Abstract
Rationale & Objective
Data suggest that exercise is beneficial for patients with chronic kidney disease (CKD) to reduce cardiovascular disease and the progression of CKD. Despite these benefits, the majority of patients with CKD remain sedentary. The purpose of this study was to identify attitudes, motivators, and barriers to exercise among individuals with CKD.
Study Design
Qualitative study.
Setting & Participants
10 focus groups (41 adult participants with CKD stages 3-4 who were not currently exercising) from the Denver Metro Area.
Analytical Approach
Thematic analysis. Clinics were purposively sampled. Focus groups were recorded and transcribed.
Results
We identified 7 themes reflecting perceptions of exercise of patients with CKD: improvement in health and quality of life; motivation from family, friends, or peers; limitations due to comorbid conditions; challenges due to environmental factors (safety, weather, and cost concerns); lack of time; family as a barrier; and lack of provider counseling on type of exercise and the benefits. Participants recognized the benefits of exercise on health, but exercise was not viewed to have a significant impact on CKD. Having a friend, family member, or group to exercise with was viewed as a significant motivator. However, particularly in Spanish-speaking participants, family was often seen as a barrier if they were not willing to exercise with the patients. Most participants expressed receiving limited information from their kidney provider regarding how exercise affected their kidney health. Spanish-speaking participants in particular expressed frustration with their nephrologist's lack of advice regarding exercise.
Limitations
Potential selection bias and inclusion of only sedentary patients with CKD.
Conclusions
Barriers and motivators to exercise were similar among participating men and women with CKD. Lack of advice from kidney providers regarding exercise was a significant barrier. Exercise interventions in patients with CKD should include not only increased patient self-efficacy and social support, but also counseling and prescribing of exercise by nephrologists.
Index Words: Exercise, chronic kidney disease, focus group, qualitative study, patient perspective
Chronic kidney disease (CKD) is now being recognized as an important worldwide public health problem. Patients with CKD have a reduced lifespan compared to the general population and the majority of patients die of cardiovascular disease (CVD).1 Physical activity is remarkably low in patients with CKD; physical function measures an average 60% to 65% of age-matched controls.2 Low physical activity is associated with increased inflammation and oxidative stress, both of which lead to increased atherosclerosis and CVD.3 Data suggest that exercise is beneficial for patients with CKD. The adjusted risk for death and end-stage kidney disease is lower in patients with CKD who are physically active compared with those who are inactive.4 Despite the benefits of exercise in patients with CKD, the majority of patients remain sedentary.
Lifestyle interventions, including exercise, for the prevention of kidney disease progression and symptoms have been consistently identified by patients as a top research priority.5, 6 Understanding patients’ attitudes, motivators, and barriers to physical activity will allow us to design socially and culturally appropriate interventions to increase physical activity in patients with CKD. However, there is a paucity of data regarding the attitudes and beliefs toward physical activity in patients with CKD who are not yet receiving dialysis. The social cognitive theory (SCT) emphasizes interactions among personal, environmental, and behavioral factors in determining human behavior.7 The theory stresses the need to identify barriers and motivations to an activity such as exercise, which can then be targeted to change the health behavior. We performed a qualitative study to identify attitudes, motivators, and barriers to exercise for patients with CKD.
Methods
Participants
We recruited adult patients aged 20 to 65 years with CKD stages 3 and 4 who were not currently physically active from nephrology clinics at the University of Colorado. We purposively sampled participants based on age, sex, race/ethnicity, and kidney function to ensure a diverse range of demographic and clinical characteristics. “Not physically active” was defined as not completing 150 minutes a week of moderate-intensity or 75 minutes a week of high-intensity aerobic physical activity.8 Focus groups were divided by sex and language (English and Spanish). Groups were divided by sex because women may have different views and barriers to exercise and may not feel comfortable discussing issues regarding exercise in front of men. Participants with more advanced CKD were chosen given their higher rate of CVD.1 We targeted 6 to 8 participants in each focus group. Participants were reimbursed $25 to cover incidental costs, and transportation was provided if needed. All participants provided informed consent.
