Abstract
Purpose:
Limited options exist for patients with advanced pancreatic cancer progressing after 1 or more lines of therapy. A phase II study in patients with previously treated metastatic pancreatic cancer showed that combining GVAX pancreas (granulocyte-macrophage colony-stimulating factor-secreting allogeneic pancreatic tumor cells) with cyclophosphamide (Cy) and CRS-207 (live, attenuated Listeria monocytogenes expressing mesothelin) resulted in median overall survival (OS) of 6.1 months, which compares favorably with historical OS achieved with chemotherapy. In the current study, we compared Cy/GVAX + CRS-207, CRS-207 alone, and standard chemotherapy in a three-arm, randomized, controlled phase IIb trial.
Patients and Methods:
Patients with previously treated metastatic pancreatic adenocarcinoma were randomized 1:1:1 to receive Cy/GVAX + CRS-207 (arm A), CRS-207 (arm B), or physician’s choice of single-agent chemotherapy (arm C). The primary cohort included patients who had failed ≥2 prior lines of therapy, including gemcitabine. The primary objective compared OS between arms A and C in the primary cohort. The second-line cohort included patients who had received 1 prior line of therapy. Additional objectives included OS between all treatment arms, safety, and tumor responses.
Results:
The study did not meet its primary efficacy endpoint. At the final study analysis, median OS [95% confidence interval (CI)] in the primary cohort (N = 213) was 3.7 (2.9–5.3), 5.4 (4.2–6.4), and 4.6 (4.2–5.7) months in arms A, B, and C, respectively, showing no significant difference between arm A and arm C [P = not significant (NS), HR 1.17; 95% CI, 0.84–1.64]. The most frequently reported adverse events in all treatment groups were chills, pyrexia, fatigue, and nausea. No treatment-related deaths occurred.
Conclusions:
The combination of Cy/GVAX + CRS-207 did not improve survival over chemotherapy. (ClinicalTrials.gov ID: NCT02004262)
Introduction
Pancreatic adenocarcinoma is a disease with a high mortality rate and limited effective therapeutic options. Over 80% of pancreatic cancers are unresectable at diagnosis due to the presence of regional or distant disease at diagnosis (1). Even those who undergo potentially curative resection are likely to succumb to the disease within a few years. The chemotherapeutic combinations FOLFIRINOX (5-fluorouracil/lecovorin, irinotecan, and oxaliplatin) and gemcitabine/nab-paclitaxel for patients with metastatic pancreatic cancer have improved response rates, disease-free survival, and median overall survival (OS) compared with those observed with single-agent chemotherapy. However, outcomes remain poor, at an estimated survival of less than 1 year (2). Only a single combination therapy, liposomal irinotecan with fluorouracil/folinic acid, has been approved for second-line therapy in gemcitabine-treated patients based on prolonged OS over fluorouracil/folinic acid (6.28 vs. 4.2 months; NAPOLI-1; ref. 3). As a result, there is an urgent and unmet need to develop more effective therapies for patients with advanced pancreatic cancer with disease progression after first-line therapy.
Immunotherapy carries potential advantages over chemotherapy (e.g., lower toxicity and more durable responses) and recent progress in immunotherapy has occurred for various other malignancies (4–6). Although immunotherapy is emerging as a treatment option for some gastrointestinal cancers, activity remains poor in pancreatic cancer, in part due to a relative absence of immune-infiltrating effector T cells in the tumor microenvironment (7). Immunotherapy strategies aim to expand tumor-specific T cells and induce their migration into the tumor microenvironment. One such strategy utilizes the immunotherapeutic agent CRS-207, which is a live, attenuated Listeria monocytogenes (Lm) strain carrying double deletions (LADD) that render it nonvirulent, making it a promising agent for presentation of tumor-associated antigens and activation of immune response. CRS-207 is the LADD platform with an inserted expression cassette that expresses the tumor-associated antigen mesothelin (8, 9). CRS-207 retains the ability to stimulate innate immunity and activate mesothelin-specific cell-mediated immunity. A recently completed open-label, randomized, controlled phase II study of patients with previously treated metastatic pancreatic cancer found that sequential administration of low-dose cyclophosphamide (Cy), GVAX (granulocyte-macrophage colony-stimulating factor-secreting allogeneic pancreatic tumor cells) followed by CRS-207 improved overall survival (OS) compared with Cy/GVAX alone (10). Low-dose Cy was given to enhance the immune response by depleting regulatory T cells and enhance expansion of effector T cells (11). The study resulted in a median OS of 6.28 months [95% confidence interval (CI), 4.47–9.40 months] for patients treated with CRS-207 + Cy/GVAX. In a subset analysis, median OS in patients with > 2 prior regimens was 5.7 months (95% CI, 3.4–9.7). In light of these promising results, a phase IIb randomized, multicenter study was conducted to compare Cy/GVAX + CRS-207 with chemotherapy in patients with metastatic pancreatic cancer (ClinicalTrials.gov ID: NCT02004262).
Patients and Methods
Study design
This multicenter, randomized, open-label phase IIb trial was conducted at 21 centers in the United States and Canada. Patients were randomized 1:1:1 to receive 2 doses per course of Cy/GVAX + 4 doses per course of CRS-207 (arm A), 6 doses per course of CRS-207 alone (arm B), or physician’s choice of single-agent chemotherapy (arm C). Standard chemotherapy options for arm C included capecitabine, infusional 5-fluorouracil (5-FU), gemcitabine, irinotecan, and erlotinib because there were no standard-of-care reference regimens for patients with multiple lines of prior therapy at the time of the study. Randomization was stratified by progressive or stable disease status at study entry based on investigator’s assessment. There were two cohorts in the study, the primary cohort and the second-line cohort. The primary cohort comprised of patients who had received ≥2 prior lines of therapy, including one gemcitabine-based regimen, specifically in the metastatic disease setting (third line +). The second-line cohort included patients who had received exactly one prior regimen of chemotherapy for metastatic pancreatic cancer.
The primary endpoint was to compare OS of arm A with arm C in the primary cohort (third line +). Secondary endpoints were safety, OS in the primary cohort between arms B and C, and other efficacy, immunologic, biomarker, and safety parameters in arm A versus arm B. Exploratory endpoints included but were not limited to tumor responses using RECIST v1.1 and safety and survival analyses in the second-line cohort. This study was performed in accordance with Good Clinical Practice and the Declaration of Helsinki. The study was reviewed by local institutional review boards, biosafety committees, the U.S. Food and Drug Administration, and the NIH Recombinant DNA Advisory Committee. Interim data were reviewed by an independent data monitoring committee, including an interim analysis of futility. Written informed consent was obtained from all patients.
Patients
Eligible patients had histologically proven, previously treated, metastatic adenocarcinoma of the pancreas, were ≥18 years old, with an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, and adequate organ function. Patients were excluded if they had brain metastases, major artificial implants or devices that could not be easily removed (portacaths and biliary stents were allowed), hepatic cirrhosis or clinical or radiographic ascites, thromboembolic disease within 2 months, HIV, hepatitis B or C, or autoimmune disease.
Treatment
In arms A and B, one treatment course was 20 weeks, consisting of six study drug administrations at 3-week intervals (Fig. 1). In arm A, Cy (200 mg/m2, Baxter) was delivered intravenously 1 day before each GVAX treatment (first day of weeks 1 and 4). GVAX consisted of two irradiated, allogeneic, GM-CSF–secreting pancreatic adenocarcinoma cell lines (2.5 × 108 cells each; Johns Hopkins University, Baltimore, MD), combined and administered as six intradermal injections on the second day of weeks 1 and 4. CRS-207(1 × 109 colony-forming units, Aduro Biotech) was delivered by 1-hour intravenous infusion followed by a 4-hour observation period on the first day of weeks 7, 10, 13, and 16. In arm B, CRS-207 was administered at the same dose every 3 weeks for 6 doses. Oral antibiotics were initiated 7 days after the final CRS-207 dose of each course (amoxicillin or sulfamethoxazole trimethoprim in the event of an allergy to amoxicillin). Patients could receive additional courses of the treatment if clinically stable. The recommended chemotherapy doses in arm C were capecitabine (1,000 mg/m2 orally twice a day, days 1–14 on a 21-day cycle), 5-FU (2,400 mg/m2 continuous i.v. infusion over 46 hours on days 1 and 15 on a 28-day cycle), gemcitabine (1,000 mg/m2 i.v. on days 1, 8, and 15 on a 28-day cycle), irinotecan (150 mg/m2 i.v. on days 1 and 15 on a 28-day cycle), or erlotinib (100 mg orally once daily on a 21-day cycle).
