, relative to the population distribution. We considered individuals who fell in the weighted bottom 25th percentile not to be dependent on a certain coping behavior in response to stress, whereas we considered those above the weighted 25th percentile as dependent. We used the following cut points for each coping behavior:
Drink alcohol. Never, hardly ever, not too often, or fairly often (reference group) versus very often;
Take medication or use drugs (over-the-counter, prescription, or illicit drug use was not specified). Never, hardly ever, not too often, or fairly often (reference group) versus very often;
Overeat. Never, hardly ever, or not too often (reference group) versus fairly often or very often;
Smoke tobacco. Never, hardly ever, not too often, or fairly often (reference group) versus very often;
Exercise. Never, hardly ever, or not too often (reference group) versus fairly often or very often;
Pray. Never (reference group) versus hardly ever, not too often, fairly often, or very often;
Seek advice from social network (i.e. social support). Never or hardly ever (reference group) versus not too often, fairly often, or very often;
Seek treatment from a health professional. Never, hardly ever, not too often, or fairly often (reference group) versus very often.
Depression.
HRS used the Composite International Diagnostic Interview short form (CIDI-SF) to assess history of major depression (MD) over the previous 12 months. The CIDI-SF is based on criteria for MD set by the Diagnostic and Statistical Manual of Mental Disorders (DSM; American Psychiatric Association, 2013), which requires that respondents endorse either anhedonia or depressed mood for most of the day for most of a 2-week period or more. When compared to semi-structured interviews, the CIDI-SF has a 70 percent sensitivity and 90 percent specificity for diagnosing MD episode (Aalto-Setälä et al., 2002). Those who met this criterion completed an additional seven symptoms: lost interest, feeling tired, change in weight, trouble with sleep, trouble concentrating, feeling down, and thoughts of death. Those with a score ⩾3 were considered to meet criteria for having MD in the previous 12 months. MD symptomatology scores ranged from 0 to 7 (Steffick, 2000).
Covariates.
Demographic characteristics included gender (female, male), race/ethnicity (non-Hispanic White, non-Hispanic Black, other), marital status (married, separated or divorced, widowed, single or never married), and age. Individuals were grouped by age into categories based on trends that occur in older adulthood, such as retirement, functional impairment, and independent living transitions (Anstey et al., 2006; Black and Rush, 2002; Fields, 2016; Garner et al., 2018; Thane, 2006; Young et al., 2015). Socioeconomic characteristics included educational attainment (<high school, high school degree or equivalent, some college, college degree or above); current income-to-poverty ratio (IPR) category, a measure of income that accounts for household size (categorized as <1.00, 1.00 to <2.00, 2.00 to <3.00, 3.00 to <4.00, 4.00 to <5.00, ⩾5.00), and; household wealth. Household wealth was defined as the sum net value of primary residence, secondary residence, real estate, vehicles, businesses, IRA/Keogh, stocks and mutual funds, checking accounts, savings accounts, money market accounts, CDs, government savings bonds, treasury bills, bonds or bond funds, and all other savings; minus the net value of all mortgages, other home loans, the balance on an equity line of credit, and any other debt. Finally, analyses also accounted for number of medical comorbidities and functional limitations. Number of medical comorbidities was created by summing the number of lifetime conditions and ranged from 0 to 8: (1) hypertension; (2) diabetes; (3) cancer or malignant tumor of any kind except skin cancer; (4) chronic lung disease except asthma such as chronic bronchitis or emphysema; (5) heart attack, coronary heart disease, angina, congestive heart failure or other heart problem (6) stroke or transient ischemic attack; (7) emotional, nervous or psychiatric problems, and; (8) arthritis or rheumatism. Functional limitations were defined as reporting at least some difficulty with one or more activities of daily living, including bathing, eating, dressing, walking across a room or getting in or out of bed. Besides educational attainment, which was assessed when an individual first enrolled in HRS, all covariates were measured in 2008.
Approach
Initially, we used weighted univariate statistics and bivariate regression to describe the sample characteristics by perceived sleep quality. Next, we used multivariable logistic regression to assess the cross-sectional relationship between perceived sleep quality and each of the eight coping behaviors. The longitudinal relationship between perceived sleep quality in 2008 and MD in 2010 was assessed using multivariate logistic regression, which controlled for MD in 2008.
Path analysis, a type of structural equation modeling (Jeon, 2015), was used to examine whether coping behaviors mediated the relationship of perceived sleep quality with MD symptomatology. Assumptions of conducting path analysis in Stata/SE require that variables be either binary or continuous (i.e. ⩾5 categories). Thus, we elected to treat perceived sleep quality as a binary variable: waking rested most of the time or always versus sometimes, rarely, or never. To test the robustness of this cut point, sensitivity analyses modeled perceived sleep quality (1) using a different cut point (waking rested most of the time, always or sometimes vs rarely or never) and (2) treating it as continuous. Coping behaviors were also modeled as binary variables, as described above. MD symptomatology was modeled as a continuous measure. We included binary covariates in the model where appropriate (e.g. gender) and created dummy variables for covariates with more than two categories (e.g. age group, race/ethnicity, marital status). We adjusted the path between perceived sleep quality and each coping behavior for gender, age group, race/ethnicity, marital status, educational attainment, IPR, household wealth, functional limitations, and number of medical comorbidities. We included the same covariates in the path between perceived sleep quality in 2008 and MD symptomatology in 2010. In addition, the path between 2008 perceived sleep quality and 2010 MD symptomatology adjusted for MD symptomatology in 2008.