Data Collection
The focus group guide (Item S1) was based on previous research studies in dialysis patients and patients with CKD2, 9 and discussion among the research team. Questions were aimed at exploring perceptions, barriers, motivators, and outcome expectations to exercise. All focus groups were conducted on the University of Colorado or Denver Health Medical Center campus in nonclinical areas. One of the investigators (J.K.) facilitated the English-speaking focus groups and another Spanish-speaking investigator (S.R.) facilitated the Spanish-speaking groups. A second investigator (E.A.) took notes during the sessions. One of the investigators was a nephrologist (J.K.) but did not directly care for any of the participants in the study. All facilitators of the focus groups were women. All focus groups were digitally audiotaped and transcribed. Focus groups were conducted until theoretical saturation was reached, the point at which we were no longer gaining new insights. Each participant also completed a brief demographic questionnaire that included age, sex, race/ethnicity, and how long the patient has had CKD. Each focus group was 60 to 90 minutes in length.
This study was approved by the Colorado Institutional Review Board (Record Number 16-0033), and we followed the Consolidated Criteria for Reporting Qualitative Health Research (COREQ).10
Analysis
Using thematic analysis, J.K. and E.A. read the transcripts line by line; identified key concepts, themes, and ideas; and developed a preliminary coding scheme. The investigators coded the data in parallel and identified the main themes. The investigators (J.K, E.A, and M.R.) then discussed and reviewed the main themes and reduced overlap and redundancy among the categories until agreement was reached. J.K. recoded the transcripts to the revised themes and then all investigators reviewed them again. Investigator triangulation ensured that the range and depth of the concepts from the data were captured in the themes.
Results
We conducted 10 focus groups with 41 participants from May 2016 through December 2016. Six focus groups were conducted in English and 4 focus groups were conducted in Spanish. The range of participants in the groups was 2 to 7. Participant characteristics are shown in Table 1. More than 50% of participants were 60 to 65 years of age, 51.2% were women, and 29.3% were Spanish speaking.
Table 1.
Characteristics of Study Participants
| Characteristic | N (%) |
|---|---|
| Age, y | |
| 30-39 | 3 (7.3%) |
| 40-49 | 6 (14.6%) |
| 50-59 | 10 (24.4%) |
| 60-65 | 22 (53.7%) |
| Sex | |
| Men | 20 (48.8%) |
| Women | 21 (51.2%) |
| Language | |
| Spanish | 12 (29.3%) |
| Race | |
| White | 29 (70.7%) |
| Black | 7 (17.1%) |
| Other | 5 (12.2%) |
| Ethnicity | |
| Hispanic | 18 (43.9%) |
| Duration of kidney disease | |
| <1 y | 7 (17.5%) |
| 1-3 y | 13 (32.5%) |
| 4-7 y | 9 (22.5%) |
| 8-10 y | 4 (10.0%) |
| 10-12 y | 1 (2.5%) |
| 13-15 y | 2 (5.0%) |
| >15 y | 4 (10.0%) |
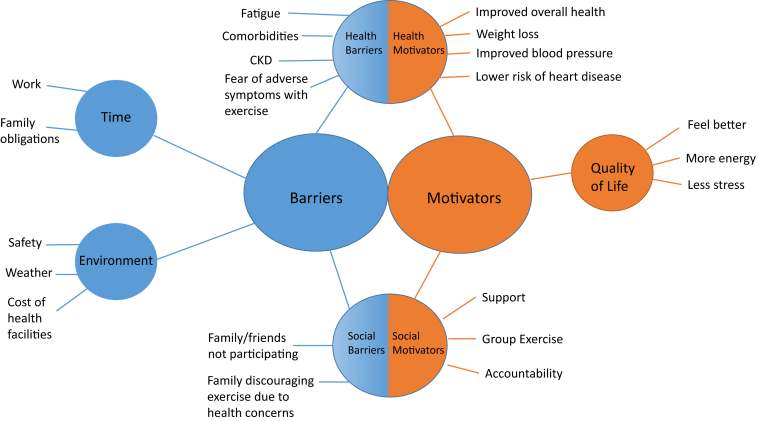
Seven themes were identified: 2 related to motivators (improved overall health and quality of life and motivation from family, friends, or peers) and 5 related to barriers (limited by comorbid conditions, physical environment [safety, weather, and cost concerns], lack of time, family as a barrier; and lack of provider counseling on type of exercise and the benefits). Figure 1 summarizes the resulting themes. Selected quotations from each theme are provided in Table 2.
