Abstract
OBJECTIVE AND AIM:
Chronic obstructive pulmonary disease (COPD) is one of the most common chronic diseases. The patient's fear and anxiety of shortness of breath and coughing during exercise may lead to a decrease in patients' daily activities. Therefore, the present study aimed to determine the effect of empowerment program based on the social cognitive theory (SCT) on the daily activity of patients with COPD.
METHODS:
This quasi-experimental study was performed on 70 patients with COPD referred to Kashani and Hajar centers in 2019. Samples were randomly divided into two groups of experimental and control. Data collection tools included demographic information questionnaire and activity of daily living questionnaire, specific for COPD, and a researcher-made questionnaire for measuring SCT constructs. For the experimental group, the training program consisted of four theoretical and practical sessions of 40 min/week. The data were collected at three time points, before, immediately and 3 months after the training are 3 time. The data were analyzed by SPSS software using descriptive and inferential statistics.
RESULTS:
The difference between the mean scores of behavioral ability, self-efficacy, and empowerment in the three stages was significant only in the experimental group (P < 0.001). The mean daily activity score of patients before, immediately, and 3 months after intervention showed a statistically significant difference between the two groups (52.46 ± 21.98, 63.36 ± 21.95, and 71.34 ± 19.02), respectively, in the intervention group, and (51.79 ± 19.29, 53.70 ± 19.28, and 53.82 ± 19.26), respectively, in the control group (P < 0.001).
CONCLUSION:
The results of this study showed that empowerment of patients through interventions based on SCT can increase the daily activity of patients with COPD. Because nurses play an important role in patient education and improvement, it is hoped that the findings of this study will be used as a strategy to increase the daily activity and ultimately improve the quality of life in these patients.
Keywords: Activity of daily living, chronic obstructive pulmonary disease, social cognitive theory
Introduction
Chronic diseases are the leading cause of death worldwide. The rapid rise of these diseases represents major health challenges worldwide. Chronic diseases are the most common causes of death in the subgroup of no communicable diseases, such as heart disease, cancers, chronic lung disease, and diabetes.[1]
Chronic illness is a multidimensional experience where the patient has to adapt to different situations and individuals and keep up with the stresses and consequences of the disease.[2] Overall, chronic diseases are one of the major challenges of health-care systems.[3] Chronic obstructive pulmonary disease (COPD) is one of the most common chronic diseases that is progressive and is characterized by irreversible airway restriction and includes both chronic bronchitis and pulmonary emphysema.[4]
This disease is a common and debilitating condition and is recognized as the fourth leading cause of death in the world.[5] The prevalence of the disease in the adult population is 6%–10%[6,7] and about 300 million people are affected.[8] It is estimated that by 2020, the disease will become the fifth most debilitating disease after depression, accidents, and cerebrovascular diseases and rank fifth in terms of medical costs.[9] COPD is the fourth leading cause of death worldwide,[10,11,12] with 3 million people dying each year of the disease.[13,14,15] In the United States, COPD is the third leading cause of death with more than 12 million people.[15,16,17] On the other hand, according to the Iranian Census of 2008, 7 million out of the 70 million population of the country have respiratory diseases, which shows the prevalence of this disease in our society.[18,19] In this condition, dyspnea is usually progressive and worsens with exercise and activity.[20] As the disease progresses, patients' shortness of breath increases as they engage in the activities of daily living, thus causing patients to become anxious and anxious about the activity. Patients' fear and anxiety of shortness of breath and coughing during exercise lead to a decrease in patients' daily activities, resulting in the patient's regression in daily activities.[21] Patients are, therefore, restricted and isolated due to their lack of control over symptoms. Functional status disorder is a common condition in patients with COPD.[22] Today, we know that a set of individual, interpersonal, and environmental factors act as protective behaviors that influence people's participation in daily activities, and it can be argued that the key to effective interventions to promote regular physical activity can be cognition, better understanding, and proper use of psychological determinants of behavior.[23,24] In this regard, considering the most important factors known to be modifiable individual, interpersonal, and environmental factors that somehow influence physical activity and participation in physical activity, the application of social cognitive theory (SCT) as a theoretical framework for educational intervention seems reasonable.[25,26] The SCT was introduced by Bandura in 1963. This theory holds that behavioral change is due to the reciprocal interaction of individual, behavioral, and environmental factors, and the interaction of these three dimensions leads to behavior change.[27] In this theory, in addition to expressing predictive factors and principles influencing behavior formation, behavioral ability (knowledge and skill) constructs, outcome expectancy, outcome evaluation, self-efficacy, self-regulation, and reinforcement are the most important determinants and guides in design. Introducing educational interventions as a consequence of SCT, it is an interpersonal theory that assumes that behavior is carried out using individual factors (attitudes, beliefs, and self-efficacy), behavioral factors and environmental factors; environmental factors are factors that affect one's behavior, but is not physically part of the person. The social environment includes family members, friends, peers at school, and colleagues with some environmental factors.