ABSTRACT
Background
Rates of childhood obesity are higher in American Indian and Alaska Native populations, and food insecurity plays a major role in diet-related disparities. To address this need, local healthcare providers and a local nonprofit launched the Navajo Fruit and Vegetable Prescription (FVRx) Program in 2015. Children up to 6 y of age and their caregivers are enrolled in the 6-mo program by healthcare providers. Families attend monthly health coaching sessions where they receive vouchers redeemable for fruits, vegetables, and healthy traditional foods at retailers participating in the FVRx program.
Objectives
We assessed the impact of a fruit and vegetable prescription program on the health outcomes and behaviors of participating children.
Methods
Caregivers completed voluntary surveys to assess food security, fruit and vegetable consumption, hours of sleep, and minutes of physical activity; healthcare providers also measured children's body mass index [BMI (kg/m2)] z score at initiation and completion of the program. We calculated changes in health behaviors, BMI, and food security at the end of the program, compared with baseline values.
Results
A total of 243 Navajo children enrolled in Navajo FVRx between May 2015 and September 2018. Fruit and vegetable consumption significantly increased from 5.2 to 6.8 servings per day between initiation and program completion (P < 0.001). The proportion of participant households reporting food insecurity significantly decreased from 82% to 65% (P < 0.001). Among children classified as overweight or obese at baseline, 38% achieved a healthy BMI z score at program completion (P < 0.001). Sixty-five percent of children were retained in the program.
Conclusions
The Navajo FVRx program improves fruit and vegetable consumption among young children. Children who are obese or overweight may benefit most from the program.
Keywords: produce prescription program, childhood obesity; American Indians; Navajo; indigenous; rural; body mass index
Introduction
Childhood overweight and obesity is a major health concern in the United States, especially among American Indian and Alaska Native (AI/AN) populations. Rates of pediatric overweight and obesity in this population now exceed those of the general US population (1). A 2017 study of 184,000 AI/AN youth ages 2–19 y found that nearly half were classified as either overweight or obese (2). Childhood obesity can contribute to increased risk for many conditions later in the life course, including type 2 diabetes, nonalcoholic fatty liver disease, and polycystic ovarian syndrome (3). The rise in childhood overweight and obesity parallels a trend in earlier onset of diet-related chronic diseases among AI/AN populations; for instance, type 2 diabetes, typically manifested in adults, is now encountered more commonly among AI/AN children and adolescents (4–7).
A key determinant related to childhood nutritional problems is food insecurity. Food insecurity is defined as “the disruption of food intake or eating patterns because of lack of money and other resources (8).” For many AI/AN populations, food insecurity is a major driver of health disparities (2, 9). High rates of food insecurity in Native communities (10–12) are largely due to historical patterns of colonization that replaced indigenous food systems with a forced reliance on affordable but calorie-dense foods (13–15). Given the complex historical and cultural forces that have shaped Native food systems, a socioecological model provides a logical framework to inform childhood obesity interventions in AI/AN populations (16). A multilevel intervention that targets health behavior while simultaneously strengthening food systems might arguably have greater impact on childhood obesity than a program focused solely on behavior change or environmental change alone (17–19).
One such strategy is the Fruit and Vegetable Prescription Program (FVRx), which works with stores and growers to increase community access to fruits and vegetables, while providing food vouchers and tailored health coaching to families with children facing diet-related disparities (20). Produce prescription programs have demonstrated success in increasing fruit and vegetable consumption and, among individuals with diabetes, improving blood glucose control (21–25). However, these programs have been predominantly implemented in urban areas, and to our knowledge, there are no published reports of any program implemented in an indigenous community. Furthermore, few studies have examined the effect of produce prescription programs on the health behaviors of young children, and none, to our knowledge, have evaluated pediatric body mass index [BMI (kg/m2)] outcomes (26). Evaluating the impact of produce prescription programs is critical to identifying effective strategies for promoting healthy behaviors in early childhood and addressing the burden of childhood overweight and obesity.
In 2015, the Community Outreach and Patient Empowerment (COPE) Program launched the Navajo FVRx Program to increase healthy food access and promote early child health (23). Stakeholders chose this program as a cross-sector strategy that would address the diverse needs of families with young children, healthcare providers, store retailers, and local growers. Healthcare providers prescribe vouchers that are redeemable for fruits, vegetables, and healthy traditional foods at participating supermarkets, convenience stores, and farmers markets. Enrolled families also attend monthly health coaching sessions. Providers collect routine programmatic data for monitoring and evaluation purposes. This report describes the impact of FVRx among children enrolled in the first 4 y of implementation. Program evaluation focused on determining changes in health behavior, BMI, and household food insecurity.
Methods
We conducted a programmatic evaluation among all children 6 y of age or younger enrolled in the Navajo FVRx program between May 2015 and September 2018.
Program setting and design
The Navajo Nation is one of the largest tribal reservations in the United States, spanning over 27,000 square miles across Utah, Arizona, and New Mexico. Per 2010 Census data, the Navajo Nation is home to over 170,000 residents, of whom approximately 11,000 (6.5%) are children under the age of 6 y (27, 28). Navajo Nation is classified as a food desert, which the USDA defines as a region with limited access to affordable and nutritious food (29, 30). Only 13 supermarkets operate on the Nation—a geographical area approximately the size of West Virginia (15). In addition, there are >100 convenience stores and trading posts, yet these small stores carry fewer nutritious foods than supermarkets (15). More than 70% of Navajo households are food insecure, among the highest reported rates in the United States. (31).
