Abstract
We assessed the ability of high-risk criteria developed by Boston Health Care for the Homeless Program to identify increased mortality during a 10-year cohort study (January 2000–December 2009) of 445 unsheltered adults. To qualify as high-risk for mortality, an individual slept unsheltered for six consecutive months or longer plus had one or more of the following characteristics: tri-morbidity, defined as co-occurring medical, psychiatric, and addiction diagnoses; one or more inpatient or respite admissions; three or more emergency department visits; 60 years old or older; HIV/AIDS; cirrhosis; renal failure; frostbite, hypothermia, or immersion foot. A total of 119 (26.7%) individuals met the high-risk criteria. The remaining 326 individuals in the cohort were considered lower-risk. During the study, 134 deaths occurred; 52 (38.8%) were among high-risk individuals. Compared with sheltered individuals, the age-standardized mortality ratio for the high-risk group was 4.0 (95% confidence interval 3.0, 5.2) times higher and for the lower-risk group was 2.2 (1.8, 2.8) times higher. The hazard ratio, a measure of survival, for the high-risk group was 1.7 (1.2, 2.4) times that of the lower-risk group. High-risk criteria predicted an increased likelihood of mortality among unsheltered individuals. The lower-risk group also had high mortality rates compared with sheltered individuals.
Keywords: Homeless persons, unsheltered, mortality, vulnerability
Homelessness remains a major issue in the United States. According to the U.S. Department of Housing and Urban Development (HUD) Annual Homeless Assessment Report to Congress, nearly two million people experienced homelessness in 2017.1 On a single night in January 2017 in the U.S., approximately 550,996 people were homeless, of whom 190,094 (34.5%) were living unsheltered, also known as sleeping rough.1 The majority (69%) of individuals living unsheltered were chronically homeless, defined by HUD as individuals with a diagnosable disability who have been continuously homeless for one year or longer or have experienced four or more episodes of homelessness over the previous three years.1,2 Chronically homeless persons make up approximately 10–15% of the general homeless population but use 50% or more of the available emergency services.1,3 In an effort to improve health outcomes and decrease use of costly health and social services for the unsheltered chronically homeless population, securing housing in permanent supportive housing (PSH) programs, such as Housing First, has been a key strategy for this vulnerable group.4
A sparse but growing literature suggests that unsheltered individuals in the U.S. are homeless longer than their sheltered homeless counterparts, are sicker, and bear a higher burden of co-occurring medical, psychiatric, and substance use disorders.5–8 These individuals also use emergency services more frequently and lack continuity of care.6,7,9 The unsheltered population has been shown to have a high burden of risk factors for mortality and a higher mortality rate than sheltered individuals.10,11
Previous research identified risk factors for mortality in a sheltered homeless population in Boston.12–14 Clinicians and homeless service providers at the Boston Health Care for the Homeless Program (BHCHP) adapted these risk factors into high-risk criteria for use in clinical and research contexts with the unsheltered population to understand better the risk factors for morbidity and mortality. Later, a PSH organization, Common Ground (now known as Community Solutions), further adapted the high-risk criteria to create a Vulnerability Index (VI) to prioritize individuals for PSH, even though the criteria had not been developed or validated for this purpose.15,16
In this study, we aim to determine if the high-risk criteria developed by BHCHP predicted an increased risk of mortality in a cohort of unsheltered individuals. This paper describes and assesses these criteria through survival analysis and age-standardized all-cause and cause-specific mortality rates. We used the 2000–2009 Massachusetts adult population and a 2003–2008 sheltered homeless cohort from Boston as comparison groups. These data are unique as these are the only longitudinal data available on unsheltered adults in the U.S. We hypothesized that the high-risk criteria would predict significantly high mortality rates and that those in the lower-risk group would still experience excess mortality compared with sheltered individuals and the general population.
Methods
Study design and study population.
We conducted a 10-year prospective study from January 1, 2000 to December 31, 2009 of 445 unsheltered adult patients of BHCHP’s street team, as described in depth elsewhere.11 The street team is a multidisciplinary team of clinicians who care for unsheltered adults where they live (i.e., on the streets, on park benches, under bridges). The analytic cohort consisted of individuals aged 18 years and older who had slept outside for at least one night and had at least one face-to-face encounter with a BHCHP street team clinician during the year 2000. Our study received institutional review board approval from Boston University Medical Center and Harvard T.H. Chan School of Public Health.
Data collection.
