Abstract
Inequity and health disparities can be exacerbated as a result of gentrification when long-term residents are displaced, or remain but are not able to take advantage of new opportunities. The disappearance of old and emergence of new food establishments may increase the proximity to and density of healthy food options, however, affordability and consumption of healthy food, nor a decrease in risk of adverse health outcomes are not guaranteed. Our study aims to understand the relationship between gentrification, neighborhood food environment, and childhood obesity. We describe food opportunities changes in New York City using National Establishments Time Series Database stratified by gentrification status. Using data from the Columbia Center for Children’s Environmental Health birth cohort study, we evaluate the impact of the area-level changing food chances on the body mass index z-scores of children at age five. Overall, gentrifying neighborhoods have the highest number of food chances and experience the most substantial increase in both healthy (p < 0.001) and unhealthy (p < 0.001) food chances between 1990–2010. After adjusting for covariates, higher access to healthy food chances was associated with both lower BMI z-score (p < 0.01) and less likelihood of being overweight or obese (p < 0.001) for five-year-old children. Our results suggest gentrification was associated with contemporaneous changes in the neighborhood food chances in NYC and children exposed to greater healthy foods experienced a lower probability of excess body weight by five years old. Further research is needed to understand other potential pathways connecting gentrification to childhood BMI.
Keywords: Food environment, childhood obesity, gentrification, New York City
Introduction
In the United States over the last five decades, the percentage of children and adolescents affected by obesity has more than tripled (1). Nationally, nearly 1 in 5 school age children and young people (6–19 years) is obese. These trends are similar in New York City, where almost half of elementary school children and Head Start children are not at a healthy weight (2). Obesity prevalence also impacts the very young; 1 in 5 kindergarten students, and 1 in 4 Head Start children (birth to age five), are obese (2). Adults and children who are overweight are at increased risk for diabetes, heart disease, stroke, high blood pressure, arthritis, and some cancers (3). Marginalized communities bear a disproportionate share of the burden of obesity and related health conditions, i.e., diabetes (4,5). Given that obesity begins early in life (6), childhood obesity has immediate and long-term effects on physical, social, and emotional health; the gravity of this public health issue is of great concern.
Obesity results from an imbalance of energy consumption and expenditure. The food environment provides the key ingredient in the energy equation -- the energy. The availability (5,7–10), accessibility (11,12) and proximity (13–15) of healthy and unhealthy food purchasing and consumption opportunities (9,15,16) have been associated with obesity. Also, food prices and food affordability are influential determinants of the food choices, and therefore determinants of obesity, and other metabolic chronic diseases (17–19).
The influx of investment that accompanies gentrification, reinvestment of capital, social upgrading of locale by incoming affluent groups, and landscape change, results in direct or indirect displacement of low-income groups (20). Gentrification also brings a change in the urban food environment, affecting the access to and availability of various forms of food and beverages, grocery stores, restaurants, large big-box stores, farmer’s markets, bodegas, and other food establishments (21–25). Recent studies have indicated that shifts in the food environment in the United States (US) are transforming urban centers (11,13,26) from food deserts (i.e., low-income areas where a significant number of residents are located more than one mile from a supermarket) (27) to areas with abundant food options, including fresh food markets and sit-down restaurants. Breyer and colleagues report that the growing abundance of food options does not necessarily correlate with increased consumption of healthy foods for all residents. They posit that while healthy food options appear plentiful, healthy foods are economically inaccessible for socioeconomically marginalized households (28). Healthy foods closer to home does not guarantee these healthful foods reach the tables of marginalized residents. Breyer and colleagues (28) state this type of disconnect is most stark in gentrifying neighborhoods.
The food-related opportunities shaped by gentrification and residents’ associated food choices can be described regarding the sociological concept of habitus that links structural factors to individual behavior or practices (29). “Food habitus” can be thought of as a set of dispositions and tastes towards food that account for food and nutrition-related practices that become apparent in an individual’s body, including one’s weight (30). Thus, food habitus represents the dialectical relationship between the individual’s food-related choices and the opportunities afforded by the food environment. Insights to obesogenic environments can be illuminated by focusing on the interplay between the structural opportunities, or food chances (i.e., chance to purchase and consume food), that exist within the food ecology and individual-level food choices. Understanding the trends in the food environment is integral to addressing whether shifts in capital investments and shifts in the demographic composition of the neighborhood as a consequence of gentrification has an impact on the long-term health of residents.
This project focuses on the structural opportunities within New York City’s (NYC) food environment. We examined associations between obesity measures of five-year-old children and 1) neighborhood healthy food chances 2) neighborhood unhealthy food chances 3) neighborhood gentrification status during 1990–2010 in NYC. Secondarily, the relationship between gentrification and food chances was examined, to provide greater context to the relationship between obesity measures and the neighborhood food environment.
Methods
The project involves secondary longitudinal data analyses that integrates information from the Columbia Center for Children’s Environmental Health’s (CCCEH) prospective birth cohort, National Time-Series Establishments Database (NETS), New York University Furman Center, and New York City Department of Planning Community District Profiles. This work aims to evaluate the role of gentrification and food environment in the cycle of children’s environmental health disparities, specifically obesity. The combination of these data sources provided the opportunity to examine how participants’ neighborhood food environment influence the weight of children in the context of gentrification. The Institutional Review Board at Columbia University Medical Center approved research protocols related to CCCEH and NETS.
Participants
CCCEH has conducted a longitudinal birth cohort study beginning in 1998 that has been described extensively elsewhere (31,32). Briefly, CCCEH enrolled 727 women ages 18–35 years old during their third trimester of pregnancy. Women were included if they self-identified as either African American or Dominican and resided in Northern Manhattan or the South Bronx for at least one year before pregnancy. Exclusion criteria included mother’s report of cigarette smoking or use of other tobacco products during pregnancy, illicit drug use, diabetes, hypertension, known HIV, or a first prenatal visit after the 20th week of gestation. Research staff abstracted medical records of mother and infant at delivery to ascertain prenatal medical history and birth outcomes. Mother-child dyads participate in follow-up visits every three months throughout the first two years and annually thereafter.
