ABSTRACT
Introduction
Digestive organ cancer is a major public health issue both in Asia and in Mongolia. The most prevalent cancer-related deaths in Mongolia are registered as caused by the stomach, esophagus, and liver. There is a lack of study which investigated the accurate incidence of digestive organ cancer nationwide.
Purpose
We aimed to investigate the incidence of stomach and esophageal cancers in Mongolian population.
Materials and methods
Epidemiologic data were collected between 2009 and 2018 through the oncology departments of hospitals and medical centers in all provinces, soums (the smallest unit of provinces), and major districts of the capital city. We used appropriate statistical methods in SPSS software.
Results
The incidence of esophageal cancer in last 10 years (2009–2018) was 10.09 in 100,000 populations and the highest incidence was registered in Uvs (38.13), Bayan-Ulgii (24.15), and Zavkhan (18.18) provinces, respectively. The incidence of stomach cancer was 20.33 in 100,000 populations and the highest incidences were registered in Uvs (53.01), Khovd (46.02), and Darkhan-Uul (40.50) provinces, respectively.
Conclusion
The incidences of these cancers have increased last 10 years in some provinces. Stomach and esophageal cancers incidence in Mongolia is considerably higher compared to the other Asian countries. The nationwide targeted prevention program is needed.
How to cite this article
Lonjid T, Sambuu T, Tumurbat N, et al. Incidence of Stomach and Esophageal Cancers in Mongolia: Data from 2009 to 2018. Euroasian J Hepato-Gastroenterol 2020;10(1):16–21.
Keywords: Age-standardized rate, Cancer epidemiology, Esophageal cancer, Gastric cancer, Mongolia
INTRODUCTION
Mongolians have the highest incidence of stomach and esophageal cancers, age-standardized cancer death rates in the Asia Pacific region,1 which is underpinned by diagnosis at a later stage, common cancers associated with poor survival, and limited quality of health services.2 In Mongolia, a nationwide cancer registry database has been established in mid-1960s as a hospital-based registry in National Cancer Center, and the data quality of the cancer registry database has been sustained at an excellent level since the enactment of the data from the Center for Health Development Mongolia in mid-2000s.2,3
Based on the WHO data of 2018, Mongolian esophageal cancer incidence and mortality were 18.5 and 16.3 per 100,000 populations, which ranked 2nd and 3rd, respectively.
South Korea (100’000:39.6) had the highest rate of stomach cancer in 2018, followed by Mongolia (100’000:33.1) and Japan (100’000:27.5). Nevertheless, Mongolia (100’000:25.0) leads to the mortality of stomach cancer, while Japan (100’000:9.5) and South Korea ranked 32 and 54, respectively.4
Thus so far, we do not have any research on the new cases of stomach and esophageal cancers, even though all cancer prevalence studies have been done previously in Mongolia. Currently, esophageal and stomach cancers studies are left behind the liver cancer studies in our country. We aimed to update statistical data of the new cases of esophageal and stomach cancers among the population of Mongolia by region between the year of 2009 and 2018. For fulfilling this aim, we made following objectives, such as, collecting and analyzing new cases of esophageal and stomach cancers data of 21 provinces and 9 districts from 2009 to 2018, and evaluating and comparing the collected data from all unit hospitals across Mongolia.
MATERIALS AND METHODS
Study Design
This study was designed as a descriptive method and data were collected from newly diagnosed cases of esophageal and stomach cancers in hospitals from 21 provinces and 9 districts of the capital city from 2009 to 2018. We collected data using the “Able Soft” program (Able Soft LLC, Ulaanbaatar, Mongolia). Stomach and esophageal cancers incidence data were collected from April, 2018 to December, 2019. The diagnosis of esophageal and stomach cancers was based on ICD-10 classification. The population number was referred from the official data of National Statistics Office of Mongolia.