Data were collected at initial and subsequent encounters and consisted of demographic characteristics, encounter time and location, and reason for visit. The database was updated with each patient encounter. Date and cause of death were added to the database when a patient was known to have died. Upon enrollment, a medical chart review was conducted to determine if an individual met the criteria described below. Individuals who met the criteria were considered high-risk for mortality and individuals who did not meet criteria were considered lower-risk for mortality. The high-risk variable was dichotomous, and the qualifying criteria were not recorded in the database. The high-risk variable had no missing data. All individuals received the same care from BHCHP regardless of risk stratification.
Study groups.
We used standardized mortality ratios (SMR) to compare mortality rates in the unsheltered study cohort to the 2000–2009 Massachusetts adult population and a 2003–2008 sheltered homeless cohort.11,17 Data for the Massachusetts population were taken from the Centers for Disease Control and Prevention (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER) for ages 18 to 84 years from 2000–2009.11 Data for the adult homeless cohort were obtained from the 2013 study by Baggett et al., and included 28,033 homeless adults 18 years old or older who had one or more encounters with a BHCHP clinician between January 1, 2003 to December 31, 2008.11,17
Development of the high-risk for mortality criteria.
The criteria were developed by BHCHP based on clinical evidence and homelessness mortality studies conducted at BHCHP during the later 1990s.12–14,18 The criteria were heavily influenced by the findings from a small cluster of 12 deaths among unsheltered Boston adults during the winter of 1998–99 and the causes and risk factors for death found in two early homelessness mortality studies.12–14,18 Research into the cluster of deaths showed that three-quarters had been seen in an emergency department or had an inpatient admission within three weeks of death, half had been admitted to BHCHP’s medical respite program, a 24-hour nursing and medical program for homeless individuals who no longer require hospitalization, during the six months prior to death, most (87%) had been at a detoxification unit within six weeks of death, most (66%) suffered “tri-morbidity” (i.e., co-occurring medical, psychiatric, and addiction diagnoses), all had major medical issues and an active substance use disorder, and two-thirds had a major mental illness.14,18 Previous research showed HIV/AIDS to be leading cause of death and that a subgroup of the homeless population had an extremely high risk of death due to certain medical conditions such as renal disease, liver disease, and arrhythmias.12,13,18 In the years following these 12 street deaths and the homeless mortality studies, BHCHP prospectively followed a cohort of unsheltered adults to evaluate mortality risk over time using the high-risk criteria.
The high-risk criteria were: an unsheltered individual age 18 or older had been sleeping on the streets for six consecutive months or more, plus any one or more of the following criteria: suffered from tri-morbidity; one or more inpatient admission(s) or BHCHP respite admission(s) anytime during the previous year; three or more visits to the emergency department in previous three months; 60 years old or older; HIV/ AIDS diagnosis; cirrhosis, end-stage liver disease, or renal failure diagnosis; and/or history of frostbite, hypothermia, or immersion foot. The BHCHP medical respite unit is a facility where homeless or previously homeless adults can be admitted to recover from medical issues when they do not need to be admitted to the hospital but are too ill to recover in a shelter or on the streets. Tri-morbidity was assessed by medical chart review through the diagnoses listed in a patient’s BHCHP chart. When a member of the cohort had medical, psychiatric, and addiction diagnoses listed in their chart, they were considered to have tri-morbidity.
Statistical analyses.
Statistical analyses were performed using Stata®14 (StataCorp, College Station, TX) and Microsoft® Office Excel 2013. The risk groups were used as standard populations for age-standardized mortality ratio calculations. The dates and causes of death were confirmed by linking the study database to the Massachusetts Department of Public Health death occurrence files using LinkPlus 2.0, as described in Roncarati et al. 2018.11 The SMRs were calculated in the same method also described in Roncarati et al. 2018: creating age-specific per person-year mortality rates for the young, middle, and old age categories for Massachusetts population and the sheltered homeless cohort; multiplying the age-specific per person-year mortality rates by age-specific person-year for both risk groups; summing the three age-specific products separately for the risk groups to determine the expected number of deaths for each group; and dividing the number of observed deaths by the number of expected deaths separately for both risk groups.11 Standardized mortality ratios were calculated when the number of deaths in a category was five or more and 95% confidence intervals (CI) were calculated for the SMRs.
We also created Kaplan-Meier Survival Estimate curves by risk level and assessed for differences in survival by risk level using age-stratified Log-Rank Tests for Equality. We then modeled time until death using a Cox Proportional Hazard Model controlling for age, race/ethnicity, and gender. Significance of multi-category prediction (i.e., age and race/ethnicity) was assessed using a Likelihood Ratio Test. A significance level of <.05 was used for all statistical testing.
