Background
Fear of cancer recurrence (FoR)1 is common2 and eHealth intervention research targeting FoR has been identified as a priority.3 User-based approaches for eHealth intervention development increase usability, adherence, and efficacy.4 The purpose of this study was to develop and refine “FoRtitude,” a targeted eHealth intervention for FoR through employing user-centered design methodologies, ultimately to yield a refined intervention for a subsequent randomized efficacy trial (ClinicalTrials.gov NCT03384992).
FoRtitude eHealth Intervention
FoRtitude, previously described in detail5, was designed based on clinical experience (LIW) tailoring CBT-based coping strategies for the management of FoR. FoRtitude included a web-based program with an interactive mobile text messaging feature, designed to translate three CBT coping strategies (Relaxation, Cognitive restructuring, Worry practice) from clinician-delivered to an internet-delivered format. The FoRtitude website consisted of didactic content and interactive tools designed to promote use of coping skills targeted to FoR, provided through text-based content, videos, audio-recordings, and graphic images. An interactive text messaging feature allowed BCS to request telephone-based text messages with reminders of how to use the three coping strategies to reduce FoR.
Methods
Using the Behavioral Intervention Technology (BIT) model,6 we conducted a mixed-methods study to systematically collect data from breast cancer survivors (BCS; N=17) with clinically significant FoR to inform iterative development and refinement of FoRtitude in three phases: (1) Content review; (2) Usability testing; and (3) Field testing. Eligibility criteria matched inclusion criteria for the subsequent randomized trial and included female sex, Stage I-III breast cancer, 1–15 years post-completion of treatment, no current evidence of cancer, fluency in English, clinically significant FoR (Fear of Cancer Recurrence Inventory severity subscale score ≥137), internet familiarity, and access to a mobile telephone with short message service (SMS) text messaging capabilities. BCS were recruited through clinics at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University or through word of mouth (“snowball sampling”). This project was approved by the Institutional Review Board of Northwestern University. Participants provided written or online informed consent.
FoRtitude content and functionality was informed by our prior web-based intervention research on depression post-cancer treatment.8 Content review: BCS (n=5) were provided with web-based FoRtitude site didactic content, which included psychoeducational materials on FoR and three CBT-based coping strategies (Relaxation, Cognitive Restructuring, Worry practice) and the application of these strategies to reduce FoR. Semi-structured interviews assessed ease of comprehension and relevance (see Supplemental Appendix 1 for interview guide). Site content revisions incorporated BCS’ input prior to Usability testing. Usability testing: BCS (n=4) accessed FoRtitude using a laptop during in-person interviews. A modified “think aloud” exercise with embedded questions about usability of specific site components solicited feedback and suggestions for improvements (see Supplemental Appendix 2 for interview guide). Data informed FoRtitude refinements, which were incorporated prior to field testing. Field testing: BCS (n=8) utilized FoRtitude as intended for the planned FoRtitude efficacy trial. BCS received an email with a weblink to the FoRtitude website with instructions to use FoRtitude 3–4 times per week for 4 weeks. BCS completed up to 4 telephone-based semi-structured interviews to identify technical issues and obtain feedback to improve site content and usability (see Supplemental Appendix 3 for interview guide). To maximize feedback, BCS could elect to participate in weekly interviews or in 1–2 interviews after using the site for 4 weeks.
Data Analysis
Participant characteristics were collated using descriptive statistics. Qualitative interviews were audio-recorded and transcribed. Directed content analysis9 was used to analyze content review and usability interview data. Initial coding in ATLAS.ti (v.7.5) was deductive, using a pre-determined framework based on FoRtitude content areas. Codes were added inductively as themes emerged, then summarized to determine themes. Field testing interview data was analyzed by tabulating and summarizing content for each semi-structured question.
Results
As shown in Figure 1, 52 BCS were approached, 36 (69%) consented, of which 25 met eligibility criteria and 17 participated. Reasons for refusal (n=16, 31% of BCS approached) included being too busy to participate (n=6), lack of interest (n=6), concerns about privacy (n=2), too physical ill (n=1), and desire to avoid reminders of cancer (n=1). Participant demographics are presented in Table 1.