The sample size for this study (n = 1174) is a function of the number of individuals who participated in HRS experimental modules; however, post hoc analyses reveal that our analyses were sufficiently powered. In the analysis sample, the prevalence of poor perceived sleep quality—when defined as those waking rested sometimes, rarely, or never versus waking rested most of the time or always—is 38.9 percent, and the proportion of those who meet criteria for MD using the CIDI-SF is 68.4 percent for those with poor perceived sleep quality, and 31.6 percent for those without poor perceived sleep quality. Therefore, testing associations between perceived sleep quality and CIDI-SF MD symptomatology with a 0.05 type I error and a 0.20 type II error would require a total of 70 persons. The large sample size in this study permits adjustment for multiple covariates as well as mediation analyses.
Descriptive and logistic regression models were estimated using SAS software version 9.4 (SAS Institute Inc., 2013) and path models were fit using Stata/SE version 15.0 (StataCorp, 2017). For all analyses, survey analytic methods were used to account for HRS's complex survey design.
Results
Approximately 11 percent of the sample had poor perceived sleep quality, defined as rarely/never waking up rested. Table 1 shows the descriptive characteristics of the sample stratified by perceived sleep quality. Those with poor perceived sleep quality had less education and lower IPR relative to those with better quality sleep. The proportion of the analysis sample who met criteria for MD was 8 percent in 2008, and 9 percent in 2010. In addition, MD was more common among those who rarely/never woke rested compared to those who always/most of the time woke rested (24% vs 5%, respectively).
Table 1.
Bivariate descriptive statistics by sleep quality, HRS.a
| Characteristics | Total (n = 1174) | Feel rested in the
morning |
p valueb | ||
|---|---|---|---|---|---|
| Most of the time (n = 717) | Some of the time (n = 332) | Rarely or never (n = 125) | |||
| Female | 697 (55.5) | 415 (54.4) | 199 (56.1) | 83 (59.9) | 0.6167 |
| Age category | 0.1552 | ||||
| 54 to <65 | 379 (48.2) | 210 (45.0) | 119 (51.5) | 50 (56.9) | |
| 65 to <75 | 437 (28.4) | 280 (30.1) | 117 (27.0) | 40 (22.9) | |
| 75 to <85 | 287 (18.4) | 177 (19.2) | 81 (17.9) | 29 (16.3) | |
| 85 to 106 | 71 (5.0) | 50 (5.8) | 15 (3.7) | 6 (4.0) | |
| Race/ethnicity | 0.7883 | ||||
| Non-Hispanic White | 870 (78.9) | 541 (79.4) | 235 (77.4) | 94 (80.5) | |
| Non-Hispanic Black | 169 (10.0) | 103 (10.1) | 53 (11.0) | 13 (7.0) | |
| Other | 135 (11.1) | 73 (10.5) | 44 (11.6) | 18 (12.6) | |
| Marital status | 0.5430 | ||||
| Married | 712 (62.7) | 449 (64.8) | 197 (59.9) | 66 (58.6) | |
| Separated or divorced | 140 (13.6) | 85 (13.3) | 36 (12.9) | 19 (16.7) | |
| Widowed | 230 (15.5) | 136 (15.0) | 67 (16.4) | 27 (16.0) | |
| Single or never married | 92 (8.2) | 47 (6.9) | 32 (10.8) | 13 (8.8) | |
| Baseline educational attainmentc | 0.0059 | ||||
| <High school | 241 (16.2) | 139 (15.4) | 67 (13.7) | 35 (26.4) | |
| High school degree or equivalent | 434 (36.7) | 263 (35.7) | 122 (38.4) | 49 (37.2) | |
| Some college | 253 (22.3) | 149 (20.3) | 80 (26.6) | 24 (21.6) | |
| College degree and above | 246 (24.9) | 166 (28.6) | 63 (21.3) | 17 (14.8) | 0.0101 |
| IPR | 0.0101 | ||||
| <1.00 | 85 (6.9) | 42 (5.3) | 24 (7.2) | 19 (14.6) | |
| 1.00 to <2.00 | 216 (16.0) | 107 (13.1) | 78 (19.6) | 31 (22.2) | |
