Abstract
Angiocentric glioma (AG) is a rare subtype of neuroepithelial tumor in children and young adults that commonly presents with seizures. To study the clinical characteristics, treatment and prognosis of patients with AG, the features of two cases of AG were described and 108 cases reported in the literature were assessed. The cases of the present study were two males aged 8 and 16 years, who mainly presented with seizures. MRI revealed superficial, non-enhanced lesions in the left temporal and right frontal lobe, respectively. The two patients underwent gross total resection (GTR) and remained seizure-free without neurological deficits after 3.5 and 2.5 years, respectively. Histopathological examination revealed that the tumors consisted of monomorphous cells that surrounded the blood vessels and neurons in the cerebral cortex, and formed concentric sleeves or pseudorosettes. Furthermore, immunostaining indicated that the diffuse infiltrative neoplastic cells were positive for glial fibrillary acidic protein and a dot-like pattern of epithelial membrane antigen was observed. AG mostly appeared similar to low-grade gliomas on MRI. GTR of the lesions was curative and radiation or chemotherapy were not required. AG typically has a favorable prognosis, with low mortality and incidence of disability.
Keywords: angiocentric glioma, neuroepithelial tumor, low-grade glioma, children/young adults, pseudorosettes
Introduction
Angiocentric glioma (AG) is a rare central nervous system (CNS) neoplasm that was first reported by Lellouch-Tubiana et al (1) and Wang et al (2) in 2005. AG was recognized as a distinct clinicopathologic entity by the World Health Organization (WHO) classification of CNS tumors in 2007 and was defined as ‘an epilepsy-associated, stable or slow-growing cerebral tumor primarily affecting children and young adults, histologically characterized by an angiocentric pattern of growth, monomorphous bipolar cells and features of ependymal differentiation (3,4). Since its initial description, an increasing number of cases of AG have been reported in the literature. In the 2016 WHO classification of CNS tumors (5), AG was considered as a WHO grade I tumor and was classified as ‘other gliomas’. The majority of studies on AG focus on the cytological features of the disease (6,7), while there is a lack of clinical and imaging data, as well as descriptions of the surgical treatment. The present study describes two patients with AG that received surgical treatment and provides a review of all previously reported cases to date.
Case study
Case 1
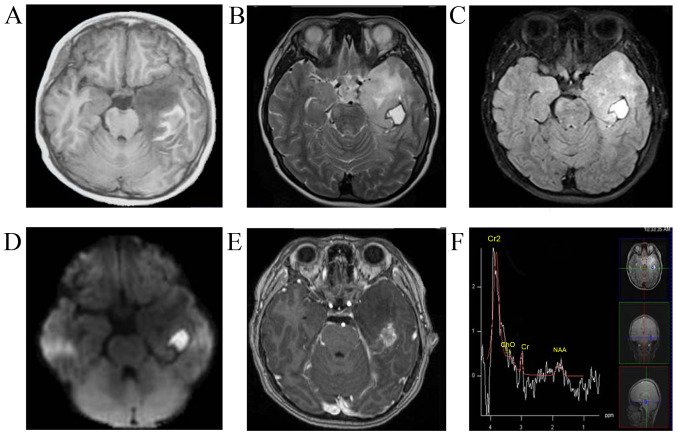
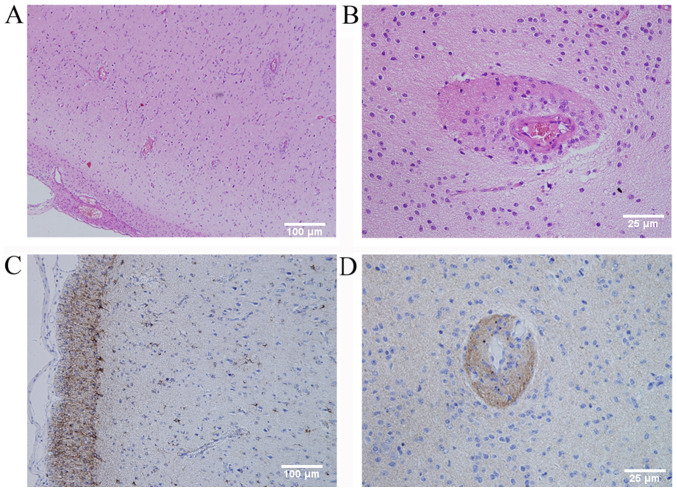
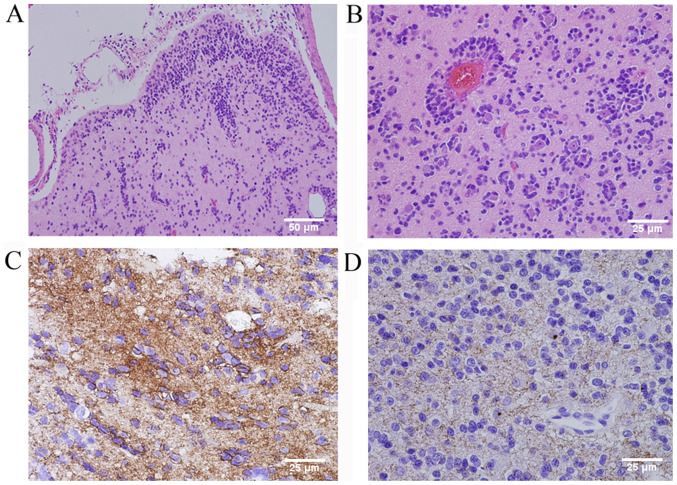
The first case was an 8-year-old male who presented with a 3-month history of seizures, headaches and vomiting. The patient was admitted to the Chinese PLA General Hospital (Beijing, China) in June 2016. MRI revealed a left temporal non-enhancing lesion [T1 hypointense, T2 hyperintense, diffusion-weighted imaging hyperintense, fluid-attenuated inversion recovery (FLAIR) hyperintense], measuring 2×2×1.5 cm, with a peripherally enhanced 1×1 mm cystic lesion and obvious brain edema around the lesion. The patient underwent magnetic resonance spectroscopy, which revealed a decrease in the N-acetylaspartate peak and no significant increase in the choline peak (Fig. 1). The patient was then subjected to a left craniotomy and underwent gross total resection (GTR). The tumor was located in the inferior temporal lobe and had a relatively clear boundary. Part of the tumor tissue was fish flesh-like in appearance and the patient had recurrent hemorrhage without vascular changes. Intra-operative frozen histological analysis suggested low-grade glioma. The final pathological assessment (Fig. 2) revealed that tumor cells surrounded the blood vessels and neurons in the cortex. The infiltrating tumor cells were glial fibrillary acidic protein (GFAP)-positive and epithelial membrane antigen (EMA) staining was observed in a distinct dot-like pattern in the cytoplasm. The Ki-67 proliferative rate was 5% and the cells were S-100- and neurospecific nucleoprotein (NeuN)-positive, and protein 53 (p53)-, synaptophysin (Syn)-, oligodendrocyte transcription factor-2 (Olig-2)- and creatine kinase (CK)-negative. According the 2016 WHO classification of CNS tumors (3,4), tumors with an angiocentric pattern of growth, GFAP-positive, NeuN- positive and low Ki-67 proliferative rate were diagnosed as AG (WHO grade I). At the 3.5-year follow-up, the patient continued to be seizure-free and did not exhibit any neurological deficits. Post-operative MRI also revealed no recurrence of the tumor.
