Abstract
Introduction
Traditionally, health care delivery in the USA has been structured around in-person visits. The COVID-19 pandemic has forced a shift to virtual care models in order to reduce patient exposure to high-risk environments and to preserve valuable health care resources. This report describes one large primary care system’s model for rapid transition to virtual care (RTVC).
Setting and Participants
A RTVC model was implemented at the VA Connecticut Health Care System (VACHS), which delivers care to over 58,000 veterans.
Program Description
The RTVC model included immediate virtual care conversion, telework expansion, implementation of virtual respiratory urgent care clinics, and development of standardized note templates.
Program Evaluation
Outcomes include the rates of primary encounter types, staff teleworking, and utilization of virtual respiratory urgent care clinics. In under 2 weeks, most encounters were transitioned from in-person to virtual care, enabling telework for over half of the medical staff. The majority of virtual visits were telephone encounters, though rates of video visits increased nearly 18-fold.
Discussion
The RTVC model demonstrates expeditious and sustained transition to virtual care during the COVID-19 pandemic. Our experiences help inform institutions still reliant on traditional in-person visits, and future pandemic response.
KEY WORDS: virtual care, COVID-19, prevention, pandemic, primary care
INTRODUCTION
The COVID-19 pandemic presents fundamental challenges to health care delivery, with an impetus to shift to virtual care in the outpatient setting in order to reduce patient and health care worker exposure to high-risk environments and to preserve valuable health care resources.
Despite mechanisms for reimbursing telemedicine and recent increasing trends in telemedicine visits, care in the USA has been predominantly structured around in-person visits.1 Data from 2018 show telehealth utilization rates of 0.95% (9.5 visits per 1000 beneficiaries) in the Medicare program2 and 1.13% (11.3 users per 1000 enrollees) in an all-payer database.3 Veterans Affairs (VA) data (averaged from October 2019 through February 2020) show that 4.2% and 0.68% of all appointments were telephone visits and video visits, respectively.4
The in-person model has shortcomings: optimal care can often be delivered without requiring patients to be physically present in clinic. This includes preventive care, chronic disease follow-up, and goals of care discussions. In addition, in-person care may be costly and time consuming, especially for those with poor transportation access, significant mobility limitation, or who live in remote areas.
The COVID-19 pandemic has provided an urgency to shift to virtual care (including telephone visits, video visits, and secure messaging) as a public health strategy. Current data suggest that medical facilities are high-risk environments for disease transmission for both patients and health care workers.5–8 The shift from in-person to virtual care has been driven by the premise that this may reduce disease transmission, maintain the safety of the health care work force, reduce burden to emergency rooms/urgent care centers, and conserve personal protective equipment. We aim to describe the VA Connecticut Primary Care Rapid Transition to Virtual Care (RTVC) model and to review early data regarding this practice shift.
SETTING/PARTICIPANTS
The VA Connecticut Health Care System (VACHS) consists of eight primary care sites, including a major tertiary care medical center with specialty, emergency, and hospital care; a smaller medical center with full ambulatory services; and six community-based outpatient clinics (CBOCs) with primary and mental health care only. There are 80 individual primary care providers delivering care to 58,058 veterans.
PROGRAM DESCRIPTION
The VA Health Care System is uniquely positioned to rapidly implement virtual care as a public health strategy. First, the VA cares for an older patient population, with multiple complex comorbidities,9 the population for whom COVID-19 presents the highest risk. Thus, efforts to maintain provision of care while preventing exposure to high-risk environments may have a potent benefit. Second, the VA is an early adopter of virtual care delivery. While the VA is a federally funded system not beholden to fee-for-service pressures, budgeting is still dependent on documentation of workload. Over the past 5 years, the VA has provided workload credit and incentivized its providers (via pay for performance) for the use of telephone visits, video visits, and secure messaging. Finally, the VA’s hierarchical structure, organized in specified geographic units, with clear chains of command, allows for rapid deployment of best practices.
Below, we describe VA Connecticut’s Primary Care Rapid Transition to Virtual Care (RTVC) model and deployment timeline.
Phase 1
Immediate conversion of in-person visits to virtual visits, and expansion of staff teleworking. All primary care patient-aligned care teams (PACT) (typically consisting of a primary care provider (PCP), an RN, and medical support staff) were mandated to immediately review upcoming schedules to determine the most appropriate modality of care, advise patients against in-person care unless clinically necessary, and offer either video or telephone replacement visits. Critical face-to-face needs were addressed with PCP approval, with efforts made to coordinate any necessary care with other services. This phase of the RTVC model also included establishing home telework rotations for primary care providers, nurses, and support personnel. Clinics remained staffed by those “on site,” with maintenance of adequate personnel to address in-person patient needs. Telework and video care were supported via virtual mandatory online training and peer-to-peer and informatics support. Once virtual care transition was successfully implemented, all CBOCs were closed to in-person visits, while remaining open for telephone and video care.