During the follow-up visit of five-year-olds, body size measurements (weight and height) were collected (n=486). Children were measured in bare or stocking feet while wearing light clothing (i.e., pediatric gown, underwear, or shorts and a t-shirt). Weight was assessed using a digital scale.
A Detecto Cardinal 750 digital scale/stadiometer (Cardinal Scale Manufacturing Company) was used to collect standing height measurements until January 2010. After January 2010, CCCEH researchers assessed standing height with the Holtain-Harpenden Wall Mounted Stadiometer Counter 602VR (Holtain Limited). Body mass index z-scores (BMIZ) were quantified using the SAS programs provided by the CDC (33). According to the CDC child growth charts, the overweight category is defined as BMI 85th to less than the 95th percentile while obese is defined as 95th percentile or greater for age and sex. The mothers’ weight before pregnancy was self-reported during the third trimester.
New York City food environment and gentrification
The NETS database (Dun and Bradstreet data from January of each year to create an annual census of businesses and many nonprofit and government agencies) (34–36) was used to develop a food environment measure for each sub-borough areas (SBA; geographical unit similar to community district) in NYC for each year from 1990–2010. Kaufman and colleagues (37) recently analyzed NETS to measure health-relevant business over the same 21-year time span in the NYC metropolitan area. Of the 25 categories defined by the research team, 13 relate to food establishments. Aggregate level data for unhealthy and healthy food chances are the central interest in our analyses. Unhealthy food chances are defined as fast food restaurants, pizza restaurants, bakeries and candy/confectionary stores, meat markets, and corner store/deli often described as “bodegas.” Convenience stores were not included in the aggregate measure because corner stores represent this category in NYC. Healthy food chances are defined as fruit and vegetable markets, natural food markets and nut stores, fish markets, small grocery stores, and large supermarkets. Our analyses operationalized the food environment by the average food chances per square kilometer. To increase accuracy, bodies of water are excluded from the area of the neighborhoods.
Second, we used the Furman Center of New York University (38) gentrification classification system to measure gentrification status of NYC’s neighborhoods during the same period that food chances were estimated (1990–2010). In brief, the criteria defining the classification systems relate to the median income of the neighborhood in 1990 and the median rent growth between 1990–2014. NYC is comprised of 55 SBAs. “Gentrifying” neighborhoods consist of SBAs that meet two criteria: 1) low-income in 1990 and 2) experienced rent growth above the median SBA rent growth between 1990 and 2014. “Did not gentrify” neighborhoods also started as low-income in 1990 but experienced no growth or more modest rent growth. “Not eligible to gentrify” neighborhoods” are the city’s remaining SBA, which had higher incomes in 1990.
Primary analyses
We aimed to understand the relationship between childhood obesity and the changing food environment of children in the context of gentrification. This overall analysis required evaluation the several relationships including a) food chances, time and gentrification status; b) obesity and food chances trajectories c) obesity and gentrification. Below we provide details of these three analyses conducted.
To assess how food chances change throughout the 21-year timeframe, we conducted group-based trajectory model estimation (GBTM) on the number of food chances in the SBAs where CCCEH children lived at age five during 1990–2010. GBTM models the number of food chances as a continuous function of time (measured annually) and estimates the probability of trajectory membership for each food category. GBTM was conducted on healthy and unhealthy food chances separately to generate specific trajectories for each category. We log-transformed the count of food chances to better approximate a normal distribution and estimated models with varying numbers of groups [1–6] and shapes (linear, quadratic, cubic). We evaluated model fit using the Bayesian Information Criterion (BIC), as well as the magnitude of group membership posterior probabilities. The relationship between food trajectories and gentrification status (gentrifying, did not gentrify, and not eligible to gentrify) was assessed using chi-square Fisher Exact tests. The analyses GBTM were performed using the Stata command “traj” developed by Bobby L Jones and Daniel S Nagin (39). Table 1 provides the number of groups, shape, and BIC for both healthy and unhealthy food chance trajectories.
Table 1.
Food chances trajectories according to the number of groups, shapes, and BIC
| Food Chances Category | Number of groups | Trajectory shapes1 | BIC2 (N = 24) |
|---|---|---|---|
| Healthy Food Chances | 2 | 1 1 | 1.1 |
| 2 | 1 2 | 8.3 | |
| 2 | 2 1 | 10.3 | |
| 2 | 2 2 | 17.9 | |
| 2 | 3 3 | 24.7 | |
| 2 | 4 4 | 32.5 | |
| Unhealthy Food Chances | 2 | 4 4 | -26.9 |
| 3 | 1 1 4 | 26.6 | |
| 2 | 4 1 | -30.5 | |
| 3 | 1 1 4 | 51.66 | |
| 2 | 1 4 | -53.1 |
Trajectory shapes: 1 = linear; 2 = quadratic; 3 = cubic; 4 = quartic
BIC = Bayesian information criterion (for the total number of Sub-boroughs)
One or more of the groups had a very small proportion of the observations.
The food ecology is described concerning food chances to reflect the sociological construct of habitus that provides insights to obesogenic environments by focusing on the interplay between food chances and food choices. Food chances are the food establishments available in a neighborhood.
The relationship between obesity and the previously calculated trajectories were examined through linear regression of BMI z-scores and logistic regression of overweight/obesity status based on the CDC classification (33) of five-year-old children. Given that enrollment for CCCEH occurred from 1998–2006, children reached age five between 2003–2011. This period falls within the years covered by the NETS dataset and the Furman Center’s gentrification classification of NYC neighborhoods (199–2010). CCCEH participants turned five-years-old between 2003 and 2011. This period is one year beyond the period covered by NETS and the Furman Center. For those children that turned five in 2011 (n= 26), the food chance trajectories experienced in 2010 were included in the study.
Fisher Exact tests were conducted between the binary variable of overweight/obese status and gentrification status. Similar to the previous analysis, the relationship between obesity and gentrification was assessed through linear regression of BMI z-scores and logistic regression of overweight/obesity status as the dependent variables and the gentrification status of the child’s SBA.
