Abstract
Objective:
To evaluate the effectiveness of the Kinesio Taping® method for mobility and functioning improvement for patients with knee osteoarthritis (KO).
Design:
Randomized, double-blinded, controlled trial.
Setting:
Outpatient rehabilitation department.
Subjects:
A total of 187 subjects with symptomatic I–III grade KO participated; of these, 157 subjects were included in the analyses (intervention group, n = 81 (123 knees); control group, n = 76 (114 knees).
Intervention:
The intervention group received a specific Kinesio Taping application, and the control group received non-specific knee taping for a month.
Main measures:
Changes in Knee injury and Osteoarthritis Outcome Scores (KOOS), knee active range of motion, 10-Meter Walk, and the five times sit to stand tests (5xSST) were assessed at baseline, after four weeks of taping, and a month post taping intervention. Subjective participants’ experiences and opinions on the effect of knee taping were evaluated. The chosen level of significance was p < 0.05.
Results:
The mean age of participants was 68.7 ± 9.9 in intervention group and 70.6 ± 8.3 in control group (p > 0.05). The change from baseline in gait speed in the intervention group after taping month was +0.04 ± 0.1 m/s, at follow-up +0.06 ± 0.1 m/s; in control group +0.07 ± 0.1 m/s, and +0.09 ± 0.1 m/s; the change in time needed to accomplish 5xSST was –2.2 ± 3.2 seconds, at follow-up –2.4 ± 3.1 seconds; in control group –2.8 ± 3.6 seconds, and –2.4 ± 4 seconds. Improved knee flexion and enhancement in functioning assessed by KOOS were noticed in both groups, with lasting improvement to follow up. No difference in the change in the above-mentioned outcomes was found between groups (p > 0.05). Fewer subjects (6.2% (5) vs. 21.1% (16), χ2 = 7.5, df = 2, p = 0.024) from Kinesio Taping group were unsure if taping alleviated their mobility and more intervention group patients indicated higher subjective satisfaction with the effect of knee taping to symptom and mobility alleviation than control group (p < 0.005).
Conclusion:
Investigated Kinesio Taping technique did not produce better results in mobility and functioning improvement over non-specific knee taping; however, it had higher patient-reported subjective value for symptom attenuation and experienced mobility enhancement.
Keywords: Kinesio taping, knee osteoarthritis, gait speed, functioning, symptoms
Introduction
Treatments for knee osteoarthritis are focused on the relief of pain, other symptoms and on the improvement of function.1 Besides other biomechanical interventions, in the guidelines of the American College of Rheumatology, the non-elastic patellar taping is recommended as an appropriate non-pharmacological pain-alleviating treatment modality for individuals with knee osteoarthritis.2 All recently updated clinical practice guidelines published by a number of societies, including the Osteoarthritis Research Society International, highlight the key role of non-drug, non-surgical treatments for the management of knee osteoarthritis with a focus on self-help and patient-driven treatments rather than on passive therapies delivered by clinicians.2–5
The Kinesio Taping® method is an alternative to the non-elastic taping technique, which uses specially designed waterproof, hypoallergic, elastic tape, that is the Kinesio Tex Tape.6 Differently from non-elastic, non-waterproof patellar taping techniques, which imply the need to use a hypoallergenic undertape beneath the rigid tape to prevent skin irritation, Kinesio tape can be applied directly on the skin and left for several days with good adherence. Low risk of skin irritation makes the method patient-friendly and relatively easy to use in everyday life.6–8 A patient with knee osteoarthritis (or a caregiver) could be taught to apply knee taping by a professional and then could continue the applications at home. Kinesio Taping can be regarded as a promising non-surgical intervention, possibly even as one of the self-management techniques.
Despite the increasing scientific interest and the number of researchers investigating the effectiveness of Kinesio Taping for patients with knee osteoarthritis in recent years, the studies concerning its effectiveness regarding pain relief and functional improvement report conflicting results.9–17 Recent reviews and meta-analyses conclude that this method could be helpful in knee osteoarthritis management; however, small sample size and/or lack of blinding and/or no follow-up and other methodological inadequacies are the common limitations of available studies. Therefore, the decision concerning effectiveness of Kinesio Taping for knee osteoarthritis symptom control and function improvement is inconclusive and has to be warranted by further randomized double-blinded studies.16,17
In our recently published study on the effectiveness of Kinesio Taping for pain management in knee osteoarthritis, we found a specific Kinesio Taping technique to be superior for knee pain alleviation in comparison to nonspecific elastic knee taping.18 The aim of this study was to evaluate the effectiveness of the Kinesio Taping method for knee osteoarthritis patients on the secondary outcomes assessed in the same clinical trial: the changes in other than pain symptoms and functioning, knee range of motion (ROM), gait and mobility improvement after a month-lasting course of taping. We also researched subjective patients’ experiences, tolerance and evaluation of knee taping, and also if the beneficial effects on assessed outcomes can be expected to last for a month post taping.
Methods
The study was a parallel-group, 1:1 allocation ratio, single-center, randomized, double-blinded, controlled trial. It was carried out in the Outpatient Rehabilitation Department at the Medical Academy of the Lithuanian University of Health Sciences between 8 October 2014 and 1 August 2018, with the approval of the National Review Board and Ethics Committee Kaunas subdivision (approval no. BE-2-47, 8 October 2014), and in accordance with the Declaration of Helsinki. All participants gave written informed consents. The identifier in ClinicalTrials.gov is NCT03076177. Kinesio Tex Gold™ tapes for this study were sponsored by the Kinesio Taping Association International. The Kinesio Taping Association International had no influence on the research or the interpretation of data and the conclusions drawn. The organization responsible for the integrity and conduct of this study was the Lithuanian University of Health Sciences.