Phase 2
Virtual respiratory urgent care clinics were created to support increased demand for care, staffed by licensed independent practitioners (LIPs). These were VACHS primary care provider volunteers who did this in addition to taking care of their own patient panel. These clinics provided expeditious telephone or video assessment of patients symptomatic with respiratory complaints or other symptoms concerning for COVID-19, when usual primary care teams were not immediately accessible. To accommodate rapidly increasing volume, access was quickly increased from one clinic per day to three clinics per day.
Virtual assessment was standardized via development of new COVID-19 note templates to guide assessment and medical decision-making, inform patients of test results, and counsel around isolation and return to work. Templates were updated regularly to align with CDC recommendations. Additionally, an LIP after-hours call system was adopted, also staffed by volunteer primary care providers to ensure COVID-19-positive test results were addressed expeditiously.
Concurrent to VA Connecticut primary care deployment of the RTVC model, the VA launched a broad campaign emphasizing the importance of virtual care. All VA Connecticut veterans were sent frequent communication around COVID-19, including the “Phone and Stay Home campaign”, through use of mail, secure messaging, and text messaging platforms.
PROGRAM EVALUATION
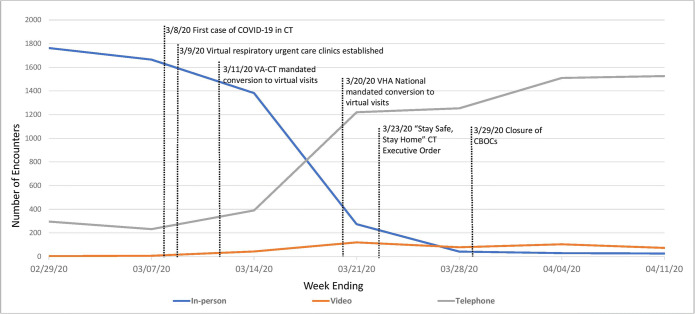
Results of the RTVC model deployment are shown in Figure 1, demonstrating the number of completed primary care encounters over time by encounter type. Sentinel epidemiological events and interventions related to RTVC deployment are also depicted. Within 2 weeks of the first confirmed COVID-19 case in Connecticut, and by the time the VA mandated transition to virtual care, 83% of all primary care visits at VACHS were completed through virtual care modalities. Three weeks after the first case in Connecticut, 97% of all primary care visits were virtual encounters.
Figure 1.
Run chart model of encounters by care delivery modality for all VA Connecticut primary care provider clinics. Identifies differences in modality trends in response to onset of COVID-19 cases and VA National, VA Connecticut and State interventions. VA Connecticut primary care encounter trends.
Though not shown, encounter trends were also assessed for each physical primary care site across VA Connecticut and reveal a consistent shift to virtual care despite varied clinic settings and populations. Rates of inbound and outbound secure messaging were also evaluated for the months of February 2020 and March 2020, demonstrating an increase of 51% and 41% for inbound and outbound messages, respectively.
In order to preserve a healthy workforce, the percent of primary care staff teleworking during this timeframe increased from zero at baseline to 59% for the pay-period of March 29, 2020–April 11, 2020. Utilization rates of the virtual respiratory urgent care clinics were also evaluated. The utilization rate for the telephone urgent care clinics was 90% of appointment slots for the first week after implementation. Utilization rates of this clinic then dropped linearly over time: from 78% the second week, to 47% the third week, to 51% the fourth week, to 38% the fifth week, to 18% 6 weeks after initiation.
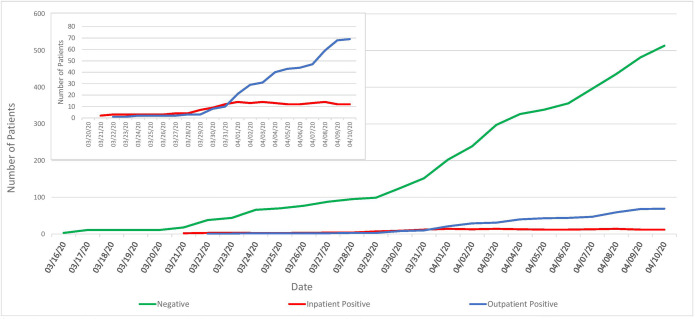
The numbers of confirmed positive COVID-19 outpatient cases and patients hospitalized for COVID-19-related illness in the VACHS are shown in Figure 2.
Figure 2.
Run chart model of COVID-19 test results by patient status used to identify disease trends and testing prevalence. COVID-19 testing VA Connecticut.
DISCUSSION
In this report, we described the deployment of a phased model to shift primary care delivery to telehealth at a large VA primary care health system in response to the COVID-19 pandemic. In under 2 weeks, the majority of encounters were transitioned from in-person to virtual care. This shift enabled telework outside of the hospital/clinic setting for over half of the medical staff. Though virtual care visits were offered before implementation of the RTVC model, the dramatic shift in encounters occurred only after telehealth transition was mandated, with in-person visits approved only at the discretion of the PCP. Despite this significant shift, we see stability in the total number of encounters, suggesting that the telehealth model sustains care in times where in-person visits present unacceptably high risks for patients. A similar shift to virtual care in a large non-VA primary care practice during the COVID-19 pandemic has been described,10 suggesting that this model may be applicable outside of the VA (although current fee-for-service reimbursement models may de-incentivize virtual care).