| 2.00 to <3.00 | 216 (15.6) | 138 (16.0) | 59 (15.3) | 19 (14.3) | |
| 3.00 to <4.00 | 161 (12.8) | 102 (13.0) | 46 (13.0) | 13 (11.3) | |
| 4.00 to <5.00 | 112 (10.7) | 76 (11.1) | 26 (10.4) | 10 (9.7) | |
| 5.00 and above | 384 (37.9) | 252 (41.6) | 99 (34.5) | 33 (27.9) | |
| Household wealth, mean (95% CI) | US$592,329 (508,199–676,460) | US$699,156 (593,179–805,134) | US$483,506 (323,972–643,039) | US$318,365 (194,537–442,193) | <0.0001 |
| Number of medical comorbidities, mean (95% CI) | 2.0 (1.9–2.1) | 1.8 (1.7–1.9) | 2.3 (2.1–2.5) | 2.6 (2.3–2.8) | <0.0001 |
| Functional limitations | 156 (11.4) | 60 (6.6) | 58 (14.6) | 38 (27.8) | <0.0001 |
| Coping behaviors in response to psychosocial stress | |||||
| Drink alcohol | 0.8975 | ||||
| Never | 1131 (78.0) | 579 (77.2) | 270 (77.6) | 103 (75.0) | |
| Hardly to very often | 249 (22.0) | 138 (22.8) | 62 (22.4) | 22 (25.0) | |
| Use drugs | <0.0001 | ||||
| Never | 1169 (84.5) | 648 (90.7) | 262 (80.8) | 88 (68.0) | |
| Hardly to very often | 211 (15.5) | 69 (9.3) | 70 (19.2) | 37 (32.0) | |
| Smoke | 0.2800 | ||||
| Never | 1264 (89.9) | 661 (90.6) | 303 (89.2) | 108 (84.6) | |
| Hardly to very often | 116 (10.1) | 56 (9.4) | 29 (10.8) | 17 (15.4) | |
| Overeat | 0.0077 | ||||
| Never or hardly | 1103 (78.3) | 592 (81.5) | 244 (72.3) | 93 (71.5) | |
| Not often to very often | 277 (21.7) | 125 (18.5) | 88 (27.7) | 32 (28.5) | |
| Exercise | 0.4931 | ||||
| Never or hardly | 1167 (81.8) | 604 (81.8) | 272 (78.5) | 107 (84.0) | |
| Not often to very often | 213 (18.2) | 113 (18.2) | 60 (21.5) | 18 (16.0) | |
| Pray | 0.0026 | ||||
| Never to fairly often | 787 (58.2) | 431 (62.6) | 164 (51.8) | 63 (45.6) | |
| Very often | 593 (41.8) | 286 (37.4) | 168 (48.2) | 62 (54.4) | |
| Seek advice from friends or family | 0.7515 | ||||
| Never to not often | 1106 (80.3) | 581 (80.0) | 252 (79.0) | 99 (76.9) | |
| Fairly or very often | 274 (19.7) | 136 (20.0) | 80 (21.0) | 26 (23.1) | |
| Seek help from a health care professional | 0.1755 | ||||
| Never | 1111 (80.2) | 578 (80.7) | 262 (79.7) | 94 (72.5) | |
| Hardly to very often | 269 (19.8) | 139 (19.3) | 70 (20.3) | 31 (27.5) | |
| Met criteria for having a major depressive episoded | |||||
| 2008 | 91 (8.0) | 34 (5.0) | 27 (7.9) | 30 (23.8) | <0.0001 |
| 2010 | 90 (8.6) | 33 (4.6) | 29 (10.7) | 28 (23.8) | <0.0001 |
IPR: income-to-poverty ratio; CI: confidence interval; HRS: Health and Retirement Study.
HRS, data collected in 2008 unless otherwise indicated.
χ2 or F test.
Educational attainment assessed during first cycle respondent participated in HRS.
Score ⩾3 in the Composite International Diagnostic Interview Short Form (CIDI-SF).
Table 2 presents odds ratios (ORs) and 95 percent confidence intervals (CIs) for the associations of perceived sleep quality with the eight coping behaviors. In adjusted models, poor perceived sleep quality was associated with greater odds of using drugs/medications to cope with stress (ORrarely or never wake rested = 2.9; 95% CI = 1.4–6.0) and overeating to cope with stress (ORsometimes wake rested= 1.6; 95% CI = 1.1–2.5). Perceived sleep quality was not significantly associated with drinking alcohol, smoking tobacco, exercising, seeking social support, or seeking treatment from a health professional to cope with stress.
Table 2.
Odds ratios (ORs) and 95 percent confidence intervals (CIs) for the association of waking rested with coping behaviors,a HRS 2008.