Figure 1.
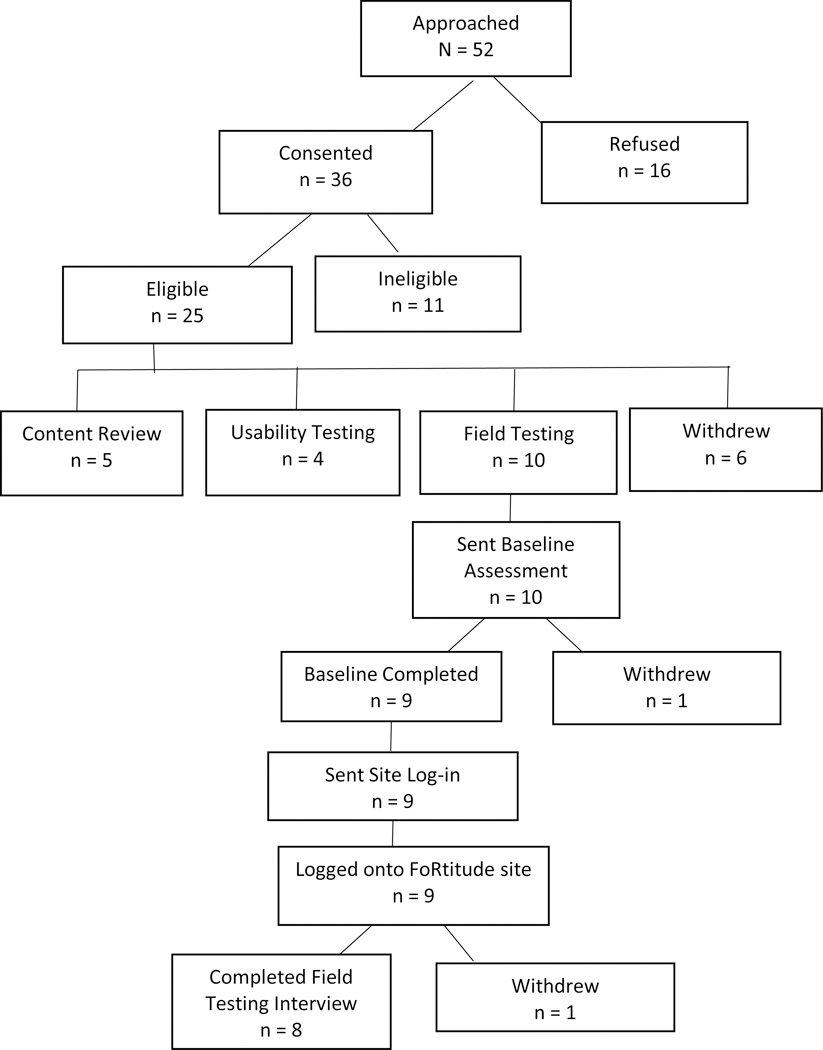
FoRtitude Recruitment (N=17)
Table 1:
FoRtitude Phase I participant demographic characteristics (n=17)
| Demographic characteristic | Value |
|---|---|
| Mean age, in years (standard deviation, range) | 50.6 (8.7; 39–69) |
| Mean time since treatment, in years (standard deviation, range) | 4.2 (3.2; 1.2–13.9) |
| Female sex (n, %), per eligibility | 17 (100.0) |
| Ethnicity (n, %) | |
| Non-Hispanic White | 13 (76.4) |
| Non-Hispanic Black | 1 (5.8) |
| Hispanic Black | 1 (5.8) |
| Non-Hispanic Asian | 2 (11.8) |
| Cancer Stage (n, %) | |
| Stage I | 7 (41) |
| Stage II | 7 (41) |
| Stage III | 3 (18) |
Content Review and Usability Testing
BCS provided positive feedback on FoRtitude with regard to relevance of the content and ease of understanding content. Themes and exemplar quotes from content review and usability testing interviews have been summarized (see online supplemental materials, Table 1). BCS described the recommendation to use FoRtitude daily as too prescriptive, and suggested allowing greater flexibility in frequency and timing of site use.