Most in-person visits were replaced by telephone visits. While video visits remained a small minority of total encounters, it is important to note that video visits increased nearly 18-fold: average rates of video visits 5 weeks before and after transition increased from 0.30 to 5.27% of all encounters.
As part of the RTVC model, virtual respiratory urgent care clinics were established to enhance access to care, as primary care teams were adapting to telehealth and telework rotations, and there was an immediate need to rapidly assess patients with possible COVID-19 symptoms. These “extra” clinics had high utilization rates, especially during the early phase of the transition to virtual care, with 80–90% of appointment slots being filled during the first 2 weeks of transition. Providing rapid access to virtual care for patients requiring evaluation for COVID-19 prevented in-person encounters, with attendant PPE use and risk for disease transmission.
The fact that nearly all visits were successfully transitioned to virtual care confirms that most patients and providers are capable of navigating replacement visits and willing and able to engage in this type of care modality during the COVID-19 pandemic. The predominance of virtual visits was telephone rather than video encounters; barriers to video visits included software that required many steps to schedule video encounters and a non-intuitive interface for patients, limiting uptake. We found that nearly all our patients had access to a phone, though many did not have a smartphone or the ability to easily use the VA’s video platform.
There were also practical challenges in obtaining vital signs, with some patients not having access to thermometers, blood pressure monitors, and pulse oximeters; the ability to physically examine patients was obviously limited. Omission of the physical exam in certain clinical scenarios may have resulted in missed diagnoses. We also encountered additional barriers around communication, including hearing and vision impairment.
As states implement plans for “reopening,” and medical clinics begin to offer more in-person care, further studies will be needed to define the optimal balance of care delivery.
It will be crucial to systematically assess whether transitioning to virtual care reduces transmission of COVID-19 to patients and among the health care workforce. Additionally, it will be important to evaluate the impact of primary care telemedicine on emergency room and inpatient utilization, and quality of care metrics and clinical outcomes. Assessment of patient/provider preferences and satisfaction is also needed. Much work remains to be done to match individual patient needs with the safest and most effective visit modality. Finally, for virtual care to be sustainable, reimbursement models must be sufficient to allow providers to remain solvent.
The COVID-19 pandemic has forced a dramatic shift in how health care is delivered, and an important “silver lining” of this crisis is that it has triggered a rethinking of the optimal balance of care-delivery modalities.
Acknowledgments
The authors thank the following: Joan M Amatruda, Kris Azu, Lorraine Binns-Grear, Deborah Bjorklund, Lucille Burgo, Eugene Constantinou, Cory Curley, Donald Curran, Vivian DeJesus, Carl Dillon, Sheryl Ford, Seonaid Hay, Diane Knight, Elizabeth Lopes, Arleen Nieves, Wanda Pannell-Mitchell, Sandra Ramos, Samuel Rice, Kimberley Roy, Aysha Saeed, Jaqueline Satchell, Monique Simmons, Mark Thompson, Rhynishka Whyte, Kristina Cavallaro, Esterina Anderson, Susan Maya, Douglas Spelman, David Levy.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in Telemedicine Use in a Large Commercially Insured Population, 2005-2017. JAMA. 2018;320(20):2147–2149. doi: 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medicare payment advisory commission. Report to Congress: MEDPAC. March 2018. Page 484, Figure 16-1. Available at: http://www.medpac.gov/docs/default-source/reports/mar18_medpac_entirereport_sec.pdf. Accessed 10 April 2020.
- 3.Yu J, Mink PJ, Huckfeldt PJ, Gildemeister S, Abraham JM. Population-Level Estimates of Telemedicine Service Provision Using An All-Payer Claims Database. Health Affairs. 2018;37(12):1931–1939. doi: 10.1377/hlthaff.2018.05116. [DOI] [PubMed] [Google Scholar]
- 4.VHA support service center (VSSC) database. 2020. Available at:https://vssc.med.va.gov. Accessed 16 April 2020.
- 5.CDC MMWR. COVID-19 in a long-term care facility, Kings County, Washington. February 27-March 9 2020. MMWR weekly. March 26;69(12):339-342. [DOI] [PMC free article] [PubMed]
- 6.Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? The Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwartz J, King C-C, Yen M-Y. Protecting Healthcare Workers During the Coronavirus Disease 2019 Outbreak: Lessons from Taiwan’s Severe Acute Respiratory Syndrome Response. Clinical infectious diseases, brief report, 2020; ciaa255.doi.org IDSA. 3/12/20, in press. [DOI] [PMC free article] [PubMed]
- 9.Agha Z, Lofren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252–3257. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- 10.Mehrotra A, Ray K, Brockmeyer DM, Barnett ML, Bender JA. Rapidly Converting to “Virtual Practices”: Outpatient Care in the Era of COVID-19. NEJM Catalyst, Innovations in Care Delivery. April 1, 2020.