Figure 1.
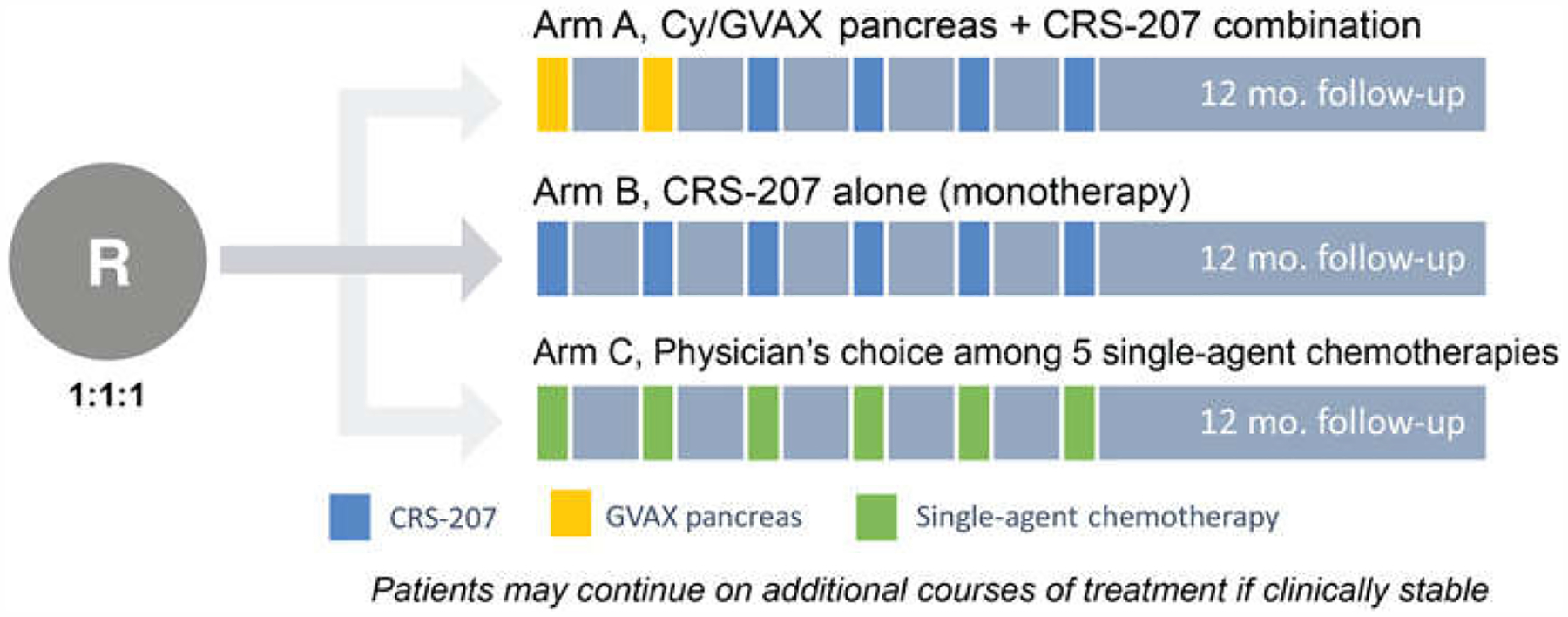
Study schematic.
Assessments
Physical examinations, complete blood count, and chemistries were performed prior to each treatment and the day after CRS-207 infusions. Safety was assessed in the full analysis set (FAS) by reported adverse events (AE). Imaging was performed at baseline and weeks 10 and 20. Tumor response was determined by investigator assessment using RECIST v1.1. Immune-related response was assessed in patients administered CRS-207 (arms A and B) using immune-related response criteria (irRC; ref. 12).
Statistical analysis
The primary efficacy analysis compared OS based on the log-rank test for Cy/GVAX and CRS-207 versus chemotherapy in the primary cohort using the intention-to-treat (ITT) population, which included all randomized patients. Secondary analyses were performed on the FAS. Power was computed for a two-stage group sequential design with a single interim analysis for futility using an overall one-sided type I error rate of 0.15. The amount of alpha spent (1-sided) for the interim analysis was 0.0015. Accordingly, the one-sided P value for the final analysis needed to be <0.1499 in order to reject the null hypothesis of equal survival. If the mOS in arm A was 6 months and that for arm C was 4 months, an estimated 45 and 48 deaths for treatment arms A and C, respectively, at the time of the primary analysis would provide more than 80% power to detect a HR of 0.67 using the log-rank test. A sample size of at least 150 treated patients (50 treated per arm) was targeted to achieve the desired power in both the ITT and FAS populations. Assuming that the survival distribution of arm B was similar to arm A, the primary analysis was planned to occur at 138 deaths in the FAS for the primary cohort (estimated at 45, 45, and 48 deaths for treatment arms A, B, and C, respectively). A final analysis was performed using all available trial data when the study was completed, which occurred after all patients had a minimum follow-up of at least 12 months or died. This paper reports the results of the final analysis. An additional 90 patients (30 per arm) would be treated in an exploratory cohort of second-line patients.
Kaplan–Meier method was used to estimate median survival and 95% CIs for mOS and progression-free survival (PFS). The log-rank test was used to compare OS and PFS between treatment arms. The Cox proportional hazards model and Wald statistics were used to estimate HRs and CIs. OS and PFS were calculated from the date of randomization until the date of death and date of disease progression or death, respectively. PFS and tumor response summaries are based on the FAS.
Results
Study population, demographics, and baseline characteristics
Initially, 513 patients were assessed for eligibility. After screening, during which 210 (41%) patients were excluded, 303 patients across 21 sites in the United States and Canada were enrolled into the two cohorts (Fig. 2). Two-hundred thirteen patients were enrolled in the primary cohort and 90 patients in the second-line cohort. Forty-four patients (20.7%) in the primary cohort discontinued prior to treatment initiation (arm A, n = 5; arm B, n = 10; arm C, n = 29). Twenty-four patients (26.7%) in the second-line cohort did not receive treatment (arm A, n = 3; arm B, n = 2; arm C, n = 19). The first patient was randomized in February 2014 and the last patient visit was August 2016.
Figure 2.