Volunteers who responded to either the invitation by the cooperating health care specialists or periodically published advertisements were assessed for eligibility by the physical medicine and rehabilitation physician. The inclusion criteria were age >18 years; radiologically verified symptomatic I–III grade knee osteoarthritis (according to the Kellgren and Lawrence system19); willingness to participate in the research. The exclusion criteria were systemic rheumatoid disease (rheumatoid arthritis, gout, etc.); fragile, very sensitive skin, or lesions in the area where the tapes were to be applied; inability to do functional tests required by the study protocol; diagnosed or suspected cancer in the area, where the tapes were to be applied; less than six months after intra-articular injections; constant usage of analgesic medicaments for pain relief in other body parts (except the knee); pregnancy; constant use of any orthotics; previous experience with the Kinesio Taping method; unwillingness to follow the study’s protocol requirements.
The enrolled subjects were scheduled for the first baseline assessment-randomization-taping visit (V0). At the first visit, the enrolled participant received his or her unique code in succession. Unique codes were randomly assigned to the Kinesio Taping (intervention) or the control group using a computer-generated list. Sequence randomization was obtained through http://www.randomization.com (the seed for reproduction: 4514, created on 19 October 2014). The random sequence was concealed until the end of the trial. The group to which the participants’ unique code was ascribed was revealed only to a certified Kinesio Taping practitioner responsible for the taping procedures.
Each participant was assessed by the same blinded researcher during three visits: at baseline (V0), at four weeks after the taping treatment (V1), and after the next four weeks without treatment (follow-up) (V2). During the visits for the re-application of tapes, the tolerance of taping and patients’ experiences with taping were evaluated through a structured questioning and clinical examination by a certified Kinesio Taping practitioner. These assessments were single blinded.
For all participants, tapes were applied once a week, four times per person, with 24 hours “tapes-off” break in-between the applications. We used the Kinesio Tex Gold FP for both groups. The subjects were asked not to start any new vigorous physical activity, to refrain from any local ointments, plasters, knee massage, local physical agents (ice, heat pads and similar, available at home) as well as from starting a new treatment. All possible colors of the tape were used randomly on participants without the difference between groups. In a bilateral knee osteoarthritis case, both knees were taped by the same technique. Participants in both groups were provided with the impartial input from the research team toward the effectiveness of the Kinesio Taping method for knee osteoarthritis.
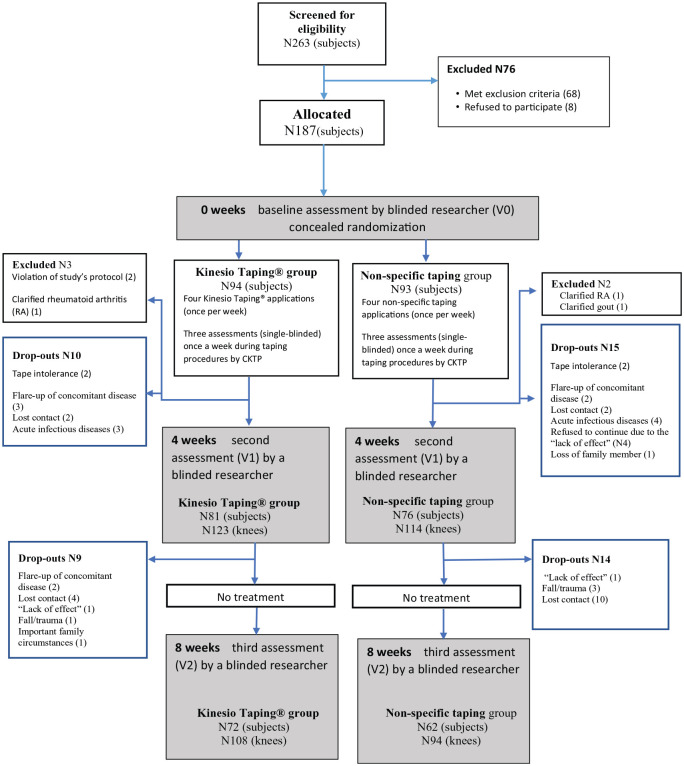
For the Kinesio Taping (intervention) group, two Y strips (“paper off” tension) were applied mainly for lymphatic correction to address possible chronic knee effusion, second seeking to improve anterior thigh muscle function (the elements of lymphatic correction and muscle correction technique were combined). Then two I strips (75%–100% of available tension) were placed over the patella tendon and medial/lateral collateral ligaments in order to increase the stimulation of mechanoreceptors over the area, improve proprioception and knee stability. The detailed description of the intervention is provided in Appendix 1. The completed Kinesio Taping application view is presented in Figure 1.
Figure 1.

The Kinesio Taping® application.
For the control group, the non-specific taping was used. Tapes were applied without using any specific Kinesio Taping technique, just having the purpose of imitating the Kinesio Taping technique for participants to assure their blinding. Two I strips above and below the knee joint and two strips (approx. 5 cm × 5 cm) over the medial and lateral knee surface were applied with 0% tension. The detailed description of the intervention and the rationales for our choice of such control technique are provided in Appendix 2. The view of the completed non-specific taping application is presented in Figure 2.
Figure 2.
The non-specific taping application.
The possible neurophysiological effects on symptoms and knee function due to the irritation of skin receptors and sensory neurons evoked by the tapes attached to the skin at the affected knee site imply a non-specific taping technique to be considered as a competing treatment with the specific Kinesio Taping technique. However, as the irritation of receptors is mild when the tape is attached without tension,6 and only a small area of the knee joint is covered by the tape, the non-specific taping, in our opinion, could be regarded as a “close to placebo” intervention.
Masking was fully assured: all subjects remained unaware of which taping technique was considered therapeutic. The assessors also remained blinded toward the subjects’ allocation until the end of the trial, as all participants were instructed not to discuss group allocation, nor how their tape applications looked like, with the assessor at V1 and V2 visits, as well as being instructed to remove the tapes at home before V1 assessment. This was fulfilled by all participants.
The primary outcome analyzed in this article was the improvement in other than pain symptoms and functioning, assessed by the change in the Knee injury and Osteoarthritis Outcome Scores:20 Other Symptoms; Function in daily living; Sport and Recreation Function; Quality of Life. The clinically meaningful change in the Knee injury and Osteoarthritis Outcome Scores are reported to be approximately 10 points.20,21 In the case of bilateral knee osteoarthritis, our subjects filled in the questionnaires for the right and left knee separately.