Three adjustment strategies were considered for each of the aforementioned linear and logistic regressions: univariate model, individual-level only model, and full model with both individual and area-level covariates. Individual-level covariates include children’s age, gender, race/ethnicity (African American or Dominican American), mother’s pre-pregnancy BMI, mother’s years of education, and use of public assistance at least once from the period during pregnancy through the child being five-years-old. Area-level covariates include SBA average population size between 1990–2010, the land area of SBAs (square km, excluding bodies of water), percent of households with SNAP benefits in the past 12 months, and percent of residents with less than high school diploma. The population size was derived from the United States Census Bureau decennial census; the American Community Survey data (2006–2010 5-year estimates) was the source of all remaining area-level covariates.
Contextual analyses
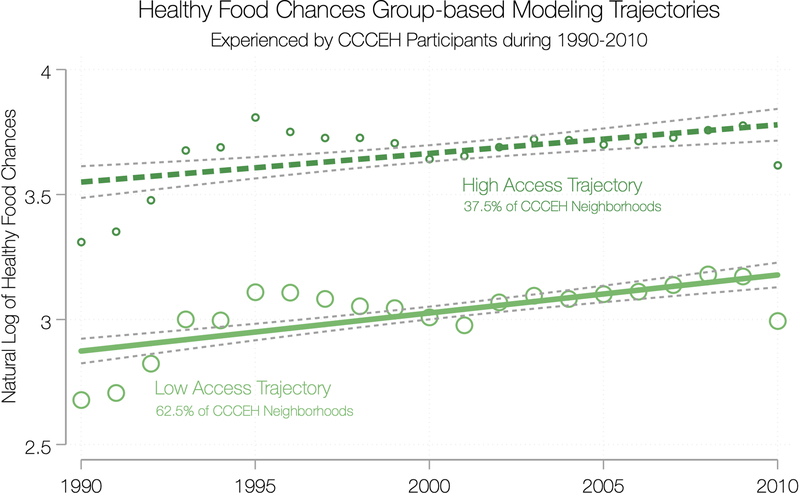
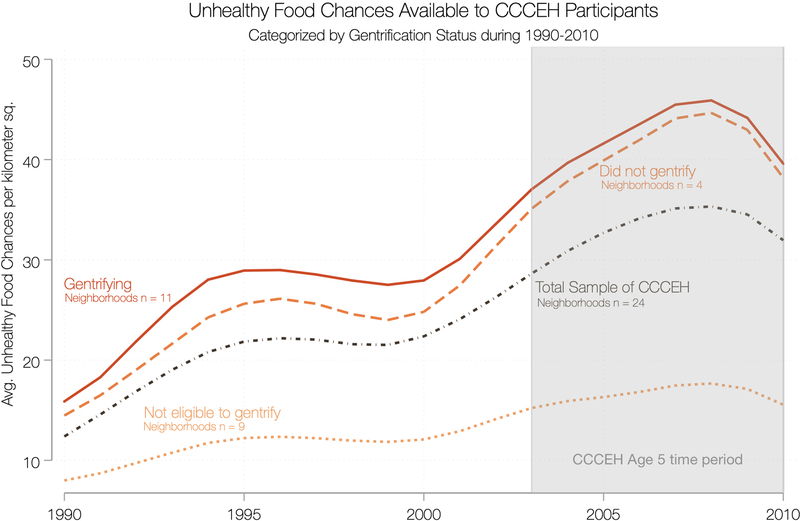
To graph changes in the food environment of CCCEH participants over time, we used locally weighted scatterplot smoothing (lowess) on the NETS data for the SBA in which CCCEH participants resided while the child was five-years-old. Lowess bandwidth of 0.4 was used to provide locally weighted scatterplot smoothing that narrowly followed the data. CCCEH participants with completed data on all variables of interests (BMI z-scores, BMI percentile, neighborhood, child’s gender, child’s age, child’s ethnicity, maternal education, pre-pregnancy BMI, and use of public assistance) reside in 24 of NYC’s 55 SBAs. Thus, only these 24 SBAs were used in the lowess plots to capture the food environment that CCCEH participants experienced. Figures 1 and 2 display the average number of food chances per square kilometer stratified by the gentrification status from 1990 to 2010.
Figure 1.
Group-based modeling trajectories for healthy food chances in neighborhoods where CCCEH participants resided when child was five-years-old
* The food ecology is described concerning food chances to reflect the sociological construct of habitus that provides insights to obesogenic environments by focusing on the interplay between food chances and food choices. Food chances are the food establishments available in a neighborhood.
Figure 2.
Group-based modeling trajectories for unhealthy food chances in neighborhoods where CCCEH participants resided when child was five-years-old
* The food ecology is described concerning food chances to reflect the sociological construct of habitus that provides insights to obesogenic environments by focusing on the interplay between food chances and food choices. Food chances are the food establishments available in a neighborhood.
Software
We performed all statistical analyses with Stata version 15 and graphics were developed with grystyle software (40). All regression analyses used cluster-robust standard errors to account for participants clustering within SBAs.
Results
The sample included 486 mother-child pairs from CCCEH with 54% female children. The majority of participants self-identified as Dominican, obtained at a least high school diploma (or GED) and never received public assistance before or while the child was five years old. Mothers’ pre-pregnancy BMI places nearly half as overweight or obese before pregnancy. At age 5 years, children predominantly lived in gentrifying neighborhoods and over a third of the sample of children were overweight or obese. Table 2 provides demographic information about the CCCEH mother-child dyads.
Table 2.