Figure 1.
(Case 1) Axial brain MRI displaying a lesion in the left temporal lobe. (A) T1-weighted MRI hypointense. (B) T2-weighted MRI hyperintense. (C) Fluid-attenuated inversion recovery hyperintense with obvious brain edema around the lesion. (D) Diffuse weighted imaging hyperintense. (E) Contrast-enhanced T1-weighted MRI non-enhanced with an enhanced rim. (F) Magnetic resonance spectrum exhibiting a marked decrease in the NAA peak and no significant increase in the Cho peak. NAA, N-acetylaspartate; Cho, choline.
Figure 2.
(Case 1) (A and B) Histopathological examination revealed that tumor cells surrounded the blood vessels and neurons in the cortex (H&E staining; original magnification, ×100 in A and ×400 in B; scale bar, 100 µm in A and 25 µm in B). (C) Immunohistochemical staining demonstrated cytoplasmic immunoreactivity for GFAP (original magnification, ×100; scale bar, 100 µm) and (D) dot-like staining for EMA (original magnification, ×400; scale bar, 25 µm). GFAP, glial fibrillary acidic protein; EMA, epithelial membrane antigen; H&E, hematoxylin and eosin.
Case 2
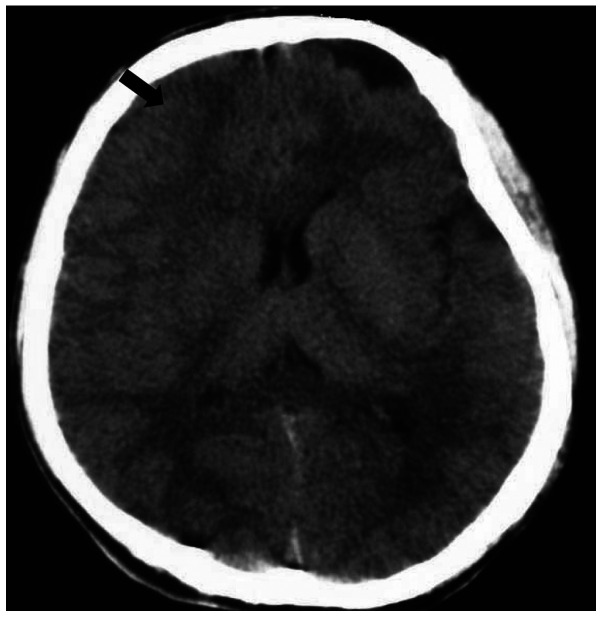
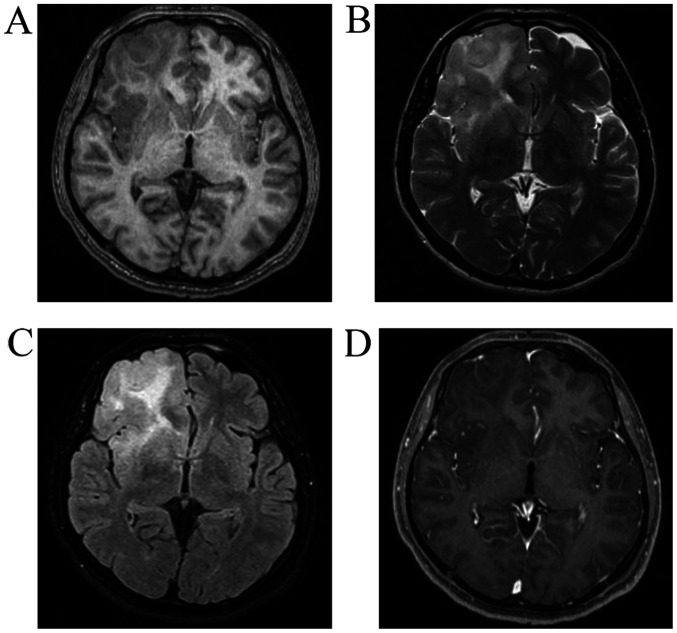
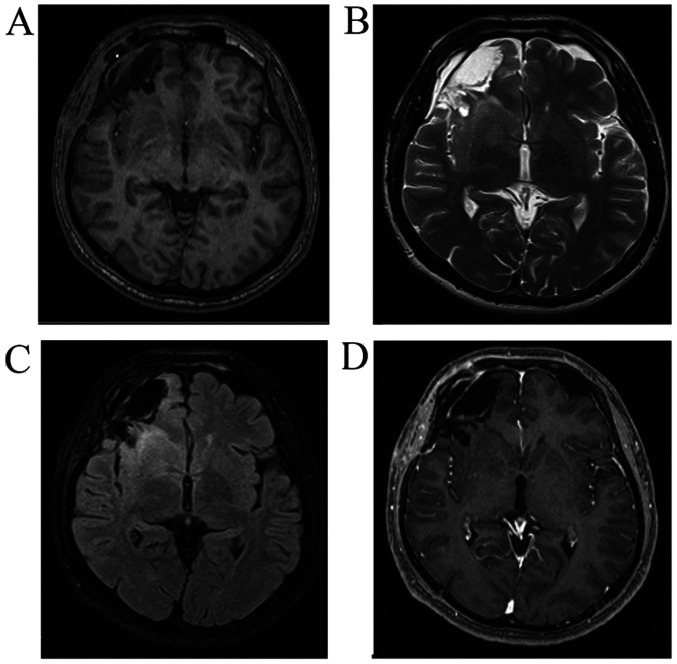
The second case was a 16-year-old male who presented with a 23-day history of recurrent seizures. The patient was admitted to the Chinese PLA General Hospital (Beijing, China) in July 2017. A CT scan revealed a round, circumscribed, hypodense lesion in the right frontal lobe (Fig. 3). MRI revealed a right frontal non-enhanced lesion (T1 hypointense, T2 and FLAIR slightly hyperintense; Fig. 4). Low-grade glioma was diagnosed at the initial stage. The patient then underwent right craniotomy. At the time of this initial surgery, the tumor was fish flesh-like in appearance and soft, had a rich blood supply and was not distinctly different from the surrounding brain tissue. Intra-operative frozen histological analysis also suggested low-grade glioma. The tumor was completely resected as tumor cells were not detected in the surgical margin based on the intra-operative histology. The final pathological assessment (Fig. 5) revealed infiltrating round or ovoid tumor cells in and under the subcortex that were partly arranged around blood vessels and neurons in concentric sleeves and pseudorosettes, demonstrating an angiocentric and creeping pattern. The tumor was dense with irregular cell nuclei and new blood vessels. No mitotic figures or necrotic cells were observed. The Ki-67 proliferative rate was 2%. The tumor was also immunoreactive for S100, vimentin, neurofilament and NeuN, but was negative for Olig-2, CD3, CD20, CD34 and CD68. These features supported the diagnosis of AG (WHO grade I). At the 2.5-year follow-up, the patient continued to be seizure-free and did not have any complications or neurological deficits. MRI at 5 months post-operatively (Fig. 6) revealed no recurrence of the tumor.
Figure 3.
(Case 2) Axial brain CT scan revealed a round, circumscribed, hypodense lesion in the right frontal lobe and an arachnoid cyst in the left frontal lobe (arrow).
Figure 4.
(Case 2) Axial brain MRI indicating a lesion in the right frontal lobe. (A) T1-weighted MRI hypointense; (B) T2-weighted MRI slight hyperintense. (C) Fluid-attenuated inversion recovery slight hyperintense with obvious brain edema around the lesion. (D) Contrast-enhanced T1-weighted MRI non-enhanced.