The secondary outcomes were the change in the active knee ROM, assessed in subject lying supine with a plastic goniometer (360°/30 cm SEAHAN®). The standard error of measurement for knee ROM was reported to range from 1° to 5°.22 Also, the change of maximal tolerable gait speed was evaluated by 10-Meter Walk test (fast-pace walking mode).23 A gain in gait speed of 0.04–0.06 m/s represents a small meaningful change;24 the gain of 0.1 m/s and more is associated with better survival.25 Mobility, lower extremity strength, and transfer skills were checked by five times sit to stand test.26 The meaningful change in the test was reported to be 2.3–2.5 seconds.26,27
For the assessment of tolerance and the subjective patients’ experiences and opinions on knee taping, the participants were examined by a certified Kinesio Taping practitioner during the weekly re-taping procedures (clinical examination, open-ended, and closed-ended questions were used). Also, after the fourth week of taping (at V1 assessment), subjects of each group were asked by a blinded assessor if, in their opinion, tapes alleviated their ability to move (possible answers to choose from were: “yes,” “no,” “tapes aggravated my mobility” and “I don’t know”).
We performed a power analysis for the sample-size estimation. A meaningful change for the Knee injury and Osteoarthritis Outcome Scores’ subscales is suggested to be 10.20 With 126 participants, our study had 80% power to detect a change in Knee injury and Osteoarthritis Outcome Score of 10 between the Kinesio Taping group and the control assuming a standard deviation of 2020,21 with a significance level of <0.05. The sample size had to be 180 participants if possible drop-outs of 30% were taken into account.
The allocation and recruitment of patients were stopped when we achieved 187 participants (we recruited seven more participants than initially planned for their willingness to participate, meeting requirements of the studies protocol, our technical possibilities to include them, and mainly due to worrying for possible larger drop-outs of already included participants during 2018 spring–summer seasons).
The statistical analysis was performed using software IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, NY). Data are presented as mean (m) ± standard deviation (SD) and 95% confidence interval (CI) for the mean for continuous variables, and N (%) for categorical variables. For baseline characteristic comparisons, primary and secondary outcomes, after testing for normality, parametric and nonparametric criteria, Student’s t-test or repeated-measures analysis of variance (ANOVA) and Mann–Whitney U or Friedman tests were used to compare quantitative samples and χ2 test for categorical variables. The Bonferroni correction was used for the comparisons of more than two groups for the categorical variables. Effect size (ES) for repeated measures and their 95% CI were calculated using Cohen’s d measure, by adjusting the calculation of the pooled SD with weights for the sample sizes, and 0.0–0.1 of Cohen’s d, meaning no effect, 0.2–0.4 meaning small effect, 0.5–0.7 meaning intermediate effect, and ⩾0.8 meaning large effect. The significance level of 0.05 was chosen for testing statistical hypotheses.
Results
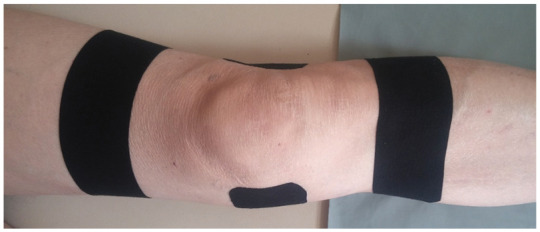
Two hundred and sixty-three volunteers were screened for eligibility. One hundred and eighty-seven were enrolled in the trial with 94 randomized to the Kinesio Taping, and 93 to the non-specific taping group. A detailed study’s flow chart is presented in Figure 3. Groups were comparable according to baseline characteristics (Table 1). There were no differences between the groups, neither in number nor according to the reasons of drop-outs (p > 0.05).
Figure 3.
The study’s flow chart.
Table 1.
The comparison of baseline characteristics between groups.
| Characteristic | KT group |
NT group |
p value |
|---|---|---|---|
| N81 subjects N123 knees |
N76 subjects N114 knees |
||
| Age (mean ± SD) | 68.7 ± 9.9 | 70.6 ± 8.3 | 0.181 |
| Sex | |||
| Male | 17 (21%) | 16 (21%) | |
| Female | 64 (79%) | 60 (79%) | 0.992 |
| Number of concomitant diseases | |||
| None | 7 (8.6%) | 4 (5.3%) | 0.134 |
| 1 | 11 (13.6%) | 15 (19.7%) | |
| 2 | 22 (27.2%) | 23 (30.3%) | |
| 3 | 17 (21%) | 23 (30.3%) | |
| ⩾4 | 24 (29.6%) | 11 (14.5%) | |
| Body mass index (BMI) | 30.5 ± 5.3 | 30.7 ± 5.2 | 0.830 |
| Also suffers pain elsewhere (not in knee area) | |||
| Yes | 63 (77.8%) | 58 (76.3%) | 0.828 |
| No | 18 (22.2%) | 18 (23.7%) | |
| Uses painkillersa for knee pain relief | |||
| No | 39 (48.1%) | 46 (60.5%) | 0.120 |
| Yes | 42 (51.9%) | 30 (39.5%) | |
| Diagnosis | |||
| Right knee osteoarthritis | 22 (22.2%) | 17 (22.4%) | 0.576 |
| Left knee osteoarthritis | 17 (21.1%) | 21 (27.6%) | |
| Bilateral knee osteoarthritis | 42 (51.9%) | 38 (50.0%) | |
| Grade of the knee osteoarthritisb | |||
| I | 14 (11.4%) | 12 (10.5%) | 0.726 |
| I–II or II | 43 (35%) | 35 (30.7%) | |
| II–III or III | 66 (53.7%) | 67 (58.8%) | |
| Duration of the knee painc | |||
| Acute | 8 (6.5%) | 9 (7.9%) | 0.678 |
| Chronic | 115 (93.5%) | 105 (92.1%) | |
| Knee surgeries in history (meniscectomies and similar, except knee replacement) | |||
| Yes | 28 (22.8%) | 29 (25.4%) | 0.678 |
| No | 95 (77.2%) | 85 (74.6%) | |
| Indicated knee trauma fact in the past | |||
| Yes | 47 (38.2%) | 41 (36%) | 0.721 |
| No | 76 (61.8%) | 73 (64%) | |
KT: Kinesio Taping® (intervention); NT: non-specific taping (control); SD: standard deviation; BMI: body mass index.