BCS reported variation in preferences for coping strategies and tools. Most BCS provided positive feedback on the Relaxation tool, which consisted of audio-recorded relaxation exercises (diaphragmatic breathing, progressive muscle relaxation, visual imagery, autogenic training). Variability in exercises available and audio-recordings in female and male voices were helpful. Longer relaxation audio-recordings (20–30 minutes) were not feasible; 10–15 minute exercises were ideal. BCS also cited Relaxation training and diaphragmatic breathing as helpful, due to portability. Most BCS identified Cognitive restructuring and the Thought record tool as helpful for managing FoR. Didactic content was easy to comprehend. ”Real life” examples illustrating application of Cognitive restructuring for managing FoR were cited as helpful. BCS reported mixed feedback on the Worry practice coping strategy and tool. While some BCS reported potential benefit, others anticipated increased worry. BCS identified Worry practice as the most challenging coping strategy because it requires confronting FoR, thus suggested providing Relaxation and Cognitive restructuring first, followed by Worry practice. BCS provided mixed feedback on whether they would utilize interactive text messaging to request text messages with reminders of FoRtitude coping strategies.
BCS suggested many strategies to increase the sense of a “personal connection” through FoRtitude, including adding a social media component to facilitate interactions among BCS to share stories, advice, and experiences using FoRtitude. BCS suggested a “testimonials” page, populated by content from BCS on managing FoR. BCS suggested more details on the study team, including photographs. BCS reported that their physician’s recommendation to use FoRtitude provided additional reassurance that it would be beneficial.
Field Testing
Eight BCS completed field testing (1=4 weekly interviews; 3=3 interviews, 2=2 interviews, 2=1 interview). BCS did not report any problems logging in and utilizing the site. Research staff monitored website use and confirmed field testing participants had accessed and reviewed the site. The most common reasons for not logging in 3–4 times per week included being too busy (n=4) or being away from a computer due to travel (n=4). One BCS reportedly did not use the site due to avoidance (eg. reminder of cancer). BCS described the FoRtitude site as helpful for managing FoR, well organized and easy to use. BCS described Relaxation (n=2), Cognitive restructuring (n=4) and Worry practice (n=1) as helpful. Worry practice also increased anxiety (n=3). Changes were suggested to improve ease of navigation. Suggested modifications to the “My Progress” page included adding graphs of anxiety scores and providing a free text box to allow participants to keep notes on helpful information from the site.
FoRtitude Site Revisions
Qualitative feedback informed iterative modifications to FoRtitude website content and functionality. Revisions to improve ease of navigation included (1) adding a header to the home page with a hyperlink to the didactic content or tool to be reviewed next to improve ease of progressing through FoRtitude content; (2) re-organizing coping strategy content horizontally (instead of vertically) so progressive content was presented left to right; and (3) adding hover text and instructions embedded within interactive tools to improve ease of use. Content improvements included (1) revisions to didactic content to improve readability; (2) adding videos to present more complex or challenging content, including a video of the lead investigator (LIW) on how to use the site, rationale for and instructions on how to use Worry practice, and a video-based guided Worry practice; and (3) creating a “My Progress” page to display didactic content and tools that had been completed, material to be reviewed, to chart anxiety scores for each tool to facilitate tracking of progress and to compare tools, and to provide a space for free text for BCS to record notes on helpful content (eg. a “coping card”). Based on feedback that the Worry practice tool was simultaneously beneficial and challenging, in addition to a video-guided worry practice, the tool was modified to add a feature allowing participants to ‘release’ their worries through clicking a button to make the free-text box where BCS typed in their worries fly off the screen. Site content order was reorganized to present Worry practice following Relaxation and Cognitive restructuring. Due to ethical and privacy concerns, FoRitude was not modified to incorporate a social networking feature for study participants to interact.