Results
Cohort characteristics.
Of 445 unsheltered adults in the study cohort, 119 (26.7%) met the high-risk for mortality criteria. Those in the high-risk group were older and more likely to be white than the lower-risk group (Table 1). Characteristics of the Massachusetts adult population and sheltered homeless cohort can be found in Roncarati et al. 2018.11
Table 1.
CHARACTERISTICS OF UNSHELTERED COHORT, 2000–2009
| Characteristic | Cohort N=445 N (%) | High-Riska N=119 N (%) | Lower-Risk N=326 N (%) | Decedents N=134 N (%) |
|---|---|---|---|---|
| Age (years) | ||||
| 18–44 | 248 (55.7) | 57 (47.9) | 191 (58.6) | 56 (41.8) |
| 45–64 | 176 (39.6) | 57 (47.9) | 119 (36.5) | 65 (48.5) |
| ≥65 | 21 (4.7) | 5 (4.2) | 16 (4.9) | 13 (9.7) |
| Race/Ethnicity | ||||
| White | 299 (67.2) | 91 (76.5) | 208 (63.8) | 108 (80.6) |
| Black | 94 (21.1) | 16 (1 3 .4) | 78 (23.9) | 15 (11.2) |
| Persons of Color/ Unknownb | 52 (11.7) | 12 (10.1) | 40 (12.3) | 11 (8.2) |
| Genderc | ||||
| Men | 322 (72.4) | 91 (76.5) | 231 (70.9) | 116 (86.6) |
| Women | 123 (27.6) | 28 (23.5) | 95 (29.1) | 18 (13.4) |
| Risk-Level | ||||
| High-Risk | 119 (26.7) | 52 (38.8) | ||
| Lower-Risk | 326 (73.3) | 82 (61.2) | ||
Notes:
High-risk individuals slept unsheltered ≥6 consecutive months and met ≥1 criteria: tri-morbidity; ≥1 hospital admission or BHCHP respite admission during previous year due to major medical issue(s); ≥3 ED visits during previous 3 months; ≥60 years old; HIV or AIDS; cirrhosis, end stage liver disease, or renal failure; and/or history of frostbite, hypothermia, or immersion foot.
Persons of Color/Unknown Race/Ethnicity category contains individuals who reported their race/ ethnicity to be American Indian, Hispanic, Asian, or race/ethnicity was unknown.
No missing data for gender.
Mortality rates.
During the study, 134 deaths occurred, including 52 (38.8%) in the high-risk group. The all-cause SMR for the high-risk group was 15.5 (95% CI 11.7, 20.2) times that of the Massachusetts adult population and 4.0 (95% CI 3.0, 5.2) times that of the sheltered homeless cohort (Table 2). The all-cause SMR for the lower-risk group was 7.9 (95% CI 6.3, 9.8) times that of the Massachusetts adult population and 2.2 (95% CI 1.8, 2.8) times that of the sheltered homeless cohort (Table 2).
Table 2.
ALL-CAUSE MORTALITY & CAUSE-SPECIFIC AGE-STANDARDIZED MORTALITY RATIOS FOR UNSHELTERED COHORT, 2000–2009 BY RISK-LEVEL COMPARED WITH MASSACHUSETTS, 2000–2009 AND TO SHELTERED COHORT, 2003–2008A
| High-Riskb | Lower-Risk | |||||
|---|---|---|---|---|---|---|
| Underlying Cause of Deathc,d | N(%) MAg | SMR (95% CI) high-risk vs. sheltered | SMRe (95% CI)f high-risk vs. cohort | N(%) MA | SMR (95% CI) lower-risk vs. sheltered | SMR (95% CI) lower-risk vs. cohort |
| All-Cause | ||||||
| Total population | 52 (100) | 15.5 (11.7, 20.2) | 4.0 (3.0, 5.2) | 82 (100) | 7.9 (6.3, 9.8) | 2.2 (1.8, 2.8) |
| Men | 45 (86.5) | 15.0 (11.1, 19.9) | 4.2 (3.1, 5.6) | 71 (86.6) | 7.4 (5.8, 9.2) | 2.4 (1.9, 3.0) |
| Women | 7 (13.5) | 9.5 (4.2, 18.8) | 3.0 (1.2, 5.7) | 11 (1 3 .4) | 5.4 (2.9, 9.5) | 1.6 (.9, 2.8)i |
| Natural Causes | ||||||
| Chronic Liver Disease | 11 (21.2) | 86.0 (45.0, 150.0) | 11.7 (6.2, 20.4)d | |||
| Cancer | 9 (17.3) | 8.1 (4.0, 15.0) | 4.5 (2.2, 8.2) | 12 (14.6) | 3.7 (2.0, 6.3) | 2.2 (1.2, 3.7) |
| Heart Disease | 7 (13.5) | 10.4 (4.5, 20.5) | 3.5 (1.5, 7.0) | 11 (13.4) | 5.2 (2.7, 9.0) | 2.0 (1.0, 3.4)i |
| Chronic Substance Use | 5 (9.6) | 104.2 (38.1, 231.0) | 4.9 (1.8, 10.9) | 11 (13.4) | 83.5 (43.8, 144.8) | 4.0 (2.0, 6.8) |
| HIV/AIDS | 5 (9.6) | 122.3 (44.8, 271.1) | 6.5 (2.4, 14.4) | 5 (6.1) | 43.1 (15.8, 95.5) | 2.3 (.8, 5.1)i |