From 2015 to 2018, 19 healthcare facilities and 25 retailers collaborated to implement the Navajo FVRx Program. Healthcare facilities ranged from hospitals to small clinics, and retailers ranged from grocery stores to convenience stores, trading posts, and farmers markets. Community input, along with technical support from Wholesome Wave, informed the program's design and implementation (32). The program is described in more detail elsewhere (23). Briefly, the pediatric Navajo FVRx program during this period was implemented as follows: Interprofessional teams first underwent training by COPE staff. Team composition varied across sites, including dieticians, physicians, nurses, nutritionists, community health representatives, and/or Head Start staff. Eligibility criteria were intentionally broad: families must have a pregnant woman (“maternal group”) or a child <6 y of age (“pediatric group”). Teams were allowed to further narrow their site-specific enrollment criteria; for instance, some sites used the Indian Health Service Food Insecurity Screening Questionnaire to enroll families experiencing food insecurity (33, 34). For pediatric groups, providers enrolled children and their caregivers into a 6-mo program, first explaining the program and inviting the family to participate. Families who agreed to take part received an enrollment packet including an FVRx ID card, a list of participating retailers, and a handout describing allowable food items, i.e., fruits, vegetables, and healthy Diné (Navajo) foods such as blue cornmeal, dried steam corn, and sumac berries. Providers prescribed vouchers valued at US$1 per household member per day, with a maximum value of $5/d. FVRx providers held monthly sessions to deliver health coaching. While providers had flexibility in session content and delivery, most were delivered as group sessions. All families received information on healthy nutrition and participated in interactive food demonstrations and goal setting. The child and primary caregiver were required to attend a session to be eligible for monthly vouchers. Other family members, such as grandparents and siblings, were also encouraged to attend to strengthen family health habits.
An evidence-based childhood obesity prevention curriculum, Healthy Habits, Happy Homes, was commonly utilized by providers (35). The original home-based intervention uses motivational interviewing to promote American Academy of Pediatrics (AAP) “5-2-1-0” recommendations for childhood obesity prevention through three modes of delivery: home visits, mailed educational materials and incentives, and weekly text messages (36). In discussion with the program's creators, we retained the core content of MI-based coaching on behavior change delivered by lay health educators. We worked with local providers to adapt sessions so they could be delivered individually (in homes) or in group settings (in a clinic or community settings). We also adapted sessions to the Navajo context based on feedback from trainers and families to: 1) involve children in sessions and goal setting; 2) include Diné foods and language (e.g., Diné children's books as incentives, memory game with Diné words for fruits and vegetables, cooking demonstrations and recipe cards using traditional foods). While FVRx teams were not required to use any specific curriculum, all of the sites represented in this report used Happy Homes.
In order to strengthen the food environment and ensure program success, the FVRx Program also established the following eligibility criteria for participating retailers: a) located on the reservation or, if adjacent to the reservation, strengthens local food systems by stocking local produce and/or traditional foods; and b) stocks a minimum threshold of healthful produce based on adapted Robert Wood Johnson Foundation stocking recommendations for small retail stores (37). To help stores achieve these criteria, COPE implemented the Healthy Navajo Stores Initiative to offer training, technical assistance, supplies, and equipment to increase the availability, quality, and promotion of fresh and frozen produce and traditional foods (38).
Data collection
The Navajo FVRx Program was implemented as standard of care by healthcare teams, and data were collected for program evaluation and quality improvement purposes. Sites administered voluntary surveys to caregivers of child participants at the beginning and end of the program. Data collected included the child's age and gender, household size and participation in the Supplemental Nutrition Assistance Program (SNAP), Women Infants and Children Program (WIC), and Food Distribution Program on Indian Reservations (FDPIR), as well as fruit and vegetable consumption using questions from the Behavioral Risk Factor Surveillance System (39). The surveys asked caregivers to report their child's daily physical activity, sleep, and screen time, and answer the United States Department of Agriculture's (USDA) 6-item short form Food Security Questionnaire (40). Providers collected height and weight at the first and last session.
Outcomes of Interest
We categorized household food security as “secure,” “low food security,” and “very low food security” using thresholds defined by USDA (8). The height and weight were used to calculate BMI, which was subsequently converted to a percentile for age and sex using the CDC Children's BMI Group Calculator US version (41). Weight categories were as follows: underweight, BMI <5th percentile; healthy weight, BMI ≥5th percentile and <85th percentile; overweight: BMI ≥85th percentile and <95th percentile; obese, BMI ≥95 percentile. We also used AAP recommendations for daily fruit and vegetable consumption (≥5 servings/d), physical activity (≥60 min/d), sleep (≥12 h/d for children <1 y old, ≥ 11 h/d for children 3–5 y and ≥9 h/d for children >5 at program initiation), and screen time (<2 h/d) (36). For retention, providers defined a priori a minimum acceptable threshold of ≥4 sessions.