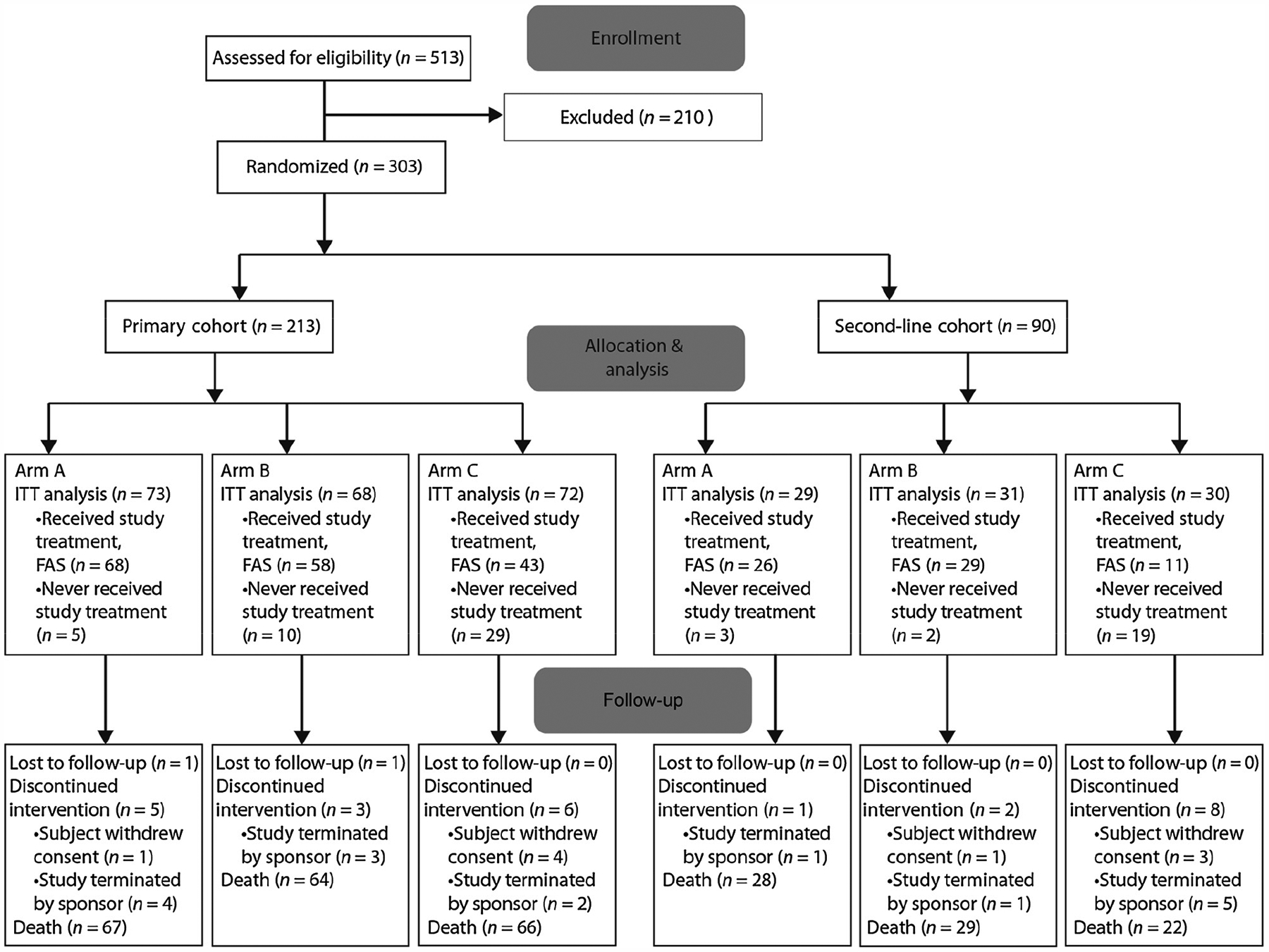
CONSORT diagram of subject disposition.
Demographics and baseline characteristics in the FAS are summarized in Table 1. In the primary and second-line cohorts, 91.1% and 87.9% of patients, respectively, had progressive disease upon enrollment. Numerically, more patients in arm B had lung-only metastases, whereas more patients in arm C had undergone primary tumor resection and had liver metastases (Supplementary Table S1). The mean age of patients who had received at least one treatment dose was 63.4 and 64.4 years for the primary and second-line cohorts, respectively. In the primary cohort, the median time on protocol treatment was 44, 43, and 42 days in arms A, B, and C, respectively. In the second-line cohort, the median time on protocol treatment was 58, 43, and 36 days in arms A, B, and C, respectively. A list of chemotherapy regimens chosen for arm C patients is included in Supplementary Table S2.
Table 1.
Demographics and baseline characteristics (FAS): Primary cohort (top) and second-line cohort (bottom)
| Primary cohort | Cy/GVAX + CRS-207 arm A (N = 68) | CRS-207 arm B (N = 58) | Chemotherapy arm C (N = 43) | Total (N = 169) |
|---|---|---|---|---|
| Age (years), mean (SD) | 63.3 (8.0) | 63.2 (8.9) | 64.0 (10.9) | 63.4 (9.0) |
| Gender, n (%) | ||||
| Male | 37 (54.4) | 29 (50.0) | 17 (39.5) | 83 (49.1) |
| Female | 31 (45.6) | 29 (50.0) | 26 (60.5) | 86 (50.9) |
| Ethnicity, n (%) | ||||
| Hispanic or Latino | 3 (4.5) | 3 (5.2) | 1 (2.3) | 7 (4.2) |
| Not Hispanic or Latino | 64 (95.5) | 55 (94.8) | 42 (97.7) | 161 (95.8) |
| Unknown | 1 | 0 | 0 | 1 |
| Race, n (%) | ||||
| American Indian/Alaskan Native | 1 (1.5) | 0 | 0 | 1 (0.6) |
| Asian | 0 | 4 (6.9) | 2 (4.7) | 6 (3.6) |
| Black/African American | 5 (7.5) | 2 (3.4) | 4 (9.3) | 11 (6.5) |
| Native Hawaiian/Pacific Islander | 0 | 1 (1.7) | 0 | 1 (0.6) |
| White | 60 (89.6) | 50 (86.2) | 37 (86.0) | 147 (87.5) |
| Other | 1 (1.5) | 1 (1.7) | 0 | 2 (1.2) |
| Unknown | 1 | 0 | 0 | 1 |
| ECOG performance status, n (%) | ||||
| 0 = Fully active | 26 (38.2) | 15 (25.9) | 17 (39.5) | 58 (34.3) |
| 1 = Restricted but ambulatory | 42 (61.8) | 43 (74.1) | 25 (58.1) | 110 (65.1) |
| 2 = No work activities but ambulatory | 0 | 0 | 1 (2.3) | 1 (0.6) |
| Disease status at study entry, n (%) | ||||
| Progressive disease | 62 (91.2) | 53 (91.4) | 39 (90.7) | 154 (91.1) |
| Stable disease | 6 (8.8) | 5 (8.6) | 4 (9.3) | 15 (8.9) |
| Stage at initial diagnosis, n (%) | ||||
| IA | 0 | 1 (1.7) | 0 | 1 (0.6) |
| IB | 0 | 1 (1.7) | 2 (4.7) | 3 (1.8) |
| IIA | 4 (5.9) | 2 (3.4) | 3 (7.0) | 9 (5.3) |
| IIB | 11 (16.2) | 7 (12.1) | 5 (11.6) | 23 (13.6) |
| III | 11 (16.2) | 6 (10.3) | 4 (9.3) | 21 (12.4) |
| IV | 37 (54.4) | 31 (53.4) | 23 (53.5) | 91 (53.8) |
| Unknown | 5 (7.4) | 10 (17.2) | 6 (14.0) | 21 (12.4) |
| Number of any prior therapies, n (%) | ||||
| 1 | 0 | 0 | 0 | 0 |
| 2 | 30 (44.1) | 36 (62.1) | 17 (39.5) | 83 (49.1) |
| 3 | 16 (23.5) | 16 (27.6) | 13 (30.2) | 45 (26.6) |
| 4 | 12 (17.6) | 4 (6.9) | 7 (16.3) | 23 (13.6) |
| 5 | 7 (10.3) | 2 (3.4) | 5 (11.6) | 14 (8.3) |
| 6 | 2 (2.9) | 0 | 1 (2.3) | 3 (1.8) |
| 7 | 1 (1.5) | 0 | 0 | 1 (0.6) |
| Number of prior metastatic therapy regimens, n (%) | ||||
| 1 | 0 | 0 | 0 | 0 |
| 2 | 35 (51.5) | 42 (72.4) | 23 (53.5) | 100 (59.2) |
| 3 | 19 (27.9) | 12 (20.7) | 15 (34.9) | 46 (27.2) |
| 4 | 9 (13.2) | 3 (5.2) | 4 (9.3) | 16 (9.5) |
| 5+ | 5 (7.4) | 1 (1.7) | 1 (2.3) | 7 (4.1) |
| Baseline CA 19–9 (U/mL), median (min, max) | 1,213.5 (0.8, 232185.0) | 445.6 (0.8, 576,817.0) | 1,537.0 (1.0, 225,856.8) | 955.7 (0.8, 576,817.0) |