| Self-regulatory coping behavior | Crude |
Adjustedb |
||
|---|---|---|---|---|
| Sometimes | Rarely or never | Sometimes | Rarely or never | |
| Drink alcohol | 1.0 (0.7–1.4) | 1.1 (0.6–2.2) | 1.0 (0.7–1.4) | 1.2 (0.6–2.2) |
| Take medication or use drugs | 2.3*** (1.4–3.8) | 4.6*** (2.4–9.0) | 1.7* (1.1–2.8) | 2.9* (1.4–6.0) |
| Smoke tobacco | 1.2 (0.7–2.1) | 1.7 (0.9–3.5) | 1.0 (0.5–1.8) | 1.2 (0.5–2.9) |
| Overeat | 1.7* (1.2–2.5) | 1.8* (1.0–3.0) | 1.6* (1.1–2.5) | 1.5* (0.9–2.8) |
| Exercise | 1.2 (0.8–1.9) | 0.9 (0.4–1.7) | 1.3 (0.8–1.9) | 0.9 (0.4–2.1) |
| Pray | 1.6** (1.1–2.2) | 2.0** (1.3–3.2) | 1.4 (0.9–2.1) | 1.4 (0.9–2.1) |
| Social support | 1.1 (0.7–1.5) | 1.2 (0.7–2.1) | 0.9 (0.6–1.4) | 0.9 (0.5–1.8) |
| Treatment from health professional | 1.1 (0.7–1.6) | 1.6 (0.9–2.7) | 0.9 (0.6–1.4) | 1.3 (0.7–2.4) |
HRS: Health and Retirement Study.
Logistic regressions, each behavior tested as an outcome in separate models (n = 1178).
Accounts for gender, age, race/ethnicity, marital status, educational attainment, income-to-poverty ratio category, household wealth, functional limitations, and number of medical comorbidities.
Type III p < 0.05;
Type III p < 0.005;
Type III p < 0.0005.
We then examined the longitudinal relationship between perceived sleep quality and MD. Table 3 presents the association between 2008 perceived sleep quality and 2010 MD, accounting for MD in 2008. In the adjusted model, there was a dose–response relationship between poor perceived sleep quality and MD (ORsometimes wake rested = 2.1 (95% CI = 1.0–4.5); and ORrarely or never wake rested = 4.8 (95% CI = 1.5–9.6)). When including coping behaviors in the adjusted model the magnitude of associations remained consistent.
Table 3.
Odds ratios and 95 percent confidence intervals for relationship of sleep quality with symptoms of major depressiona and mediation by self-regulatory coping behavior, HRS 2008 and 2010b.
| Frequency of waking up rested | Crude | Adjustedc | Mediation by coping behaviorsd |
|---|---|---|---|
| Always | Ref. | Ref. | Ref. |
| Sometimes | 2.5*** (1.3–4.7) | 2.1* (1.0–4.5) | 2.0* (1.0–4.2) |
| Rarely or never | 6.5*** (3.2–13.2) | 3.8* (1.5–9.6) | 3.9* (1.6–9.9) |
HRS: Health and Retirement Study.
Measured in 2010 using the Composite Interview Diagnostic Short Form (CIDI-SF), those with a symptom score ⩾3 were considered to meet criteria for having a major depressive episode.
n = 1174.
Accounts for 2008 depression status, gender, age, race/ethnicity, marital status, educational attainment, income-to-poverty ratio category, household wealth, functional limitations, and number of medical comorbidities.
In addition to the covariates included in the adjusted model, this model examines mediation by self-regulatory coping behaviors and includes binary measures of high dependence (⩾75th percentile vs <75th percentile (reference)) on taking medication or using drugs, drinking alcohol, smoking tobacco, overeating, prayer, seeking social support, or seeking treatment from a health care professional when dealing with stressful life events.
Type III p < 0.05;
Type III p < 0.0005.
Figure 1 presents results of the path analysis for 2010 symptoms of a MD episode over the previous 12 months. Parameter estimates (βs) represent direct effects. As expected, perceived sleep quality in 2008 was associated with MD symtomatology in 2010 (β = 0.35; 95% CI = 0.08–0.62). In addition, consistent with regression results in Table 2, poor perceived sleep quality was associated with using drugs/medication (β = 0.09; 95% CI = 0.03–0.14) and overeating (β = 0.09; 95% CI = 0.03–0.15). Poor perceived sleep quality was also associated with prayer (β = 0.09; 95% CI = 0.01–0.17) to cope with stress. However, in this model, none of the coping behaviors were associated with MD symtomatology. Consistent with this null effect, the mediation analysis indicated that coping behavior did not mediate the relationship of 2008 perceived sleep quality with 2010 MD symtomatology (11.0%, 95% CI = −3.5 to 25.5; p = 0.14). Regardless of how sleep quality was treated in path analyses (i.e. sensitivity analyses that used (1) a different cut point for binary perceived sleep quality and (2) perceived sleep quality as a 3-level continuous variable), coping behaviors did not mediate the relationship of sleep quality with MD symtomatology.
Figure 1.