Just nonsteroidal anti-inflammatory drugs were referred by participants.
Grades are presented according to the Kellgren and Lawrence system: the cases, where radiologist indicated grade I–II or II–III, were ascribed to higher grade group.
Acute pain implies pain duration of less than three months with active treatment, or less than six months if the patient did not receive an adequate treatment; chronic pain implies pain that lasts more than three months with treatment, or more than six months without an adequate pain management.
After four weeks of knee taping, a significant improvement was found in knee injury and Osteoarthritis Outcome Score subscales, ROM, mobility, and gait speed within both groups and the improvement remained during one-month follow-up, however, without differences in the improvement between the groups, p > 0.05. The summarized data about the changes in functioning and mobility variables are presented in Table 2.
Table 2.
The changes in functioning, knee AROM, gait speed, and mobility (within-group and between-groups comparisons).
| Variables | Group | Baseline values (V0), M ± SD | Value after taping month (V1), M ± SD | Value at follow-up (four weeks post taping month) (V2), M ± SD | A change after a taping month (V1–V0), M ± SD | A change at follow-up from baseline (V2–V0), M ± SD | Within-group comparison, V0 versus V1, effect size (95% CI) | Within-group comparison, V0 versus V2, effect size (95% CI) | Comparison of changes in outcomes between groups after a taping month, p value | Comparison of changes in outcomes between groups at a follow-up, p value |
|---|---|---|---|---|---|---|---|---|---|---|
| KOOS subscalesa | ||||||||||
| Symptoms | KT | 60.6 ± 17.6 | 70.1 ± 15.8 | 68.2 ± 16.8 | 9.1 ± 14.7 | 7 ± 14 | 0.62 (0.33 to 0.85) | 0.50 (0.21 to 0.76) | 0.869 | 0.337 |
| NT | 56.5 ± 18.5 | 65.5 ± 18.6 | 64.6 ± 18.7 | 9 ± 14.4 | 5 ± 15 | 0.62 (0.36 to 0.9) | 0.34 (0.06 to 0.64) | |||
| Function in daily living | KT | 58.8 ± 15 | 66.4 ± 15.4 | 66.6 ± 15.7 | 7.6 ± 12.7 | 7.2 ± 11.6 | 0.6 (0.35 to 0.89) | 0.62 (0.35 to 0.90) | 0.181 | 0.6 |
| NT | 55.6 ± 16.4 | 64.4 ± 15.7 | 64.8 ± 14.4 | 8.8 ± 12.5 | 6.2 ± 15.1 | 0.71 (0.43 to 0.97) | 0.41 (0.13 to 0.71) | |||
| Sport and recreation | KT | 38.3 ± 19.6 | 46.1 ± 22.1 | 44.9 ± 21.2 | 7.9 ± 17.7 | 8.7 ± 15.5 | 0.45 (0.23 to 0.74) | 0.42 (0.17 to 0.71) | 0.799 | 0.468 |
| NT | 28.4 ± 17.4 | 36.7 ± 19.9 | 30.3 ± 17.1 | 6.6 ± 15.8 | 9 ± 18.9 | 0.56 (0.37 to 0.91) | 0.49 (0.26 to 0.85) | |||
| Quality of life | KT | 37 ± 16.3 | 46.4 ± 18.6 | 43.9 ± 18.9 | 9.4 ± 17.7 | 5 ± 17.4 | 0.49 (0.31 to 0.82) | 0.31 (0.08 to 0.62) | 0.181 | 0.731 |
| NT | 34.4 ± 15.5 | 39.4 ± 18.1 | 42.8 ± 18.7 | 5.6 ± 17.9 | 6.4 ± 18.3 | 0.29 (0.05 to 0.58) | 0.35 (0.12 to 0.69) | |||
| Knee flexion (°) | KT | 118.2 ± 14 | 120.8 ± 14.5 | 121.8 ± 13.7 | 2.6 ± 6.5 | 2.9 ± 8.3 | 0.38 (0.14 to 0.64) | 0.44 (0.17 to 0.71) | 0.447 | 0.473 |
| NT | 112.6 ± 14 | 115.7 ± 13.8 | 117.4 ± 12.7 | 3.1 ± 7 | 3.4 ± 9 | 0.45 (0.18 to 0.71) | 0.56 (0.24 to 0.82) | |||
| Knee extension deficit (°) | KT | 2.6 ± 3.7 | 2.2 ± 3.4 | 2 ± 2.8 | –0.4 ± 2 | –0.8 ± 2.5 | –0.21 (–0.45 to 0.05) | –0.09 (–0.35 to 018) | 0.524 | 0.546 |
| NT | 2.9 ± 3.4 | 2.6 ± 3.2 | 2.3 ± 2.7 | –0.2 ± 1.9 | –0.6 ± 2 | –0.15 (–0.41 to 0.11) | –0.32 (–0.58 to 0.00) | |||
| 5xSSTb (s) | KT | 15.6s ± 5.6 | 13.4s ± 4.5 | 12.7s ± 4.1 | –2.2s ± 3.2 | –2.4s ± 3.1 | –0.76 (–1.01 to –0.37) | –0.96 (–1.21 to –0.53) | 0.227 | 0.097 |
| NT | 16.8s ± 6.3 | 14.1s ± 5.4 | 13.63 ± 4.8 | –2.8s ± 3.6 | –2.4s ± 4 | –0.84 (–1.08 to –0.42) | –0.68 (–1.02 to –0.23) | |||
| Gait speed (m/s) | KT | 1.05 ± 0.3 | 1.11 ± 0.2 | 1.13 ± 0.3 | 0.04 ± 0.1 | 0.06 ± 0.1 | 0.68 (0.33 to 0.96) | 0.5 (0.15 to 0.81) | 0.938 | 0.438 |
| NT | 0.96 ± 0.3 | 1.04 ± 0.3 | 1.09 ± 0.3 | 0.07 ± 0.1 | 0.09 ± 0.1 | 0.45 (0.15 to 0.8) | 0.63 (0.3 to 1.03) | |||
AROM: active range of motion; KOOS: Knee injury and Osteoarthritis Outcome Scores; KT: Kinesio Taping® group; NT: control (non-specific taping) group; CI: confidence interval.