Conclusions
Qualitative findings from BCS with elevated FoR informed refinements to FoRtitude, an important step in preparation for efficacy testing. FoRtitude was described as beneficial, relevant, easy to comprehend, and following iterative user-driven refinements, easy to use. Individual preferences for coping strategies were reported. Brief, portable coping strategies were the most helpful. Many BCS suggested adding a social media component to FoRtitude to facilitate interactions with other BCS. Negative feedback led to the addition of briefer tools and more flexible instructions. The small sample size limits definitive confirmation of qualitative themes, which may not be generalizable beyond female BCS. Results support the feasibility of CBT-based targeted FoR eHealth interventions to address FoR, thus are aligned with FoR research priorities.3 Results indicate intervention models need to accommodate individual preferences, including technology-enabled interactions among BCS regarding FoR. eHealth-delivered FoR interventions overcome many obstacles to psychosocial care10 providing a scalable, accessible treatment option for this pervasive and distressing concern.
Supplementary Material
Key Points:
Research evaluating eHealth interventions for the management of fear of recurrence (FoR) is needed
We employed user-centered design methods to develop and evaluate FoRtitude, a targeted eHealth intervention designed to deliver three cognitive behavioral therapy (CBT)–based coping strategies tailored to the management of FoR
Using an iterative process, breast cancer survivors (N=17) with clinically significant FoR provided input on FoRtitude content (n=5) and usability (n=4), then conducted field testing (n=8) to refine FoRtitude content and enhance user-centered design in preparation for a randomized trial evaluating efficacy
Based on qualitative interviews, FoRtitude was described as beneficial, relevant, and easy to comprehend. Iterative testing (usability n=4) led to the identification of opportunities to improve ease of site use, and field testing (n=8) confirmed FoRtitude was easy to use, supporting the feasibility of delivering three CBT-based coping strategies using an online format
Individual preferences for coping strategies and frequency and timing for using FoRtitude were reported, indicating intervention research should accommodate flexibility
Acknowledgments
Research reported in this manuscript was supported by the National Cancer Institute (1R21CA173193–01A1) and in part by the Wake Forest Baptist Comprehensive Cancer Center’s NCI Cancer Center Support Grant (P30CA012197) including use of the Qualitative and Patient-Reported Outcomes Shared Resource. The authors acknowledge Mark Reinecke for contributing to FoRtitude content development, Mia Sorkin for recruitment and data collection, and Jaime Hunter for tabulating field testing responses. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest Statement
The authors report no conflicts of interest to disclose.
Publisher's Disclaimer: This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process which may lead to differences between this version and the Version of Record. Please cite this article as doi: 10.1002/pon.5297
References
- 1.Lebel S, Ozakinci G, Humphris G, et al. From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support Care Cancer. 2016;24(8):32653268. [DOI] [PubMed] [Google Scholar]
- 2.Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7(3):300–322. [DOI] [PubMed] [Google Scholar]
- 3.Butow P, Shaw J, Vaccaro L, Sharpe L, Dhillon H, Smith B. A research agenda for fear of cancer recurrence: A Delphi study conducted in Australia. Psychooncology. 2019;28(5):989996. [DOI] [PubMed] [Google Scholar]
- 4.Yardley L, Morrison L, Bradbury K, Muller I. The Person-Based Approach to Intervention Development: Application to Digital Health-Related Behavior Change Interventions. J Med Internet Res. 2015;17(1):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wagner LI, Duffecy J, Penedo F, Mohr DC, Cella D. Coping strategies tailored to the management of fear of recurrence and adaptation for E-health delivery: The FoRtitude intervention. Cancer. 2017;123(6):906–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohr DC, Schueller SM, Montague E, Burns MN, Rashidi P. The Behavioral Intervention Technology Model: An Integrated Conceptual and Technological Framework for eHealth and mHealth Interventions. J Med Internet Res. 2014;16(6):e146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simard S, Savard J. Screening and comorbidity of clinical levels of fear of cancer recurrence. J Cancer Surviv. 2015;9(3):481–491. doi: 410.1007/s11764-11015-10424-11764. Epub 12015 Jan 11721. [DOI] [PubMed] [Google Scholar]
- 8.Duffecy J, Sanford S, Wagner L, Begale M, Nawacki E, Mohr DC. Project onward: an innovative e-health intervention for cancer survivors. Psycho-Oncology Psycho-Oncology. 2012(2):n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 10.Institute of Medicine. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. The National Academies Press; http://www.iom.edu/CMS/3809/34252/47228.aspx. Published 2008. Accessed January 15, 2012. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