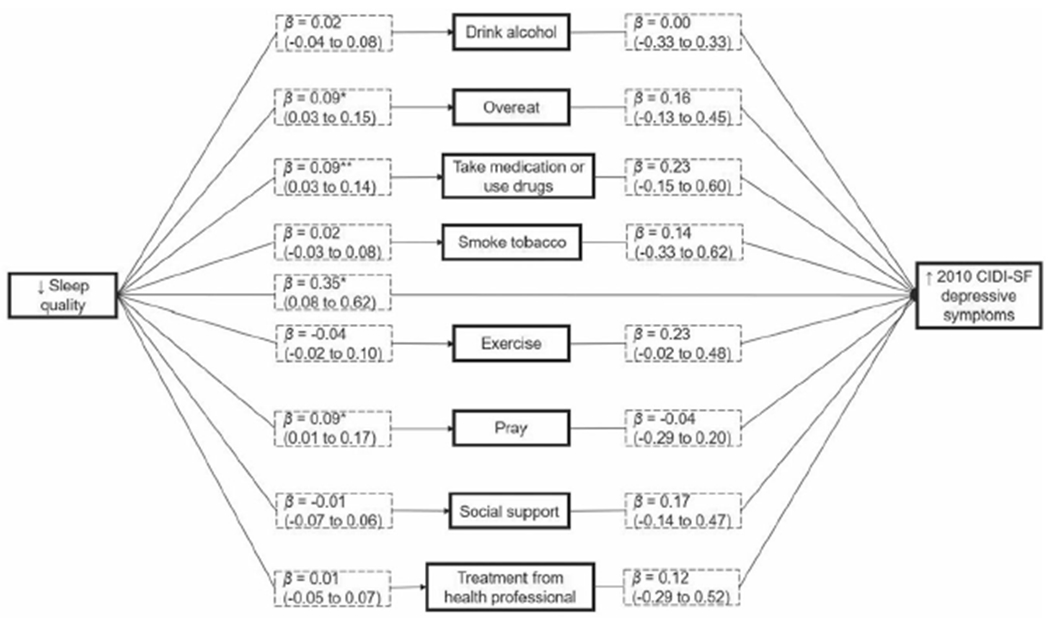
Mediation of the association between 2008 sleep quality and 2010 symptoms of a depressive episode in previous 12 months. Data come from the Health and Retirement Study, cycles 2008 and 2010 (n = 1174). Parameter estimates (βs) were generated using path analysis in Stata/SE v. 15.0; represent direct effects with 95% confidence intervals (CIs). Paths between sleep quality and each coping behavior were adjusted for age group, gender, race/ethnicity, marital status, educational attainment, income-to-poverty ratio category, household wealth, functional limitations, and number of medical comorbidities. These same covariates were accounted for in the path between 2008 sleep quality and 2010 depression symptoms, in addition to depression symptoms in 2008. Coping behaviors explained 11.0% (95% CI = −3.5 to 25.5) of the association between sleep quality in 2008, and depression symptoms in 2010. Depression symptoms measured using the Composite International Diagnostic Interview Short Form (CIDI-SF) and scores range from 0 to 7.
*p < 0.05; **p < 0.005.
Discussion
In this representative sample of older US adults, approximately 11% reported poor perceived sleep quality, indicated by rarely or never waking up rested. Our findings indicated that perceived sleep quality was associated with specific coping behaviors in older adults, including using medications/drugs, overeating, and praying. However, these coping behaviors were not associated with subsequent MD symtomatology and, therefore, did not mediate the relationship of perceived sleep quality with MD symtomatology. This suggests that the increased risk of MD due to poor perceived sleep quality among older adults is not attributable to coping behavior.
Results from this study are partially consistent with prior findings. In our sample, those with poor sleep were more likely to report using medications/drugs to cope with stress. Similarly, in a national sample of US adults, poor sleep was associated with greater misuse of sleep aid medications (Albert et al., 2017). Our observation that overeating in response to stress was more common among those with poor sleep is also consistent with prior brain imaging evidence, which demonstrates that sleep deprivation stimulates brain processes associated with the desire to consume food (Benedict et al., 2012). However, findings are less consistent with studies that specifically examined the influence of sleep quality on behaviors in response to stress. For example, Palagini et al. (2016) reported insomnia symptoms (measured using self-report on a severity index) were not associated with either religion or substance use (i.e. alcohol or other drugs) to cope with stress. And, among Japanese adults, both smoking and drinking alcohol were associated with sleep disorders (Otsuka et al., 2017). Inconsistencies across studies may be due to variation in how sleep and coping behaviors were measured. In addition, coping behaviors in response to sleep may be distinct between subpopulations (e.g. adult patients with hypertension vs older adults).
These findings provide insight concerning the influence of perceived sleep quality on coping behavior. Poor perceived sleep quality was associated with greater medication/drug use and overeating to cope with stress. Poor perceived sleep quality was also associated with using prayer to cope with stress in mediation analyses. Despite overeating potentially providing a short-term mental health benefit (Pecoraro et al., 2004), there are negative implications over the long-term. In a study of adolescent females, emotional eating has been associated with an impaired ability to identify and adaptively cope with emotional states among adults and adolescents (Gianini et al., 2013; Masheb and Grilo, 2006). Prayer may provide both short- and long-term health benefits. While prayer may not change an individual’s circumstances, prayer can combat the negative effects of experiencing trauma and acute stress, possibly mediated by increased feelings of calm and/or optimism (Ai et al., 2007; Harris et al., 2010). In addition, prayer may function through similar pathways to those of mindfulness-based therapies, such as meditation, which has been associated with improved outcomes for those with a number of conditions including mood disorders, epilepsy, and cancer (Arias et al., 2006; Ott et al., 2006). Assessment of medication/drug use in HRS was not specific and simultaneously captured use and abuse of over-the-counter medication, prescribed medication, and illicit drugs. This makes it challenging to assess potential health implications of this coping behavior.