CCCEH participants characteristics at child age five
| Participant Characteristics | (N=486) |
|---|---|
| Race | |
| Dominican / Dominican American | 292 60% |
| African American | 194 40% |
| Gender | |
| Female | 261 54% |
| Caregiver Education Level | |
| GED, HS Diploma or more | 354 73% |
| Ever Received Public Assistance | |
| Yes | 80 17% |
| Child Body Mass Index | |
| Overweight or Obese | 187 39% |
| Maternal Body Mass Index | |
| Overweight or Obese | 222 46% |
| Gentrification Status and SBAs | |
| Gentrifying | 11 68% |
| Mott Haven/Hunts Point | |
| Morrisania/East Tremont | |
| Bedford Stuyvesant | |
| Bushwick | |
| North Crown Heights/Prospect Heights | |
| Lower East Side/Chinatown | |
| Morningside Heights/Hamilton Heights | |
| Central Harlem | |
| East Harlem | |
| Washington Heights/Inwood | |
| Astoria | |
| Did not gentrify | 4 26% |
| Highbridge/S. Concourse | |
| University Heights/Fordham | |
| Kingsbridge Heights/Mosholu | |
| Soundview/Parkchester | |
| Not eligible to gentrify | |
| Riverdale/Kingsbridge | 9 6% |
| Throgs Neck/Co-op City | |
| Pelham Parkway | |
| Williamsbridge/Baychester | |
| Park Slope/Carroll Gardens | |
| East Flatbush | |
| Elmhurst/Corona | |
| Rockaways | |
| North Shore | |
Trajectory analyses of food chances
GBTM of unhealthy and healthy food chances in CCCEH SBAs result in models with two trajectory groups that follow parallel increasing slopes (see figures 1 and 2). The trajectories for healthy food chances were best fit with a linear term function of time and the trajectories for unhealthy food chances were best fit with a more complex model that requires a quadratic function of time. Results of these analyses are provided in table 1. The food chances trajectories are classified as either low or high access. However, it should be recognized that the “low” and “high” descriptors are relative to the type of food chances category and lack an equivalent numeric representation. In other words, SBAs classified as “high access” to healthy foods is not equivalent to the number of food chances available in “high access” unhealthy food SBAs. The range for healthy food chances per square kilometer is between 2 and 7; while the range for unhealthy food chances is 8 to 54, indicating that it is more likely, in any SBA, that an individual will come in contact with an unhealthy vs healthy food outlet. This indicates that within an SBA, it is far more likely that an individual will interact with an unhealthy food establishment vs. a healthy food establishment. The healthy food chances GBTM suggests that 63% of SBAs where CCCEH participants resided during 1990–2010 were low access healthy food chances trajectories, while the remaining neighborhoods are classified as high access. GBTM of unhealthy food chances found 75% of SBAs contain low access trajectories.
Gentrification status and trajectories of food chances
In the CCCEH sample, the majority of households resided in gentrifying SBAs (see table 3). Nearly a quarter of the participants resided in SBAs that did not gentrify between 1990–2010. These SBAs that did not gentrify only include the low access trajectories of healthy and unhealthy food chances. Only 27 participants resided in SBAs not eligible to gentrify. Low access to unhealthy foods is more common in SBAs that are not eligible to gentrify. There are statistically significant (p < 0.001) differences between gentrification status and unhealthy and healthy food chances trajectories.
Table 3.
Food chances trajectories and gentrification status among CCCEH participants at age five
| Exposure | Gentrifying | Did not gentrify | Not eligible to gentrify | Total | P>|z| Fisher’s Exact Test |
|---|---|---|---|---|---|
| Healthy Food Chances Analyses | |||||
| Low Access | 174 (55%) | 127 (40 %) | 15 (5%) | 316 | |
| High Access | 158 (93%) | 0 (0.0%) | 12 (7%) | 172 | |
| Total | 332 (68 %) | 127 (26%) | 27 (6%) | 486 | 0.000 *** |
|
Unhealthy Food Chances Analyses | |||||
| Low Access | 151 (50%) | 127 (42%) | 25 (8%) | 303 | |
| High Access | 181 (99%) | 0 (0.0%) | 2 (1%) | 183 | |
| Total | 332 (68%) | 127 (26%) | 27 (6%) | 486 | 0.000 *** |
(p < .05)
(p ≤ 0.01)
(p ≤ 0.001)
Regression analyses of children’s BMI and food chances trajectories
We analyzed the relationship between children’s BMI z-score and food chances GBTM. Across all models, children residing in neighborhoods with high access to healthy foods have lower BMI-z scores and less likely to be overweight or obese compared to children who resided in neighborhoods with low access to healthy foods (see table 4). BMI-z is significantly lower in adjusted models at the individual level (beta = −0.32; 95% CI: 0.5, −0.1). Children are less likely to be overweight or obese controlling for individual and area level covariates respectively (OR= 0.58; 95% CI: 0.4, 0.8; OR= 0.35; 95% CI: 0.2, 0.8). Across all models, children residing in neighborhoods with high access to unhealthy food chances trajectories had slightly lower BMI-z scores. The logistic regression model predicting overweight or obesity adjusted for individual-level covariates was significant (OR=0.68; 95% CI: 0.5, 1.0).
Table 4.
Obesity measures and food chance trajectories regression analyses for CCCEH participants at age five
| BMI-Z | Overweight/Obese | |||||
|---|---|---|---|---|---|---|
| Exposure | Model 1 a (N= 486) |
Model 2 b (N= 486) |
Model 3 c (N= 486) |
Model 1 a (N= 486) |
Model 2 b (N= 486) |
Model 3 c (N= 486) |
| Beta (95% CI) |
Beta (95% CI) |
Beta (95% CI) |
OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
|
| Healthy Food Chances Analyses: | ||||||
| Low Access Trajectory | Ref | ref | ref | ref | Ref | ref |
| High Access Trajectory | −0.19 (−0.4 to 0.0) |
−0.32** (−0.5 to -0.1) |
−0.43 (−0.9 to 0.0) |
0.78 (0.5 to 1.2) |
0.58*** (0.4 to 0.8) |
0.35** (0.2 to 0.8) |
| Unhealthy Food Chances Analyses: | ||||||
| Low Access Trajectory | ref | ref | ref | ref | Ref | ref |
| High Access Trajectory | −0.09 (−0.3 to 0.2) |
−0.19 (−0.5 to 0.1) |
−0.18 (−0.6 to 0.3) |
0.88 (0.6 to 1.3) |
0.68* (0.5 to 1.0) |
0.59 (0.3 to 1.3) |
(p < 0.05)
(p ≤ 0.01)
(p ≤ 0.001)
Univariate model
Adjusted individual-level model (individual level covariates included gender, age, ethnicity, maternal education, maternal pre-pregnancy BMI, and public assistance)
Adjusted model with individual and neighborhood level covariates (including SBA population, area in kilometers squared excluding bodies of water, SNAP recipients, and educational attainment)
Regression analyses of children’s BMI and gentrification status
The majority of children in the study are not overweight or obese (n=299), and 71% of them live in gentrifying neighborhoods. A small percentage (5%) of healthy weight children reside in SBAs not eligible to gentrify and the, remaining 24% lived in SBAs that did not gentrify during 1990–2010. Similar to their healthy counterparts, overweight or obese children (n=187) primarily live in gentrifying SBAs (65%), a small percentage live in SBAs not eligible to (6%), and a slightly higher percentage live in SBAs that did not gentrify (29%). There are no statistically significant differences between these groups (see table 5).