Statistical analyses
Paired t-tests were used to evaluate within-case differences in BMI, the number of servings of fruit and vegetables consumed per day, the number of minutes of physical activity per day, the hours of sleep per night, and the hours of screen time per day. McNemar's tests were conducted to analyze changes in paired nominal data, including food security status and the number of children meeting AAP recommendations for fruit and vegetable consumption and physical activity, sleep, and screen times. All analyses were conducted using Microsoft Excel version 16.17.
Ethical considerations
The FVRx Program and its impact evaluation were carried out under programmatic auspices and not as a research study. Nonetheless, data collection forms and procedures were approved by corresponding health boards, tribal agency councils, and the Navajo Human Research Review Board. Providers were given a written script to obtain verbal consent prior to asking caregivers to complete the surveys. The informed consent requirement for use of personal data for program evaluation was waived.
Results
Program enrollment and retention
Between May 2015 and September 2018, there were 243 Navajo FVRx program participants who met criteria for inclusion in the pediatric group, as shown in Figure1. These participants had a total of 1034 FVRx encounters, including intake, monthly, or exit sessions. Based on reported household size, we estimate that the program reached a total of 1278 beneficiaries. Sixty-five percent of children were retained in the program.
FIGURE 1.
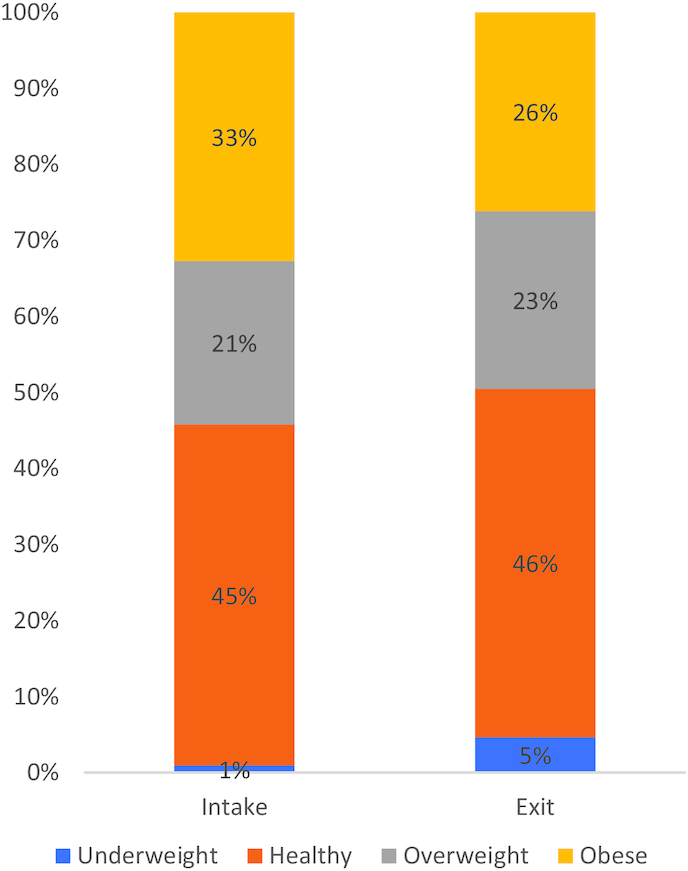
Changes in weight category, n = 107.
Of the 243 children in the pediatric cohort, 31 (13%) were missing intake forms. Of the remaining 212 children with baseline data, 122 completed exit surveys. In this paper, we present baseline characteristics (n = 212) and preprogram to postprogram (pre-post) changes (n = 122) among this FVRx pediatric cohort.
Baseline characteristics
Table 1 displays characteristics of FVRx participants at baseline. The mean ± SD participant age was 3.96 ± 1.87 y, and half the participants were female. Table 2 summarizes household characteristics of the cohort. The median household size was 5 members. The majority of households faced low food security (57%) or very low food security (23%) at baseline. In addition, the majority of households participated in ≥1 food assistance program, with 66% enrolled in the WIC Program. We compared baseline child and household characteristics for participants with only intake data those for participants with both intake and exit data and found no significant differences between the 2 groups at baseline.
TABLE 1.
Baseline characteristics of the FVRx pediatric cohort (n = 212)1
| Cohort values (n = 212) | ||
|---|---|---|
| n (%) | Mean ± SD | |
| Sex | 119 | |
| Male | 59 (50%) | 59 (50%) |
| Female | 60 (50%) | |
| Age, y | 130 | 3.96 ± 1.87 |
| Age category, y | 3.96 ± 1.87 | |
| 0–1 | 11 | |
| >1–2 | 14 | |
| >2–3 | 13 | |
| >3–4 | 24 | |
| >4–5 | 32 | |
| >5–6 | 36 | |
| BMI z score | 151 | 79.9 ± 24.9 |
| Weight category | ||
| Underweight | 2 (1%) | |
| Healthy | 59 (39%) | |
| Overweight | 33 (22%) | |
| Obese | 57 (38%) | |
| Health behavior | ||
| Fruit and vegetable consumption, servings/d | 199 | 5.3 ± 2.3 |
| Fruit, servings/d | 2.6 ± 1.3 | |
| Vegetable consumption, servings/d | 2.8 ± 1.3 | |
| Physical activity, min/d | 168 | 91.3 ± 106.4 |
| Sleep, h/d | 180 | 9.1 ± 8.8 |
| Screen time, h/d | 182 | 2.6 ± 4.4 |
1FVRx, Fruit and Vegetable Prescription Program.