Figure 5.
(Case 2) Histopathological examination revealed infiltrative round or ovoid tumor cells in and under the cortex, and partly arranged around blood vessels and neurons in concentric sleeves and pseudorosettes and demonstrated an angiocentric and creeping pattern (H&E staining; original magnification, ×200 in A and ×400 in B; scale bar, 50 µm in A and 25 µm in B). (C) Immunohistochemical staining demonstrated strong cytoplasmic immunoreactivity for GFAP (original magnification, ×400; scale bar, 25 µm) and (D) dot-like staining for EMA (original magnification, ×400; scale bar, 25 µm). GFAP, glial fibrillary acidic protein; EMA, epithelial membrane antigen; H&E, hematoxylin and eosin.
Figure 6.
(Case 2) Axial brain MRI at 5 months post-operatively revealing no recurrence of the tumor in the right frontal lobe. (A) T1-weighted MRI. (B) T2-weighted MRI. (C) Fluid-attenuated inversion recovery. (D) Contrast-enhanced T1-weighted MRI.
Discussion
A literature review of studies on AG published in English or Chinese between January 2005 and December 2019 (Fig. 7), performed using Medline, PubMed and the China National Knowledge Infrastructure database, revealed that a total of 108 cases, including the two cases of the present study, have been reported (Table SI) (1,2,6–54). Of the 108 patients with AG, 61 were male and 47 were female (male/female ratio, 1:0.77). The age at the time of admission ranged between 1.5 and 83 years (median age, 13 years) and the majority of the patients were children and young adults. A total of 90 patients (85.7%; 90/105) presented with a long history of several types of intractable seizures (symptoms in three cases were not described). Only 15 patients exhibited different symptoms. Of these 15 patients, eight had headaches, four of which had decreased vision (7,12,47), three experienced dizziness, one of which had otalgia (9,19,49), two had ataxia (11,47), two had swallowing disorders (34,37), two presented with weakness and numbness of the left side of the body (17,45) and one had strabismus (34). The majority of the AG tumors (94.4%; 102/108) were in a supratentorial location situated within/under the cerebral cortex and 81.5% (88/108) were located in a single lobe. A total of six tumors were located in the brainstem (11,34,37,47). In a total of 46 cases, the tumor was in the left brain and in 43 cases, it was in the right brain. As AG arises in a superficial location in the cerebrum, which is typically completely removed, the literature indicated that gross total resection (GTR) of this lesion is curative. A total of 64.9% (61/94) of the patients with AG underwent GTR and 27.7% (26/94) underwent subtotal resection (STR). Furthermore, 7 cases only had a biopsy (7,34,37,47). The follow-up time ranged between 0.25 and 168 months (mean, 23.5 months). Of the patients with resection, 93.1% (81/87) were free of seizures during the follow-up time and the 6 patients with seizure recurrence had all undergone STR. A total of 10 patients received adjuvant therapy including radiation or chemotherapy, of which six received STR and four had a biopsy as the lesions were located in the brainstem (6,14,34,37). Histopathological evaluation revealed that the tumors were WHO grade I, with one exception, which was WHO grade III–IV (17).