The incidence of esophageal and stomach cancers in 21 provinces and 9 districts of the capital city was calculated as mean annual numbers per 100,000 populations. Age-standardized rate (ASR) was utilized by the direct method and it was rated by weighting age-specific incidence rates to the world population5 by following formula:
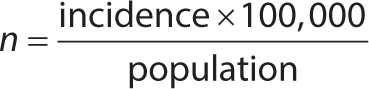 |
Nationwide esophageal and stomach cancers numbers were estimated per 100,000 populations and analyzed using following arithmetic mean at 5-, 5-, and 10-year intervals:
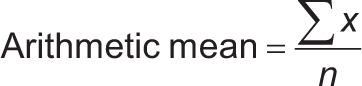 |
Geographical mapping was done by ArcView GIS software (ESRI 380 New York Street Redlands, California, USA).
Ethical Approval
This study was approved by the Institutional Review Board (IRB) of the Institute of Medical Sciences, Mongolian National University of Medical Sciences on 29 June, 2017.
Ethical approval for this study was obtained from Ethics Committee of Ministry of Health on 26 July, 2017 (approval number: 22).
RESULTS
Esophageal Cancer
Five-, 5-, and 10-year period average numbers of cases and age-standardized rates (ASRs) of esophageal and stomach cancers by region for the study period are presented in Table 1. During 2009–2018, an estimate of 2,566 new esophageal cancer cases occurred in Mongolia. The highest incidence rates of esophageal cancer were observed in Western region, which was 23.16 per 100,000 people. The Central-Gobi region had the lowest incidence rates (8.8) of esophageal cancer.
Table 1.
National average numbers of new cases and age-standardized rates per 100,000 populations of esophageal and stomach cancers in Mongolia, by region from 2009 to 2018
| Sites | ICD-10 | Mongolia | UB city | Western region | Khangai region | Central-Gobi region | Eastern region | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | ASR | Cases | ASR | Cases | ASR | Cases | ASR | Cases | ASR | Cases | ASR | ||
| 2009–2013 | |||||||||||||
| Esophagus | C15 | 1,212 | 10.34 | 248 | 4.95 | 424 | 23.51 | 248 | 8.7 | 165 | 7.72 | 127 | 13.95 |
| Stomach | C16 | 2,316 | 18.69 | 729 | 12.16 | 573 | 32.08 | 400 | 14.66 | 408 | 16.92 | 206 | 22.11 |
| 2014–2018 | |||||||||||||
| Esophagus | C15 | 1,354 | 9.87 | 288 | 3.99 | 446 | 22.81 | 286 | 9.29 | 243 | 9.88 | 91 | 8.86 |
| Stomach | C16 | 3,222 | 21.98 | 1,121 | 15.62 | 638 | 31.9 | 666 | 22.95 | 585 | 21.85 | 212 | 20.05 |
| 2009–2018 | |||||||||||||
| Esophagus | C15 | 2,566 | 10.09 | 536 | 4.45 | 870 | 23.16 | 534 | 8.99 | 408 | 8.8 | 218 | 11.41 |
| Stomach | C16 | 5,538 | 20.33 | 1,850 | 13.72 | 1,211 | 31.99 | 1,066 | 18.8 | 993 | 19.38 | 418 | 21.08 |
New cases of esophageal cancer have been reported with national average ASRs of 10.09 per 100,000 populations for the last 10 years. Among the country, Uvs, Bayan-Ulgii, and Zavkhan provinces which located in Western region had been a higher incidence than the national average. The highest incidence rates of esophageal cancer were observed in Uvs (38.1) province which 4 times higher than the national average. The lowest incidence rates of esophageal cancer were observed in Umnugobi (1.67) province.
New cases of esophageal cancer have been reported with capital city average ASRs of 4.47 per 100,000 populations for the last 10 years. The highest and lowest incidences of the esophageal cancer were observed in Baganuur (11.11) and Chingeltei (1.09), respectively based on the data of capital city in the last 10 years (2009–2018) (Table 1).
In the last 10 years (2009–2018) in Mongolia, more new cases of esophageal cancer were reported in western and eastern regions than the other zones.
In a comparison between 2009–2013 and 2014–2018, new cases of the provinces have decreased from 12.64 to 12.40 per 100,000 populations in the last 5 years.