Figure 1.
Summary of themes identified as barriers and motivators to physical activity. Abbreviation: CKD, chronic kidney disease.
Table 2.
Selected Participant Quotations for Each Theme Identified
| Theme | Quotations | Focus Group Contributing to Theme |
|---|---|---|
| Improved overall health and quality of life | “Well, when you exercise, all the levels get stable, like your sugar level, your blood pressure, your weight, you gain energy, to be healthy.” (Group 5, man, Spanish speaking) “Every time I work out, I feel less tired. I feel better when I exercise.” (Group 7, man, Spanish speaking) “Mobility and flexibility. I’ve got arthritis-I’ve got it bad in the knees and hips and arms and hands. If I exercise, if I do it regularly, it helps.” (Group 2, man) “Helps you live longer.” (Group 3, woman) |
Groups 1-10 |
| Motivation from family, friends, or peers | “You can talk to someone who can relate while you are walking, so that’s always helpful and nice, but there is someone who understands that you are limited too because they are as well.” (Group 3, woman) “I need to commit to someone to exercise, I don’t know why I need someone or wait for someone to do it and not do it on my own.” (Group 5, man, Spanish speaking) “Group of conversation with information, many of them, with testimonials of other patients and their experiences, regarding if the exercises have helped them and the results.” (Group 8, woman, Spanish speaking) |
Groups 1-10 |
| Limited by comorbid conditions | “I am afraid that I will have a stroke…pain in my chest, so to not feel it, I avoid exercise.” (Group 6, man) “In that case, you feel like you will die, you feel dizzy and that is why I think I will get a stroke or heart attack, but your heart is agitated, working extra to the maximum.” (Group 5, man, Spanish speaking) “I used to love to exercise but now I can’t do it. You know, I just can’t breathe right, I don’t have the energy.” (Group 2, man) |
Groups 1, 2, 3, 5-7, 10 |
| Physical environment: safety, weather, and cost | “It’s not safe to go out after 5 pm where I live.” (Group 10, woman, Spanish speaking) “In the winter, it is too cold and there is nowhere for me to exercise inside.” (Group 2, man) “I don’t have the money to go to a gym or take (exercise) classes.” (Group 1, man) |
Groups 1-10 |
| Lack of time | “I’m more tired now. I work full time and I’m doing like 10 hours a day. I’m just so worn out at the end of the day.” (Group 4, woman) “I have too much stress at work; and work takes too much of my time.” (Group 2, man) “I take care of my grandkids, I make the food, the chores of the house, I don’t have time for exercise.” (Group 8, woman, Spanish speaking) |
Groups 1-10 |
| Family as a barrier to exercise | “They are taking care of me so I don’t exercise, because I get tired and they keep telling me not to exercise.” (Group 5, man, Spanish speaking) “I tell my wife, let’s go walking and if she doesn’t want to go, I don’t go.” (Group 7 woman, Spanish speaking) “I like walking but my husband doesn’t like it and I don’t go on my own.” (Group 8, woman, Spanish speaking) |
Groups 2, 4, 5, 7, 8, 10 |
| Lack of exercise counseling from kidney provider | “Basically, they tell you exercise would be beneficial but nothing specific.” (Group 2, man) “My doctor has actually said nothing.” (Group 3, woman) “If I have trust with my doctor, I think he can tell me ‘if you want to see your grandkid grow, then put more energy, more motivation in exercise’.” (Group 10, woman, Spanish speaking) |
Groups 1-10 |
Motivations
Improving Overall Health and Quality of Life
Exercise was recognized as having a beneficial impact on health, both mentally and physically. The recognized benefits included weight loss, cardiovascular protection, lowered blood pressure, improved glucose control, reduced stress, preventing further functional decline, and increased longevity. However, exercise was not viewed to have a significant impact on kidney disease progression or symptoms of CKD. Participants were not aware of benefits of exercise specifically related to kidney disease. One participant acknowledged that “If I thought that it would help my kidney disease I would probably put a bigger foot forward to try to do better at exercise” (group 1, man). The Spanish-speaking groups reflected more often on the tangible benefits of exercise such as less fatigue and feeling better after exercise, whereas the English-speaking groups more frequently identified the intangible benefits of exercise such as reduction in blood pressure and improved glucose control. “We should think of exercise as something that gives us energy and if we do exercise, that will give us energy” (group 8, woman, Spanish speaking).