TABLE 2.
Baseline household characteristics of the FVRx pediatric cohort (n = 212)1
| n (%) | Median | |
|---|---|---|
| Household size | 198 | 5 |
| Participation in food assistance programs | 190 | |
| SNAP only | 35 (18%) | |
| WIC only | 28 (15%) | |
| SNAP and WIC | 95 (50%) | |
| FDPIR and WIC | 1 (1%) | |
| None | 31 (16%) | |
| Household food security | 202 | |
| Food secure | 41 (20%) | |
| Low food security | 115 (57%) | |
| Very low food security | 46 (23%) |
1FDPIR, Food Distribution Program on Indian Reservations; SNAP, Supplemental Nutrition Assistance Program; WIC, Women, Infants, and Children.
Health outcomes and behaviors
As shown in Figure 1, among participants with both intake and exit measurements, 54% met criteria for overweight/obese at baseline compared with 49% at follow-up (P > 0.05).
As shown in Table 3, fruit and vegetable consumption increased significantly from 5.2 to 6.8 servings per day, P < 0.001. Likewise, the proportion of participants meeting AAP recommendations for fruit and vegetable consumption increased from 66% at baseline to 82% at follow-up (P < 0.001) (Figure 2). However, there was no significant difference in average daily minutes of physical activity, hours of sleep, or hours of screen time from baseline to follow-up, nor was there a significant change in the proportion of participants meeting AAP recommendations for these activities.
TABLE 3.
Change in health behaviors and health outcomes (n = 122)1
| Variable | n | Baseline | Exit | P value2 |
|---|---|---|---|---|
| Fruit and vegetable consumption, servings/d | 122 | 5.2 ± 2.1 | 6.8 ± 2.2 | <0.001 |
| Fruit consumption, servings/d | 2.7 ± 1.2 | 3.6 ± 1.0 | ||
| Vegetable consumption, servings/d | 2.6 ± 1.2 | 3.3 ± 1.2 | ||
| Physical activity, min/d | 109 | 83.9 ± 103.5 | 108.6 ± 189.4 | 0.25 |
| Sleep, h/d | 107 | 9.3 ± 11.3 | 8.7 ± 2.6 | 0.71 |
| Screen time, h/d | 113 | 2 ± 1.6 | 1.8 ± 1.1 | 0.63 |
| BMI z score | 107 | 77.6 ± 25.5 | 73.06 ± 28.7 | 0.14 |
1Values are means ± SDs unless otherwise indicated.
2Paired t-test.
FIGURE 2.
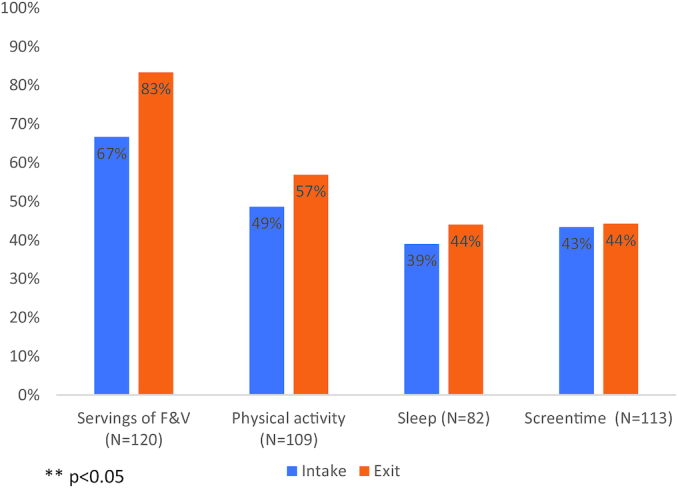
Changes in children meeting AAP recommendations, n = 120. AAP, American Academy of Pediatrics.
Subgroup analysis of children initially classified as overweight/obese
We conducted a subgroup analysis of children with an initial BMI ≥85th percentile to determine if children who were classified as overweight or obese at baseline differed from the study population as a whole with respect to change in BMI and fruit and vegetable consumption (Table 4). Among those children classified as overweight or obese at baseline with pre-post data (n = 58), 38% had a BMI percentile that fell in the healthy range at the end of the program. (Figure 3). The mean BMI percentile among this subgroup significantly decreased from 95.6 to 73.1, P < 0.001. Likewise, average fruit and vegetable consumption increased from 5.3 to 6.9 servings per day, P < 0.001.
TABLE 4.
Changes in health behaviors and health outcomes among children who were overweight or obese at baseline (n = 58)1
| Variable | n | Baseline | Exit | P value2 |
|---|---|---|---|---|
| BMI z score | 58 | 95.6 ± 4.1 | 73.06 ± 28.7 | <0.001 |
| Fruit and vegetable consumption, servings/d | 58 | 5.3 ± 2.5 | 6.9 ± 2.1 | <0.001 |
1Values are means ± SDs unless otherwise indicated.