Table 5.
Overweight/obese status and gentrification status among CCCEH participants at age five
| Exposure | Gentrifying | Did not gentrify | Not eligible to gentrify | Total | P>|z| Fisher’s Exact Test |
|---|---|---|---|---|---|
| Neither overweight nor obese | 211 (70.57 %) | 73 (24.41 %) | 15 (5.02 %) | 299 | |
| Overweight or obese | 121 (64.71 %) | 54 (28.88%) | 12 (6.42 %) | 187 | |
| Total | 332 (68.31%) | 127 (26.13%) | 27 (5.56%) | 486 | 0.386 |
SBAs that did not gentrify (as compared with gentrifying neighborhoods) were associated with higher BMI z-scores. However, this was only statistically significant in the unadjusted model (beta= 0.18; CI: 0.0, 0.3). This positive relationship was also present in the logistic regression analyses of overweight or obesity status but also lacked statistical significance. SBAs not eligible to gentrify (as compared with gentrifying neighborhoods) were also associated with higher BMI z-scores and being overweight or obese, but also lacked statistical significance. Full details are presented in table 6.
Table 6.
Obesity measures and gentrification status
| BMI-Z | Overweight/Obese | |||||
|---|---|---|---|---|---|---|
| Exposure | Model 1 a (N= 486) |
Model 2 b (N= 486) |
Model 3 c (N= 486) |
Model 1 a (N= 486) |
Model 2 b (N= 486) |
Model 3 c (N= 486) |
| Beta (95% CI) |
Beta (95% CI) |
Beta (95% CI) |
OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
|
| Gentrification Status | ||||||
| Gentrifying | ref | ref | ref | ref | ref | ref |
| Did not Gentrify | 0.18 * (0.0 to 0.3) |
0.13 (−0.1 to 0.3) |
0.06 (−0.6 to 0.3) |
1.29 (0.9 to 1.9) |
1.23 (0.8 to 1.8) |
1.13 (0.7 to 1.8) |
| Not eligible to gentrify | 0.36 (−0.1 to 0.8) |
0.31 (−0.2 to 0.8) |
0.24 (−0.6 to 1.1) |
1.40 (0.7 to 2.9) |
1.32 (0.6 to 3.1) |
.91 (0.3 to 3.1) |
(p < 0.05)
(p ≤ 0.01)
(p ≤ 0.001)
Univariate model
Adjusted individual-level model (individual level covariates included gender, age, ethnicity, maternal education, maternal pre-pregnancy BMI, and public assistance)
Adjusted model with individual and neighborhood level covariates (including SBA population, area in kilometers squared excluding bodies of water, SNAP recipients, and educational attainment)
Food chances and gentrification status
The SBAs where CCCEH participants resided, food chances increase over time, across all categories of gentrification, there seems to be a surge in food chances around 1995, with a steady increase from 2000 until 2008 where the number of food chances declines (see figure 3). This pattern is present in all three categories of food chances; however, the sum, mean and range vary between healthy and unhealthy food chances (see figures 4 and 5).
Figure 3.
Total food chances available to Columbia Center for Children’s Environmental Health participants categorized by gentrification status during 1990–2010
n = Neighborhoods defined by NYC sub-borough areas
* Area of neighborhood excludes bodies of water
** The food ecology is described concerning food chances to reflect the sociological construct of habitus that provides insights to obesogenic environments by focusing on the interplay between food chances and food choices. Food chances are the food establishments available in a neighborhood.
Figure 4.
Average healthy food chances available to Columbia Center for Children’s Environmental Health participants categorized by gentrification status during 1990–2010
n = Neighborhoods defined by NYC sub-borough areas
* Area of neighborhood excludes bodies of water
** The food ecology is described concerning food chances to reflect the sociological construct of habitus that provides insights to obesogenic environments by focusing on the interplay between food chances and food choices. Food chances are the food establishments available in a neighborhood.
Figure 5.
Average unhealthy food chances available to Columbia Center for Children’s Environmental Health participants categorized by gentrification status during 1990–2010
n = Neighborhoods defined by NYC sub-borough areas
* Area of neighborhood excludes bodies of water
** The food ecology is described concerning food chances to reflect the sociological construct of habitus that provides insights to obesogenic environments by focusing on the interplay between food chances and food choices. Food chances are the food establishments available in a neighborhood.
Gentrifying SBAs have the most food chances across all years, (mean = 49.4; median = 47.8; range = 17.7–104.4). SBAs that did not gentrify followed (mean = 68.2; median = 57.4; range = 14.9 −253.1). SBAs not eligible to gentrify offered the lowest number of food chances per square kilometer during 1990–2010 (mean = 26.1; median = 24; range = 5.2–70.5.