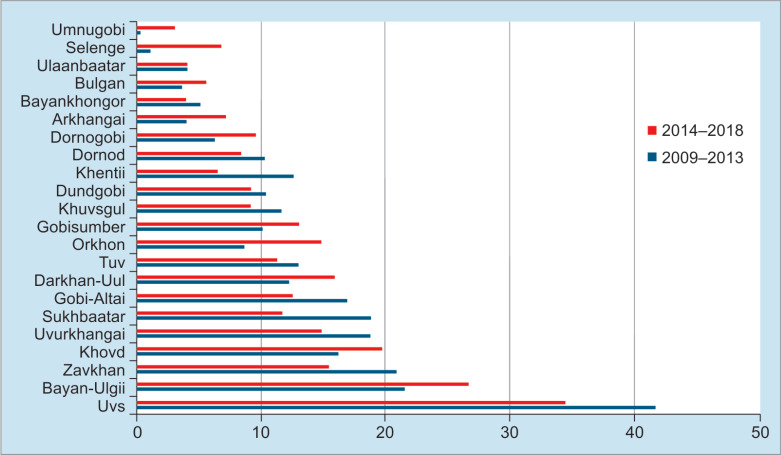
The average incidence rate of esophageal cancer for 5 years was increased in Arkhangai, Bayan-Ulgii, Bulgan, Gobisumber, Darkhan-Uul, Dornogobi, Orkhon, Umnugobi, Selenge, and Khovd provinces while the others were reduced. Therefore, Orkhon, Selenge, and Dornogobi were increased by 6.5, 5.67, and 3.62, respectively (from the first 5 years to the last 5 years) cases per 100,000 populations (Fig. 1).
Fig. 1.
Comparison of national average numbers of new cases and age-standardized rates per 100,000 of the esophageal cancer, by province between 2009–2013 and 2014–2018
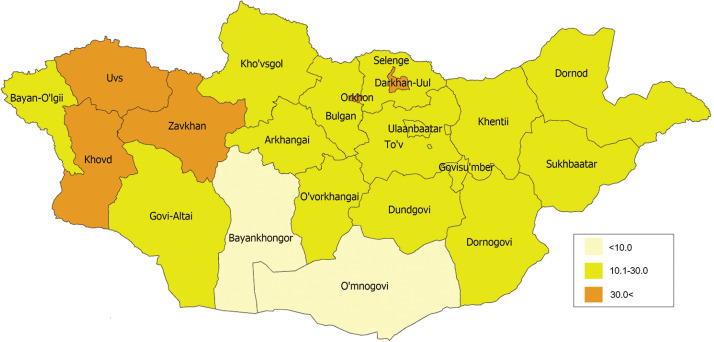
Therefore, the geographical mapping of the incidence of esophageal cancer per 100,000 populations from 2009 to 2018 was particularly different from each other, which was higher in Western region (Fig. 2).
Fig. 2.
New incidence rate of esophageal cancer by an average number from 2009 to 2018, by provinces, per 100,000 population
Stomach Cancer
A total of 5,538 new stomach cancer cases were diagnosed in the country last 10 years (2009–2018). Likeliness to esophageal cancer, the rates were higher in Western region.
The ASRs of esophageal and stomach cancers in urban areas were 4.47 and 13.88, respectively; the burden was markedly higher in rural areas than in urban ones, with ASRs of 12.52 ± 8.0 and 23.16 ± 13.0 in rural areas, respectively.
New cases of stomach cancer have been reported with national average ASRs of 20.33 per 100,000 populations for the last 10 years. Among the country, Uvs, Khovd, and Darkhan-Uul provinces had been a higher incidence than the national average. The highest incidence rates of stomach cancer were observed in Uvs (53.01), Khovd (46.02), and Darkhan-Uul (40.50) provinces, which were 3 and 2.5 times higher than the national average, respectively.
The data of the capital city in the last 10 years (2009–2018) with the highest incidence rates of stomach cancer were observed in Baganuur (30.77), Songinokhairkhan (24.36), and Nalaikh (20.87) districts (Table 1).
In the last 10 years (2009–2018) in Mongolia, more new cases of stomach cancer were reported in western and central regions than the other regions.
In a comparison between 2009–2013 and 2014–2018, new cases of the provinces have increased from 20.62 to 24.30 per 100,000 populations in the last 5 years.