2Paired t-test.
FIGURE 3.
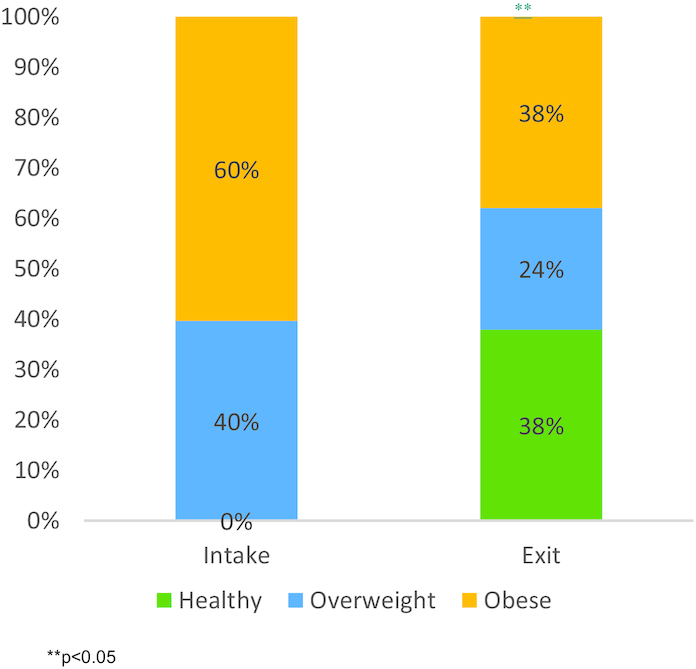
Changes in BMI categories among children classified as overweight or obese at baseline (n = 58).
Household food security
We found that the proportion of households reporting adequate food security also significantly increased from 18% at intake to 35% at program completion (P = 0.001). It is notable, however, that 65% of families remained food insecure at the time of program completion.
Discussion
This report describes the impact of a produce prescription program on health behaviors and health outcomes among young Navajo children. Children enrolled in the program significantly increased their fruit and vegetable consumption, and there was a significant decrease in BMI percentile between baseline and follow-up among children who were initially overweight or obese. The proportion of families facing food insecurity also significantly decreased between baseline and follow-up. These data suggest that produce prescription programs may be an effective intervention to curb childhood overweight and obesity among rural indigenous populations.
Our results corroborate findings from other evaluations of produce prescription programs, which also describe increased fruit and vegetable consumption (24, 25). However, the majority of these programs have been implemented among adult patient populations, often through the use of farmers markets in larger cities. Our findings are consistent with those described by Saxe-Custack et al., who described a significant increase in fruit and vegetable consumption among children in a produce prescription program in Flint, Michigan (27). These findings suggest that produce prescription programs may be an effective healthcare intervention for food-insecure families and could potentially reduce childhood obesity across diverse settings.
Few studies have investigated the impact of produce prescriptions on health outcomes specifically. One study of a program targeting low-income individuals with diabetes found that blood sugar control improved over the course of a 12-week program in which individuals received a stipend ($10/week) for fruits and vegetables (42). However, this evaluation did not detect a change in average blood pressure or weight before and after program participation. Although we did not observe a significant difference in BMI percentile among all children, a subgroup analysis of children who were initially overweight or obese found that more than a third of children returned to a healthy BMI percentile at the end of the 6-mo program, and their average BMI percentile declined from 95.6 to 73.1. Thus, children who are overweight or obese for their age may particularly benefit from enrollment in the Navajo FVRx program and should be considered a priority target population for the intervention.
Although we observed a significant decrease in household food insecurity among participants in the Navajo FVRx program, the level of food insecurity among participants at the end of the program (65%) was still 17 times higher than the US national rate of food insecurity at this time (11.1%) (43). Other studies have highlighted the high rates of food insecurity among children in the Navajo Nation in particular, and there remains a critical need to ensure access to sufficient, safe, and nutritious food at the population level (18). We have previously reported higher rates of fruit and vegetable purchasing at stores participating in the Healthy Navajo Stores Initiative, suggesting that this multilevel intervention could have a community-wide impact on reducing food insecurity by offering a consistent supply of healthier options in small stores serving the rural reservation (32).
We did not observe a change in other health behaviors (screen time, sleep, or physical activity) associated with obesity prevention. Teams that used the Happy Homes curriculum covered these topics. However, we speculate that providers may have emphasized nutrition and diet more than other health habits due to the focus of the FVRx Program.
We acknowledge several limitations involved in this program evaluation. First, because surveys were voluntary, many participants lacked complete data. It is possible that families who completed the surveys were more engaged in the program and thus more likely to have improvements. However, baseline characteristics among families with and those without exit data did not differ significantly. Second, the extent to which improvements in fruit and vegetable consumption, food security, and BMI were sustained after the program remains undetermined. Third, due to the combined nature of the intervention, we were unable to isolate or directly attribute the observed changes to vouchers, FVRx nutrition education, or the combination of both. While the proportion of underweight children changed from 1% to 4%, this change was statistically significant; future program efforts should monitor for excessive weight loss. Given the intentional decision to implement a multilevel intervention, we were more interested in understanding the program's impact in its entirety, rather than teasing out the relative contribution of specific programmatic elements. Future efforts could include evaluating changes in health outcomes among adult family members and analysis of site-based variations associated with greater impact. Last, reliance on self-reported health behavior may have subjected our results to social desirability bias. However, because the analysis examined within-case differences, it is unlikely that any inflation or deflation in these measures substantially impacted results. Longer follow-up could assess if improvements in health behaviors and health outcomes are sustained.