Participants also discussed how exercise may empower them to improve their health. Several participants noted that exercise could be used as a way to make them feel they are taking control of something in their life. “You can say, ‘I have this disease but it doesn’t have me’” (group 1, man). “I would suggest to not keep thinking that you have the disease, to keep moving forward, fighting it because if you keep thinking that you are sick you get worse” (group 7, man, Spanish speaking).
Motivation From Family, Friends, and Peers
Social support was mentioned as a motivating factor regarding exercise participation. Social support was preferred from friends, family, or peers with similar health comorbid conditions. Group activities ranged from exercise classes and dance classes to running groups. Groups improved exercise adherence by holding participants accountable and providing additional motivation to complete exercise goals. Women frequently acknowledged they would like to exercise with peers or hear testimonials of how exercise benefited others in similar circumstances. If family participated in an exercise regimen, it was viewed as encouraging further exercise. “My family monitors my fitness tracker, which holds me accountable” (group 4, woman). Many participants agreed that it would be helpful to have exercise groups with people who have kidney disease. “Yes, we have the same disease, we know what is good for us, and we can put together an exercise group to support each other” (group 10, female, Spanish-speaking). Finally, if the end result of exercise resulted in increased longevity and increased time with family or friends, it was viewed as a motivation for continued exercise.
Barriers
Limited by Comorbid Conditions
Health-related concerns were a consistent barrier to exercise among all participants. Participants’ concerns focused on the limitations imposed by their underlying medical comorbid conditions and the fear regarding how stress associated with exercise affected their health. The medical comorbid conditions that were discussed as preventing exercise included CVD, diabetes, osteoarthritis, chronic pain, hernia, and cataracts. Fatigue was the most frequently listed symptom in preventing exercise.
Health-related exercise complications appeared to have a bigger role in the male groups in preventing exercise. Their fear often revolved around the symptoms experienced during exercise, such as dizziness, chest discomfort, and shortness of breath. Several male participants voiced concerns regarding their heart or having a stroke during exercise. A concern expressed by many participants included the possibility of developing diabetic foot blisters or leg swelling during exercise. One Spanish-speaking participant was concerned that exercise would affect his kidneys in a negative way. “Yes, they say that if I use too much strength or if I lift too much weight that affects my kidneys” (group 7, man, Spanish speaking). More women than men reported a fear of falling with exercise.
Physical Environmental: Safety, Weather, and Cost
Participants discussed several environmental factors as barriers to physical activity. Being located in Colorado, many of the participants reported weather as a significant concern. Several participants noted that they are less motivated to exercise in the winter due to the cold weather and snow. Participants also reported issues with the surrounding environment in their neighborhoods. In many areas where participants lived, there were no parks or other safe areas to exercise. Women expressed concerns regarding personal safety with exercise because participants reported it was unsafe to walk alone in their neighborhood. “More because of safety, there are thefts, if it is getting dark I am scared to go out” (group 8, woman, Spanish speaking). Several participants did not have any gyms or health clubs near their homes. Although some participants reported that there were health clubs or gyms near their homes, they acknowledged that the cost was prohibitive in joining. Participants agreed that they would be more likely to exercise if they had access to and more information on opportunities for classes, group exercise events, dance classes, etc.