| External Causes | ||||||
| Injuries, non-poisoningh | 6 (11.5) | 44.0 (17.8, 91.6) | 8.4 (3.4, 17.5) | 13 (15.9) | 30.0 (16.7, 50.0) | 6.7 (3.7, 11.1) |
| Drug overdose (poisoning)d | 7 (8.5) | 16.2 (7.1, 32.1) | 1.1 (.5, 2.1)i | |||
| Substance Use Causes | ||||||
| Substance Use | 17 (32.7) | 75.2 (45.2, 117.9) | 4.1 (2.5, 6.5) | 22 (26.8) | 32.9 (21.1, 48.9) | 1.9 (1.2, 2.8) |
| Alcohol | 16 (30.8) | 212.5 (125.8, 337.7) | 14 (17.1) | 71.1 (40.5, 116.4) | ||
| Opioid | d | 8 (9.8) | 18.4 (8.5, 34.9) | |||
Notes:
Sheltered Cohort from Baggett, TP et al. Mortality Among Homeless Adults in Boston: Shifts in Causes of Death Over a 15-Year Period. JAMA 2013 Feb; 173(3):189–95
High-risk individuals slept unsheltered ≥6 consecutive months and met ≥1 criteria: tri-morbidity; ≥1 hospital admission or BHCHP respite admission during previous year due to major medical issue(s); ≥3 ED visits during previous 3 months; ≥60 years old; HIV or AIDS; cirrhosis, end stage liver disease, or renal failure; and/or history of frostbite, hypothermia, or immersion foot
No unknown Causes of Death
Causes of death <5 were suppressed; these were: diseases of digestive system, Influenza and Pneumonia, Chronic Lower Respiratory Disease, Infection (Sepsis, Viral Hepatitis), Anoxic Brain Injury, Cerebrovascular Disease, Renal Failure, Central Nervous System Disease, Mental Disorder, Ill-Defined Conditions, Suicide, Homicide
SMR is Standardized Mortality Ratio and were calculated for deaths ≥5
CI is Confidence Interval
MA is Massachusetts
Injuries, non-poisoning category contains Transportation Accidents codes V01-V99, Other External Causes of Accidental Injuries codes W00-X59 except for X40-X49 which represent accidental poisonings by noxious substances, and Events of Undetermined Intent codes Y20-Y34 except for codes Y10-Y19 which represent poisonings of undetermined intent. Methodology in collapsing ICD-10 categories based on similar methodology in Health of Boston 2014–2015 Report from the Boston Public Health Commission: http://www.bphc.org/healthdata/health-of-boston-report/Documents/HOB-2014–2015/FullReport_HOB_2014–2015.pdf
SMR not significant at p-value <.05 level; all SMRs without symbol were significant at p-value <.05
Causes of death.
Among the unsheltered homeless group, the highest rates of death for the high-risk group were for conditions directly attributable to substance use, especially alcohol; communicable diseases such as HIV/AIDs; injuries such as falls, drownings, and hypothermia; and noncommunicable disease such as cancer and heart disease (Table 2). All comparisons with the high-risk group were statistically significant. The lower-risk group cause-specific SMRs were about half those of the high-risk group but were still high compared with the population of Massachusetts and a sheltered cohort in Boston. The patterns for cause-specific SMRs were similar to the high-risk group with a few differences. The lower-risk group had SMRs, including their confidence intervals, that demonstrated statistical significance for substance use, but with more opioid-attributable deaths; a statistically significant SMR for HIV/AIDS compared with Massachusetts but not significant compared with the sheltered cohort; a statistically significant SMR for injuries; and statistically significant SMRs for heart disease and cancer compared with Massachusetts yet only significant for cancer when compared with the sheltered cohort. Overdose deaths occurred evenly throughout the study. The overdose deaths were not clustered. On average there was one overdose death per year. The overdose deaths primarily occurred among the younger lower-risk group.