| Second-line cohort | Cy/GVAX + CRS-207 arm A (N = 26) | CRS-207 arm B (N = 29) | Chemotherapy arm C (N = 11) | Total (N = 66) |
| Age (years), mean (SD) | 63.9 (11.8) | 64.1 (9.4) | 66.6 (10.9) | 64.4 (10.6) |
| Gender, n (%) | ||||
| Male | 11 (42.3) | 19 (65.5) | 6 (54.5) | 36 (54.5) |
| Female | 15 (57.7) | 10 (34.5) | 5 (45.5) | 30 (45.5) |
| Ethnicity, n (%) | ||||
| Hispanic or Latino | 0 | 2 (6.9) | 0 | 2 (3.0) |
| Not Hispanic or Latino | 26 (100) | 27 (93.1) | 11 (100) | 64 (97.0) |
| Race, n (%) | ||||
| American Indian/Alaskan Native | 0 | 0 | 0 | 0 |
| Asian | 1 (3.8) | 1 (3.4) | 0 | 2 (3.0) |
| Black/African American | 3 (11.5) | 2 (6.9) | 0 | 5 (7.6) |
| Native Hawaiian/Pacific Islander | 0 | 1 (3.4) | 0 | 1 (1.5) |
| White | 22 (84.6) | 25 (86.2) | 11 (100) | 58 (87.9) |
| Other | 0 | 0 | 0 | 0 |
| ECOG performance status, n (%) | ||||
| 0 = Fully active | 10 (38.5) | 13 (44.8) | 6 (54.5) | 29 (43.9) |
| 1 = Restricted but ambulatory | 16 (61.5) | 16 (55.2) | 5 (45.5) | 37 (56.1) |
| 2 = No work activities but ambulatory | 0 | 0 | 0 | 0 |
| Disease status at study entry, n (%) | ||||
| Progressive disease | 22 (84.6) | 26 (89.7) | 10 (90.9) | 58 (87.9) |
| Stable disease | 4 (15.4) | 3 (10.3) | 1 (9.1) | 8 (12.1) |
| Stage at initial diagnosis, n (%) | ||||
| 0 | 0 | 0 | 0 | 0 |
| IA | 0 | 0 | 0 | 0 |
| IB | 0 | 3 (10.3) | 0 | 3 (4.5) |
| IIA | 3 (11.5) | 3 (10.3) | 1 (9.1) | 7 (10.6) |
| IIB | 3 (11.5) | 4 (13.8) | 4 (36.4) | 11 (16.7) |
| III | 6 (23.1) | 6 (20.7) | 2 (18.2) | 14 (21.2) |
| IV | 10 (38.5) | 7 (24.1) | 4 (36.4) | 21 (31.8) |
| Unknown | 4 (15.4) | 6 (20.7) | 0 | 10 (15.2) |
| Number of any prior therapies, n (%) | ||||
| 1 | 17 (65.4) | 17 (58.6) | 7 (63.6) | 41 (62.1) |
| 2 | 5 (19.2) | 8 (27.6) | 3 (27.3) | 16 (24.2) |
| 3 | 2 (7.7) | 1 (3.4) | 0 | 3 (4.5) |
| 4 | 2 (7.7) | 2 (6.9) | 0 | 4 (6.1) |
| 5 | 0 | 0 | 1 (9.1) | 1 (1.5) |
| 6–9 | 0 | 0 | 0 | 0 |
| 10 | 0 | 1 (3.4) | 0 | 1 (1.5) |
| Number of prior metastatic therapy regimens, n (%) | ||||
| 1 | 24 (92.3) | 28 (96.6) | 11 (100) | 63 (95.5) |
| 2 | 2 (7.7) | 0 | 0 | 2 (3.0) |
| 3 | 0 | 0 | 0 | 0 |
| 4 | 0 | 0 | 0 | 0 |
| 5+ | 0 | 1 (3.4) | 0 | 1 (1.5) |
| Baseline CA 19–9 (U/mL), median (min, max) | 411.9 (3.0, 11,700.0) | 1,114.9 (10.0–263,933.2) | 150 (3.0, 10,946.9) | 688.3 (3.0, 263,933.2) |
Efficacy outcomes
Primary cohort (third+line).
Seventy-three, 68, and 72 patients were randomized to arms A, B, and C, respectively (ITT population). The study did not meet its primary efficacy endpoint comparison at the time of the primary analysis, as there was no difference in median OS between arm A (Cy/GVAX + CRS-207) and arm C (chemotherapy). The study continued as planned and at the time of the final analysis, the ITT patient numbers were unchanged and the median (95% CI) OS was 3.7 (2.9–5.3) versus 4.6 (4.2, 5.7) months [HR 1.17, 95% CI 0.84–1.64, not significant (NS)] in arms A and C, respectively (Fig. 3). The median (95% CI) OS in arm B (CRS-207) was 5.4 (4.2–6.4) months, which was not significantly different from that in arm C (one-sided P = NS).
Figure 3.
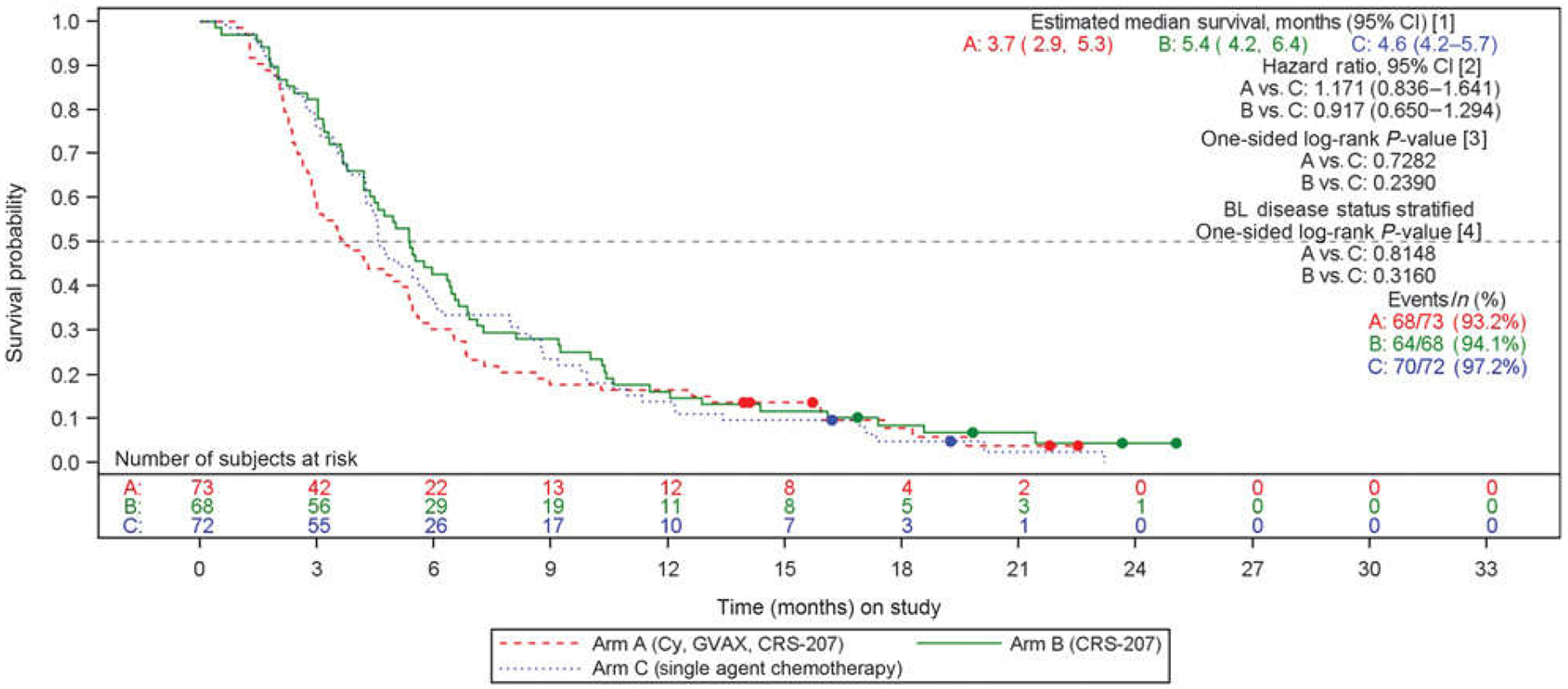
OS by treatment arm: primary cohort, ITT population. [1] Estimates are based on Kaplan–Meier methodology. [2] Estimates are based on a Cox proportional hazards model stratified by baseline disease status at study entry using treatment arm as the factor. [3] P values are from a one-sided log-rank test. [4] P values are from a stratified one-sided log-rank test using baseline disease status at study entry as the stratification factor. BL, baseline.