Lack of Time
Participants reported that exercise is time consuming. Most participants reported lack of time as a reason they are not exercising. Many of the participants work and had difficulty finding time to exercise. “It is a time thing. Sometimes after work you get home and you just want to lie down as you are tired from work” (group 6, man). Family child care obligations were also a concern, more in women than men. Women participants discussed having to care for grandchildren as a reason for lack of time to exercise. One participant said “I don’t go [work out] because of time, I take care of my grandkids and I am with them all the time” (group 10, woman, Spanish speaking).
Family as a Barrier to Exercise
While social support was seen as a motivator by all participants, it was also seen as a barrier, specifically in regard to family and most often in Spanish-speaking participants. If other family members did not participate in an exercise regimen, it was often seen as discouraging exercise habits. One participant discussed her struggles to get her family to exercise, “I struggle with my family because nobody wants to go out. I always tell them let’s go for a walk and no one goes. I think that is the problem, I need more support from my family…” (group 10, woman, Spanish speaking). For some participants, family discouraged exercise, cautioning about physical health and ability to tolerate exercise.
Lack of Provider (Nephrologist) Counseling on Type of Exercise and the Benefits
Many participants expressed receiving limited information from their kidney physician regarding how exercise affected their kidney health. When participants received counseling about exercise, information lacked specifics and tended to focus on what amount of walking constitutes exercise. Some participants perceived this negatively because walking was not always the preferred method of exercise. The benefits of exercise that participants’ physicians most frequently listed focused on improvement in blood pressure and glucose control. Participants expressed interest in receiving more education regarding the benefits of exercise from their physicians. Specific information that participants thought would be beneficial included the impact of exercise on kidneys, specific exercise regimens to achieve health benefit, variety of exercise regimens, and information regarding how to interpret symptoms that participants experienced during exercise (ie, dizziness or leg swelling). “I would like my doctor to tell me which exercises will benefit my kidneys, we can get better you know, so the kidney can be more stable” (group 10, woman, Spanish speaking). Participants also thought it would be beneficial if their physician held them accountable and specifically asked about their exercise regimens at future visits. “I actually like structure, as long as they gave me the set ‘I want you to do…(blank)’ and told me so many hours or so many minutes a week” (group 1, man).
Participants predominantly in the male Spanish-speaking groups expressed frustration with their physicians regarding what constituted exercise. Many Spanish-speaking participants had a labor-intensive job that they believed constituted adequate exercise. One Spanish-speaking participant said, “I am a painter and am moving all the time… and my doctor says that is not exercise. Exercise is to walk.” Another Spanish-speaking participant stated, “All day (I am) cutting the yard, sweating and drinking water, but the doctor told me that is not exercising. That is my routine, he said.” One woman was frustrated that she could not understand what the physicians were telling her. “Well, I have a problem, they say so many things and I don’t learn them, when I was a girl, I went to school but didn’t learn to read” (group 8, woman, Spanish speaking).
Suggestions for Encouraging Exercise in Patients With CKD
Suggestions for supporting exercise in patients with kidney disease are shown in Box 1.
Box 1. Suggestions for Supporting Exercise in Patients With CKD.
Social Support
-
•
Peer support groups
-
•
Exercise groups (peers, family, or friends)
-
•
Family/friend support
-
•
Accountability
Health Care Provider Involvement
-
•
Improved knowledge of the benefits of exercise in patients with kidney disease
-
•
Counseling on safety and types of exercise to perform
-
•
Exercise prescriptions (specific regimen including frequency and duration)
-
•
Accountability; providers to follow-up on exercise progress at future visits
-
•
Help arrange CKD support/exercise groups
Community Support
-
•List of health clubs, gyms, and parks in neighborhoods
-
oList of free or low-cost indoor gyms/recreation space
-
o
Abbreviation: CKD, chronic kidney disease.
Discussion
Our study extends what is known about the perceived motivators and barriers to physical activity in patients with CKD. We found that social support and health care providers play a critical role in supporting exercise in patients with CKD. Nearly all participants reported that support from family, friends, or peers would hold them accountable and would increase the likelihood of exercise. Additionally, participants wanted information from their health care providers regarding the benefits of exercise, specifically for patients with kidney disease, as well as the type, frequency, and intensity of exercise they should be doing.