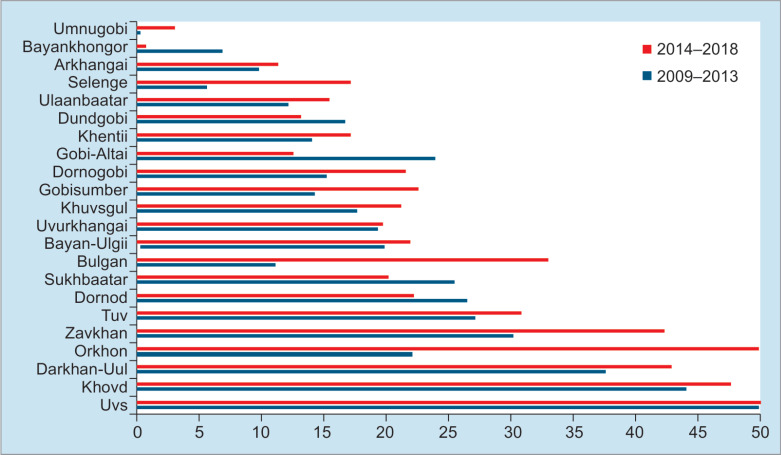
The 5-year average was reduced in Sukhbaatar, Gobi-Altai, Uvs, Bayankhongor, Dornod, and Dundgobi provinces while others increased. Orkhon, Bulgan, and Selenge were increased by 28.65, 21.88, and 11.6, respectively (from the first 5 years to the last 5 years) cases per 100,000 population (Fig. 3).
Fig. 3.
Comparison of national average numbers of new cases and age-standardized rates per 100,000 of the stomach cancer, by province between 2009–2013 and 2014–2018
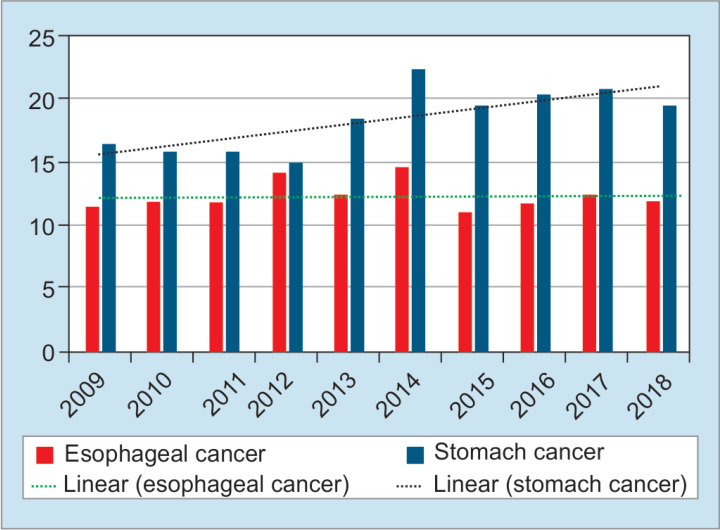
Therefore, the geographical mapping of the incidence of stomach cancer in the 100,000 population from 2009 to 2018 was different from each other, which was higher in Western region (Fig. 4). The stomach cancer trend line is increasing while the esophageal cancer trend line is staying stable in the last 10 years (Fig. 5).
Fig. 4.
New incidence of stomach cancer by an average of 2009–2018, by provinces, per 100,000 population
Fig. 5.
Change of national average number of incidence of esophageal and stomach cancers 2009–2018, per 100,000 population
DISCUSSION
This descriptive study provides patterns of stomach and esophageal cancers incidence for 2009–2018 in Mongolia. We made this survey because of the high incidence rate in GLOBOCAN data.4 From the results of our study, the trend line of stomach cancer is increasing during last 10 years. The government of Mongolia have been developed some national programs, such as, “National Cancer Control Program 2007–2017, Mongolia”6 and “Cancer Registry Guidelines”2 to reduce the risk of common cancers including stomach and esophagus and to provide an effective control of cancer, and these essays were affected better registration of cancers of digestive organ. Better registration may influence the increasing incidence of the stomach cancer, but on the contrary, the actual number of cancer incidence is truly increasing. However, Chimed et al. reported that the incidence of stomach cancer in 2008–2012 was decreased.2 Interestingly, our results for last 10 years showed mild increase of stomach cancer.