A normalized score (100 indicating no problems, and 0 indicating extreme problems) is calculated for each subscale
Five times sit to stand test is used for assessing mobility, lower extremity strength, and transfer skills.
During the single-blinded assessments carried out by a certified Kinesio Taping practitioner, no major side effects or deterioration of functioning were observed that would imply the need to discontinue knee taping. The patients from the intervention group more often expressed the experienced positive impact of taping for symptom alleviation and mobility in comparison to the control group, p < 0.05. No differences were observed in the occurrence of mild skin irritation and/or other subjective sensations evoked by tapes between the groups (p > 0.05), except for a mild intermittent sense of wetness and/or cold under the tapes that was more often noted by the participants from the Kinesio Taping group, p < 0.05. It is worth noting that this mild complaint was commonly expressed by the participants during a cold autumn or winter season and was mostly experienced by the participants when being outside. The summarized comparisons between the groups concerning the subjective tolerance, experiences and observed skin reactions to tapes are presented in Table 3.
Table 3.
The summarized comparisons of subjects’ experiences/tolerance/side effects of taping.a
| Experiences/opinions/observational data | Group | Yes % (subjects) | No % (subjects) | Comparison between groups, p value |
|---|---|---|---|---|
| Sense of mild intermittent wetness and/or cold under the tapes | KT | 11.1 (9) | 88.9 (72) | p = 0.012 |
| NT | 1.3 (1) | 98.7 (75) | ||
| Sense of mild intermittent warmth under the tapes | KT | 9.9 (8) | 90.1 (73) | p = 0.277 |
| NT | 5.3 (4) | 94.7 (72) | ||
| Mild intermittent itching under the tapes | KT | 8.6 (7) | 91.4 (74) | p = 0.407 |
| NT | 5.3 (4) | 94.7 (72) | ||
| Mild intermittent paresthetic sensation (burning, tingling, pricking) under the tapes | KT | 9.9 (8) | 90.1 (73) | p = 0.887 |
| NT | 9.2 (7) | 90.8 (69) | ||
| Indicated stair climbing alleviation when with tapes | KT | 11.1 (9) | 88.9 (72) | p = 0.038 |
| NT | 2.6 (2) | 97.4 (74) | ||
| Alleviation in changing body position and/or general mobility (expressed as “my knee feels more stable,” “strengthened,” “less fear to move,” “I feel enforcement” when with tapes) | KT | 44.4 (36) | 55.6 (45) | p = 0.003 |
| NT | 22.4 (17) | 77.6 (59) | ||
| Observed mild skin reactions/irritation or skin lesionsb | KT | 11.1 (9) | 88.9 (72) | p = 0.906 |
| NT | 10.5 (8) | 89.5 (68) |
KT: Kinesio Taping® group; NT: control (non-specific taping) group.
The results that are presented in this table comprise summarized data acquired during the single-blinded assessments by a certified Kinesio Taping practitioner (only the patient was blinded to intervention).
All observed skin reactions were mild and did not require any treatment or discontinuation of taping (mild erythema, small areas of pealing of superficial epidermis layers, mild rashes, few petechiae were among those that were observed).
Similarly, after a month of taping, the majority of the participants informed the blinded assessor of the positive feedback on taping and responded that in their opinion, knee tapes did alleviate their mobility: 80.2% (65) in the Kinesio Taping group and 67.1% (51) in the control group. Only 13.6% (11) from the Kinesio Taping group and 11.8% (9) from the control group answered that knee taping did not help them to move easier. None of the participants noted knee taping to aggravate their mobility function; however, significantly, more participants (21.1% (16) vs. 6.2% (5), χ2 = 7.5, df = 2, p = 0.024) from non-specific taping were unsure if the tapes had alleviated their mobility and responded: “I don’t know if taping applications helped me to move easier.”
Discussion
Our results indicate that the month-long course of knee taping with Kinesio Tex Gold FP was well tolerated by the majority of knee osteoarthritis patients. There occurred no major side effects or function deterioration that would require to discontinue the intervention. Also, patients experienced clinically meaningful improvements in knee flexion, gait speed, mobility and functioning20,21,24–27 during the taping month that lasted up to a month post intervention. However, although we had found the specific Kinesio Taping technique to be superior over the non-specific technique for pain reduction,18 this advantage did not produce any detectible benefit for gait speed, ROM, mobility and functioning (assessed by Knee injury and Osteoarthritis Outcome Scores) improvement. No difference in these outcomes between groups was found. The possibility that there is a subjective difference in the perception of the effect on symptom alleviation and the sense of mobility improvement between Kinesio Taping and control applications experienced by the patients is much less sound evidence.
These findings should be interpreted regarding certain limitations of our research. The design of our study and the absence of a no-tape group render the conception regarding the effectiveness of knee taping inconclusive because our results do not show any absolute effect. A relatively short taping course and a lack of a longer follow-up are other limitations for assessing a chronic condition. The standardization of Kinesio Taping application for knee osteoarthritis patients concerning the complexity of individual person having the knees treated by the same technique makes the generalizations on the effectiveness of the Kinesio Taping method, which emphasizes the individualized approach to each case, limited, too.
In addition, our conclusions on the safety of, and the tolerance to the month of knee taping intervention should be interpreted with consideration that the brand of the tape might have had an important impact on these results. A wide variety of commercially available kinesiology tape brands nowadays might produce different effects and safety hazards in clinical practice.
The possible bias in certified Kinesio Taping practitioners’ records due to the lack of blinding of this assessor slightly weakens the strength of our statistical comparison of some subjective tolerance outcomes as well. Also, the positioning of a non-specific application through guaranteed blinding of participants made it a competing intervention to specific Kinesio Taping technique: we could not investigate the effects of true placebo intervention as control.