Survival analysis.
Among the unsheltered homeless group, the high-risk group’s Kaplan-Meier Survival Estimate curves showed lower probabilities of survival at five and 10 years compared with the low-risk group (Fig. 1). Log-Rank Tests for Equality were statistically significant, indicating that the two survival curves were significantly different from each other. The mortality hazard for the high-risk group was 1.7 (95% CI 1.2, 2.4) times that of the lower-risk group, meaning that there were 1.7 times the number of deaths for the high-risk group compared to the lower-risk group (Table 3). Additional variables were included in the survival analysis as controls (Table 3).
Figure 1.
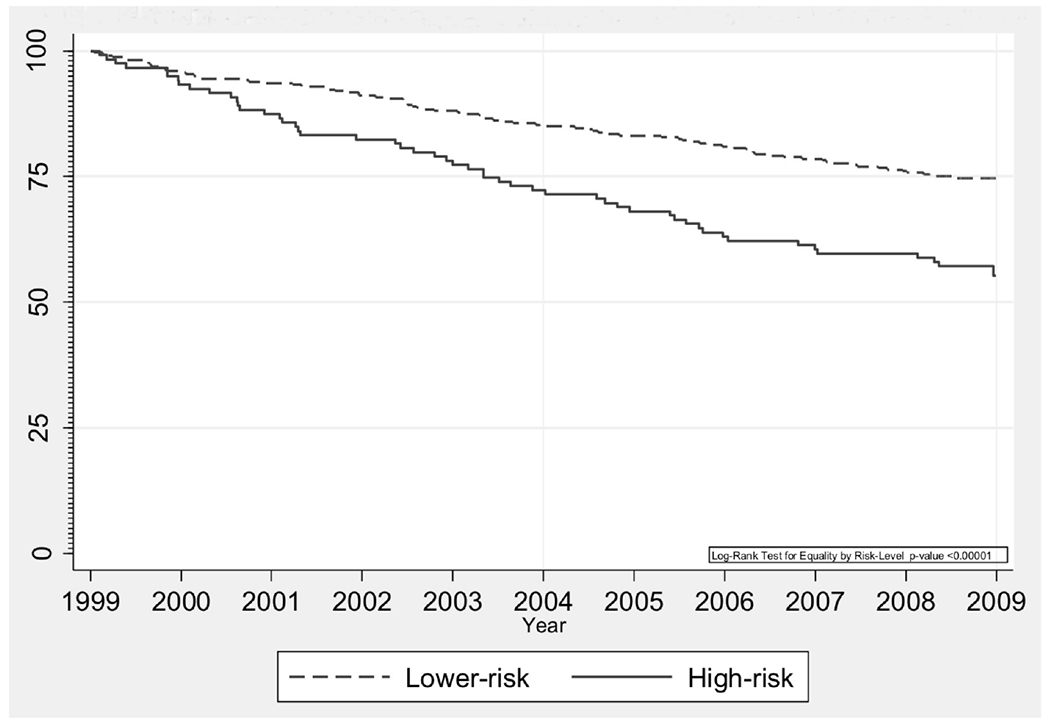
Kaplan-Meier survival estimates for unsheltered cohort by risk-level.
Table 3.
CHARACTERISTICS ASSOCIATED WITH MORTALITY RISK IN THE UNSHELTERED COHORT (N=445)
| Hazard Ratio (95% CI) | p-value (.05) | |
|---|---|---|
| Age (years) | ||
| 18–44 | 1.0 | |
| 45–64 | 1.5 (1.0, 2.1) | .032 |
| 65–84 | 3.6 (2.0, 6.7) | <.0001 |
| Race/Ethnicity | ||
| White | 1.0 | |
| Black | .5 (.3, .8) | .006 |
| Persons of Color/Unknowna | .5 (.3, 1.0) | .054 |
| Genderb | ||
| Women | 1.0 | |
| Men | 2.7 (1.6, 4.4) | <.0001 |
| Risk-Level | ||
| Lower-Risk | 1.0 | |
| High-Riskc | 1.7 (1.2, 2.4) | .003 |
Notes:
Persons of Color/Unknown were individuals who reported their race/ethnicity to be American Indian, Hispanic, Asian, or race/ethnicity was unknown
No missing data for Gender
High-risk individuals slept unsheltered ≥6 consecutive months and met ≥1 criteria: tri-morbidity; ≥1 hospital admission or BHCHP respite admission during previous year due to major medical issue(s); ≥3 ED visits during previous 3 months; ≥60 years old; HIV or AIDS; cirrhosis, end stage liver disease, or renal failure; and/or history of frostbite, hypothermia, or immersion foot
CI is Confidence Interval
Discussion
Our study assessed the ability of criteria developed by BHCHP to identify unsheltered individuals at increased risk of death. This study adds significantly to the growing literature on unsheltered homelessness and mortality among homeless populations. The mortality rate for the high-risk group was 15 times higher than the Massachusetts population and four times higher than a sheltered cohort. Within the unsheltered cohort, Cox modeling showed a 1.7-fold risk of death for the high-risk group compared with the lower-risk group. The all-cause SMR for the lower-risk group was nearly eight times that of Massachusetts’ and more than double that of the sheltered Boston cohort leading us to conclude that both the lower-risk and the high-risk group had substantial risk for mortality.