Stomach cancer remains one of the most common and deadly disease in Mongolia.7 There are generally no early signs or symptoms of stomach cancer and it contains a poor prognosis cancer because almost 80% cases diagnosed in late stage.8 However, stomach cancer 5-year survival rate is around 90% if it is diagnosed at the early stage. It continues to cause significant damage to the health of the population and the economy of the country.9 Stomach cancer was 14.8% of the 6,073 new cases of cancer diagnosed in 2018.10 Eighty-five percent of it was diagnosed at stage III or IV, and it causes the high mortality due to stomach cancer.11 Therefore, effective management of the prevention, early detection, and treatment of stomach cancer is important to reduce the mortality. Countries, such as, South Korea, Japan, and China have high incidence of stomach cancer but have a low mortality rate due to the implementation of national evidence-based prevention and early detection program for stomach cancer. However, the ASR stomach cancer in Mongolia (20.33 in 100,000 populations) is similar to Japan (27.5) and China (20.7), but it is lower than South Korea (39.6).4 However, in our country, more than 80% of people diagnosed with late-stage stomach cancer, which results in higher mortality rates.
World Health Organization (WHO) classifies stomach cancer incidence into 5 categories: >11.1, 7.3–11.1, 5.0–7.3, 3.8–5.0, and <3.8 per 100,000 populations. The Mongolian national average was 20.33, which is considered to be a high incidence country category. According to the WHO 5 categories, new cases in Ulaanbaatar and 21 provinces were 73.33%, 10%, 6.67%, 3.33%, and 6.67%. We included the average of new cases from 2009 to 2018 into 3 categories: <10, 10.1–30, and >30.1 per 100,000 populations due to low contrast when mapping new cases of stomach cancer to the geographical zoning of Mongolia (Fig. 4).
The presence of helicobacter pylori infection, overcrowded civilization in capital city, and poor living condition are associated with stomach cancer.12–14 Mongolia is the country which have high rate of helicobacter infection with 67–76% in patients with gastric complaints or early stomach cancer.15–17 Previous studies have shown that heavy alcohol use,18 smoking,19 low fruit and vegetable intake,20 the consumption of hot traditional tea or meals, and high consumption of meat7 are the risk factors of both stomach and esophageal cancers. In addition, the high prevalence of helicobacter pylori infection is associated with local antibiotic-resistance patterns.21
Esophageal cancer is a common cancer worldwide that ranked 7th in all cancers and its incidence has been stable during last decade in our study. 572,034 new cases have been reported and 508,585 cases of it ended up death in 2018.4 Among all cases, nearly 80% esophageal cancer occurred in less developed countries.22 WHO classifies esophageal cancer into 5 categories which is the highest number of 4.8 per 100,000 populations. However, the ASR esophageal cancer in Mongolia (10.09 in 100,000 populations) is higher than Japan (5.4) and South Korea (2.6) but it is similar to China (13.9).4 The Mongolian national average was 10.09, which is considered to be a high incidence category. According to the WHO incidence classification of esophageal cancer, new cases of 66.6% of regions Mongolian territory included high incidence rate, and the incidence and mortality of esophageal cancer were 18.5 and 16.3 per 100,000, respectively that ranked 2nd and 3rd in the world.23 We comprised the average of new cases from 2009 to 2018 into 3 categories: <5.0, 5.1–15.0, and >15.1 per 100,000 populations due to low contrast when mapping new cases of esophageal cancer to the geographical zoning of Mongolia (Fig. 2).
In the previous study of esophageal cancer, helicobacter pylori infection level has been relatively lower in Japan, China, and other East Asian countries while having a high prevalence of esophageal cancer. In contrast, countries, such as, India, Bangladesh, Pakistan, and Thailand are having a high prevalence of Helicobacter pylori infection when esophageal cancer is less. It might be related to individual genetic characteristics of ethnics.24 A study in Pakistan found that new cases of esophageal cancer were recorded mainly in countries where mountainous that more than 304.8 meters above sea level (MASL), such as, Mongolia (900–1,500 MASL), China, Turkmenistan, and Pakistan. In this current study, we found the similar results with Uvs (7,589–4,278 MASL), Bayan-Ulgii (1,301–4,374 MASL), and Khovd (1,126–4,204 MASL) provinces, which were in a high prevalence of esophageal cancer and located in mountainous area.