The strengths of our study are as follows: the randomized, controlled, double-blinded (for majority of researched outcomes) study design; the sample-size calculation with a power of 80%; the assessment of symptoms, functioning, and mobility by different instruments (subjective and objective) providing a possibility to get a more complete picture of the knee osteoarthritis patients’ experiences with knee taping, tolerance, and outcomes on symptom alleviation, knee function, and mobility improvement. We have probably studied more knees than any other currently available study on the effectiveness of Kinesio Taping for knee osteoarthritis.
Some researchers who investigated the effects of Kinesio Taping on functional status in patients with knee osteoarthritis, but used other measurement scales for functioning, similarly to our study’s results found no superiority of Kinesio Taping over sham intervention; however, they also reported improvements in this outcome in both groups after taping interventions.11,13,14 Kocyigit et al.14 who, similarly to us, applied Kinesio Taping and sham taping on knee area suggested that increment in functioning in both groups may be explained by the mechanical support provided by both taping methods. Probably, this hypothesis, as well as possible neurophysiological effects induced by skin receptors’ irritation due to tapes,28 can also partly explain our results on the improvement of functioning in both groups.
Rahlf et al.9 and Öğüt et al.,10 however, reported Kinesio Taping to produce higher than sham taping improvements in functioning immediately after treatment. It is noteworthy that in these studies, the researchers used sham taping not directly on the knee joint region. Perhaps, the significant differences in functioning between intervention and control groups that were reported can be explained by the absence of any proprioceptive boost in the knee area in sham groups.
We have found only one study by Aydoǧdu et al.29 that used Knee injury and Osteoarthritis Outcome Scores for functioning estimation for knee osteoarthritis patients who were either treated by the conventional rehabilitation procedures, or conventional rehabilitation procedures plus Kinesio Taping for three weeks. The authors of this study reported immediate improvement in all subscales approximately 1-hour post first taping session, but for an unknown reason did not assess the control group at the same time-frame making the interpretation of the findings complicated. However, the post-treatment (three weeks later) improvements in functioning did not reveal the superiority of the conventional therapy plus Kinesio Taping for quadriceps and hamstring muscles over the conventional therapy alone.
Our results, however, suggest that knee taping alone for four weeks produced similar clinically meaningful improvements in functioning. It could be hypothesized that when conventional therapy is not available, knee taping by any of our researched application techniques might be considered as a possible intervention for knee osteoarthritis patients for symptom, functioning, and mobility improvement. Nevertheless, further research is needed to verify this.
In contrast to some studies that reported notable superiority of Kinesio Taping for knee flexion10,12,13 and gait speed,13 our results failed to support these findings. Although we found statistically significant improvements in knee flexion within both groups, and the positive effect lasted until the follow-up, the change was of questionable clinical value as not likely exceeding measurement error.22 The change in the extension deficit was even smaller. Similarly, Kaya Mutlu et al.13 reported improved flexion with no significant improvements in knee extension. Rahlf et al.9 did not find positive effect of Kinesio Taping on the ROM. The different designs of reported trials and multifarious taping applications used in the studies can be the possible reason for the diverse outcomes. This aggravates any comparisons and interpretation of unequal findings.
However, in our study, the observed overall improvement in gait speed and mobility within both groups, though without specific benefit of Kinesio Taping over control, in general is a very desirable effect for daily clinical management of knee osteoarthritis. The subjects from both groups were found to have increased risk for recurrent falls, accord-ing to the results of five times sit to stand test (>15 seconds)30 at baseline. This risk significantly improved after a month of sole taping intervention. These positive changes continued up to one month of follow-up in both groups. The change in gait speed reached a clinically meaningful difference and tended to increase with time. Such improvements are associated with better functional performance and survival in the elderly.24,25
Therefore, the possible beneficial effects of knee taping should be further researched. Studies that could verify the absolute effect of knee taping interventions are warranted.
Based on our results, it could be hypothesized that even a smaller proprioceptive stimulation from knee area, provided by a non-specific taping application, was enough to slightly reduce pain,18 improve proprioception,31,32 and lead to clinically meaningful positive changes in function. It should not be disregarded that another possible reason for similar results on functioning and mobility in both groups of our study could be implied by a ceiling effect: the more advanced knee osteoarthritis is, the older the patient is, the more concomitant diseases are present, the less improvement in knee ROM and in other mobility outcomes is realistic.33,34 The majority of our volunteered subjects had an advanced (II or III grade) stage of knee osteoarthritis were obese and of older age with a high comorbidity count, and half of them suffered from bilateral knee osteoarthritis. These factors might be a reason for a small possible improvement in objective functioning measures in general, and therefore, possible superiority of specific Kinesio Taping application (which was reported by patients subjectively) could not be detected by objective changes. The possibility that both groups of patients reached their ceiling in functional outcomes cannot be fully rejected.
However, our results might indicate that for knee osteoarthritis patients specific therapeutic application on the affected knee does not necessarily mean a bigger improvement at least in Knee injury and Osteoarthritis Outcome Scores, ROM, mobility, and gait speed. The possibility to obtain nearly the same results in functioning by providing the application that is less complicated, easier to learn for the elderly, and allows less tape consumption would be more cost-effective, as well as have a very desirable result for any knee osteoarthritis patient and/or his or her caregiver. Therefore, further studies are needed on how much stimulation by tapes in the knee area is actually efficient for knee osteoarthritis patients to reach clinically meaningful improvements in functioning, mobility, and gait speed.
Our analysis of expressed subjective patients’ opinions and experiences with knee taping revealed some possible advanced effects of the specific Kinesio Taping application in comparison to non-specific taping for symptom and mobility improvement, which were not detected by the commonly used instruments. Significantly more subjects from our Kinesio Taping group indicated knee tapes to alleviate their stair climbing, the changing of body’s position during daily activities, more often noted sense of joint support, decreased fear to move, increased stability, and an “ease to move when with tapes” in comparison to the control group. In the long term, such effects can improve the prevailing hypomobility of knee osteoarthritis patients and lead to better disability reduction and improved quality of life in the performance of daily activities1,4,33,35 in comparison to control technique.