There are numerous health benefits to exercise in patients with CKD. In a study of more than 3,000 participants with estimated glomerular filtration rates < 60 mL/min, the incident rate of CKD requiring dialysis in patients with poor physical activity was twice the rate in patients with ideal physical activity.11 After adjustment for age, sex, race, income, education, history of stroke, and coronary heart disease, ideal physical activity was associated with a 50% reduced risk for end-stage kidney disease compared to poor physical activity (hazard ratio [HR], 0.50; 95% confidence interval [CI], 0.32-0.78).11 The adjusted risk for death is lower in patients with CKD who are physically active compared with those who are inactive (HR, 0.44; 95% CI, 0.33-0.58).4 Additionally, patients with CKD have a high burden of other chronic diseases for which exercise is beneficial, specifically diabetes and hypertension. Patients with CKD also have at least a 2- to 3-fold increased risk for cardiovascular events compared to the general population.1 Thus, potential benefits to exercise in this population include improvements in blood pressure control, quality of life, kidney disease progression, control of diabetes, cardiovascular health, and survival. Increasing physical activity in patients with CKD may have a significant impact on outcomes. All the patients included in our study recognized the health and quality-of-life benefits of exercise. However, the patients were not aware of kidney-specific benefits of exercise. Many expressed that they would be more likely to exercise if they knew it may have a positive effect on their kidney disease. Additionally, patients were concerned about their health during exercise and reported fears of worsening symptoms, such as chest pain, during exercise. Our study found that patients were receiving little information regarding exercise from their health care providers.
Health care providers have the most direct contact with patients and often are the people who inform patients of their health behaviors. From the patient perspective, the majority claim they are not receiving exercise advice/recommendations from health care providers. In a study of more than 500 patients in a primary care setting, only 4% reported that they received advice on exercise.12 Similar to our findings, another qualitative study in patients with CKD performed in the United Kingdom also found lack of information regarding benefits of exercise from health care providers.9 The patients in our study expressed that they would be receptive to advice from their provider and wanted more detailed information regarding exercise. Despite national guidelines recommending encouragement of physical activity as part of the management of CKD, only 28.5% of kidney specialists report routinely prescribing exercise for their patients.13 In this study, 40% of providers were concerned about the risks of exercise and >50% believed that patients would not exercise even if they were advised to do so.13
The SCT is one of the leading behavior change theories used to explain and predict physical activity.7 The SCT emphasizes personal and environmental factors as determinants of behavior. Self-efficacy and knowledge are key determinants of physical activity in many patient populations with chronic diseases. Increasing self-efficacy based on SCT models has been successful in increasing physical activity.14, 15 Improved counseling by health care providers in patients with CKD can address knowledge gaps and improve self-efficacy in patients with CKD. Studies done in overweight patients without CKD have shown that provider-based interventions on physical activity can be effective.16 Studies have shown that physician counseling and written materials result in an increase in the percentage of previously sedentary overweight individuals who exercise.17 In providers caring for other populations, the main barriers to exercise counseling include lack of time and lack of knowledge or experience on how to counsel patients.18 These same barriers may exist for providers caring for patients with CKD, but studies are needed to determine this.
Similar to findings from Clarke et al,9 social and family support were motivators for exercise. The majority of patients thought that group exercise with other patients with CKD would provide the most motivation for exercise. Social support is an important construct used in the SCT and it has been shown to be successful in promoting behavior change.19 Formulating or strengthening social networks has been shown to be beneficial to patients with CKD.20 Helping patients set up support groups and exercise groups with other patients with CKD may increase physical activity.
Barriers reported in our study are similar to previous studies regarding exercise in both patients with9 and without CKD.21, 22, 23 Time constraints, health concerns, physical environment concerns, and lack of counseling from health care providers were noted from all participants in our study. We found differences in barriers across sex and language. Compared with men, women reported more concerns regarding the physical environment and safety with exercise. Additionally, women reported lack of time due to child care obligations more often than men. Spanish-speaking patients, primarily men, expressed the most frustration with their health care providers. These patients felt disconnected from their health care providers regarding exercise discussions and in particular what type of activity constitutes exercise. Many of these patients reported heavy labor–intensive jobs and were told by their provider that this did not constitute exercise. This may in part be due to language barriers, but patients reported the use of interpreters at visits. This further supports the notion that increased knowledge and exercise counseling by health care providers is important.