[27,28] Constructs of this theory are behavioral ability (knowledge and skill), expectation of outcome (predicting the likely outcomes of a behavior), outcome assessment (value that one places on the probable outcomes of a particular behavior), observational learning, the environment (family or physical or social conditions around the person), self-efficacy (one's confidence in the ability to follow one's behavior), and self-control (setting goals and creating plans for one's chosen behaviors).[29] The strongest and most powerful construct in changing one's behavior is self-efficacy,[30,31]
Another important construct of SCT that is used in educational interventions to promote physical activity of patients is empowerment.[32] Both knowledge and skill are essential to the performance of a behavior, that is to say, to perform a particular behavior, one must first know what that behavior is and then must know how to do and execute it. In other words, behavioral ability indicates that one must know and practice how to do it.[31,33] The concept of behavioral ability leads to a distinction between learning and capability, because a task may be learned but not implemented, if capability entails learning. Therefore, the main goal of educational interventions should be to develop behavioral abilities to implement a new type of behavior.[33] Because the selection of the training model is a first step in the educational planning process, the present study aimed to determine the impact of cognitive theory-based empowerment program, on the daily activities of patients with COPD.
Methods
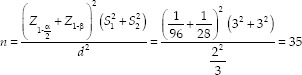
The present study was a two-group, quasi-experimental study conducted on 70 patients with COPD in educational hospitals of Shahrekord. The required sample size was determined based on the previous study,[18] with 95% confidence interval and error rate of 2.3 sample size in each group at least 35 and in the total study equal to 70 persons. Ten percent of the falls totaled 80 patients.
The research units were randomly divided into intervention and control groups using random allocation software. Inclusion criteria were complete consent of the study unit, age range of 45–75 years,[19] diagnosis of COPD by a specialist physician, Stage 2 disease based on GOLD classification, and literacy of the patient or the accompanying patient. The sample was excluded from the study if it did not agree to continue cooperating or exacerbate the symptoms of another patient. This study was approved by the Ethics Committee of Shahrekord University of Medical Sciences (IR.SKUMS.REC.1397.167). After the intervention, the educational content of the intervention group was provided to the control group. The data were collected using a demographic questionnaire, a daily activity assessment questionnaire in COPD, and a researcher-made questionnaire based on model constructs. The validity and reliability of the daily activity questionnaire was confirmed by Dr. Dalvandi, and the overall Cronbach's alpha coefficient was 0.93. Internal consistency and test–retest methods were also used to determine the reliability of the instrument, and based on the correlation test of the questionnaire, it has good reliability.[34] The researcher-made questionnaire is structured on the basis of behavioral ability, reinforcement, and self-efficacy constructs because they are more effective in changing behavior.[35] There were 17 four-question constructions of consciousness construct, 10 three-question constructs of skill, 11 five-question constructs of reinforcement, and 6 five-question constructs of self-efficacy. To determine face validity, the questionnaire was provided to several health education professionals to express their views on the difficulty of understanding the concepts, ambiguities, and misunderstandings of the questions. After the experts' comments on the items, the content validity of the questionnaire was calculated in two ways: content validity ratio (CVR) and content validity index (CVI). To determine the ratio of content validity (need for any question) experts will be consulted. CVR values above 0.56 were accepted based on the Lawshe table. Content validity index (CVI), clarity and simplicity of each question were assessed and the values above 0.79 were accepted.[36,37] After validation, the reliability of the pilot sample was calculated from four patients (this group was not included in the original study), which was α =0.81. After completing the researcher-made questionnaires in pretest by interview, the questionnaire was reviewed by the interviewer who had received the necessary training to complete the questionnaires. Moreover, nine faculty members arrived at the School of Nursing and Health. Training sessions for 5–6 participants in each session were held for 40 min in the experimental group using lecture, group discussion, question and answer, and PowerPoint in the hospital training classes [Table 1].[38,39,40] At the end of each training session, a pamphlet containing a regular and comprehensive set of all points stated during the session was given to patients in the control group. During this period, they received routine treatments and care; training in the experimental group provided the researcher with follow-up calls (every 15 days) with the aim of examining the treatments and care provided to them.[41] After 3 months, the questionnaires were again completed by the interviewer responsible for data collection and interviewing.[42] The training model was designed and approved by five nephrologists and ten faculty members of the Faculty of Nursing and Midwifery.