Individuals in the high-risk group were older on average than those who did not meet the criteria. The older average age for the high-risk group could reflect a greater proportion of chronically homeless individuals in the high-risk group. Unsheltered Black individuals had half the risk of death that unsheltered White individuals in our study had. Higher rates of death for White homeless adults has been a consistent finding across homeless mortality studies although the reasons for this finding remain unknown.12,13,17–20 Further investigation is warranted. Age-adjusted cause-specific SMRs were about twice as high for the high-risk as for the lower-risk group (and were significant). We suggest that the high-risk criteria identified those whose conditions and disabilities were more advanced or of longer duration.
Our study suggests that the high-risk criteria identify those with a greater risk of death, and it also showed that unsheltered homeless persons who did not meet these high-risk criteria were at much higher risk of mortality compared with both a sheltered homeless cohort and to the general population. The high-risk criteria were intended for clinicians who care for unsheltered adults to have an additional clinical tool to heighten their awareness of risk of death for this population. This study was not intended to validate the use of high-risk criteria for the prioritization of individuals for housing nor does it validate the Vulnerability Index (VI). Our (BHCHP’s) high-risk criteria and the VI are related but the purpose and methodology for each differ. The BHCHP criteria were developed to assist clinicians in identifying health conditions and health care utilization patterns that may place unsheltered adults at higher risk of death. In contrast, the VI is a tool to assist in prioritizing both sheltered and unsheltered homeless persons to receive limited housing resources.15,21 The BHCHP criteria are determined through a formal clinical assessment as well as extensive review of medical records, whereas the VI was developed as a self-report survey and has not been fully validated.16,21 The VI has been used as an effective community-organizing tool that has helped prioritize thousands of homeless individuals for placement in PSH in communities throughout the U.S.15,22 Most homeless service providers use some version of the VI to help prioritize PSH. A common version of the VI is called Vulnerability Index-Service Prioritization Decision Assistance Tool or VI-SPDAT created by Community Solutions and OrgCode Consulting, Inc. in 2013.23 The VI-SPDAT is a HUD approved tool for prioritizing chronically homeless persons for resources.23,24
Limitations.
This study has certain limitations. The high-risk criteria used by BHCHP result in a dichotomous variable rather than a continuous score. Future investigation could include each of the criteria in a model instead of using a dichotomous variable to further understand which components of the criteria contribute most to increased mortality. Members of the high-risk group as a result tended to be older on average and likely homeless for longer. However, when age was controlled in the Cox model, the mortality hazard for the high-risk group was 1.7 times higher than that of the lower-risk group. The length of time homeless was not known for the lower-risk group, and future studies should account for the length of homelessness, as well as time spent sleeping outside, to better determine the effects of chronicity on risk of mortality.
As in our previous study, a potential for selection bias exists because some people living on the streets during the enrollment period may not have been encountered by the BHCHP street team.11 This risk was minimized by the street team having a strong network of ties with all outreach workers and services in the Greater Boston area. Our study focused on death data from Massachusetts; deaths occurring in other states were not included in our analysis. Individuals who traveled and subsequently died outside Massachusetts could be a source of selection bias insofar as those individuals capable of travel may differ from those unable or unwilling to do so. This limitation could be addressed in the future by using national death data.
Our study used criteria derived from previous mortality studies and clinical evidence to predict mortality among homeless people living outside in an urban setting. The findings from our study are applicable to similar-sized urban settings within the U.S. Although our data are from 2000–2009, the results are still informative for people experiencing unsheltered homelessness today, primarily since this study encompassed a full decade and to date is the only longitudinal dataset available on this elusive population of unsheltered adults in the U.S.