Overall there are fewer healthy food chances than unhealthy food chances available to CCCEH participants across all years and gentrification categories. Gentrifying SBAs have both the greatest number of healthy (mean = 6; median = 5.5; range = 1.2–14.9), and unhealthy (mean = 36.7; median = 31.7; range = 9.1–93.2) food chances across all years. Food chances afforded by SBAs that did not gentrify had fewer healthy (mean = 4.1; median = 4.1; range = 1.7 −7.9) and unhealthy (mean = 30.2; median = 26.9; range = 9.6–68.1) food chances are less than gentrifying SBAs. SBAs not eligible to gentrify offered the lowest number of food chances per square kilometer for both healthy (mean = 2.7; median = 2.7; range = 0.4–5.7) and unhealthy (mean = 13.5; median = 12.1; range = 2.1–35.7) food chances.
Discussion
This study evaluated shifts in food chances as a function of gentrification, and the relationship between area-level healthy and unhealthy food chances and the BMI of five-year-old children in a birth cohort study. An increase in food chances was noted between 1990–2010. Gentrifying neighborhoods experienced the most significant increase of opportunities to purchase foods, including both healthy and unhealthy food chances, and participants living in areas that were not eligible to gentrify experienced lower availability of healthy and unhealthy food sources throughout the time period. Greater area-level availability of healthy foods was associated with lower BMI at age 5. Although unhealthy food sources were more abundant, there was no observed relationship between area-level availability of unhealthy foods and excess weight in this sample. While most of the birth cohort sample lived in areas classified as gentrifying, there was no statistically significant association of area-level gentrification with BMI at age 5.
Changes in urban food ecology as a function of gentrification have not only taken hold in New York City but across the nation. Our findings provide insights to study the effect of gentrification on health retrospectively. Despite the lack of a universally accepted operational definition, gentrification connotes images of a capital investment that often create a flourishing food ecology. For instance, communities defined as food deserts are transformed into an abundance of food opportunities. Some researchers are not convinced that these new establishments will transfer into actual uptake of healthier food consumption (28,41). We hypothesized that gentrification would increase healthier food chances. The NETS data indicate that there was an overall increase in food chances throughout the city regardless of gentrification status, including an overall increase in healthy food chances in gentrifying neighborhoods until 2008. However, gentrifying neighborhoods held not only the greatest abundance of healthy food chances but also the greatest abundance of unhealthy food chances. The simultaneous increase suggests that all food chances are increasing, but there are more opportunities to choose unhealthy options. In terms of food habitus, residents may lean towards what is more available, accessible, and affordable to obtain in their neighborhoods. The food habitus formed by the historic lack of healthy foods chances will take time to change, even when healthy foods become available and affordable.
Moreover, a change in habitus does not occur immediately. Thus, lasting dispositions towards one’s food choices may remain. Residents that have formed a less health-promoting food habitus due to a past absence of healthy food chances could be more susceptible to continuing to choose the unhealthy options that are becoming increasingly available in their neighborhood.
Given the literature on the abundance of fast food outlets in marginalized communities (27,42–46), it was surprising that gentrifying SBAs experienced more of an increase in unhealthy food chances as compared with SBAs that did not gentrify. This may be a result of overall growth and opportunities for capital investment of food businesses signaling broader changes to the retail ecology irrespective of healthfulness. Lastly, it should be noted that we believe the decline near the end of our observation period and across all gentrification statuses may be a result of the 2008 economic crisis as well as trends toward more online food retail.
The two trajectories identified by the GBTM analyses for healthy and unhealthy food chances resemble the lowess curves for both of these categories confirming the latter analyses. The significant relationships between a) gentrification status and food chances and b) healthy food chance trajectories and obesity would suggest an association between gentrification status and obesity. However, this was not detectable, and future investigations may provide insight as to whether such an association would be observed with sufficient statistical power and variation in the environment. It is clear that the process of gentrification may influence the food ecology, and a food environment higher in availability healthy foods may be protective against children developing obesity. The relationship between gentrification and childhood obesity, and the causal nature of links along this pathway, would benefit from further research.
The lack of association between increased access to unhealthy foods and obesity is contrary to public discourse about the association between fast-food outlets and BMI. Yet, this finding is consistent with prior work in NYC (47). The ubiquitous nature of bodegas, fast food restaurants, and other unhealthy food chances in NYC may have oversaturated the environment such that healthy food access is more of a limiting factor, constraining food choices of CCCEH participants.
Availability of healthy foods as measured in this study is only one of many factors that play into household food purchases. If household food purchases are determined largely by cost, there may be a preference toward familiar, less expensive foods, limiting the risk of dissatisfaction and potential food waste. Moreover, highly processed foods are less likely to be wasted due to perishability. As previously mentioned, habitus takes time to change therefore an expanded time frame for future research efforts to capture potential changes in habitus is needed.
Beyond the household, it is important to consider policy-related influences from our community and government on children who are five-years-old. In our sample, 17% of families received public assistance at least once during the time of this study. Some programs, i.e., the Women, Infants, and Children (WIC) only benefit families until the child’s fifth birthday. Thus, nutritional intake may suffer once no longer eligible. Further research beyond the age of five can provide more insights to the impact of aging out of WIC. Also, children of this age may participate in meals provided by his or her public school; as many as, two meals and one snack per school day. United States public school meal programs are notoriously underfunded and often provided ultra-processed foods. Food choices of under-resourced families become limited while a child’s palate adapts to a constrained menu. Gentrification may exacerbate the lack of resources for local public schools in the most economically disadvantaged areas, and increase segregation as a result of the decision not to attend local schools in which children are assigned. (48,49). Currently, 40 percent of NYC kindergartners do not attend his or her assigned school; leading to concentrated poverty in zoned schools (49).
Strengths and limitations
There are several limitations to this study that should be acknowledged. First, the sample is limited to less than half of NYC neighborhoods and a specific cohort associated with CCCEH. A city-wide sample and better yet, a national sample would provide a better representation of gentrification in the United States. Secondly, the complexity associated with measuring gentrification limits our understanding of the multifaceted social process. Using the Furman Center’s definition relies on the assumption that gentrification can be distilled to a simple categorical variable for the entire time period rather than varying in intensity and dynamic over time. There may be nuances or levels of gentrification that change the status of a neighborhood during the period of study. Future analyses may consider creating a continuum measure of gentrification that is informed by input from community residents.