Table 1.
Educational sessions for patients with chronic obstructive pulmonary disease based on the social cognitive theory
| Educational session | Session topic | Factors | Educational strategy |
|---|---|---|---|
| First session | Explain the study purpose, increased awareness about disease, and the importance of physical activity | Awareness | Lecture, group discussion, and question and answer |
| Second session | Training on how to breathe properly, using sprays and oxygen and practicing | Skill | View - View and repeat the show by individual |
| Third session | Raising motivation and strengthening the patient’s emotional field for regular physical activity and daily activities | Self-ability | Lecture, group discussion, and question and answer |
| Fourth session | Training sessions with family caregivers of patients (training on how to care for patients) Understanding the associations and organs that help patients and how to get proper education in the disease | Reinforcing | Group discussion and brainstorming and group problem solving |
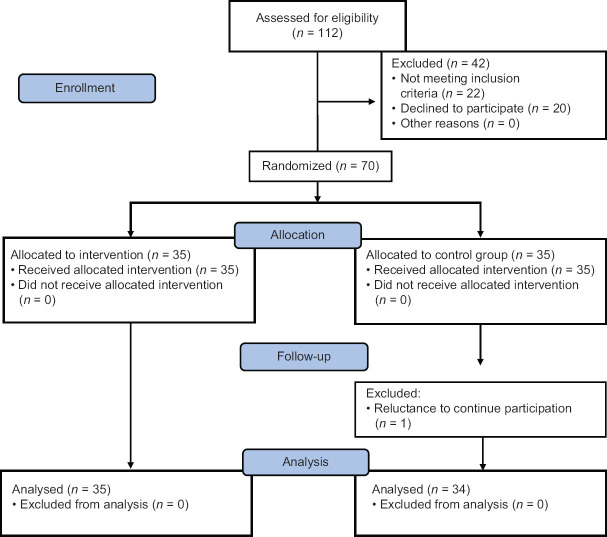
During the implementation of the progress program, it was evaluated in terms of achieving regular goals, which enabled the training program to continue according to learners' needs and in line with predetermined goals. According to the results of the questionnaires, low awareness of patients was considered as the most important problem. Increased levels of daily activity were identified as target behavior. Based on the targeting, the researcher decided to increase patient awareness first and then improve patient self-efficacy and skill and then to strengthen the patients' families by attending meetings and increasing their support for structural patients. During the follow-up period, patients were assessed for behavioral changes and daily activity levels were assessed immediately and 3 months after the intervention. Posttest questionnaires were completed by the researcher immediately and 3 months after the intervention for patient who remain in study [Figure 1] and the data were analyzed using SPSS software version 21 (SPSS Inc., Chicago, IL, USA) and descriptive tests (mean, standard deviation, frequency, and percentage) and analytical tests (t-test, Mann–Whitney, Chi-squared test, repeated measures analysis, and Friedman).
Figure 1.
Flow of patients through the trial
Results
The mean age of the patients was 43.51 ± 6. 21 years. According to independent t-test, there was no significant difference between the experimental and control groups in terms of age (P = 0.45).
Other demographic characteristics of patients are listed in Table 2.
Table 2.