Figure 7.
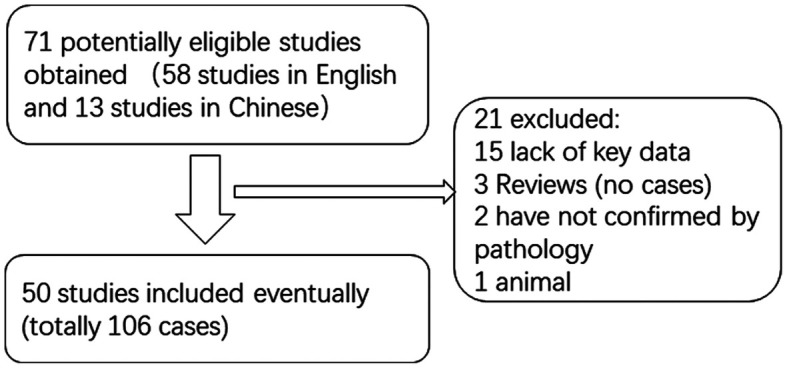
Flowchart of the selection and identification process of the cases included in the present study. After careful screening, 50 studies that included 106 cases were evaluated.
The present case study reported on two patients that were surgically treated at the Chinese PLA General Hospital (Beijing, China). The cases were similar to the ones reported in the literature, regardless of age, symptoms, tumor location and prognosis. The 8- and 16-year-old patients of the present study presented with intractable seizures and the 16-year-old patient also presented with headaches and vomiting. In the two patients, the tumor was located in the superficial cerebrum, in the left temporal lobe and in the right frontal lobe, respectively. The two patients underwent GTR. During the follow-up period of 42 and 30 months, the patients were seizure-free and did not experience any tumor recurrence.
Only a few studies have reported on the appearance of AG on CT scan (17,19). Hu et al (19) reported one case of AG that exhibited a hyperdense lesion on CT scan, which may be linked to hemorrhage and hemosiderin deposition. The 16-year-old patient in our cases showed a hypodense lesion on CT scan. The majority of AGs are similar to low-grade gliomas on MRI, i.e., hypointensity on T1-weighted imaging, hyperintensity on T2-weighted imaging, hyperintensity on FLAIR and non-enhanced on the contrast. AG tumors have a well-delineated boundary but may grow diffusely without an obvious edge. Previous studies reported that AG had a cortical rim of hypointensity on T1 and T2 around the lesion, which may be related to long-term compression by the slow-growing low-grade AG (1,14,19). The two patients in the present study also revealed similar characteristics to low-grade glioma, and a rim around the lesion was seen in the second patient.
As there is a lack of specific clinical manifestations and radiological features for AG, diagnosis still depends primarily on histopathological examination. Monomorphic, diffusely infiltrating bipolar spindled cells are commonly arranged around cortical blood vessels or neurons in concentric sleeves and pseudorosettes, which was the typical angiocentric gliomas pattern (15). Immunohistochemical staining results are generally positive for GFAP, S-100 and vimentin, and EMA has a dot-like pattern (8). Based on these findings, the main entities that were considered in the differential diagnosis were ependymoma and AG (6). The neuronal markers NeuN, Syn and chromogranin A (CgA) were usually negative. The Ki-67 proliferative index was ~1% and not >5%. This tumor type is also similar to other benign brain tumor types, including focal cortical dysplasia, ganglioglioma and certain neuroepithelial neoplasms, including pilomyxoid astrocytoma and supratentorial cortical ependymoma. Differences between AG and various easily misdiagnosed brain tumors are presented in Table I (5,55–61).
Table I.
Differential diagnosis between AG and other types of brain tumor.