The OS data in the FAS population were similar to those for ITT. Sixty-eight, 58, and 43 patients were included in the FAS for arms A, B, and C, respectively. These numbers reflect the disproportionate dropout rate of arm C patients prior to treatment. The median (95% CI) OS was 4.2 (3.0–5.4) for arm A vs. 4.7 (3.8–6.0) months (P = NS, HR 1.12; 95% CI, 0.75–1.66, NS) for arm C. The median (95% CI) OS for arm B (CRS-207) was 5.4 (4.2–6.3) months, which was not significantly different from arm C (P = NS; HR, 0.97; 95% CI, 0.65–1.46).
PFS and tumor response summaries were evaluated in the FAS population. PFS was similarin all groups (2.3, 2.1, and 2.1 months in arms A, B, and C, respectively; Supplementary Fig. S1). Although a one-sided P value showed a statistically significant difference between arms A and C, results may have been biased by the high number of untreated subjects in arm C (40.3%). The majority of patients in each treatment group had progressive disease as their best overall response (BOR) based on RECIST v1.1 criteria. The proportion of patients with stable disease was highest in arm A, and one subject in arm A had a partial response (1.5%). Disease control rates (stable disease + partial response) were 23.5%, 13.8%, and 11.6% in arms A, B, and C, respectively. Treatment effect by baseline characteristics is provided in Fig. 4. Chemotherapy arm performed better in patients 65 years and younger. In those with stable disease prior to study entry, arms A and B were favored, although the absolute numbers were small.
Figure 4.
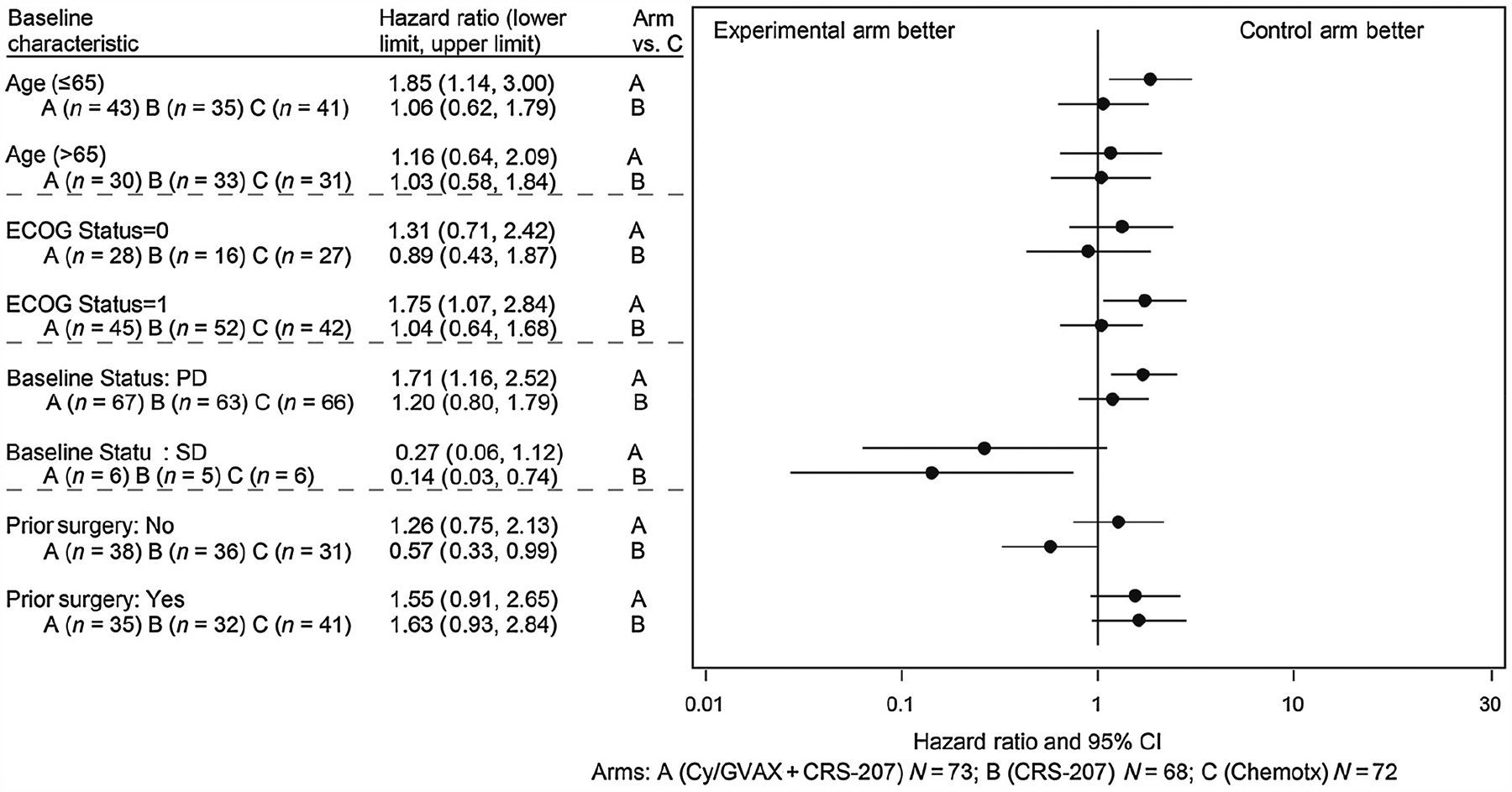
Forest plot of OS by select baseline characteristics in the primary cohort. Chemotx, chemotherapy; PD, progressive disease; SD, stable disease.
Second-line cohort.
Twenty-nine, 31, and 30 patients were randomized to arms A, B, and C, respectively (ITT population). The median OS was 4.3, 4.1, and 9.1 months in arms A, B, and C, respectively. The FAS included 26, 29, and 11 patients in arms A, B, and C, respectively. Again, these numbers reflect the disproportionate dropout among arm C patients (63.3%). The median OS in the FAS was 4.6, 4.0, and 6.9 months in arms A, B, and C, respectively.
There was no statistically significant difference in PFS between arms A and C, with a median of 2.4 months in each arm, as evaluated in the FAS. Similar to the primary cohort, progressive disease was the BOR for the majority of patients in all treatment arms. One subject had a partial response (9.1%) in chemotherapy arm. Disease control rates were 23.1%, 20.7%, and 18.2% in arms A, B, and C, respectively.
Safety.
Safety evaluations were performed in the FAS. All treatments were generally well tolerated, with <5% of patients reporting serious AEs (SAE) related to study treatment. There were no treatment-related deaths. The treatment-related AE profile was similar to prior experience in the experimental arms and consisted mainly of low-grade AEs of pyrexia, chills, fatigue, and nausea in all study arms (Table 2). There were four related, unexpected SAEs reported: confusional state, hypoxia, hypertension, and bacteremia.
Table 2.