The residence of the capital city is having low incidence rate of esophageal and stomach cancers compared to the national average and the rural area. It might be related with the education, income, and living condition. However, the incidence of esophageal and stomach cancers is higher in Western part of Mongolia and these results are similar with the study of Chimed et al.2 According to Chimed et al. study, authors explained the regional difference of the incidence rate because of the utilization of limited resource of far rural area. Also they suggested that it is really needed to improve health education, especially in rural population.
Present study is a crucial overview of esophageal and stomach cancers burden, risk factor prevalence, and the prospects of prevention, using collected data of all hospitals over whole country and health departments of rural area. The National Cancer Registry of Mongolia is the main organization to register all cancer-related data. Unfortunately, gastrointestinal cancers often to be diagnosed at the late stage in developing countries, including Mongolia.8 The local researchers explained that it causes poor activities of early cancer detection program, lack of diagnostic equipment, and unsuccessful treatment.
The primary and secondary prevention program implementation affects to reduce an incidence and mortality in East Asian and other countries.25 According to the change of structure of the population, our health system requires a new guidelines and healthcare.
CONCLUSION
There is a considerable burden of esophageal and stomach cancers in Mongolia, especially in Western region. Most of the diagnosed cancers could be prevented. The activities or programs to prevent these cancers, especially in rural area, are in urgent need, but on the contrary, rural people need to improve their health education and change the lifestyle to prevent gastrointestinal cancers. However, cancer registry procedures including active collection of histology information were improved but there is still lack of researches to investigate the related factors of gastrointestinal cancers. Also there is a lack of cooperation between national organizations to accurate registration of gastrointestinal cancer and to fight against these harmful cancers. Further regard is needed to reduce the incidence of esophageal and gastric cancers, especially in rural areas.
ACKNOWLEDGMENTS
We thank our colleagues from the department of Internal Medicine of Institute Medical Sciences, Mongolian National University of Medical Sciences; and researchers from National Center for Public Health and National Cancer Center, Mongolia who provided insight and expertise that greatly assisted for the research.
Footnotes
Source of support: The current study was supported by Science and Technology Foundation, Ulaanbaatar, Mongolia (Grant No: SHUUZ2017/06). The sponsors have no role in the design of the study and in the collection, analysis, and interpretation of date in the present study
Conflict of interest: None
REFERENCES
- 1.Shin H-R, Carlos MC, Varghese C. Cancer control in the Asia Pacific region: current status and concerns. Jpn J Clin Oncol. 2012;;42((10):):867––881.. doi: 10.1093/jjco/hys077. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Chimed T, Sandagdorj T, Znaor A, et al. Cancer incidence and cancer control in Mongolia: Results from the National Cancer Registry 2008-12. Int J Cancer. 2017;;140((2):):302––309.. doi: 10.1002/ijc.30463. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Sandagdorj T, Sanjaajamts E, Tudev U, et al. Cancer incidence and mortality in Mongolia - National Registry Data. Asian Pac J Cancer Prev. 2010;;11((6):):1509––1514.. [PubMed] [Google Scholar]
- 4.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;;68((6):):394––424.. doi: 10.3322/caac.21492. DOI: [DOI] [PubMed] [Google Scholar]
- 5.Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;;45((5):):747––755.. doi: 10.1016/j.ejca.2008.11.032. DOI: [DOI] [PubMed] [Google Scholar]
- 6.MOH. National Cancer Control Program 2007-17 Mongolia. Ulaanbaatar:: Ministry of Health Mongolia;; 2007.. [Google Scholar]
- 7.Dorzhgotov B. Risk factors in the manifestations of the 5 principal forms of cancer in the People’s Republic of Mongolia. Sante Publique (Bucur) 1989;;32((4):):361––367.. [PubMed] [Google Scholar]
- 8.Banks M, Graham D, Jansen M, et al. British Society of Gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut. 2019;;68((9):):1545––1575.. doi: 10.1136/gutjnl-2018-318126. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suzuki H, Oda I, Abe S, et al. High rate of 5-year survival among patients with early gastric cancer undergoing curative endoscopic submucosal dissection. Gastric Cancer. 2016;;19((1):):198––205.. doi: 10.1007/s10120-015-0469-0. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Jiang F, Shen X. Current prevalence status of gastric cancer and recent studies on the roles of circular RNAs and methods used to investigate circular RNAs. Cell Mol Biol Lett. 2019;;24((1):):53.. doi: 10.1186/s11658-019-0178-5. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Health indicators. Development Center for Health. 2018..