| Tumor type | Predilection age | Symptoms | Tumor location | Radiological features | Histopathological examination | Immunoreactive factors | WHO grades | (Refs.) |
|---|---|---|---|---|---|---|---|---|
| AG | Children and young adults | Epilepsy | Frontal and temporal lobe | Similar to low-grade glioma, non-enhanced on the contrast MRI, small mass | Angiocentric pattern of growth, monomorphous bipolar cells | GFAP, S-100, vimentin, EMA | I | (5,55) |
| Focal cortical dysplasia | Early childhood | Intractable epilepsy | Frontal lobe | Normal or increased cortical thickness, subtle changes in the smoothness of gyri or sulci, not enhanced with gadolinium | Heterotopic neurons in white matter, hypertrophic neurons and abnormal dendrites | None | None | (58) |
| Gangliogliom | Children and young adults | Chronic seizures and iICP | Temporal lobe and cerebellum | Nodular, cystic, rim-like or entirely solid, enhanced on contrast MRI | Mixed population of ganglion and glial cells | GFAP, NeuN, NF | I | (59) |
| Pilomyxoid astrocytoma | Children | Focal neurological deficits and iICP | Suprasellar-hypothalamic region and cerebellum | Bordered lesion with heterogeneous contrast enhancement | Prominent mucoid matrix and angiocentric arrange ment of monomorphous, bipolar tumor cells | GFAP, S-100, NSE, Olig2 | II | (60) |
| Supratentorial cortical ependymoma | Adults | Epilepsy and focal neurological deficits | Frontal and parietal lobe | Solid or mixed solid/cystic appearance, enhanced in a heterogeneous pattern on the contrast MRI, mostly larger than 4 cm | Perivascular pseudorosettes and to a lesser extent in true ependymal rosettes | MIB-1, L1 and Ki-67 | II–III | (56) |
| Astroblastoma | Children and young adults, female | Seizures, focal neurologic deficits and iICP | Occipital and frontal lobe | Large, well-demarcated, lobulated mass, solid and cystic components with a characteristic bubbly appearance, with inhomogeneous contract enhancement | Perivascular pseudorosettes and prominent perivascular hyalinization | GFAP, vimentin | Not established | (57) |
| Diffuse gliomas | Adults and elderly individuals | Seizures, focal neurologic deficits cognitive, dysfunction and iICP | Cerebral hemisphere | Non-enhanced in diffuse low-grade gliomas, garlanded enhancement with a heterogeneous pattern and cystic appearance in high-grade gliomas on contrast MRI | Diffusely infiltrating, necrosis, cell nucleus dissociation and hemorrhage | GFAP, S-100, Olig2, EMA, nestin and high Ki-67 | II–IV | (5,61) |
Characteristics listed above are for the majority. Diffuse gliomas mainly include oligodendroglioma, astrocytoma, anaplastic glioma and glioblastoma. iICP, increased intracranial pressure; AG, angiocentric glioma; WHO, World Health Organization; GFAP, glial fibrillary acidic protein; EMA, epithelial membrane antigen; NF, neurofilament; NeuN, neurospecific nucleoprotein; NSE, neurospecific enolase; Olig2, oligodendrocyte transcription factor-2; MIB-1, mind bomb enzyme 3 ubiquitin protein ligase 1; L1, ligand 1.
While AG has been established as a distinct tumor type, its cytogenesis remains elusive. Wang et al (2) posited that AG arises from ependymoma and astroblastoma. Lellouch-Tubiana et al (1) suggested that AG has radial glia or neuronal origin. Bandopadhayay et al (62) and Qaddoumi et al (63) observed that an myeloblastosis quaking (MYB-QKI) gene rearrangement occurred in the majority of tumors, which contributed to the tumorigenesis, and this rearrangement was specific to angiocentric gliomas. Therefore, MYB-QKI gene fusion may be a defining genetic alteration typical for AG. While mutations of isocitrate dehydrogenase-1 most commonly result in the replacement of arginine at position 132 by histidine (R132H) in WHO grade II and III diffuse gliomas and secondary glioblastomas, this was not identified in AG (20,34,43). Therefore, this may facilitate the differential diagnosis of AG from tumors with a higher potential for recurrence.
AG is a slow-growing, stable tumor and lesions in the cerebral cortex are generally benign and may be cured by surgical excision alone. Adjuvant therapy, including chemotherapy or radiation, are not typically required (45). However, angiocentric gliomas arising in structures that are not amenable to surgical resection, including the brainstem, may require stereotactic biopsies and adjuvant therapy (37). Seizure control was dependent on the degree of tumor resection. According to the present review, AG is associated with a more favorable prognosis, with low mortality and incidence of disability. In two cases of tumor recurrence (2,42), the histopathological evaluation revealed a malignant neoplasm (WHO grade III) that was ultimately fatal.
AG is a recently described rare tumor of the CNS and exhibits radiological features on MRI that usually resemble those of diffuse low-grade glioma. AG tends to be non-malignant and curable and typically has a favorable prognosis. However, certain tumors may undergo malignant transformation. Longer follow-up periods are required to accurately establish the time to recurrence, to determine whether additional treatment is required and to establish the overall survival time.
Supplementary Material