Conclusions.
Our results confirm that the high-risk for mortality criteria predicted significantly high mortality rates but also that those in the lower-risk group experienced excess mortality compared with sheltered individuals and the general Massachusetts population. The use of these criteria and other measures to prioritize the unsheltered population and other homeless subpopulations is a complex issue. Our findings suggest that sleeping unsheltered, for any length of time, may well be an independent risk factor for increased mortality and a necessary factor in the assessment of vulnerability among homeless populations.
Acknowledgements
Special thanks to my mentors at Harvard T. H. Chan School of Public Health, especially Howard Koh, MD, MPH, Tyler VanderWeele, PhD, and Henning Tiemeier, MD, PhD for their support and encouragement. A thank you to James J. O’Connell, MD and Stacy E. Swain, MPH, MDiv who created the High-Risk for Mortality Criteria in 1999 and enrolled participants in this study. Additional thank you to Stacy E. Swain, MPH, MDiv for creating the database that made this study possible, and to the many research assistants who helped maintain the database. A special thank you to the patients, the daytime and nighttime outreach workers in Boston, and everyone at Boston Health Care for the Homeless Program, especially the Street Team. No one was compensated beyond their normal employment.
Funding/Support
Research described in this publication was supported by award R25CA057711 from the National Cancer Institute of the National Institutes of Health. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures
None reported.
Publisher's Disclaimer: Disclaimer
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Meeting Presentations
This study was presented in part as an abstract as a poster at the 2017 National Health Care for the Homeless Conference & Policy Symposium, Washington, DC, May 21–24, 2017.
Contributor Information
Jill S. Roncarati, Department of Social and Behavioral Sciences at Harvard T. H. Chan School of Public Health, Boston Health Care for the Homeless Program, Dana-Farber Cancer Institute Center for Community-Based Research.
James J. O’Connell, Boston Health Care for the Homeless Program and the Division of General Internal Medicine at Massachusetts General Hospital.
Stephen W. Hwang, MAP Centre for Urban Health Solutions at St. Michael’s Hospital.
Travis P. Baggett, Boston Health Care for the Homeless Program, the Division of General Internal Medicine, and the Tobacco Research and Treatment Center at Massachusetts General Hospital.
Francis E. Cook, Department of Epidemiology, Harvard T. H. Chan School of Public Health.
Nancy Krieger, Department of Social and Behavioral Sciences at the Harvard T. H. Chan School of Public Health.
Glorian Sorensen, Dana-Farber Cancer Institute Center for Community-Based Research and the Department of Social and Behavioral Sciences at Harvard T. H. Chan School of Public Health.
References
- 1.Henry M, Bishop K, de Sousa T, et al. The 2017 Annual Homeless Assessment Report to Congress PART 2: Estimates of homelessness in the United States. Washington, DC: The U.S. Department of Housing and Urban Development, 2018. Available at: https://files.hudexchange.info/resources/documents/2017-AHAR-Part-2.pdf. [Google Scholar]
- 2.Tregoning H, Coloretti NA. Homeless emergency assistance and rapid transition to housing: defining “chronically homeless.” Washington, DC: The U.S. Department of Housing and Urban Development, 2015. Available at: https://www.hudexchange.info/resources/documents/Defining-Chronically-Homeless-Final-Rule.pdf. [Google Scholar]
- 3.Kuhn R, Culhane DP. Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: results from the analysis of administrative data. Am J Community Psychol. 1998. April;26(2):207–32. 10.1023/A:1022176402357 [DOI] [PubMed] [Google Scholar]
- 4.Tsemberis S, Eisenberg RF. Pathways to housing: supported housing for street-dwelling homeless individuals with psychiatric disabilities. Psychiatr Serv. 2000. April;51(4):487–93. 10.1176/appi.ps.51.4.487 [DOI] [PubMed] [Google Scholar]
- 5.Levitt AJ, Culhane DP, DeGenova J, et al. Health and social characteristics of homeless adults in Manhattan who were chronically or not chronically unsheltered. Psychiatr Serv. 2009. July;60(7):978–81. 10.1176/ps.2009.60.7.978 [DOI] [PubMed] [Google Scholar]