Of note, this study did not find that coping behavior mediates the relationship between perceived sleep quality and MD symptomatology. Despite associations of poor sleep with certain coping behaviors, the actual amount of time that certain individuals engage in specific coping behaviors may be more dependent on other social or socioeconomic stressors. Future research may incorporate perceptions of stress exposure (e.g. duration, frequency, source) when assessing associations of perceived sleep quality, coping behavior, and MD. In addition, while certain coping behaviors have long-term negative impacts on physical health (e.g. smoking and risk of cancer, overeating and development of diabetes), these same behaviors may have short-term positive impacts on mental health (Mezuk et al., 2013). For example, nicotine has been shown to reduce stress reactivity among regular smokers (Rohleder and Kirschbaum, 2006). In addition, high fat/high sugar foods reduce the production of stress hormones in the brains of rats (Pecoraro et al., 2004). Specific to MD, several studies demonstrate that engaging in “poor” health behaviors (e.g. smoking, poor diet, drinking) under high levels of stress can reduce MD longitudinally when compared to not engaging in these behaviors (Jackson et al., 2010; Mezuk et al., 2010).
It is important to note that the relatively null findings reported here may reflect the older age of the sample. The relationship between perceived sleep quality and stress reactivity decreases from midlife to late-life (Blaxton et al., 2017). Furthermore, older adults may be better able to neutrally or positively reframe life circumstances (Benyamini et al., 2000), consistent with the theory of positivity effect (Mather and Carstensen, 2005). Daily life events tend to have a weaker impact on depressive symptoms among older adults versus younger adults (Whitehead and Bergeman, 2014). Older adults also have more functional limitations and medical conditions that can interfere with sleep quality and depressive symptoms, which may mask any relationship between these variables and coping behaviors.
Limitations
Given that both perceived sleep quality and coping behavior were measured at the same timepoint in our analyses, it is possible that inherent preference (e.g. personality) for certain coping behaviors at the time of a stressful life event can influence sleep (McCrae and Costa, 1986). For example, coping behavior among men who were recently diagnosed with cancer predicted severity of sleep disturbances and interference with daily tasks due to sleep problems (Hoyt et al., 2009). Specifically, men who reported avoidance-oriented coping (e.g. denial of illness severity or decreasing contact with social networks) versus task-oriented coping (e.g. problem solving to address treatment side effects or expressing emotions to social networks) were more likely to have sleep problems six months later. Similarly, in a small study of women with breast cancer and men with prostate cancer, avoidance-oriented coping during radiation therapy was also associated with poorer rated sleep at six-months follow-up (Thomas et al., 2010).
Use of a single item to measure perceived sleep quality in the 2008 HRS wave is also a limitation. However, in 2010, HRS assessment of sleep quality was more comprehensive. In addition to asking respondents how often they woke rested—as in 2008—respondents were asked how often they (1) have trouble falling asleep, (2) have trouble with waking up during the night, and (3) have trouble with waking up too early and not being able to fall asleep again. Each item was scored using the same 3-point Likert-type scale. The correlation of respondent scores in 2010 for the single “sleeping rested” item with sleep quality based on all four items was 0.68, suggesting a moderate to high agreement within individuals and that minimal information is lost when using the single sleep quality item. Links between MD and sleep quality are bidirectional (Kahn et al., 2013). Therefore, to further assess the validity of using a single item to ascertain sleep quality we confirmed that depression in 2008 was associated with poorer perceived sleep quality in 2010 within HRS (Supplemental Table 1). Finally, there may be residual confounding by other indicators of socioeconomic status beyond those addressed in this study (e.g. access to amenities, area-level poverty, cost of living).
Conclusion
Poor perceived sleep quality was associated with specific coping behaviors among older adults. However, the prospective association of poor perceived sleep quality with MD was not mediated by coping behavior. Further research should consider perceptions of stress (e.g. frequency, duration, and source) as well as other health outcomes sensitive to coping behavior (e.g. substance abuse, cardiovascular health).
Supplementary Material
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Mental Health (grant number T32 MH73553) to R.S.B., a grant from the American Diabetes Association (1-16-ICTS-082) to B.M., and a grant from the Department of Veterans Affairs (IIR 14-324) to K.Z.
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental material
Supplemental material for this article is available online.