Demographic characterization of participants
| Variable | Group | Intervention, n (%) | Control, n (%) |
|---|---|---|---|
| Sex | Male | 16 (47.1) | 18 (51.4) |
| Female | 18 (59.2) | 17 (48.6) | |
| Education level | Primary school | 11 (50) | 11 (45.8) |
| Less than high school | 2 (9.1) | 3 (12.5) | |
| Diploma | 6 (27.3) | 7 (29.9) | |
| University | 3 (13.6) | 3 (12.5) | |
| Smoking | No | 19 (79.2) | 23 (79.3) |
| Yes | 5 (20.7) | 6 (20.8) | |
| Job | At home | 12 (46.2) | 13 (41.2) |
| Employee | 6 (23.1) | 9 (26.5) | |
| Not employed | 6 (23.1) | 6 (17.6) | |
| Retired | 2 (7.7) | 7 (14.7) |
Based on the results of independent t-test and Chi-square test, the two intervention and control groups were matched for all demographic characteristics. There was no significant difference between the two groups (P > 0.05). The daily activity score of the two groups at the beginning of the intervention was not significantly different. In contrast, immediately and 3 months after the intervention, the daily activity score in the intervention group was significantly higher than the control group [Table 3].
Table 3.
Determination and comparison of the mean activity of daily living score before, immediately, and three months after intervention in the two groups
| Variable | Time | Mean±SD | P | |
|---|---|---|---|---|
| Intervention group | Control group | |||
| Activity of daily living | Before intervention | 52.46±21.98 | 51.79±19.29 | 0.314 |
| After intervention | 53.36±21.95 | 53.70±19.28 | <0.001 | |
| 3 months after intervention | 61.34±19.02 | 53.82±19.26 | <0.001 | |
SD=Standard deviation
According to Table 4, the results showed that there was no significant difference in the mean scores of knowledge, skill, reinforcement, and self-efficacy between the two groups before intervention. However, the difference in the assessment immediately after the test and the 3-month follow-up was based on the independent t-test (P < 0.05). The variance with repeated measures showed a significant difference in the process of mean score change in the three measurement stages (before the intervention, immediately after the intervention, and 3 months after the intervention) (P < 0.001).
Table 4.
Descriptive-analytic comparison of the mean scores of model constructs before and 1 and 3 months after intervention in the two study groups
| Variable | Time | Mean±SD | P | |
|---|---|---|---|---|
| Intervention group | Control group | |||
| Self-efficacy | Before intervention | 10.54±4.19 | 10.57±5.2 | 0.213 |
| After intervention | 10.54±4.19 | 10.57±5.2 | <0.001 | |
| 3 months after intervention | 12.34±4.02 | 10.62±5.2 | <0.001 | |
| Skill | Before intervention | 18.22±4.65 | 19.02±5.70 | 0.202 |
| After intervention | 18.22±4.65 | 19.02±5.70 | <0.001 | |
| 3 months after intervention | 20.05±4.44 | 19.11±5.61 | <0.001 | |
| Reinforcement | Before intervention | 20.77±6.89 | 19.22±7.45 | 0.103 |
| After intervention | 20.77±6.89 | 19.22±7.45 | <0.001 | |
| 3 months after intervention | 26.88±7.21 | 19.22±7.45 | <0.001 | |
SD=Standard deviation
Discussion
The purpose of this study was to investigate the effect of empowerment program based on SCT on the activities of daily living of patients with COPD. Bandura's SCT refers to people's beliefs about their ability to make decisions and act on the basis of their consequences and likely outcomes. This theory is based on the idea that humans learn about others' behaviors, rules, knowledge, skills and strategies, beliefs, and attitudes in the social environment of appropriate behaviors, in which much of our learning is based on modeling and observation.[26] According to the initial assessment of patients' knowledge, scores were at a low level, so according to the model constructs, the researcher tried to increase patients' awareness and subsequently improve patients' self-efficacy and skills, and then with families entering meetings and increasing support. They also increase the structural strength of patients in intervention group. The results of the study showed that designing and implementing a training program in accordance with the social cognitive model can make a significant difference in the self-efficacy, reinforcement factors, and skills of the patients in the experimental group. In the present study, after the intervention, the knowledge and skills of the experimental group increased compared to the control group. The first study showed that the knowledge score significantly increased in the experimental group after the intervention.[43] Shirvani et al. in their study found that the implementation of cognitive–social model training program on adolescent girls had a positive effect on promoting adolescent girls' physical activity.[44] These results are similar to the findings of the present study, because the same is true of physical activity. In other words, one cannot simply expect a steady increase in physical activity by increasing awareness.