Moreover, food chances categories may not have been able to capture gradations within the food environment. For example, food chances labeled as “healthy” may offer “unhealthy” items (e.g., candy at a supermarket) and vice versa (e.g., apple slices or salads at fast food restaurants). Also, there may be differences in the food choices made by individuals shopping and eating at these food establishments, such that our categorization oversimplifies the multi-faceted nature of variation in the food environment. As previously mentioned, including an investigation of food habitus (the interplay between food chances and food choices) can provide useful insights for understanding food practices and reducing disparities in childhood obesity. We were limited to data collected during CCCEH follow-up visits that did not capture household food choices or diet quality.
Despite these limitations, this study had substantial strengths. The multiple sources of data coalesced to provide a multi-faceted picture of the food environment experienced by CCCEH five-year-old children. The longitudinal nature of the NETS data allowed for the food environment changes associated with the social process of gentrification to be captured over time. As a single measure of food availability is unlikely to describe the food environment, we were able to measure both unhealthy and unhealthy food chances for 21 years. Lastly, we applied GBTM, enabling the identification food chance trajectories that provided an empirical basis for identifying and describing groups.
Conclusions
Our results suggest gentrification influences neighborhood food environment in NYC and children exposed to plentiful food chances as well as greater healthy foods experienced a lower body mass index by age five. The interplay between obesogenic food chances and choices is integral to preventing childhood obesity. Figure 6 provides a visual representation of how our work builds on a foundation of children’s environmental health research that aims to reduce inequities. Further research is needed to understand the pathways through which gentrification impacts childhood obesity and to inform policy and community actions that can break the cycle of childhood obesity in marginalized populations.
Figure 6.
Breaking the cycle of children’s obesity and environmental health disparities
* The food ecology is described concerning food chances to reflect the sociological construct of habitus that provides insights to obesogenic environments by focusing on the interplay between food chances and food choices. Food chances are the food establishments available in a neighborhood.
Acknowledgments
We want to acknowledge the support of the Break the Cycle of Children’s Environmental Health program that provided an opportunity to bring this project into fruition. Also, we appreciate the mothers, children, and research staff of CCCEH as well as the helpful feedback, patience, and insights of Jesse Cahill, Whitney Cowell, Lori Hoepner, Bobby Jones, Helen-Maria Lekas, and Leslie Rubin.
Footnotes
Conflicts of interest: No conflicts of interest to disclose. Funding: This publication was made possible by the National Heart, Lung, and Blood Institute (NHLBI) grant 5F31HL131441–03, U.S. Environmental Protection Agency (US EPA) grant RD83214101 and National Institute for Environmental Health Sciences (NIEHS) grant 1RC2ES018784 and P01 ES09600. This work was also funded in part by grant K01HD067390 from the Eunice Kennedy Shiver National Institute for Child Health and Human Development (NICHD).
References
- 1.Hales C, Carroll M, Fryar C, Ogden C. Prevalence of obesity among adults and youth: United States, 2015–2016. Hyattsville, MD: 2017. URL: https://www.cdc.gov/healthyschools/obesity/facts.html [PubMed] [Google Scholar]
- 2.Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. JAMA 2018;319(23):2410–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378(9793):815–25. [DOI] [PubMed] [Google Scholar]
- 4.Goldfinger JZ, Arniella G, Wylie-Rosett J, Horowitz CR. Project HEAL: Peer Education Leads to Weight Loss in Harlem. J Health Care Poor Underserved 2008;19(1):180–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford PB, Dzewaltowski DA. Disparities in obesity prevalence due to variation in the retail food environment: three testable hypotheses. Nutr Rev 2008;66(4):216–28. [DOI] [PubMed] [Google Scholar]
- 6.Haire-Joshu D, Tabak R. Preventing obesity across generations: Evidence for early life intervention. Annu Rev Public Health 2016;37(1):253–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity. Am J Prev Med 2006;30(4):333–9. [DOI] [PubMed] [Google Scholar]
- 8.Morland KB. An evaluation of a area-level intervention to a local food environment. Am J Prev Med 2010;39(6):e31–8. [DOI] [PubMed] [Google Scholar]
- 9.Black JL, Macinko J. Neighborhoods and obesity. Nutr Rev 2008;66(1):2–20. [DOI] [PubMed] [Google Scholar]
- 10.Lee H The role of local food availability in explaining obesity risk among young school-aged children. Soc Sci Med 2012;74(8):1193–203. [DOI] [PubMed] [Google Scholar]
- 11.Lake A, Townshend T. Obesogenic environments: exploring the built and food environments. J R Soc Promot 2016;126(6):262–7. [DOI] [PubMed] [Google Scholar]
- 12.Larkin M Can cities be designed to fight obesity? Lancet 2003;362(9389):1046–7. [DOI] [PubMed] [Google Scholar]
- 13.Holsten JE. Obesity and the community food environment: A systematic review. Public Health Nutr 2009;12(3):397–405. [DOI] [PubMed] [Google Scholar]
- 14.Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place 2009;15(2):491–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drewnowski A. Obesity and the food environment. Am J Prev Med 2004;27(3):154–62. [DOI] [PubMed] [Google Scholar]
- 16.Howard PH, Fitzpatrick M, Fulfrost B. Proximity of food retailers to schools and rates of overweight ninth grade students: An ecological study in California. BMC Public Health 2011;11(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31(1):7–20. [DOI] [PubMed] [Google Scholar]