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study were included in this published article.
Authors' contributions
GQH, JSZ and YM conceived the present study. GQH performed the data analysis. QPG and SY provided and analyzed the imaging and pathological data. GQH performed software analysis of the data and figures. YM supervised the research. GQH and JSZ drafted and reviewed the initial manuscript, and performed the literature review. YM edited the manuscript. All authors read and approved the manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Written informed consent for publication was provided by the patients' guardians as the patients were both under the age of 18.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Lellouch-Tubiana A, Boddaert N, Bourgeois M, Fohlen M, Jouvet A, Delalande O, Seidenwurm D, Brunelle F, Sainte-Rose C. Angiocentric neuroepithelial tumor (ANET): A new epilepsy-related clinicopathological entity with distinctive MRI. Brain Pathol. 2005;15:281–286. doi: 10.1111/j.1750-3639.2005.tb00112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang M, Tihan T, Rojiani AM, Bodhireddy SR, Prayson RA, Iacuone JJ, Alles AJ, Donahue DJ, Hessler RB, Kim JH, et al. Monomorphous angiocentric glioma: A distinctive epileptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol. 2005;64:875–881. doi: 10.1097/01.jnen.0000182981.02355.10. [DOI] [PubMed] [Google Scholar]
- 3.Brat DJ, Scheithauer BW, Fuller GN, Tihan T. Newly codified glial neoplasms of the 2007 WHO classification of tumours of the central nervous system: Angiocentric glioma, pilomyxoid astrocytoma and pituicytoma. Brain Pathol. 2007;17:319–324. doi: 10.1111/j.1750-3639.2007.00082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW. The 2016 world health organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016;131:803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 6.Mott RT, Ellis TL, Geisinger KR. Angiocentric glioma: A case report and review of the literature. Diagn Cytopathol. 2010;38:452–456. doi: 10.1002/dc.21253. [DOI] [PubMed] [Google Scholar]
- 7.Marburger T, Prayson R. Angiocentric glioma: A clinicopathologic review of 5 tumors with identification of associated cortical dysplasia. Arch Pathol Lab Med. 2011;135:1037–1041. doi: 10.5858/2010-0668-OAR. [DOI] [PubMed] [Google Scholar]
- 8.Alexandru D, Haghighi B, Muhonen MG. The treatment of angiocentric glioma: Case report and literature review. Perm J. 2013;17:e100–e102. doi: 10.7812/TPP/12-060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rho GJ, Kim H, Kim HI, Ju MJ. A case of angiocentric glioma with unusual clinical and radiological features. J Korean Neurosurg Soc. 2011;49:367–369. doi: 10.3340/jkns.2011.49.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fulton SP, Clarke DF, Wheless JW, Ellison DW, Ogg R, Boop FA. Angiocentric glioma-induced seizures in a 2-year-old child. J Child Neurol. 2009;24:852–856. doi: 10.1177/0883073808331078. [DOI] [PubMed] [Google Scholar]
- 11.Covington DB, Rosenblum MK, Brathwaite CD, Sandberg DI. Angiocentric glioma-like tumor of the midbrain. Pediatr Neurosurg. 2009;45:429–433. doi: 10.1159/000277616. [DOI] [PubMed] [Google Scholar]
- 12.Shakur SF, McGirt MJ, Johnson MW, Burger PC, Ahn E, Carson BS, Jallo GI. Angiocentric glioma: A case series. J Neurosurg Pediatr. 2009;3:197–202. doi: 10.3171/2008.11.PEDS0858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sugita Y, Ono T, Ohshima K, Niino D, Ito M, Toda K, Baba H. Brain surface spindle cell glioma in a patient with medically intractable partial epilepsy: A variant of monomorphous angiocentric glioma? Neuropathology. 2008;28:516–520. doi: 10.1111/j.1440-1789.2007.00849.x. [DOI] [PubMed] [Google Scholar]
- 14.Preusser M, Hoischen A, Novak K, Czech T, Prayer D, Hainfellner JA, Baumgartner C, Woermann FG, Tuxhorn IE, Pannek HW, et al. Angiocentric glioma: Report of clinico-pathologic and genetic findings in 8 cases. Am J Surg Pathol. 2007;31:1709–1718. doi: 10.1097/PAS.0b013e31804a7ebb. [DOI] [PubMed] [Google Scholar]
- 15.Buccoliero AM, Castiglione F, Degl'innocenti DR, Moncini D, Spacca B, Giordano F, Genitori L, Taddei GL. Angiocentric glioma: Clinical, morphological, immunohistochemical and molecular features in three pediatric cases. Clin Neuropathol. 2013;32:107–113. doi: 10.5414/NP300500. [DOI] [PubMed] [Google Scholar]
- 16.Arsene D, Ardeleanu C, Ogrezeanu I, Danaila L. Angiocentric glioma: Presentation of two cases with dissimilar histology. Clin Neuropathol. 2008;27:391–395. doi: 10.5414/NPP27391. [DOI] [PubMed] [Google Scholar]
- 17.Aguilar HN, Hung RW, Mehta V, Kotylak T. Imaging characteristics of an unusual, high-grade angiocentric glioma: A case report and review of the literature. J Radiol Case Rep. 2012;6:1–10. doi: 10.3941/jrcr.v6i10.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qi X, Duan Z, Yao K, Liu C. Clinicopathological features of angiocentric glioma: A report of two cases. J Diag Pathol. 2012:266–269. [Google Scholar]
- 19.Hu XW, Zhang YH, Wang JJ, Jiang XF, Liu JM, Yang PF. Angiocentric glioma with rich blood supply. J Clin Neurosci. 2010;17:917–918. doi: 10.1016/j.jocn.2009.10.024. [DOI] [PubMed] [Google Scholar]
- 20.Wu JT, Wang L, Chen GQ, Jin YJ. Angiocentric glioma with refractory epelepsy in children. Chin J Stereotact Funct Neurosurg. 2012;25:109–114. [Google Scholar]