We included only patients from Colorado and excluded older adults (aged >65 years) and thus our findings may not be transferable to all patients with CKD stages 3 and 4. We included only participants who were not currently physically active and results may have been different in patients who are currently exercising. Additionally, despite significant recruiting efforts, not all our focus groups had 6 to 8 participants. We did not collect information regarding employment, income, or comorbid conditions.
Notwithstanding these limitations, our study also has several strengths. We included men and women of all races/ethnicities and included Spanish-speaking patients. To our knowledge, this is the first study in patients with CKD not receiving dialysis to examine both English- and Spanish-speaking patients.
Our study provides better understanding of motivators and barriers to exercise for patients with CKD. Findings of our study highlight the importance of the relationship between health care providers and patients. Intervention programs aimed at improving exercise should incorporate exercise counseling and perhaps exercise prescriptions by providers. Increased engagement by providers will provide improvements in patient knowledge and self-efficacy. Additionally, providers may be able to help organize support and exercise groups for patients with CKD. Changing the culture of CKD care to include exercise counseling and encouragement may lead to improved outcomes.
Article Information
Authors’ Full Names and Academic Degrees
Jessica Kendrick, MD, MPH, Michael Ritchie, MD, and Emily Andrews, MS.
Authors’ Contributions
Research idea and study design: JK; data acquisition: JK, EA; data analysis and interpretation: JK, MR, EA; supervision or mentorship: JK. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
This work was supported by National Heart Blood and Lung Institute R01 HL132868. The funders did not have any role in study design; data collection, analysis, or reporting; or the decision to submit for publication.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Acknowledgements
We thank Ms Silvia Raghunath for assistance in facilitating the Spanish focus groups.
Peer Review
Received January 24, 2019. Evaluated by 2 external peer reviewers, with direct editorial input from the Editor-in-Chief. Accepted in revised form March 13, 2019.
Footnotes
Complete author and article information provided before references.
Item S1: Focus Group Question Guide.
Supplementary Material
Item S1. Focus Group Question Guide.
References
- 1.Go A.S., Chertow G.M., Fan D., McCulloch C.E., Hsu C.Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 2.Johansen K.L., Painter P. Exercise in individuals with CKD. Am J Kidney Dis. 2011;59(1):126–134. doi: 10.1053/j.ajkd.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart L.K., Flynn M.G., Campbell W.W. The influence of exercise training on inflammatory cytokines and C-reactive protein. Med Sci Sports Exerc. 2007;39:1714–1719. doi: 10.1249/mss.0b013e31811ece1c. [DOI] [PubMed] [Google Scholar]
- 4.Beddhu S., Baird B.C., Zitterkoph J. Physical activity and mortality in chronic kidney disease (NHANES III) Clin J Am Soc Nephrol. 2009;4:1901–1906. doi: 10.2215/CJN.01970309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tong A., Sainsbury P., Carter S.M. Patients’ priorities for health research: focus group study of patients with chronic kidney disease. Nephrol Dial Transplant. 2008;23(10):3206–3214. doi: 10.1093/ndt/gfn207. [DOI] [PubMed] [Google Scholar]
- 6.Hemmelgarn B.R., Pannu N., Ahmed S.B. Determining the research priorities for patients with chronic kidney disease not on dialysis. Nephrol Dial Transplant. 2017;32(5):847–854. doi: 10.1093/ndt/gfw065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McAlister A.L., Perry C.L., Parcel G.S. How individuals, environments and health behaviors interact: social cognitive theory. In: Glanz K., Rimer B., Viswanath K., editors. Health Behavior and Health Education: Theory, Research and Practice. 4th ed. John Wiley and Sons; San Francisco, CA: 2008. pp. 169–185. [Google Scholar]