Treatment-emergent AEs (all grades) occurring in ≥10% of patients in any arm
| Cy/GVAX + CRS-207 arm A (N = 94) | CRS-207 arm B (N = 87) | Chemotherapy arm C (N = 54) | Total (N = 235) | |||||
|---|---|---|---|---|---|---|---|---|
| System organ class preferred term | n (%) | Rate | n (%) | Rate | n (%) | Rate | n (%) | Rate |
| General disorders and administration-site conditions | ||||||||
| Chills | 59 (62.8) | 2.92 | 81 (93.1) | 5.45 | 5 (9.3) | 0.58 | 145 (61.7) | 3.32 |
| Pyrexia | 51 (54.3) | 2.53 | 58 (66.7) | 3.90 | 9 (16.7) | 1.04 | 118 (50.2) | 2.70 |
| Fatigue | 50 (53.2) | 2.48 | 38 (43.7) | 2.56 | 26 (48.1) | 3.01 | 114 (48.5) | 2.61 |
| Vaccination-site erythema | 77 (81.9) | 3.82 | 0 | — | 0 | — | 77 (32.8) | 1.76 |
| Vaccination-site induration | 53 (56.4) | 2.63 | 0 | — | 0 | — | 53 (22.6) | 1.21 |
| Vaccinations-site pain | 53 (56.4) | 2.63 | 0 | — | 0 | — | 53 (22.6) | 1.21 |
| Vaccination-site edema | 51 (54.3) | 2.53 | 0 | — | 0 | — | 51 (21.7) | 1.17 |
| Vaccination-site pruritus | 49 (52.1) | 2.43 | 0 | — | 0 | — | 49 (20.9) | 1.12 |
| Vaccination-site bruising | 25 (26.6) | 1.24 | 0 | — | 0 | — | 25 (10.6) | 0.57 |
| Edema peripheral | 15 (16.0) | 0.74 | 6 (6.9) | 0.40 | 2 (3.7) | 0.23 | 23 (9.8) | 0.53 |
| Disease progression | 13 (13.8) | 0.64 | 5 (5.7) | 0.34 | 2 (3.7) | 0.23 | 20 (8.5) | 0.46 |
| Gastrointestinal disorders | ||||||||
| Nausea | 42 (44.7) | 2.08 | 44 (50.6) | 2.96 | 29 (53.7) | 3.36 | 115 (48.9) | 2.63 |
| Vomiting | 32 (34.0) | 1.59 | 32 (36.8) | 2.15 | 13 (24.1) | 1.51 | 77 (32.8) | 1.76 |
| Abdominal pain | 30 (31.9) | 1.49 | 33 (37.9) | 2.22 | 12 (22.2) | 1.39 | 75 (31.9) | 1.72 |
| Constipation | 25 (26.6) | 1.24 | 21 (24.1) | 1.41 | 10 (18.5) | 1.16 | 56 (23.8) | 1.28 |
| Diarrhea | 12 (12.8) | 0.59 | 18 (20.7) | 1.21 | 20 (37.0) | 2.32 | 50 (21.3) | 1.14 |
| Metabolism and nutritional disorders | ||||||||
| Decreased appetite | 24 (25.5) | 1.19 | 16 (18.4) | 1.08 | 19 (35.2) | 2.20 | 59 (25.1) | 1.35 |
| Hypokalemia | 7 (7.4) | 0.35 | 10 (11.5) | 0.67 | 7 (13.0) | 0.81 | 24 (10.2) | 0.55 |
| Hyponatremia | 13 (13.8) | 0.64 | 7 (8.0) | 0.47 | 3 (5.6) | 0.35 | 23 (9.8) | 0.53 |
| Hypoalbuminemia | 8 (8.5) | 0.40 | 9 (10.3) | 0.61 | 2 (3.7) | 0.23 | 19 (8.1) | 0.43 |
| Investigations | ||||||||
| Aspartate aminotransferase increased | 17 (18.1) | 0.84 | 20 (23.0) | 1.34 | 1 (1.9) | 0.12 | 38 (16.2) | 0.87 |
| Blood alkaline phosphatase increased | 18 (19.1) | 0.89 | 13 (14.9) | 0.87 | 2 (3.7) | 0.23 | 33 (14.0) | 0.76 |
| Alanine aminotransferase increased | 12 (12.8) | 0.59 | 16 (18.4) | 1.08 | 1 (1.9) | 0.12 | 29 (12.3) | 0.66 |
| Weight decreased | 10 (10.6) | 0.50 | 6 (6.9) | 0.40 | 3 (5.6) | 0.35 | 19 (8.1) | 0.43 |
| Nervous system disorders | ||||||||
| Headache | 18 (19.1) | 0.89 | 19 (21.8) | 1.28 | 2 (3.7) | 0.23 | 39 (16.6) | 0.89 |
| Dizziness | 7 (7.4) | 0.35 | 10 (11.5) | 0.67 | 3 (5.6) | 0.35 | 20 (8.5) | 0.46 |
| Skin and subcutaneous tissue | ||||||||
| Pruritus | 11 (11.7) | 0.55 | 5 (5.7) | 0.34 | 1 (1.9) | 0.12 | 17 (7.2) | 0.39 |
| Rash | 1 (1.1) | 0.05 | 4 (4.6) | 0.27 | 7 (13.0) | 0.81 | 12 (5.1) | 0.27 |
| Palmar-plantar erythrodysesthesia syndrome | 0 | — | 0 | — | 11 (20.4) | 1.27 | 11 (4.7) | 0.25 |
| Musculoskeletal and connective tissue disorders | ||||||||
| Back pain | 18 (19.1) | 0.89 | 13 (14.9) | 0.87 | 3 (5.6) | 0.35 | 34 (14.5) | 0.78 |
| Myalgia | 7 (7.4) | 0.35 | 11 (12.6) | 0.74 | 0 | — | 18 (7.7) | 0.41 |
| Vascular disorders | ||||||||
| Hypotension | 18 (19.1) | 0.89 | 18 (20.7) | 1.21 | 0 | — | 36 (15.3) | 0.82 |
| Hypertension | 10 (10.6) | 0.50 | 13 (14.9) | 0.87 | 0 | — | 23 (9.8) | 0.53 |
| Blood and lymphatic system disorders | ||||||||
| Anemia | 19 (20.2) | 0.94 | 18 (20.7) | 1.21 | 9 (16.7) | 1.04 | 46 (19.6) | 1.05 |
| Thrombocytopenia | 12 (12.8) | 0.59 | 10 (11.5) | 0.67 | 4 (7.4) | 0.46 | 26 (11.1) | 0.60 |
| Respiratory, thoracic, and mediastinal disorders | ||||||||
| Dyspnea | 8 (8.5) | 0.40 | 7 (8.0) | 0.47 | 6 (11.1) | 0.69 | 21 (8.9) | 0.48 |
| Cardiac disorders | ||||||||
| Tachycardia | 13 (13.8) | 0.64 | 15 (17.2) | 1.01 | 2 (3.7) | 0.23 | 30 (12.8) | 0.69 |
Serious treatment-emergent AEs were reported for 46.8%, 36.8%, and 27.8% of patients in arm A, B, and C, respectively. Across all patients, the most frequently reported SAE other than disease progression (8.5%) was abdominal pain (4.3%), which was not considered related to the study drug. Overall, 13.2% of patients reported an AE leading to death, none of which was related to the study drugs. The incidence of deaths occurring up until data cutoff was 17%, 9.2%, and 5.6% in arms A, B, and C, respectively, with the primary cause of death being progressive disease. One subject in arm B reported an SAE of Listeria bacteremia, occurring after the final CRS-207 administration, which was deemed treatment related by the investigator. The infection resolved after completing antibiotics and subsequent cultures were negative; the patient continued in the follow-up portion of the study.
Neutrophil/lymphocyte ratio.
In a post hoc, pooled analysis of the primary and second-line cohorts, the baseline neutrophil/lymphocyte ratio (NLR) was associated with outcome. Patients with baseline NLR ≤5 (n = 216) demonstrated improved survival over patients with NLR > 5 (n = 85; HR 0.46; 95% CI, 0.35–0.62; Fig. 5). Baseline NLR was well balanced between arms (Supplementary Table S1).
Figure 5.