According to the results of the study by Ghasemi et al. in 2017, “the effect of educational intervention based on socio cognitive theory on the prevention of cardiovascular risk factors” was carried out on students, their mothers, and their educators in Zanjan. The results showed that there was no significant difference between the two groups in the mean scores of social cognitive theory before intervention, but after intervention, the mean score of knowledge structures and perception of position and self-efficacy were significantly higher in the experimental group (P < 0.05).[45] The results of the study showed that there was no significant difference between the two groups regarding reinforcement construct before intervention, but immediately and 3 months after intervention this difference was significant in the experimental group. The findings of this study are in line with those of Gustafson and Rhodes, who examined the relationship between reinforcement structures and physical activity and confirmed its positive effect.[46]
However, the study by Peterson et al. aimed to examine the relationship between parental social support and physical activity in 1421 students is inconsistent with the present study, which stated that there is a reverse relationship between empowerment and physical activity.[47] Furthermore, in the study by Lubans and Sylva with SCT model, at the end of the intervention program, there was a significant difference between the amount of structural reinforcement and physical activity scores between the intervention and control groups.[48] Numerous studies have confirmed the association between perceived self-efficacy and behaviors related to health promotion.[49,50,51,52]
The last variable studied in this study was self-efficacy. In this construct, it was attempted to increase the level of confidence in increasing the level of daily activity in conditions that the patient had a correct understanding of the barriers to activity. Therefore, in the experimental group, by increasing the motivation and strengthening the patient's emotional domain to perform regular physical activity and daily activities, the results showed a significant change in the scores of this construct in the two groups before and 3 months after the intervention.
Consistent with this study, the results of a 2012 study by Ramirez et al. to improve physical activity in children showed that self-efficacy is a strong predictor of physical activity in children.[53] Studies by Mahdizadeh et al. have shown that self-efficacy is one of the important factors for physical activity. Thus, in people with high self-efficacy, the motivation to continue behavior over time, even with obstacles, is greater.[54]
The results of Rogers et al.'s study[32] showed that after intervention, perceived self-efficacy, empowerment, and skill of patients in the intervention group were significantly increased. The findings of the study by Reisi et al.[55] also indicated an increase in self-efficacy after the training program. This study is one of the few studies on daily activity improvement in COPD that was performed as a double-blind clinical trial with control and test groups. The main strength of this study is the use of SCT as a theoretical framework of research in a sense, it is an innovation. Furthermore, considering the positive results of this study in patients, this theory can be applied in the fields of education, research, and clinical practice for respiratory and other chronic patients.
Finally, interventions based on SCT and enhancing self-efficacy, skill, and social support for these patients can be an effective step in enhancing their daily activities of life. Because the educational constructs of this model influence behavior change and lead to healthy behaviors, this model can be used to design interventions to improve the quality of life of chronic patients, including respiratory patients. Due to the large number of constructs and the length of the questionnaires, four of the constructs that were more emphasized in the studies were selected by faculty members, which is one of the weaknesses of the current study. Furthermore, personal and social differences and physical problems of patients could have an impact on the results of the study.
Conclusion
Because studies have shown that symptoms of COPD (dyspnea) substantially decrease daily activity and jeopardize one's health, empowering these patients to tolerate activity and perform daily activity as much as possible is of particular importance. The findings of this study showed that SCT-based empowerment program had a positive impact on the daily activities of people with COPD. The program influenced patients' awareness, skill, empowerment, and self-efficacy in four domains, so that by increasing the sample's knowledge score, it could influence patients' motivation to learn. Furthermore, by training on how to breathe properly, spraying practically could have a positive effect on patients' skills and enhance self-efficacy by enhancing family presence and enhancing motivation and emotional well-being. Therefore, considering the positive effects of this program in promoting daily activity in chronic respiratory patients, it is suggested to use this program to promote the health of respiratory and chronic patients in the nursing and health community.
Financial support and sponsorship
This study was part of a MS thesis supported by Shahrekord University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article was part of a master thesis with the approval code IR.SKUMS.REC.1398.041 of the Ethics Committee of Shahrekord University of Medical Sciences. The authors would like to extend our gratitude to thank all participants who wholeheartedly participated in this research.