- 12.Correa P. Helicobacter pylori infection and gastric cancer. Cancer Epidemiol Biomarkers Prev. 2003;;12((3):):238s––241s.. [PubMed] [Google Scholar]
- 13.Ko K-P, Shin A, Cho S, et al. Environmental contributions to gastrointestinal and liver cancer in the Asia-Pacific region. J Gastroenterol Hepatol. 2018;;33((1):):111––120.. doi: 10.1111/jgh.14005. DOI: [DOI] [PubMed] [Google Scholar]
- 14.Gantuya B, Bolor D, Oyuntsetseg K, et al. New observations regarding Helicobacter pylori and gastric cancer in Mongolia. Helicobacter. 2018;;23((4):):e12491.. doi: 10.1111/hel.12491. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsuhisa T, Yamaoka Y, Uchida T, et al. Gastric mucosa in Mongolian and Japanese patients with gastric cancer and Helicobacter pylori infection. World J Gastroenterol. 2015;;21((27):):8408––8417.. doi: 10.3748/wjg.v21.i27.8408. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gantuya B, El-Serag HB, Matsumoto T, et al. Gastric microbiota in Helicobacter pylori-negative and -positive gastritis among high incidence of gastric cancer area. Cancers (Basel) 2019;;11((4):):504.. doi: 10.3390/cancers11040504. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tserentogtokh T, Gantuya B, Subsomwong P, et al. Western-type Helicobacter pylori CagA are the most frequent type in Mongolian patients. Cancers (Basel) 2019;;11((5):):725.. doi: 10.3390/cancers11050725. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ma S-H, Jung W, Weiderpass E, et al. Impact of alcohol drinking on gastric cancer development according to Helicobacter pylori infection status. Br J Cancer. 2015;;113((9):):1381––1388.. doi: 10.1038/bjc.2015.333. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Humans IWGotEoCRt. Biological agents. Volume 100 B. A review of human carcinogens. IARC Monogr Eval Carcinog Risks Hum. 2012.;vol. 100:pp. 1––441.. (Pt B) [PMC free article] [PubMed] [Google Scholar]
- 20.Moore MA, Sobue T. Strategies for cancer control on an organ-site basis. Asian Pac J Cancer Prev. 2010;;11(Suppl 2:):149––164.. [PubMed] [Google Scholar]
- 21.Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection–the Maastricht IV/Florence Consensus Report. Gut. 2012;;61((5):):646––664.. doi: 10.1136/gutjnl-2012-302084. DOI: [DOI] [PubMed] [Google Scholar]
- 22.Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;;144((8):):1941––1953.. doi: 10.1002/ijc.31937. DOI: [DOI] [PubMed] [Google Scholar]
- 23.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;;127((12):):2893––2917.. doi: 10.1002/ijc.25516. DOI: [DOI] [PubMed] [Google Scholar]
- 24.Park B, Yang S, Lee J, et al. Genome-wide association of genetic variation in the PSCA gene with gastric cancer susceptibility in a Korean population. Cancer Res Treat. 2019;;51((2):):748––757.. doi: 10.4143/crt.2018.162. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balakrishnan M, George R, Sharma A, et al. Changing trends in stomach cancer throughout the world. Curr Gastroenterol Rep. 2017;;19((8):):36.. doi: 10.1007/s11894-017-0575-8. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]