Although the data on patients’ subjective experiences were mostly gathered through single-blinded assessments of certified Kinesio Taping practitioners, it is noteworthy that to a certain extent, it was backed up by the results from the double-blinded assessments on patients’ opinions toward the effectiveness of knee taping for mobility improvement, as well as on pain reduction.18 Therefore, this should not be underestimated. We were unable to find another study which would investigate the subjective opinions of knee osteoarthritis patients toward the effectiveness of their knee taping intervention. Our findings suggest that the specific Kinesio Taping technique could be expected to produce better results in certain symptom alleviation and can have higher value for knee osteoarthritis patients. This might therefore produce better compliance with intervention and should probably be considered as a priority choice, possibly a self-help and patient-driven treatment at least for those knee osteoarthritis patients who express pain, lack of joint control, instability or fear of movement among their complaints.
Clinical Messages.
A month of knee taping with Kinesio® Tex Gold™ FP was a well-tolerated intervention by knee osteoarthritis patients.
Investigated Kinesio Taping technique did not produce better results in mobility and functioning improvement over non-specific knee taping; however, it had higher patient-reported subjective value for symptom attenuation and experienced mobility enhancement.
Supplemental Material
Supplemental material, Suppl_Material for The effectiveness of Kinesio Taping® for mobility and functioning improvement in knee osteoarthritis: a randomized, double-blind, controlled trial by Venta Donec and Raimondas Kubilius in Clinical Rehabilitation
Acknowledgments
The authors would like to thank all rehabilitation team members of the Rehabilitation Department, Medical Academy, Lithuanian University of Health Sciences, who from October 2014 to August 2018 provided valuable assistance for undertaking the research summarized here.
Footnotes
Authors’ contribution: V.D. contributed to the conception and design of the work; also to the acquisition, analysis, and to the interpretation of data for the work; drafted the work; made final approval of the version to be published; provided agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. R.K. contributed to the analysis and the interpretation of data for the work; revised the work critically for important intellectual content; provided final approval of the version to be published; provided agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Kinesio® Tex Gold™ tapes for this study were sponsored by the Kinesio Taping Association International. Kinesio Taping Association International had no influence on the research or the interpretation of data and conclusions drawn.
ORCID iD: Venta Donec  https://orcid.org/0000-0003-0476-1053
https://orcid.org/0000-0003-0476-1053
Supplemental material: Supplemental material for this article is available online.
References
- 1. Sofat N, Kuttapitiya A. Future directions for the management of pain in osteoarthritis. Int J Clin Rheumatol 2014; 9: 197–216, http://www.ncbi.nlm.nih.gov/pubmed/25018771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2012; 64(4): 465–474, http://doi.wiley.com/10.1002/acr.21596 [DOI] [PubMed] [Google Scholar]
- 3. Jevsevar DS. Treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg 2013; 21(9): 571–576, https://journals.lww.com/jaaos/Fulltext/2013/09020/Treatment_of_Osteoarthritis_of_the_Knee_.8.aspx [DOI] [PubMed] [Google Scholar]
- 4. McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014; 22(3): 363–388, http://www.ncbi.nlm.nih.gov/pubmed/24462672 [DOI] [PubMed] [Google Scholar]
- 5. Bennell KL, Hall M, Hinman RS. Osteoarthritis year in review 2015: rehabilitation and outcomes. Osteoarthritis Cartilage 2016; 24(1): 58–70, https://linkinghub.elsevier.com/retrieve/pii/S1063458415012819 [DOI] [PubMed] [Google Scholar]
- 6. Kase K, Wallis J, Kase T. Clinical therapeutic applications of Kinesio taping method. 2nd ed. Tokyo, Japan: Ken Ikai Co. Ltd, 2003. [Google Scholar]
- 7. Therapy M. ACR OA guidelines non-pharmacological—knee and hip. Arthritis Care Res 2009, https://www.rheumatology.org/Portals/0/Files/ACR%20OA%20Guidelines%20Non-pharmacological%20-%20Knee%20and%20Hip.pdf
- 8. Hinman RS, Crossley KM, McConnell J, et al. Efficacy of knee tape in the management of osteoarthritis of the knee: blinded randomised controlled trial. BMJ 2003; 327(7407): 135, http://www.ncbi.nlm.nih.gov/pubmed/12869456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rahlf AL, Braumann KM, Zech A. Kinesio taping improves perceptions of pain and function of patients with knee osteoarthritis: a randomized, controlled trial. J Sport Rehabil 2019; 28: 481–487, https://journals.humankinetics.com/doi/10.1123/jsr.2017-0306 [DOI] [PubMed] [Google Scholar]
- 10. Ogut H, Guler H, Yildizgoren MT, et al. Does kinesiology taping improve muscle strength and function in knee osteoarthritis? A single-blind, randomized and controlled study. Arch Rheumatol 2018; 33(3): 335–343, http://www.ncbi.nlm.nih.gov/pubmed/30632535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wageck B, If TD, Nunes GS, et al. Kinesio taping does not improve the symptoms or function of older people with knee osteoarthritis : a randomised trial. J Physiother 2018; 62(3): 153–158, 10.1016/j.jphys.2016.05.012 [DOI] [PubMed] [Google Scholar]
- 12. Cho HY, Kim EH, Kim JYY, et al. Kinesio taping improves pain, range of motion, and proprioception in older patients with knee osteoarthritis: a randomized controlled trial. Am J Phys Med Rehabil 2015; 94(3): 192–200. [DOI] [PubMed] [Google Scholar]