In sum, this program evaluation of a cross-sector, multilevel produce prescription program—comprising vouchers, health coaching, and store support—resulted in increased fruit and vegetable consumption in children >7 y of age. Among children who were initially overweight or obese, 38% achieved a healthy weight after 6 mo. These findings suggest that produce prescription programs can be effectively implemented in a rural, indigenous community to address the burden of pediatric overweight and obesity. Future evaluation should include process and long-term follow-up data to contextualize and interpret outcome data and to understand if health outcomes and population-level impacts are sustained over time.
ACKNOWLEDGEMENTS
We acknowledge the many important contributions from Navajo Area Indian Health Service /638 clinic sites and providers, Navajo Department of Health programmes, and family participants in the development of the Navajo FVRx Programme.
Authors’ contributions were as follows––LJB, KT, JVWP, AS, ACW, LH, CG, MGB, TW, MT, EE, SMS, GG, SSS: designed research; LJB, LT, JVWP, EQZ, LK, AS, ACW, LH, CG, SSS: conducted research; JVWP, CB: analyzed data or performed statistical analysis; LJB, KVWP, SSS: wrote the paper; LJB, KVWP, SSS, CB: had primary responsibility for final content; LK: shared findings with patient advisors and solicited feedback; and all authors: read and approved the final manuscript.
Notes
Funding was made possible (in part) by a cooperative agreement with the US Centers for Disease Control and Prevention (#5NU58DP005872). The opinions expressed do not necessarily reflect the official views of the Indian Health Service or policies of the Department of Health and Human Services, nor does the mention of trade names, commercial practices, or organizations imply endorsement by the US Government. This work was also supported by the Notah Begay III Foundation (NB3F), the Rx Foundation, the Zegar Family Foundation, and the Leonard Family Foundation.
Author disclosures: The authors report no conflicts of interest.
Abbreviations used: AAP, American Academy of Pediatrics; AI/AN, American Indian and Alaska Native; COPE, Community Outreach and Patient Empowerment; FDPIR, Food Distribution Program on Indian Reservations; FVRx, Fruit and Vegetable Prescription Program; pre-post, preprogram to postprogram; SNAP, Supplemental Nutrition Assistance Program; WIC, Women, Infants, and Children Program
Contributor Information
Leandra J Jones, Community Outreach and Patient Empowerment Program, Gallup, New Mexico.
Joan VanWassenhove-Paetzold, Community Outreach and Patient Empowerment Program, Gallup, New Mexico; Partners In Health, Boston, Massachusetts.
Kymie Thomas, Community Outreach and Patient Empowerment Program, Gallup, New Mexico.
Carolyn Bancroft, Community Outreach and Patient Empowerment Program, Gallup, New Mexico.
E Quinn Ziatyk, Chinle Comprehensive Health Care Facility, Chinle, Arizona.
Lydia Soo-Hyun Kim, Northern Navajo Medical Center, Shiprock, New Mexico.
Ariel Shirley, Community Outreach and Patient Empowerment Program, Gallup, New Mexico.
Abigail C Warren, Community Outreach and Patient Empowerment Program, Gallup, New Mexico.
Lindsey Hamilton, Community Outreach and Patient Empowerment Program, Gallup, New Mexico.
Carmen V George, Community Outreach and Patient Empowerment Program, Gallup, New Mexico; Partners In Health, Boston, Massachusetts; Division of Global Health Equity, Brigham and Women's Hospital, Boston, Massachusetts.
Mae-Gilene Begay, Navajo Nation Community Health Representative Outreach Program, Navajo Department of Health, Window Rock, Arizona.
Taylor Wilmot, Community Outreach and Patient Empowerment Program, Gallup, New Mexico; Partners In Health, Boston, Massachusetts.
Memarie Tsosie, Community Outreach and Patient Empowerment Program, Gallup, New Mexico.
Emilie Ellis, Community Outreach and Patient Empowerment Program, Gallup, New Mexico; Partners In Health, Boston, Massachusetts.
Sara M Selig, Community Outreach and Patient Empowerment Program, Gallup, New Mexico; Partners In Health, Boston, Massachusetts; Division of Global Health Equity, Brigham and Women's Hospital, Boston, Massachusetts.
Gail Gall, Community Outreach and Patient Empowerment Program, Gallup, New Mexico.
Sonya S Shin, Email: sshin@bwh.harvard.edu, Community Outreach and Patient Empowerment Program, Gallup, New Mexico; Partners In Health, Boston, Massachusetts; Northern Navajo Medical Center, Shiprock, New Mexico.