- 21.Sun FH, Piao YS, Wang W, Chen L, Wei LF, Yang H, Lu DH. Brain tumors in patients with intractable epilepsy: A clinicopathologic study of 35 cases. Zhonghua Bing Li Xue Za Zhi. 2009;38:153–157. (In Chinese) [PubMed] [Google Scholar]
- 22.Ma XM, Liu HM, Li YL, He J, WANG LZ, Xu Y, Chen B. Hippocampus glioma with temporal lobe epilepsy as the main manifestation: The clinicopathologic properties. Acad J Second Mil Med Univ. 2010;31:60–62. doi: 10.3724/SP.J.1008.2010.00060. [DOI] [Google Scholar]
- 23.Li JY, Langford LA, Adesina A, Bodhireddy SR, Wang M, Fuller GN. The high mitotic count detected by phospho-histone H3 immunostain does not alter the benign behavior of angiocentric glioma. Brain Tumor Pathol. 2012;29:68–72. doi: 10.1007/s10014-011-0062-0. [DOI] [PubMed] [Google Scholar]
- 24.Raghunathan A, Olar A, Vogel H, Parker JR, Coventry SC, Debski R, Albarracin CT, Aldape KD, Cahill DP, III, Powell SZ, Fuller GN. Isocitrate dehydrogenase 1 R132H mutation is not detected in angiocentric glioma. Ann Diagn Pathol. 2012;16:255–259. doi: 10.1016/j.anndiagpath.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Miyahara H, Toyoshima Y, Natsumeda M, Uzuka T, Aoki H, Nakayama Y, Okamoto K, Fujii Y, Kakita A, Takahashi H. Anaplastic astrocytoma with angiocentric ependymal differentiation. Neuropathology. 2011;31:292–298. doi: 10.1111/j.1440-1789.2010.01161.x. [DOI] [PubMed] [Google Scholar]
- 26.Takada S, Iwasaki M, Suzuki H, Nakasato N, Kumabe T, Tominaga T. Angiocentric glioma and surrounding cortical dysplasia manifesting as intractable frontal lobe epilepsy-case report. Neurol Med Chir (Tokyo) 2011;51:522–526. doi: 10.2176/nmc.51.522. [DOI] [PubMed] [Google Scholar]
- 27.Pokharel S, Parker JR, Parker JC, Jr, Coventry S, Stevenson CB, Moeller KK. Angiocentric glioma with high proliferative index: Case report and review of the literature. Ann Clin Lab Sci. 2011;41:257–261. [PubMed] [Google Scholar]
- 28.Rosenzweig I, Bodi I, Selway RP, Crook WS, Moriarty J, Elwes RD. Paroxysmal ictal phonemes in a patient with angiocentric glioma. J Neuropsychiatry Clin Neurosci. 2010;22:123.E18–E20. doi: 10.1176/jnp.2010.22.1.123.e18. [DOI] [PubMed] [Google Scholar]
- 29.Koral K, Koral KM, Sklar F. Angiocentric glioma in a 4-year-old boy: Imaging characteristics and review of the literature. Clin Imaging. 2012;36:61–64. doi: 10.1016/j.clinimag.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 30.Miyata H, Ryufuku M, Kubota Y, Ochiai T, Niimura K, Hori T. Adult-onset angiocentric glioma of epithelioid cell-predominant type of the mesial temporal lobe suggestive of a rare but distinct clinicopathological subset within a spectrum of angiocentric cortical ependymal tumors. Neuropathology. 2012;32:479–491. doi: 10.1111/j.1440-1789.2011.01278.x. [DOI] [PubMed] [Google Scholar]
- 31.Varikatt W, Dexter M, Mahajan H, Murali R, Ng T. Usefulness of smears in intra-operative diagnosis of newly described entities of CNS. Neuropathology. 2009;29:641–648. doi: 10.1111/j.1440-1789.2009.01038.x. [DOI] [PubMed] [Google Scholar]
- 32.Adamek D, Siwek GP, Chrobak AA, Herman-Sucharska I, Kwiatkowski S, Morga R, Radwańska E, Urbanowicz B. Angiocentric glioma from a perspective of A-B-C classification of epilepsy associated tumors. Folia Neuropathol. 2016;54:40–49. doi: 10.5114/fn.2016.58914. [DOI] [PubMed] [Google Scholar]
- 33.Ampie L, Choy W, DiDomenico JD, Lamano JB, Williams CK, Kesavabhotla K, Mao Q, Bloch O. Clinical attributes and surgical outcomes of angiocentric gliomas. J Clin Neurosci. 2016;28:117–122. doi: 10.1016/j.jocn.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 34.Chan E, Bollen AW, Sirohi D, Van Ziffle J, Grenert JP, Kline CN, Tihan T, Perry A, Gupta N, Solomon DA. Angiocentric glioma with MYB-QKI fusion located in the brainstem, rather than cerebral cortex. Acta Neuropathol. 2017;134:671–673. doi: 10.1007/s00401-017-1759-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chatterjee D, Gupta K, Singla N, Radotra BD. Angiocentric glioma of hippocampus-report of a rare intractable epilepsy-related tumor. Neurol India. 2016;64:340–343. doi: 10.4103/0028-3886.177627. [DOI] [PubMed] [Google Scholar]
- 36.Cheng S, Lü Y, Xu S, Liu Q, Lee P. Cystoid angiocentric glioma: A case report and literature review. J Radiol Case Rep. 2015;9:1–9. doi: 10.3941/jrcr.v9i7.2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.D'Aronco L, Rouleau C, Gayden T, Crevier L, Décarie JC, Perreault S, Jabado N, Bandopadhayay P, Ligon KL, Ellezam B. Brainstem angiocentric gliomas with MYB-QKI rearrangements. Acta Neuropathol. 2017;134:667–669. doi: 10.1007/s00401-017-1763-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ersen A, Canda MS, Men S, Yucesoy K, Kalemci O, Canda T. Angiocentric glioma: The infiltrative glioma with ependymal differentiation. Turk Patoloji Derg. 2017;33:251–255. doi: 10.5146/tjpath.2014.01262. [DOI] [PubMed] [Google Scholar]
- 39.Grajkowska W, Matyja E, Daszkiewicz P, Roszkowski M, Peregud-Pogorzelski J, Jurkiewicz E. Angiocentric glioma: A rare intractable epilepsy-related tumour in children. Folia Neuropathol. 2014;52:253–259. doi: 10.5114/fn.2014.45566. [DOI] [PubMed] [Google Scholar]