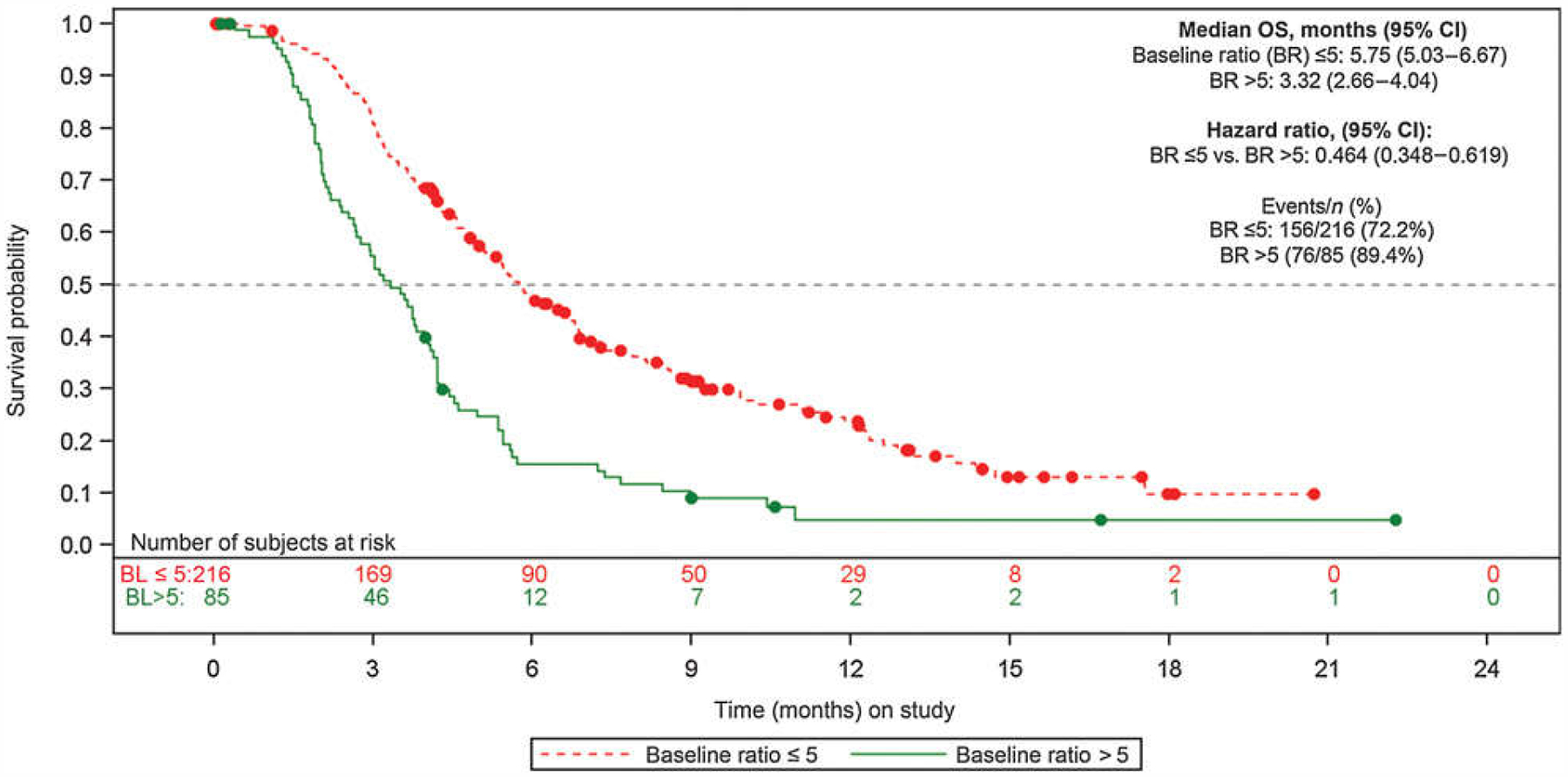
Neutrophil/lymphocyte ratio. NLR >5 N = 85: arm A = 28, arm B = 26, arm C = 31; NLR ≤ 5 N = 216: arm A = 74, arm B = 72, arm C = 70.
Discussion
Despite the emergence of more effective chemotherapeutic combinations, the prognosis of metastatic pancreatic ductal adenocarcinoma remains poor, with a median OS of about 1 year and a 5-year survival rate of <5% (2, 13). Once metastatic pancreatic cancer progresses on first-line chemotherapy, prognosis is dismal and treatment options are even more limited. Novel therapies are therefore greatly needed, and immunotherapy has become a focus of investigation due to its favorable toxicity profile and the potential for durable response.
In the current trial, the immunotherapeutic combination of Cy/GVAX + CRS-207 was well tolerated, but did not improve survival over standard chemotherapy. Nevertheless, some important observations drawn from this trial may guide the process of developing cancer immunotherapeutic agents and designing trials to compare conventional and novel therapies. Identification of the study population was based on a subset analysis from a prior randomized phase IIa study (10) that suggested benefit of Cy/GVAX + CRS-207 over Cy/GVAX alone as third-line therapy for pancreatic cancer. Lines of therapy were retrospectively calculated, which produced artificial subsets, as regimens can be given in different stages of disease. In the current study, a prior line of therapy referred to chemotherapy administered specifically for metastatic disease. Therefore, one could speculate that patients in the second-line cohort may have received multiple lines of chemotherapy, one or more as treatment for localized disease and an additional line for metastatic disease. Indeed, 34.6%, 41.4%, and 36.4% of second-line cohort patients in arms A, B, and C, respectively, had previously received more than one prior chemotherapy regimen. Enrolling patients who have received multiple lines of chemotherapy but are still stable enough to enroll in a clinical trial may select for patients with favorable disease biology (i.e., slower growth kinetics and ongoing response or stability with standard chemotherapy). Compared with the prior study, patients on the current study had higher CA 19–9 levels, higher rates of poorly differentiated tumors, and higher rates of liver involvement, all of which may have influenced the poorer outcomes. However, these poor prognostic factors reflect the real-world status of pancreatic cancer patients upon presentation. Baseline NLR has been reported to correlate with prognosis. In our study cohort, a baseline NLR ≤5 correlated with improved survival in a pooled analysis, consistent with previous studies (14). Post hoc generated Gustave Roussy Immune score (GRIm) was also well balanced between study cohorts, corroborating the NLR results. In arm A, 26%, 16.4%, and 2.7% of subjects had GRIm scores of 1, 2, and 3, respectively, compared with 34.3%, 13.4%, and 3% in arm B, and 34.7%, 13.9%, and 1.4% in arm C, respectively.
A disproportionate number of patients in the single-agent chemotherapy arm discontinued after randomization and prior to first dose (40% in the primary cohort, 63% in the second-line cohort). Presumably, these patients, who had already failed multiple lines of chemotherapy, withdrew upon randomization to receive single-agent chemotherapy in order to pursue more aggressive and novel options. This is in contrast to the NAPOLI-1 trial, which was a global study where 90% of patients randomized to the fluorouracil/folinic acid arm received study assigned treatment despite 70% of these patients having received only ≤1 prior therapy for metastatic disease (3). In this study, 21%, 37%, and 49% of patients in arms A, B, and C of the primary cohort went on to receive subsequent lines of therapy and 67% of the time these were combination chemotherapy regimens, indicating that these patients may have been more accepting of combination treatments. The high dropout rate in the chemotherapy arm prior to patients receiving any treatment illustrates the difficulty in running open-label randomized trials comparing novel agents with standard chemotherapy.
A small subset of patients who had stable disease upon enrollment may have benefited from immunotherapy (Fig. 4); however, the absolute number of patients in this group was small. Interestingly, OS among patients who received CRS-207 monotherapy patients was 5.4 months, which was numerically better than chemotherapy. In a treatment-refractory patient population, an OS of 5.4 months is potentially meaningful.
The immunosuppressive environment of a patient with pancreatic cancer both at the systemic and local tumor microenvironment levels remains difficult to surmount with immunotherapy strategies. When administered before surgery to patients with resectable pancreatic cancer, GVAX pancreas can induce infiltration of immune cells into tumors and the formation of intratumoral lymphoid aggregates, potentially turning tumors from “cold” to “hot” (15, 16). However, the actual clinical benefit remains unclear. Trials testing checkpoint inhibitors, such as cytotoxic T lymphocyte antigen-4 (CTLA-4) or programmed death (PD-1) antagonists, have demonstrated only rare objective responses (17–20) in pancreatic cancer, in particular those with microsatellite, unstable tumors. The next generation of immunotherapy studies are combining antigen-based therapies with checkpoint inhibitors to convert tumors from “cold” to “hot,” while removing inhibition from cytotoxic T cells (NCT03190265, NCT03006302, and NCT02243371). Ultimately, even more complex strategies may be required to elicit a productive antitumor response in the hostile pancreatic cancer microenvironment. As a result, emerging agents that inhibit immunosuppressive pathways such as indoleamine 2,3-dioxygenase (IDO) and adenosine, as well as ones that activate stimulatory pathways, such as OX40 agonists, are actively being developed and incorporated into novel immunotherapeutic combinations (21, 22).
Supplementary Material
Translational Relevance.