References
- 1. Story M, Strauss KF, Zephier E, Broussard BA. Nutritional concerns in American Indian and Alaska Native children: transitions and future directions. J Am Diet Assoc. 1998;98(2):170–6. [DOI] [PubMed] [Google Scholar]
- 2. Bullock A, Sheff K, Moore K, Manson S. Obesity and overweight in American Indian and Alaska Native children, 2006-2015. Am J Public Health. 2017;107(9):1502–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kelsey MM, Zaepfel A, Bjornstad P, Nadeau KJ. Age-related consequences of childhood obesity. Gerontology. 2014;60(3):222–8. [DOI] [PubMed] [Google Scholar]
- 4. Fagot-Campagna A, Pettitt DJ, Engelgau MM, Burrows NR, Geiss LS, Valdez R, Beckles GL, Saaddine J, Gregg EW, Williamson DF et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J Pediatr. 2000;136(5):664–72. [DOI] [PubMed] [Google Scholar]
- 5. Dabelea D, Hanson RL, Bennett PH, Roumain J, Knowler WC, Pettitt DJ. Increasing prevalence of Type II diabetes in American Indian children. Diabetologia. 1998;41(8):904–10. [DOI] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention (CDC) Diagnosed diabetes among American Indians and Alaska Natives aged <35 years–United States, 1994–2004. MMWR Morb Mortal Wkly Rep. 2006;55(44):1201–3. [PubMed] [Google Scholar]
- 7. Pavkov ME, Hanson RL, Knowler WC, Bennett PH, Krakoff J, Nelson RG. Changing patterns of type 2 diabetes incidence among Pima Indians. Diabetes Care. 2007;30(7):1758–63. [DOI] [PubMed] [Google Scholar]
- 8. Nord M, Andrews M, Carlson S. Household food security in the United States, 2005. [Internet] Washington: USDA Economic Research Service; 2005; [cited Nov 27, 2017]. Report No.: ERR-29. https://www.ers.usda.gov/webdocs/publications/45655/29206_err29_002.pdf?v=41334[PDF – 880 KB]. Accessed February 17, 2020. [Google Scholar]
- 9. Berryhill K, Hale J, Chase B, Clark L, He J, Daley CM. Food security and diet among American Indians in the Midwest. J Community Health. 2018;43(5):901–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jernigan VBB, Huyser KR, Valdes J, Simonds VW. Food insecurity among American Indians and Alaska Natives: a National profile using the current population survey-food security supplement. J Hunger Environ Nutr. 2017;12(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mullany B, Neault N, Tsingine D, Powers J, Lovato V, Clitso L, Massey S, Talgo A, Speakman K, Barlow A. Food insecurity and household eating patterns among vulnerable American-Indian families: associations with caregiver and food consumption characteristics. Public Health Nutr. 2013;16(4):752–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bauer KW, Widome R, Himes JH, Smyth M, Rock BH, Hannan PJ, Story M. High food insecurity and its correlates among families living on a rural American Indian Reservation. Am J Public Health. 2012;102(7):1346–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Receveur O, Boulay M, Kuhnlein HV. Decreasing traditional food use affects diet quality for adult Dene/Metis in 16 communities of the Canadian Northwest Territories. J Nutr. 1997;127(11):2179–86. [DOI] [PubMed] [Google Scholar]
- 14. Murphy NJ, Schraer CD, Thiele MC, Boyko EJ, Bulkow LR, Doty BJ, Lanier AP. Dietary change and obesity associated with glucose intolerance in Alaska Natives. J Am Diet Assoc. 1995;95(6):676–82. [DOI] [PubMed] [Google Scholar]
- 15. Kumar G, Jim-Martin S, Piltch E, Onufrak S, McNeil C, Adams L, Williams N, Blanck HM, Curley L. Healthful nutrition of foods in Navajo Nation stores: availability and pricing. Am J Health Promot. 2016;30(7):501–10. [DOI] [PubMed] [Google Scholar]
- 16. Willows ND, Hanley AJ, Delormier T. A socioecological framework to understand weight-related issues in Aboriginal children in Canada. Appl Physiol Nutr Metab. 2012;37(1):1–13. [DOI] [PubMed] [Google Scholar]
- 17. Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, Armstrong R, Prosser L, Summerbell CD. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;7(12):CD001871. [DOI] [PubMed] [Google Scholar]
- 18. Mayer K. Childhood obesity prevention: focusing on the community food environment. Fam Community Health. 2009;32(3):257–70. [DOI] [PubMed] [Google Scholar]
- 19. Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, James WP, Wang Y, McPherson K. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385(9986):2510–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sundberg MA, Warren AC, VanWassenhove-Paetzold J, George C, Carroll DS, Becenti LJ, Martinez A, Jones B, Bachman-Carter K, Begay MG et al. Implementation of the Navajo fruit and vegetable prescription programme to improve access to healthy foods in a rural food desert. J Public Health Nutrition. 2020;1–12. Doi: 10.1017/S1368980019005068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Aiyer JN, Raber M, Bello RS, Brewster A, Caballero E, Chennisi C, Durand C, Galindez M, Oestman K, Saifuddin M et al. A pilot food prescription program promotes produce intake and decreases food insecurity. Transl Behav Med. 2019;9(5):922–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bihan H, Méjean C, Castetbon K, Faure H, Ducros V, Sedeaud A, Galan P, Le Clésiau H, Péneau S, Hercberg S. Impact of fruit and vegetable vouchers and dietary advice on fruit and vegetable intake in a low-income population. Eur J Clin Nutr. 2012;66(3):369–75. [DOI] [PubMed] [Google Scholar]