References
- 1.Mortazavi SG, Arian A, Tobi K, Haji M, Zardast M. Effect of atorvastatin on blood and gasometric indicators in patients with chronic obstructive pulmonary disease: A double-blind, clinical trial. J Birjand Univer Med Sci. 2016;23:334–41. [Google Scholar]
- 2.Mirbagher-Ajorpaz N, Rezaei M. The effect of pulmonary rehabilitation program on quality of life of elderly patients with chronic obstructive pulmonary disease. Zahedan J Res Med Sci. 2011;13:30–5. [Google Scholar]
- 3.Rafii F, Soleimani M, Seyedfatemi N. A model of patient participation with chronic disease in nursing care. Koomesh. 2011;12:293–304. [Google Scholar]
- 4.Lee YM. Chronic obstructive pulmonary disease: Respiratory review of 2014. Tuberc Respir Dis (Seoul) 2014;77:155–60. doi: 10.4046/trd.2014.77.4.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crighton EJ, Ragetlie R, Luo J, To T, Gershon A. A spatial analysis of COPD prevalence, incidence, mortality and health service use in Ontario. Health Rep. 2015;26:10–8. [PubMed] [Google Scholar]
- 6.Copd. 2016. [Last accessed on 2018 Dec 10]. Available from: http://www.uptodate.com/contents/chr onic-obstructive-pulmonary-disease .
- 7.Azargon A, Gholami M, Farhadi A, Hadi Chegni M, Zendedel A. Evaluation of the persian transcript of the COPD assessment test in the measurement of COPD health status in Iranian COPD patients. Glob J Health Sci. 2015;8:225–30. doi: 10.5539/gjhs.v8n5p225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stojkovikj J, Zafirova-Ivanovska B, Kaeva B, Anastasova S, Angelovska I, Jovanovski S, et al. The prevalence of diabetes mellitus in COPD patients with severe and very severe stage of the disease. Open Access Maced J Med Sci. 2016;4:253–8. doi: 10.3889/oamjms.2016.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 10.Varmaghani M, Farzadfar F, Sharifi F, Rashidian A, Moin M, Moradi-Lakeh M, et al. Prevalence of asthma, COPD, and chronic bronchitis in Iran: A systematic review and meta-analysis. Iran J Allergy Asthma Immunol. 2016;15:93–104. [PubMed] [Google Scholar]
- 11.Khoshkesht S, Zakerimoghadam M, Ghiyasvandian S, Kazemnejad A, Hashemian M. The effect of home-based pulmonary rehabilitation on self-efficacy in chronic obstructive pulmonary disease patients. J Pak Med Assoc. 2015;65:1041–6. [PubMed] [Google Scholar]
- 12.Diette GB, Dalal AA, D'Souza AO, Lunacsek OE, Nagar SP. Treatment patterns of chronic obstructive pulmonary disease in employed adults in the United States. Int J Chron Obstruct Pulmon Dis. 2015;10:415–22. doi: 10.2147/COPD.S75034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.KalagoudaMahishale V, Angadi N, Metgudmath V, Lolly M, Eti A, Khan S. The prevalence of chronic obstructive pulmonary disease and the determinants of underdiagnosis in women exposed to biomass fuel in India – A cross section study. Chonnam Med J. 2016;52:117–22. doi: 10.4068/cmj.2016.52.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pasquale MK, Sun SX, Song F, Hartnett HJ, Stemkowski SA. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–64. doi: 10.2147/COPD.S36997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kupryś-Lipińska I, Kuna P. Impact of chronic obstructive pulmonary disease (COPD) on patient's life and his family. Pneumonol Alergol Pol. 2014;82:82–95. doi: 10.5603/PiAP.2014.0014. [DOI] [PubMed] [Google Scholar]
- 16.Kraïm-Leleu M, Lesage FX, Drame M, Lebargy F, Deschamps F. Occupational Risk Factors for COPD: A Case-Control Study. PLoS One. 2016;11:e0158719. doi: 10.1371/journal.pone.0158719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hesso I, Gebara SN, Kayyali R. Impact of community pharmacists in COPD management: Inhalation technique and medication adherence. Respir Med. 2016;118:22–30. doi: 10.1016/j.rmed.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 18.Jokar Z, Mohammadi F, Khankeh H, Rabee Z, Tafti FS. Effect of home-based pulmonary rehabilitation on daily activity of patients with chronic obstructive pulmonary disease. Evid Based Care. 2014;4:69–76. [Google Scholar]