- 13. Kaya Mutlu E, Mustafaoglu R, Birinci T, et al. Does Kinesio taping of the knee improve pain and functionality in patients with knee osteoarthritis? A randomized controlled clinical trial. Am J Phys Med Rehabil 2017; 96(1): 25–33. [DOI] [PubMed] [Google Scholar]
- 14. Kocyigit F, Turkmen MB, Acar M, et al. Kinesio taping or sham taping in knee osteoarthritis? a randomized, double-blind, sham-controlled trial. Complement Ther Clin Pract 2015; 21(4): 262–267, 10.1016/j.ctcp.2015.10.001 [DOI] [PubMed] [Google Scholar]
- 15. Park SH, Park YH, Lee JH. Effects of magnetic field therapy after taping application on pain and function of patients with knee osteoarthritis. J Phys Ther Sci 2017; 29(9): 1548–1551, http://www.ncbi.nlm.nih.gov/pubmed/28931985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lu Z, Li X, Chen R, et al. Kinesio taping improves pain and function in patients with knee osteoarthritis : a meta-analysis of randomized controlled trials. Int J Surg 2018; 59: 27–35, 10.1016/j.ijsu.2018.09.015 [DOI] [PubMed] [Google Scholar]
- 17. Ouyang J, Chang K, Hsu W, et al. Non-elastic taping, but not elastic taping, provides benefits for patients with knee osteoarthritis: systemic review and meta-analysis. Clin Rehabil 2018; 32(1): 3–17. [DOI] [PubMed] [Google Scholar]
- 18. Donec V, Kubilius R. The effectiveness of Kinesio Taping® for pain management in knee osteoarthritis: a randomized, double-blind, controlled clinical trial. Ther Adv Musculoskelet Dis [Internet] 2019; 11:1759720X1986913, http://www.ncbi.nlm.nih.gov/pubmed/31497072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res 2016; 474(8): 1886–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Engelhart L, Nelson L, Lewis S, et al. Validation of the knee injury and osteoarthritis outcome score subscales for patients with articular cartilage lesions of the knee. Am J Sports Med 2012; 40(10): 2264–2272, http://www.ncbi.nlm.nih.gov/pubmed/22962288 [DOI] [PubMed] [Google Scholar]
- 21. Singh JA, Luo R, Landon GC, et al. Reliability and clinically important improvement thresholds for osteoarthritis pain and function scales: a multicenter study. J Rheumatol 2014; 41(3): 509–515, http://www.ncbi.nlm.nih.gov/pubmed/24429183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maciel C, Santos D, Ferreira G, et al. Intra and inter examiner reliability and measurement error of goniometer and digital inclinometer use. Rev Bras Med Esporte 2012; 18(1): 38–41, http://www.scielo.br/pdf/rbme/v18n1/en_08.pdf [Google Scholar]
- 23. Kim Park I, Lee HJ, Lee O. The reliability and validity of gait speed with different walking pace and distances against general health, physical function, and chronic disease in aged adults. J Exerc Nutrition Biochem 2016; 20(3): 46–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Perera S, Mody SH, Woodman RC, et al. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006; 54(5): 743–749, http://doi.wiley.com/10.1111/j.1532-5415.2006.00701.x [DOI] [PubMed] [Google Scholar]
- 25. Hardy SE, Perera S, Roumani YF, et al. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc 2007; 55(11): 1727–1734, http://www.ncbi.nlm.nih.gov/pubmed/17916121 [DOI] [PubMed] [Google Scholar]
- 26. Goldberg A, Chavis M, Watkins J, et al. The five-times-sit-to-stand test: validity, reliability and detectable change in older females. Aging Clin Exp Res 2012; 24(4): 339–344, http://www.ncbi.nlm.nih.gov/pubmed/23238309 [DOI] [PubMed] [Google Scholar]
- 27. Meretta BM, Whitney SL, Marchetti GF, et al. The five times sit to stand test: responsiveness to change and concurrent validity in adults undergoing vestibular rehabilitation. J Vestib Res 2006; 16(4–5): 233–243, http://www.ncbi.nlm.nih.gov/pubmed/17538213 [PubMed] [Google Scholar]
- 28. Callaghan MJ, McKie S, Richardson P, et al. Effects of patellar taping on brain activity during knee joint proprioception tests using functional magnetic resonance imaging. Phys Ther 2012; 92(6): 821–830, http://www.ncbi.nlm.nih.gov/pubmed/22282771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Aydoǧdu O, Sari Z, Yurdalan SU, et al. Clinical outcomes of Kinesio taping applied in patients with knee osteoarthritis: a randomized controlled trial. J Back Musculoskelet Rehabil 2017; 30(5): 1045–1051. [DOI] [PubMed] [Google Scholar]
- 30. Buatois S, Perret-Guillaume C, Gueguen R, et al. A simple clinical scale to stratify risk of recurrent falls in community-dwelling adults aged 65 years and older. Phys Ther 2010; 90(4): 550–560, http://www.ncbi.nlm.nih.gov/pubmed/20203094 [DOI] [PubMed] [Google Scholar]
- 31. Callaghan MJ, McKie S, Richardson P, et al. Effects of patellar taping on brain activity during knee joint proprioception tests using functional magnetic resonance imaging. Phys Ther 2012; 92(6): 821–830, http://www.ncbi.nlm.nih.gov/pubmed/22282771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Langendoen J, Fleishman C. Rationales and evidence of Elastic Taping: clinician’s perspective. J Int Acad Phys Ther Res 2014; 7(1): 979–988. [Google Scholar]
- 33. Sharma L, Cahue S, Song J, et al. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum 2003; 48(12): 3359–3370, http://www.ncbi.nlm.nih.gov/pubmed/14673987 [DOI] [PubMed] [Google Scholar]
- 34. de Rooij M, van der Leeden M, Heymans MW, et al. Prognosis of pain and physical functioning in patients with knee osteoarthritis: a systematic review and meta-analysis. Arthritis Care Res 2016; 68(4): 481–492, http://doi.wiley.com/10.1002/acr.22693 [DOI] [PubMed] [Google Scholar]
- 35. Accettura AJ. Determinants of physical performance in people with knee osteoarthritis, https://macsphere.mcmaster.ca/bitstream/11375/12483/1/fulltext.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Suppl_Material for The effectiveness of Kinesio Taping® for mobility and functioning improvement in knee osteoarthritis: a randomized, double-blind, controlled trial by Venta Donec and Raimondas Kubilius in Clinical Rehabilitation