- 23. Hanbury MM, Gomez-Camacho R, Kaiser L, Sadeghi B, de la Torre A. Purchases made with a fruit and vegetable voucher in a rural Mexican-heritage community. J Community Health. 2017 Oct;42(5):942–8. [DOI] [PubMed] [Google Scholar]
- 24. Trapl ES, Smith S, Joshi K, Osborne A, Benko M, Matos AT, Bolen S. Dietary impact of produce prescriptions for patients with hypertension. Prev Chronic Dis. 2018;15:E138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Herman DR, Harrison GG, Jenks E. Choices made by low-income women provided with an economic supplement for fresh fruit and vegetable purchase. J Am Diet Assoc. 2006;106(5):740–4. [DOI] [PubMed] [Google Scholar]
- 26. Saxe-Custack A, LaChance J, Hanna-Attisha M. Child consumption of whole fruit and fruit juice following six months of exposure to a pediatric fruit and vegetable prescription program. Nutrients. 2019;12(1):E25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Navajo Epidemiology Center Navajo Population Profile: 2010 U.S. Census. Window Rock, AZ: Navajo Department of Health; 2013. https://www.nec.navajo-nsn.gov/Portals/0/Reports/NN2010PopulationProfile.pdf. Accessed May 3, 2020. [Google Scholar]
- 28. Navajo Department of Economic Development Navajo Nation Fast Facts. http://navajobusiness.com/fastFacts/Overview.htm. Accessed January 4, 2020. [Google Scholar]
- 29. United States Department of Agriculture Access to affordable and nutritious food: measuring and understanding food deserts and their consequences. 2009. https://www.ers.usda.gov/webdocs/publications/42711/12716_ap036_1_.pdf?v=0. Accessed February 17, 2020. [Google Scholar]
- 30. USDA Food Access Research Atlas. http://www.ers.usda.gov/data-products/food-access-research-atlas/go-to-the-atlas.aspx#.U-xcQGPE4lI. Accessed June 3, 2016. [Google Scholar]
- 31. Pardilla M, Prasad D, Suratkar S, Gittelsohn J. High levels of household food insecurity on the Navajo Nation. Public Health Nutr. 2014;17(1):58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wholesome Wave The Fruit and Vegetable Prescription Program. 2016; https://www.wholesomewave.org/how-we-work/produce-prescriptions. Accessed January 21, 2020. [Google Scholar]
- 33. Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, Ettinger de Cuba SA, Casey PH, Chilton M, Cutts DB et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):26–32. [DOI] [PubMed] [Google Scholar]
- 34. Indian Health Services Food Insecurity Assessment Tool and Resource List. https://www.ihs.gov/MedicalPrograms/Diabetes/HomeDocs/Resources/InstantDownloads/FoodInsecurityAssessTool.pdf. Accessed January 4, 2020. [Google Scholar]
- 35. Haines J, McDonald J, O'Brien A, Sherry B, Bottino CJ, Schmidt ME, Taveras EM. Healthy Habits, Happy Homes: randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatr. 2013;167(11):1072–9. [DOI] [PubMed] [Google Scholar]
- 36. AAP Updates Recommendations on Obesity Prevention: it's never too early to begin living a healthy lifestyle. 2015. https://www.aap.org/en-us/about-the-aap/aap-press-room/pages/AAP-Updates-Recommendations-on-Obesity-Prevention-It%27s-Never-Too-Early-to-Begin-Living-a-Healthy-Lifestyle.aspx. Accessed February 17, 2020. [Google Scholar]
- 37. Laska M, Pelletier J. Minimum stocking levels and marketing strategies of healthful foods for small retail food stores. Minneapolis, MN: Healthy Eating Research, Robert Wood Johnson Foundation; 2016. Report No.: 1088. [Google Scholar]
- 38. MacKenzie OW, George CV, Pérez-Escamilla R, Lasky-Fink J, Piltch EM, Sandman SM, Clark C, Avalos QJ, Carroll DS, Wilmot TM et al. Healthy stores initiative associated with produce purchasing on Navajo Nation. Curr Dev Nutr. 2019;3(12):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA; 2013. https://www.cdc.gov/brfss/questionnaires/index.htm. Accessed May 3, 2020. [Google Scholar]
- 40. Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the Household Food Security Scale. Am J Public Health. 1999;89:1231–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Centers for Disease Control and Prevention Children's BMI Tools for School. https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/tool_for_schools.html. Accessed May 3, 2020. [Google Scholar]
- 42. Bryce R, Guajardo C, Ilarraza D, Milgrom N, Pike D, Savoie K, Valbuena F, Miller-Matero LR. Participation in a farmers' market fruit and vegetable prescription program at a federally qualified health center improves hemoglobin A1C in low income uncontrolled diabetics. Prev Med Rep. 2017;7:176–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. USDA Economic Research Service Key Statistics & Graphics. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics.aspx. Accessed February 17,2020. [Google Scholar]