- 8.US Department of Health and Human Services . US Department of Health and Human Services; Washington, DC: 2008. 2008 Physical Activity Guidelines for Americans.http://www.health.gov/paguidelines ODPHP Publication No. U0036. [Google Scholar]
- 9.Clarke A.L., Young H.M., Hull K.L., Hudson N., Burton J.O., Smith A.C. Motivations and barriers to exercise in chronic kidney disease: a qualitative study. Nephrol Dial Transplant. 2015;30(11):1885–1892. doi: 10.1093/ndt/gfv208. [DOI] [PubMed] [Google Scholar]
- 10.Tong A., Sainsbury P., Craig J. Consolidated Criteria for Reporting Qualitative Research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 11.Muntner P., Judd S., Gao L. Cardiovascular risk factors in CKD associate with both ESRD and mortality. J Am Soc Nephrol. 2013;24(7):1159–1165. doi: 10.1681/ASN.2012070642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duaso M.J., Cheung P. Health promotion and lifestyle advice in general practice: what do patients think? J Adv Nurs. 2002;39(5):472–479. doi: 10.1046/j.1365-2648.2002.02312.x. [DOI] [PubMed] [Google Scholar]
- 13.Johansen K.L., Sakkas G.K., Doyle J., Shubert T., Dudley R.A. Exercise counseling practices among nephrologists caring for patients on dialysis. Am J Kidney Dis. 2003;41(1):171–178. doi: 10.1053/ajkd.2003.50001. [DOI] [PubMed] [Google Scholar]
- 14.Liebreich T., Plotnikoff R.C., Courneya K.S., Boule N. Diabetes NetPLAY: a physical activity website and linked email counseling randomized intervention for individuals with type 2 diabetes. Int J Behave Nutr Phys Act. 2009;6:18. doi: 10.1186/1479-5868-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.White S.M., Wojcicki T.R., McAuley E. Social cognitive influences on physical activity behavior in middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci. 2012;67(1):18–26. doi: 10.1093/geronb/gbr064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Logsdon D.N., Lazaro C.M., Meier R.V. The feasibility of behavioral risk reduction in primary medical care. Am J Prev Med. 1989;5(5):249–256. [PubMed] [Google Scholar]
- 17.Calfas K.J., Long B.J., Sallis J.F., Wooten W., Pratt M., Patrick K. A controlled trial of physician counseling to promote the adoption of physical activity. Prev Med. 1996;25(3):225–233. doi: 10.1006/pmed.1996.0050. [DOI] [PubMed] [Google Scholar]
- 18.Abramson S., Stein J., Schaufele M., Frates E., Rogan S. Personal exercise habits and counseling practices of primary care physicians: a national survey. Clin J Sport Med. 2000;10(1):40–48. doi: 10.1097/00042752-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Anderson-Bill E.S., Winett R.A., Wojcik J.R., Williams D.M. Aging and the social cognitive determinants of physical activity behavior and behavior change: evidence from the guide to health trial. J Aging Res. 2011;2011:505928. doi: 10.4061/2011/505928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bruce M., Beech B., Sims M. Social environmental stressors, psychological factors, and kidney disease. J Investig Med. 2009;57(4):583–589. doi: 10.231/JIM.0b013e31819dbb91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lidegaard L.P., Schwennesen N., Willaing I., Faerch K. Barriers to and motivator for physical activity among people with type 2 diabetes: patients’ perspectives. Diabet Med. 2016;33(12):1677–1685. doi: 10.1111/dme.13167. [DOI] [PubMed] [Google Scholar]
- 22.Kosteli M.C., Heneghan N.R., Roskell C. Barriers and enablers of physical activity engagement for patients with COPD in primary care. Int J Chronic Obstruct Pulmon Dis. 2017;12:1019–1031. doi: 10.2147/COPD.S119806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keogh J.W., Patel A., MacLeod R.D., Masters J. Perceived barriers and facilitators to physical activity in men with prostate cancer: possible influence of androgen deprivation therapy. Eur J Cancer Care. 2014;23(2):263–273. doi: 10.1111/ecc.12141. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Item S1. Focus Group Question Guide.