- 19.Abedi H, Salimi S, Feizi A, Vaghasloo SS. Assessment of relationship between self-efficacy and self-care in COPD patients. J Nurs Midwifery Urmia Univer Med Sci. 2012;10(1):68–74. [Google Scholar]
- 20.Brunner LS. Brunner and Suddarth's Textbook of Medical-Surgical Nursing. MacAlizer: Lippincott Williams and Wilkins; 2018. [Google Scholar]
- 21.Velloso M, Stella SG, Cendon S, Silva AC, Jardim JR. Metabolic and ventilator parameters of four activities of daily living accomplished with arms in COPD patients. Chest. 2003;123:1047–53. doi: 10.1378/chest.123.4.1047. [DOI] [PubMed] [Google Scholar]
- 22.Garrod R, Marshall J, Barley E, Fredericks S, Hagan G. The relationship between inflammatory markers and disability in chronic obstructive pulmonary disease (COPD) Prim Care Respir J. 2007;16:236–40. doi: 10.3132/pcrj.2007.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karimi Z, Majlesi F, Tol A, Foroushani RA, Aligol M, Mohebbi S. The effect of educational intervention on the promotion of physical activities of the elderly men in Qom City: Application of trans-theoretical model. Iran J Age. 2015;10:182–91. [Google Scholar]
- 24.Solimanian A, Niknami SH, Hajizadeh E, Shojaeezadeh D, Tavousi M. Predictors of physical activity to prevent osteoporosis based on extended Health Belief Model. PAYESH. 2014;13:313–20. [Google Scholar]
- 25.Parsamehr M, Niknejad M, Hedat E. Investigate the relationship between social cognitive patterns and motivation to do physical activity Humanities students of Yazd University. Pazhooheshnameh Modiriate Varzeshi Raftare Harekati. 2015;11:185–92. [Google Scholar]
- 26.Abdi J, Eftekhar H, Mahmoodi M, Shojayzadeh D, Sadeghi R. Effect of the intervention based on new communication technologies and the social-cognitive theory on the lifestyle of the employees with overweight and obesity. J Sch Public Health Institute Public Health Res. 2016;14:1–4. [PubMed] [Google Scholar]
- 27.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. London: John Wiley & Sons; 2008. [Google Scholar]
- 28.Reinaerts E, de Nooijer J, Candel M, de Vries N. Increasing children's fruit and vegetable consumption: Distribution or a multicomponent programme? Public Health Nutr. 2007;10:939–47. doi: 10.1017/S1368980007665495. [DOI] [PubMed] [Google Scholar]
- 29.Saffari M, Shojaeizadeh D, Ghofranipour F, Heydarnia A, Pakpour A. Health Education and Promotion-theories, Models and Methods. Tehran: Sobhan Pub; 2009. pp. 12–21. [Google Scholar]
- 30.Daranjani KS, Panah YA, Kharazmi E. The effect of health education program based on trans theoritical model on promotion of physical activity among children of patients with hypertension and diabetes. J Health. 2017;8:394–407. [Google Scholar]
- 31.Basen-Engquist K, Carmack CL, Li Y, Brown J, Jhingran A, Hughes DC, et al. Social-cognitive theory predictors of exercise behavior in endometrial cancer survivors. Health Psychol. 2013;32:1137–48. doi: 10.1037/a0031712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rogers LQ, Matevey C, Hopkins-Price P, Shah P, Dunnington G, Courneya KS. Exploring social cognitive theory constructs for promoting exercise among breast cancer patients. Cancer Nurs. 2004;27:462–73. doi: 10.1097/00002820-200411000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Glanz KA, Rimer BA, Viswanath K. Research and Practice. 4th ed. San Farancisco: Josey-Bass Publisher; 2008. Health Behavior and Health Education Theory? pp. 25–175. [Google Scholar]
- 34.Dalvandi A, Monjazebi F, Ebadi A, Khankeh H, Rahgozar M, Richter J. Psychometric properties of instruments measuring activities of daily living in patients with COPD: A systematic review. COPD. 2014;4(2):57–76. [Google Scholar]
- 35.Kara Kaşikçi M, Alberto J. Family support, perceived self-efficacy and self-care behaviour of Turkish patients with chronic obstructive pulmonary disease. J Clin Nurs. 2007;16:1468–78. doi: 10.1111/j.1365-2702.2006.01782.x. [DOI] [PubMed] [Google Scholar]
- 36.Lawshe CH. A quantitative approach to content validity. Personnel Psych. 1975;28:563–75. [Google Scholar]
- 37.Waltz CF, Bausell RB. Nursing Research: Design, Statistics, and Computer Analysis. Philadelphia: W B Saunders Co; 1981. p. 45. [Google Scholar]