References
- Aalto-Setälä T, Haarasilta L, Marttunen M, et al. (2002) Major depressive episode among young adults: CIDI-SF versus SCAN consensus diagnoses. Psychological Medicine 32(7): 1309–1314. [DOI] [PubMed] [Google Scholar]
- Ai AL, Peterson C, Tice TN, et al. (2007) The influence of prayer coping on mental health among cardiac surgery patients: The role of optimism and acute distress. Journal of Health Psychology 12(4): 580–596. [DOI] [PubMed] [Google Scholar]
- Albert SM, Roth T, Toscani M, et al. (2017) Sleep health and appropriate use of OTC sleep aids in older adults—Recommendations of a Gerontological Society of America Workgroup. The Gerontologist 57(2): 163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (5th edn). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Anstey KJ, Windsor TD, Luszcz MA, et al. (2006) Predicting driving cessation over 5 years in older adults: Psychological well-being and cognitive competence are stronger predictors than physical health. Journal of the American Geriatrics Society 54(1): 121–126. [DOI] [PubMed] [Google Scholar]
- Arias AJ, Steinberg K, Banga A, et al. (2006) Systematic review of the efficacy of meditation techniques as treatments for medical illness. The Journal of Alternative and Complementary Medicine 12(8): 817–832. [DOI] [PubMed] [Google Scholar]
- Benedict C, Brooks SJ, O’Daly OG, et al. (2012) Acute sleep deprivation enhances the brain’s response to hedonic food stimuli: An fMRI study. The Journal of Clinical Endocrinology and Metabolism 97(3): E443–E447. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Idler EL, Leventhal H, et al. (2000) Positive affect and function as influences on self-assessments of health: Expanding our view beyond illness and disability. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 55(2): P107–P116. [DOI] [PubMed] [Google Scholar]
- Black SA and Rush RD (2002) Cognitive and functional decline in adults aged 75 and older. Journal of the American Geriatrics Society 50(12): 1978–1986. [DOI] [PubMed] [Google Scholar]
- Blaxton JM, Bergeman CS, Whitehead BR, et al. (2017) Relationships among nightly sleep quality, daily stress, and daily affect. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 72(3): 363–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgard SA and Ailshire JA (2009) Putting work to bed: Stressful experiences on the job and sleep quality. Journal of Health and Social Behavior 50(4): 476–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chasens ER, Sereika SM, Weaver TE, et al. (2007) Daytime sleepiness, exercise, and physical function in older adults. Journal of Sleep Research 16(1): 60–65. [DOI] [PubMed] [Google Scholar]
- Cousson-Gélie F, Cosnefroy O, Christophe V, et al. (2010) The Ways of Coping Checklist (WCC): Validation in French-speaking cancer patients. Journal of Health Psychology 15(8): 1246–1256. [DOI] [PubMed] [Google Scholar]
- Fields NL (2016) Exploring the personal and environmental factors related to length of stay in assisted living. Journal of Gerontological Social Work 59(3): 205–221. [DOI] [PubMed] [Google Scholar]
- Foley DJ, Monjan AA, Brown SL, et al. (1995) Sleep complaints among elderly persons: An epidemiologic study of three communities. Sleep 18(6): 425–432. [DOI] [PubMed] [Google Scholar]
- Garner R, Tanuseputro P, Manuel DG, et al. (2018) Transitions to long-term and residential care among older Canadians. Health Reports 29(5): 13–23. [PubMed] [Google Scholar]
- Gianini LM, White MA and Masheb RM (2013) Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eating Behaviors 14(3): 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JI, Erbes CR, Engdahl BE, et al. (2010) Coping functions of prayer and posttraumatic growth. The International Journal for the Psychology of Religion 20(1): 26–38. [Google Scholar]
- Hoyt MA, Thomas KS, Epstein DR, et al. (2009) Coping style and sleep quality in men with cancer. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine 37(1): 88–93. [DOI] [PubMed] [Google Scholar]
- Jackson JS and Gurin G (1987) National Survey of Black Americans, 1979-1980. Ann Arbor, MI: Inter-University Consortium for Political and Social Research. [Google Scholar]
- Jackson JS, Knight KM and Rafferty JA (2010) Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health 100(5): 933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaussent I, Bouyer J and Ancelin ML (2011) Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep 34(8): 1103–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon J (2015) The strengths and limitations of the statistical modeling of complex social phenomenon: Focusing on SEM, path analysis, or multiple regression models. World Academy of Science, Engineering and Technology, International Journal of Social Behavioral Educational, Economic, Business and Industrial Engineering 9: 1597–1605. [Google Scholar]
- Kahn M, Sheppes G and Sadeh A (2013) Sleep and emotions: Bidirectional links and underlying mechanisms. International Journal of Psychophysiology 89(2): 218–228. [DOI] [PubMed] [Google Scholar]
- Landry GJ, Best JR and Liu-Ambrose T (2015) Measuring sleep quality in older adults: A comparison using subjective and objective methods. Frontiers in Aging Neuroscience 7: 166. Available at: https://www.frontiersin.org/articles/10.3389/fnagi.2015.00166/full (accessed 2 July 2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS and Folkman S (1984) Stress, Appraisal, and Coping. New York: Springer publishing company. [Google Scholar]