The poor prognosis of metastatic pancreatic ductal adenocarcinoma combined with its resistance to conventional treatment such as chemotherapy and radiation necessitates the need for novel therapies. Immunotherapies are widely researched due to the potential for durable response and a favorable toxicity profile. In the current trial, although the immunotherapeutic combination of cyclophosphamide (Cy)/GVAX (granulocyte-macrophage colony-stimulating factor-secreting allogeneic pancreatic tumor cells) + CRS-207 (live, attenuated Listeria monocytogenes expressing mesothelin) was well tolerated, it did not show a survival benefit over chemotherapy in subjects with previously treated metastatic pancreatic adenocarcinoma. Notably, survival of subjects receiving CRS-207 alone appeared similar to that of subjects treated with chemotherapy. Nevertheless, this trial illustrates the difficulties in conducting randomized trials testing novel agents against a reference therapy in a previously treated patient population. Furthermore, immunotherapeutic strategies with novel combinations may be necessary for further development in difficult-to-treat cancers.
Acknowledgments
The authors thank Jocelyn Hybiske, PhD, an independent consultant, for providing editorial services, funded by Aduro Biotech. The authors also thank the families of the patients who participated in the study.
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
Disclosure of Potential Conflicts of Interest
D.T. Le reports receiving commercial research grants from Aduro Biotech. A.H. Ko reports receiving commercial research grants to his institution from Celgene, Halozyme, Roche/Genentech, and Aduro Biotech, and is a consultant/advisory board member for Erytech, Celgene, and ARMO Biosciences. Z.A. Wainberg is a consultant/advisory board member for Merck, Five Prime Therapeutics, Novartis, and Lilly. H. Kindler is a consultant/advisory board member for AstraZeneca, Merck, Aldeyra Therapeutics, Astellas, Boehinger Ingelheim, Bristol-Myers Squibb, Erytech, Five Prime Therapeutics, Ipsen, Kyowa, and Paredox Therapeutics. A. Wang-Gillam is a consultant/advisory board member for Tyme, Merrimack, Ipsen, Bristol-Myers Squibb, Pfizer, Jacobio, and Newlink. P. Oberstein reports receiving commercial research grants from Merck; reports receiving other commercial research support from Halozyme, Genentech, Incyte, and AstraZeneca; and is a consultant/advisory board member for Merck, Purdue Pharma, Celgene, Eisai, OncLive, Tyme, Ipsen, Pfizer, Haolzyme, and Angiodynamics. H.J. Zeh III reports receiving commercial research grants from Merck Sharp & Dohme and speakers bureau honoraria from Intuitive Surgical. E. Borazanci reports receiving speakers bureau honoraria from Ipsen, Taiho, Biogen, Genzyme, Novartis, Teva, and Genentech, and is a consultant/advisory board member for Corcept, Ipsen, and Fujifilm. T. Crocenzi reports receiving other commercial research support from Bristol-Myers Squibb and AstraZeneca. A. Murphy holds ownership interest (including patents) in Aduro Biotech. A. Enstrom is an employee of Tempest Therapeutics and Amplion. D.G. Brockstedt is an employee of and holds ownership interest (including patents) in Aduro Biotech. E.M. Jaffee is an employee of Lustgarten Foundation; reports receiving commercial research grants from Aduro Biotech and Bristol-Myers Squibb; reports receiving other commercial research support from Amgen and Hertig; holds ownership interest (including patents) in Aduro Biotech; and is a consultant/advisory board member for CSTONE, DragonFly, and Genocea. No potential conflicts of interest were disclosed by the other authors.
References
- 1.Pancreatic Cancer Treatment (PDQ)-Health Professional Version; [about 4 screens]. [cited 2018 Mar 6]. National Cancer Institute; Available from: https://www.cancer.gov/types/pancreatic/hp/pancreatic-treatment-pdq. [Google Scholar]
- 2.Pancreatic cancer. Oklahoma City (OK): American Cancer Society; 2014. Available from: http://www.cancer.org/acs/groups/cid/documents/webcontent/003131-pdf.pdf. [Google Scholar]
- 3.Wang-Gillam A, Li CP, Bodoky G, Dean A, Shan YS, Jameson G, et al. Nanoliposomal irinotecan with fluorouracil and folinic acid in metastatic pancreatic cancer after previous gemcitabine-based therapy (NAPOLI-1): a global, randomised, open-label, phase 3 trial. Lancet 2016;387:545–57. [DOI] [PubMed] [Google Scholar]
- 4.Santoni M, Battelli N, Buti S. Durvalumab in stage III non-small-cell lung cancer. N Engl J Med 2018;378:869. [DOI] [PubMed] [Google Scholar]
- 5.Neelapu SS, Locke FL, Bartlett NL, Lekakis LJ, Miklos DB, Jacobson CA, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med 2017;377:2531–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Neil BH, Wallmark JM, Lorente D, Elez E, Raimbourg J, Gomez-Roca C, et al. Safety and antitumor activity of the anti-PD-1 antibody pembrolizumab in patients with advanced colorectal carcinoma. PLoS One 2017;12: e0189848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang JH, Jiang Y, Pillarisetty VG. Role of immune cells in pancreatic cancer from bench to clinical application: an updated review. Medicine 2016;95: e5541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le DT, Brockstedt DG, Nir-Paz R, Hampl J, Mathur S, Nemunaitis J, et al. A live-attenuated Listeria vaccine (ANZ-100) and a live-attenuated Listeria vaccine expressing mesothelin (CRS-207) for advanced cancers: phase I studies of safety and immune induction. Clin Cancer Res 2012;18:858–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brockstedt DG, Giedlin MA, Leong ML, Bahjat KS, Gao Y, Luckett W, et al. Listeria-based cancer vaccines that segregate immunogenicity from toxicity. PNAS 2004;101:13832–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Le DT, Wang-Gillam A, Picozzi V, Greten TF, Crocenzi T, Springett G, et al. Safety and survival with GVAX pancreas prime and Listeria Monocyto-genes-expressing mesothelin (CRS-207) boost vaccines for metastatic pancreatic cancer. J Clin Oncol 2015;33:1325–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laheru D, Lutz E, Burke J, Biedrzycki B, Solt S, Onners B, et al. Allogeneic granulocyte macrophage colony-stimulating factor-secreting tumor immunotherapy alone or in sequence with cyclophosphamide for metastatic pancreatic cancer: a pilot study of safety, feasibility, and immune activation. Clin Cancer Res 2008;14:1455–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolchok JD, Hoos A, O’Day S, Weber JS, Hamid O, Lebbe C, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res 2009;15: 7412–20. [DOI] [PubMed] [Google Scholar]
- 13.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359–86. [DOI] [PubMed] [Google Scholar]
- 14.Chen Y, Yan H, Wang Y, Shi Y, Dai G. Significance of baseline and change in neutrophil-to-lymphocyte ratio in predicting prognosis: a retrospective analysis in advanced pancreatic ductal adenocarcinoma. Sci Rep 2017;7: 753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Remigis A, de Gruijl TD, Uram JN, Tzou SC, Iwama S, Talor MV, et al. Development of thyroglobulin antibodies after GVAX immunotherapy is associated with prolonged survival. Int J Cancer 2015;136:127–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soares KC, Rucki AA, Kim V, Foley K, Solt S, Wolfgang CL, et al. TGF-beta blockade depletes T regulatory cells from metastatic pancreatic tumors in a vaccine dependent manner. Oncotarget 2015;6:43005–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012;12:252–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Overman MJ, McDermott R, Leach JL, Lonardi S, Lenz HJ, Morse MA, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 2017;18: 1182–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weber JS, D’Angelo SP, Minor D, Hodi FS, Gutzmer R, Neyns B, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 2015;16: 375–84. [DOI] [PubMed] [Google Scholar]
- 20.Sharma P, Retz M, Siefker-Radtke A, Baron A, Necchi A, Bedke J, et al. Nivolumab in metastatic urothelial carcinoma after platinum therapy (CheckMate 275): a multicentre, single-arm, phase 2 trial. Lancet Oncol 2017;18:312–22. [DOI] [PubMed] [Google Scholar]
- 21.Zhai L, Ladomersky E, Lenzen A, Nguyen B, Patel R, Lauing KL, et al. IDO1 in cancer: a Gemini of immune checkpoints. Cell Mol Immunol 2018; 15:447–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weinberg AD, Morris NP, Kovacsovics-Bankowski M, Urba WJ, Curti BD. Science gone translational: the OX40 agonist story. Immunol Rev 2011; 244:218–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