- 38.Zendehtalab H. The effect of a program designed based on precede-proceed model on adolescents’ mental health and their parents’ participation. Evidence Based Care. 2012;2(1):45–54. [Google Scholar]
- 39.Omidi S, Farmanbar R, Mokhtarpour S. The effect of educational intervention based on PRECEDE-PROCEED model on promoting traffic safety behaviors in primary schools students of Tabriz in 2014. J Educ Community Health. 2016;2:48–56. [Google Scholar]
- 40.Solhi M, Hamedan SM, Salehi M. The effect of educational intervention based on PRECEDE-PROCEED model on the life quality of women-headed households covered by Tehran Welfare Organization. Iran J Health Educ Health Promot. 2017;15:259–70. [Google Scholar]
- 41.Peerson A, Saunders M. Health literacy revisited: What do we mean and why does it matter? Health Promot Int. 2009;24:285–96. doi: 10.1093/heapro/dap014. [DOI] [PubMed] [Google Scholar]
- 42.Hamedanizadeh F, Ebadi A, Zandi A, Kachuyee H. Effectiveness of implementation of Orem self-care program on headache indices in Migraine. Trauma Monthly. 2010;3:155–61. [Google Scholar]
- 43.Whaley DD. MSc Thesis. Florida: School of Nursing. The Florida State University; 2005. The Effect of Nutrition and Physical Activity Counseling on Knowledge and Behavior of Elementary Students In a Rural, Coastal Community. [Google Scholar]
- 44.Shirvani H, Sanaeinasab H, Tavakoli R, Saffari M, Khalaji K, Me'mar S. The effect of a social cognitive theory-based educational intervention on the physical activity of female adolescents. Iran J Health Educ Health Promot. 2016;4:309–18. [Google Scholar]
- 45.Ghasemi GS, Mohebbi B, Sadeghi R, Tol A, Mirzaei H, Hassanzadeh A. The effect of educational intervention on prevention of cardiovascular risk factors among girl students of secondary course in high school: Application of Social Cognitive Theory. Nursing education journal. 2017;6:26–37. [Google Scholar]
- 46.Gustafson SL, Rhodes RE. Parental correlates of physical activity in children and early adolescents. Sports Med. 2006;36:79–97. doi: 10.2165/00007256-200636010-00006. [DOI] [PubMed] [Google Scholar]
- 47.Peterson MS, Lawman HG, Wilson DK, Fairchild A, Van Horn ML. The association of self-efficacy and parent social support on physical activity in male and female adolescents. Health Psychol. 2013;32:666–74. doi: 10.1037/a0029129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lubans D, Sylva K. Controlled evaluaton of a physical actvity interventon for senior school students: Effects of the lifetime activity program. J Sport Exercise Psychol. 2006;28:252–68. [Google Scholar]
- 49.Aljasem LI, Peyrot M, Wissow L, Rubin RR. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001;27:393–404. doi: 10.1177/014572170102700309. [DOI] [PubMed] [Google Scholar]
- 50.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29:823–9. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- 51.Wu SF, Huang YC, Lee MC, Wang TJ, Tung HH, Wu MP. Self-efficacy, self-care behavior, anxiety, and depression in Taiwanese with type 2 diabetes: A cross-sectional survey. Nurs Health Sci. 2013;15:213–9. doi: 10.1111/nhs.12022. [DOI] [PubMed] [Google Scholar]
- 52.McCleary-Jones V. Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF J. 2011;22:25–32. [PubMed] [Google Scholar]
- 53.Ramirez E, Kulinna PH, Cothran D. Constructs of physical activity behaviour in children: The usefulness of Social Cognitive Theory. Psychol Sport Exerc. 2012;13:303–10. [Google Scholar]
- 54.Mahdizadeh M, Peymam N, Taghipour A, Esmaily H, Mahdizadeh SM. Effect of health education program on promoting physical activity among diabetic women in Mashhad, Iran: Applying social cognitive theory. J Res Health Sci. 2013;13:90–7. [PubMed] [Google Scholar]
- 55.Reisi M, Mostafavi F, Javadzade H, Mahaki B, Tavassoli E, Sharifirad G. Impact of health literacy, self-efficacy, and outcome expectations on adherence to self-care behaviors in iranians with type 2 diabetes. Oman Med J. 2016;31:52–9. doi: 10.5001/omj.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]