- 18.Lang T, Caraher M. Access to healthy foods: part II. Food poverty and shopping deserts: what are the implications for health promotion policy and practice? Health Educ J 2016. Jul 24;57(3):202–11. [Google Scholar]
- 19.Cassady D, Jetter KM, Culp J. Is price a barrier to eating more fruits and vegetables for low-income families? J Am Diet Assoc 2007;107(11):1909–15. [DOI] [PubMed] [Google Scholar]
- 20.Davidson M, Lees L. New-build “gentrification” and London’s Riverside renaissance. Environ Plan A 2016;37(7):1165–90. [Google Scholar]
- 21.Kelly B, Flood VM, Yeatman H. Measuring local food environments: An overview of available methods and measures. Health Place 2011;17(6):1284–93. [DOI] [PubMed] [Google Scholar]
- 22.Gittelsohn J, Sharma S. Physical, consumer, and social aspects of measuring the food environment among diverse low-income populations. Am J Prev Med 2009;36(4): S161–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Odoms-Young AM, Zenk S, Mason M. Measuring food availability and access in African-American communities. Am J Prev Med 2009;36(4): S145–50. [DOI] [PubMed] [Google Scholar]
- 24.Lytle LA. Measuring the food environment. Am J Prev Med 2009;36(4): S134–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKinnon RA, Reedy J, Morrissette MA, Lytle LA, Yaroch AL. Measures of the food environment. Am J Prev Med 2009;36(4):S124–33. [DOI] [PubMed] [Google Scholar]
- 26.Glanz K Measuring food environments. Am J Prev Med 2009;36(4):S93–8. [DOI] [PubMed] [Google Scholar]
- 27.Gordon C, Purciel-Hill M, Ghai NR, Kaufman L, Graham R, Van Wye G. Measuring food deserts in New York City’s low-income neighborhoods. Health Place 2011;17(2):696–700. [DOI] [PubMed] [Google Scholar]
- 28.Breyer B, Voss-Andreae A. Food mirages: Geographic and economic barriers to healthful food access in Portland, Oregon. Health Place 2013;24(C):131–9. [DOI] [PubMed] [Google Scholar]
- 29.Cockerham WC. Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav 2016;46(1):51–67. [DOI] [PubMed] [Google Scholar]
- 30.Bourdieu P Outline of a theory of practice. Cambridge: Cambridge University Press, 1977. [Google Scholar]
- 31.Whyatt RM, Barr DB, Camann DE, Kinney PL, Barr JR, Andrews HF, et al. Contemporary-use pesticides in personal air samples during pregnancy and blood samples at delivery among urban minority mothers and newborns. Environ Health Perspect 2003;111(5):749–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perera FP, Rauh V, Tsai W-Y, Kinney P, Camann D, Barr D, et al. Effects of transplacental exposure to environmental pollutants on birth outcomes in a multiethnic population. Environ Health Perspect 2003;111(2):201–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Center for Disease Control and Prevention. A SAS program for the CDC growth charts. Atlanta, GA: CDC, 2000. [Google Scholar]
- 34.Rundle A, Neckerman KM, Freeman L, Lovasi GS, Purciel M, Quinn J, et al. Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect 2008;117(3):442–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neckerman KM, Bader MDM, Richards CA, Purciel M, Quinn JW, Thomas JS, et al. Disparities in the food environments of New York City public schools. Am J Prev Med 2010;39(3):195–202. [DOI] [PubMed] [Google Scholar]
- 36.Stark JH, Neckerman K, Lovasi GS, Konty K, Quinn J, Arno P, et al. Neighbourhood food environments and body mass index among New York City adults. J Epidemiol Community Health 2013;67(9):736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaufman TK, Sheehan DM, Rundle A, Neckerman KM, Bader MDM, Jack D, et al. Measuring health-relevant businesses over 21 years: Refining the National Establishment Time-Series (NETS), a dynamic longitudinal data set. BMC Res Notes 2015;8(1):1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.New York University Furman Center. State of New York City’s Housing and Neighborhoods in 2015. New York: Furman Center, 2016. URL: http://furmancenter.org/research/sonychan/2015-report. [Google Scholar]
- 39.Jones BL, Nagin DS. A Stata plugin for estimating group-based trajectory models. Sociol Methods Res 2013. Doi: 10.1177/0049124113503141. [DOI] [Google Scholar]
- 40.Jann B GRSTYLE: Stata module to customize the overall look of graphs. Boston, MA: Boston College Department Economics, 2018. [Google Scholar]
- 41.Sullivan DM. From food desert to food mirage: Race, social class, and food shopping in a gentrifying neighborhood. Adv Appl Sociol 2014;4(1):30–5. [Google Scholar]
- 42.Kwate NOA. Fried chicken and fresh apples: Racial segregation as a fundamental cause of fast food density in black neighborhoods. Health Place 2008;14(1):32–44. [DOI] [PubMed] [Google Scholar]
- 43.Kwate NOA, Yau C-Y, Loh J-M, Williams D. Inequality in obesigenic environments: Fast food density in New York City. Health Place 2009;15(1):364–73. [DOI] [PubMed] [Google Scholar]
- 44.Kwate NOA, Loh J-M. Separate and unequal: The influence of neighborhood and school characteristics on spatial proximity between fast food and schools. Prev Med 2010;51(2):153–6. [DOI] [PubMed] [Google Scholar]
- 45.Valera P, Gallin J, Schuk D, Davis N. Trying to eat healthy. Affilia 2009;24(3):300–14. [Google Scholar]
- 46.Fleischhacker SE, Evenson KR, Rodriguez DA, Ammerman AS. A systematic review of fast food access studies. Obes Rev 2010;12(5):e460–71. [DOI] [PubMed] [Google Scholar]
- 47.Bader MDM, Schwartz-Soicher O, Jack D, Weiss CC, Richards CA, Quinn JW, et al. More neighborhood retail associated with lower obesity among New York City public high school students. Health & Place. 2013;23:104–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DeSena JN, Shortell T. The world in Brooklyn: gentrification, immigration, and ethnic politics in a global city. Lanham: Lexington Books, 2014. [Google Scholar]
- 49.Harris EA, Katz J. Why are New York’s schools segregated? It’s not as simple as housing. New York Times [Internet]. 2018. May 2 [cited 2018Jun11]; URL: www.nytimes.com/interactive/2018/05/02/nyregion/new-study-school-choice-increases-school-segregation.html? [Google Scholar]