- Leggett A, Burgard S and Zivin K (2016) The impact of sleep disturbance on the association between stressful life events and depressive symptoms. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 71(1): 118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae RR and Costa PT (1986) Personality, coping, and coping effectiveness in an adult sample. Journal of Personality 54(2): 385–404. [Google Scholar]
- Masheb RM and Grilo CM (2006) Emotional overeating and its associations with eating disorder psychopathology among overweight patients with Binge eating disorder. International Journal of Eating Disorders 39(2): 141–146. [DOI] [PubMed] [Google Scholar]
- Mather M and Carstensen LL (2005) Aging and motivated cognition: The positivity effect in attention and memory. Trends in Cognitive Sciences 9(10): 496–502. [DOI] [PubMed] [Google Scholar]
- Meerlo P, Sgoifo A and Suchecki D (2008) Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Medicine Reviews 12(3): 197–210. [DOI] [PubMed] [Google Scholar]
- Mezuk B, Rafferty JA, Kershaw KN, et al. (2010) Reconsidering the role of social disadvantage in physical and mental health: Stressful life events, health behaviors, race, and depression. American Journal of Epidemiology 172(11): 1238–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B, Abdou CM, Hudson D, et al. (2013) “White box” epidemiology and the social neuroscience of health behaviors: The environmental affordances model. Society and Mental Health. Epub ahead of print 1 July. DOI: 10.1177/2156869313480892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B, Ratliff S, Concha JB, et al. (2017) Stress, self-regulation, and context: Evidence from the health and retirement survey. SSM—Population Health 3: 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman AB, Spiekerman CF, Enright P, et al. (2000) Daytime sleepiness predicts mortality and cardiovascular disease in older adults. Journal of the American Geriatrics Society 48(2): 115–123. [DOI] [PubMed] [Google Scholar]
- Otsuka Y, Kaneita Y, Itani O, et al. (2017) Relationship between stress coping and sleep disorders among the general Japanese population: A nationwide representative survey. Sleep Medicine 37: 38–45. [DOI] [PubMed] [Google Scholar]
- Ott MJ, Norris RL and Bauer-Wu SM (2006) Mindfulness meditation for oncology patients: A discussion and critical review. Integrative Cancer Therapies 5(2): 98–108. [DOI] [PubMed] [Google Scholar]
- Palagini L, Bruno RM, Cheng P, et al. (2016) Relationship between insomnia symptoms, perceived stress and coping strategies in subjects with arterial hypertension: Psychological factors may play a modulating role. Sleep Medicine 19: 108–115. [DOI] [PubMed] [Google Scholar]
- Pecoraro N, Reyes F, Gomez F, et al. (2004) Chronic stress promotes palatable feeding, which reduces signs of stress: Feedforward and feedback effects of chronic stress. Endocrinology 145(8): 3754–3762. [DOI] [PubMed] [Google Scholar]
- Rohleder N and Kirschbaum C (2006) The hypothalamic-pituitary-adrenal (HPA) axis in habitual smokers. International Journal of Psychophysiology 59(3): 236–243. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. (2013) SAS Software, version 9.4. Available at: https://www.sas.com/en_us/software/sas9.html [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, et al. (2014) Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology 43(2): 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Späth-Schwalbe E, Gofferje M, Kern W, et al. (1991) Sleep disruption alters nocturnal ACTH and cortisol secretory patterns. Biological Psychiatry 29(6): 575–584. [DOI] [PubMed] [Google Scholar]
- Stalder T and Kirschbaum C (2013) Cortisol. In: Gellman MD and Turner JR (eds) Encyclopedia of Behavioral Medicine. New York: Springer, pp. 507–512. [Google Scholar]
- StataCorp (2017) Stata Statistical Software: Release 15. College Station, TX: StataCorp. [Google Scholar]
- Steffick D (2000) Documentation of Affective Functioning Measures in the Health and Retirement Study. Available at: http://hrsonline.isr.umich.edu/sitedocs/userg/dr-005.pdf [Google Scholar]
- Ströhle A (2008) Physical activity, exercise, depression and anxiety disorders. Journal of Neural Transmission 116(6): 777–784. [DOI] [PubMed] [Google Scholar]
- Thane P (2006) The history of retirement. In: Clark GL, Munnell AH and Orszag JM (eds) The Oxford Handbook of Pensions and Retirement Income. Oxford: Oxford University Press, pp. 33–51. [Google Scholar]
- Thomas KS, Bower J, Hoyt MA, et al. (2010) Disrupted sleep in breast and prostate cancer patients undergoing radiation therapy: The role of coping processes. Psycho-Oncology 19(7): 767–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unützer J and Park M (2012) Strategies to improve the management of depression in primary care. Primary Care 39(2): 415–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade TD and Kendler KS (2000) The relationship between social support and major depression: Cross-sectional, longitudinal, and genetic perspectives. The Journal of Nervous and Mental Disease 188(5): 251–258. [DOI] [PubMed] [Google Scholar]
- Whitehead BR and Bergeman CS (2014) Ups and downs of daily life: Age effects on the impact of daily appraisal variability on depressive symptoms. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 69(3): 387–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young Y, Kalamaras J, Kelly L, et al. (2015) Is aging in place delaying nursing home admission? Journal of the American Medical Directors Association 16(10): 900.e1–900.e6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