- 6.Nyamathi AM, Leake B, Gelberg L. Sheltered versus nonsheltered homeless women differences in health, behavior, victimization, and utilization of care. J Gen Intern Med. 2000. August;15(8):565–72. 10.1046/j.1525-1497.2000.07007.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linton KF, Shafer MS. Factors associated with the health service utilization of unshel-tered, chronically homeless adults. Soc Work Public Health. 2014;29(1):73–80. 10.1080/19371918.2011.619934 [DOI] [PubMed] [Google Scholar]
- 8.Byrne T, Montgomery AE, Fargo JD. Unsheltered homelessness among veterans: correlates and profiles. Community Ment Health J. 2016. February;52(2):148–57. Epub 2015 Aug 20. 10.1007/s10597-015-9922-0 [DOI] [PubMed] [Google Scholar]
- 9.Tsai J, Kasprow WJ, Kane V, Rosenheck RA. Street outreach and other forms of engagement with literally homeless veterans. J Health Care Poor Underserved. 2014. May;25(2):694–704. 10.1353/hpu.2014.0087 [DOI] [PubMed] [Google Scholar]
- 10.Montgomery AE, Szymkowiak D, Marcus J, et al. Homelessness, unsheltered status, and risk factors for mortality: findings from the 100 000 homes campaign. Public Health Rep. 2016. November;131(6):765–72. Epub 2016 Oct 19. 10.1177/0033354916667501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roncarati JS, Baggett TP, O’Connell JJ, et al. Mortality among unsheltered homeless adults in Boston, Massachusetts, 2000–2009. JAMA Intern Med. 2018. September 1;178(9):1242–8. 10.1001/jamainternmed.2018.2924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hwang SW, Lebow JM, Bierer MF, et al. Risk factors for death in homeless adults in Boston. Arch Intern Med. 1998. July 13;158(13):1454–60. 10.1001/archinte.158.13.1454 [DOI] [PubMed] [Google Scholar]
- 13.Hwang SW, Orav EJ, O’Connell JJ, et al. Causes of death in homeless adults in Boston. Ann Intern Med. 1997. April 15;126(8):625–8. 10.7326/0003-4819-126-8-199704150-00007 [DOI] [PubMed] [Google Scholar]
- 14.O’Connell JJ, Mattison S, Judge CM, et al. A public health approach to reducing morbidity and mortality among homeless people in Boston. J Public Health Manag Pract. 2005. Jul-Aug;11(4):311–6. 10.1097/00124784-200507000-00009 [DOI] [PubMed] [Google Scholar]
- 15.Wikipedia. Homeless Vulnerability Index. San Francisco, CA: Wikipedia, 2018. Available at: https://en.wikipedia.org/wiki/Homeless_Vulnerability_Index. [Google Scholar]
- 16.Kanis B Vulnerability Index: prioritizing outreach & housing placement by mortality risk. New York City, NY: Common Ground Community, 2006. Available at: https//:slideplayer.com/slide/7487896/#.XSya57LZzzY.google. [Google Scholar]
- 17.Baggett TP, Hwang SW, O’Connell JJ, et al. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med. 2013. February 11;173(3):189–95. 10.1001/jamainternmed.2013.1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control (CDC). Deaths among the homeless—Atlanta, Georgia. MMWR Morb Mortal Wkly Rep. 1987. May 22;36(19):297–9. [PubMed] [Google Scholar]
- 19.Centers for Disease Control. Deaths among homeless persons—San Francisco, 1985–1990. MMWR Morb Mortal Wkly Rep. 1991. December 20;40(50):877–80. [PubMed] [Google Scholar]
- 20.Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994. August 4;331(5):304–9. 10.1056/NEJM199408043310506 [DOI] [PubMed] [Google Scholar]
- 21.Cronley C, Petrovich J, Spence-Almaguer E, Preble K. Do official hospitalizations predict medical vulnerability among the homeless?: a postdictive validity study of the vulnerability index. J Health Care Poor Underserved. 2013. May;24(2):469–86. 10.1353/hpu.2013.0083 [DOI] [PubMed] [Google Scholar]
- 22.Fessler P Ending homelessness: a model that just might work. Washington, DC: National Public Radio (NPR), 2011. Available at: https://www.npr.org/2011/03/07/134002013/ending-homelessness-a-model-that-just-might-work. [Google Scholar]
- 23.Clarity Human Services. 9 reasons why the VI-SPDAT is the standardized assessment tool of choice. Las Vegas, NV: Clarity Human Services, 2016. Available at: http://info.clarityhumanservices.com/blog/vi-spdat-standardized-assessment. [Google Scholar]
- 24.Office of Policy Development and Research. Summary report assessment tools for allocating homelessness assistance: state of the evidence. Washington DC: The U.S. Department of Housing and Urban Development, 2015. Available at: https://www.huduser.gov/portal//publications/pdf/assessment_tools_Convening_Report2015.pdf. [Google Scholar]