- 40.Kakkar A, Sharma MC, Suri V, Kaushal S, Chandra SP, Garg A, Sarkar C. Angiocentric glioma: A treatable cause of epilepsy: Report of a rare case. Neurol India. 2014;62:677–679. doi: 10.4103/0028-3886.149405. [DOI] [PubMed] [Google Scholar]
- 41.Keser H, Barnes M, Moes G, Lee HS, Tihan T. Well-differentiated pediatric glial neoplasms with features of oligodendroglioma, angiocentric glioma and dysembryoplastic neuroepithelial tumors: A morphological diagnostic challenge. Turk Patoloji Derg. 2014;30:23–29. doi: 10.5146/tjpath.2013.01204. [DOI] [PubMed] [Google Scholar]
- 42.McCracken JA, Gonzales MF, Phal PM, Drummond KJ. Angiocentric glioma transformed into anaplastic ependymoma: Review of the evidence for malignant potential. J Clin Neurosci. 2016;34:47–52. doi: 10.1016/j.jocn.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 43.Ni HC, Chen SY, Chen L, Lu DH, Fu YJ, Piao YS. Angiocentric glioma: A report of nine new cases, including four with atypical histological features. Neuropathol Appl Neurobiol. 2015;41:333–346. doi: 10.1111/nan.12158. [DOI] [PubMed] [Google Scholar]
- 44.Sajjad J, Kaliaperumal C, Bermingham N, Marks C, Keohane C. ‘Unusual brain stone’: Heavily calcified primary neoplasm with some features suggestive of angiocentric glioma. J Neurosurg. 2015;123:1256–1260. doi: 10.3171/2014.11.JNS131158. [DOI] [PubMed] [Google Scholar]
- 45.Gonzalez-Quarante LH, Fernández Carballal C, Agarwal V, Vargas Lopez AJ, Gil de Sagredo Del Corral OL, Sola Vendrell E. Angiocentric glioma in an elderly patient: Case report and review of the literature. World Neurosurg. 2017;97:755.e5–e755.e10. doi: 10.1016/j.wneu.2016.10.034. [DOI] [PubMed] [Google Scholar]
- 46.Tauziède-Espariat A, Fohlen M, Ferrand-Sorbets S, Polivka M. A unusual brain cortical tumor: Angiocentric glioma. Ann Pathol. 2015;35:154–158. doi: 10.1016/j.annpat.2015.01.006. (In French) [DOI] [PubMed] [Google Scholar]
- 47.Weaver KJ, Crawford LM, Bennett JA, Rivera-Zengotita ML, Pincus DW. Brainstem angiocentric glioma: Report of 2 cases. J Neurosurg Pediatr. 2017;20:347–351. doi: 10.3171/2017.5.PEDS16402. [DOI] [PubMed] [Google Scholar]
- 48.Whitehead MT, Vezina G. MR spectroscopic profile of an angiocentric glioma. Anticancer Res. 2015;35:6267–6270. [PubMed] [Google Scholar]
- 49.Wu CX, Zheng D, Yao K, Liu N. Clinical, imaging and pathological findings of angiocentric gliomas: An analysis of 8 cases. Clin J Neuromed. 2015;9:869–873. [Google Scholar]
- 50.Feng LJ, Wen ZB, Wang XL, Yu Y, Jiang SS. Intracranial angiocentric glioma: Case report. Chin J Med Imaging Technol. 2015;4:522–524. [Google Scholar]
- 51.Li YY, Lan YQ, Chen YM. A case of angiocentric glioma. Chin J Magn Reson Imaging. 2017;3:230–232. [Google Scholar]
- 52.Liang Y, Di HJ, Fu J, Leng H. A case of angiocentric glioma. J Cliff Exp Pathol. 2016;7:831–832. [Google Scholar]
- 53.Liu F, Zhang LY, Guo L, Hu WW, Li Z. Angiocentric glioma: A case report and review of the literature. J Clin Exp Pathol. 2016;10:1174–1177. [Google Scholar]
- 54.Xu WJ, Zheng ZY, Liu W. Insular angiocentric glioma: Report of 1 case. J Clin Exp Pathol. 2015;6:717–719. [Google Scholar]
- 55.Wen PY, Huse JT. 2016 World health organization classification of central nervous system tumors. Continuum (Minneap Minn) 2017;23:1531–1547. doi: 10.1212/CON.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 56.Mohaghegh MR, Chitsaz A, Okhovat AA, Pour EB. Supratentorial cortical ependymoma: An unusual presentation of a rare tumor. Adv Biomed Res. 2015;4:72. doi: 10.4103/2277-9175.153896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hammas N, Senhaji N, Alaoui Lamrani MY, Bennis S, Chaoui EM, El Fatemi H, Chbani L. Astroblastoma-a rare and challenging tumor: A case report and review of the literature. J Med Case Rep. 2018;12:102. doi: 10.1186/s13256-018-1623-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Crino PB. Focal cortical dysplasia. Semin Neurol. 2015;35:201–208. doi: 10.1055/s-0035-1552617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kubicky CD, Sahgal A, Chang EL, Lo SS. Rare primary central nervous system tumors. Rare Tumors. 2014;6:5449. doi: 10.4081/rt.2014.5449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ma X, Wang Y, Liu H, Yu H, He J. Pilomyxoid astrocytomas with rare rosenthal fibers. Brain Tumor Pathol. 2016;33:35–39. doi: 10.1007/s10014-015-0244-2. [DOI] [PubMed] [Google Scholar]
- 61.Esparragosa I, Diez-Valle R, Tejada S, Gállego Pérez-Larraya J. Management of diffuse glioma. Presse Med. 2018;47:e199–e212. doi: 10.1016/j.lpm.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 62.Bandopadhayay P, Ramkissoon LA, Jain P, Bergthold G, Wala J, Zeid R, Schumacher SE, Urbanski L, O'Rourke R, Gibson WJ, et al. MYB-QKI rearrangements in angiocentric glioma drive tumorigenicity through a tripartite mechanism. Nat Genet. 2016;48:273–282. doi: 10.1038/ng.3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Qaddoumi I, Orisme W, Wen J, Santiago T, Gupta K, Dalton JD, Tang B, Haupfear K, Punchihewa C, Easton J, et al. Genetic alterations in uncommon low-grade neuroepithelial tumors: BRAF, FGFR1, and MYB mutations occur at high frequency and align with morphology. Acta Neuropathol. 2016;131:833–845. doi: 10.1007/s00401-016-1539-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study were included in this published article.