Abstract
Background
Perception by workers of their health problems as work-related is possibly associated with sickness absence (SA). The aim of this study was to to study the relationship between perceived work-relatedness of health problems and SA among workers who visit their GP, taking the influence of other potential determinants into account and to study the influence of these determinants on SA. Design and setting prospective cohort study in 32 Dutch GP practices.
Methods
A secondary analysis of RCT data among workers, aged 18–63 years, who visited their GP. We measured self-reported SA days in 12 months and high SA (>20 days in 12 months) and compared workers who perceived work-relatedness (WR+) with workers who did not (WR−). With multivariable linear and logistic regression models, we analyzed the influence of age, gender, experienced health, chronic illness, prior SA, number of GP consultations and perceived work ability.
Results
We analyzed data of 209 workers, 31% perceived work-relatedness. Geometric mean of SA days was 1.6 (95% CI: 0.9–3.0) for WR+− workers and 1.2 (95% CI: 0.8–1.8) for WR− workers (P = 0.42). Incidence of high SA was 21.5 and 13.3%, respectively (odds ratio 1.79; 95% CI: 0.84–3.84). SA was positively associated with chronic illness, prior SA, low perceived work ability and age over 50.
Conclusions
Perceived work-relatedness was not associated with SA. SA was associated with chronic illness, prior SA, low perceived work ability and age over 50.
Keywords: At-risk groups, chronic disease, gender, occupational/environmental medicine, primary care, work-related stress
Key Messages.
Many workers who visit their GP perceive their health problem as work-related.
A low expectation to be able to work is associated with sickness absence.
Chronic illness and prior absenteeism are associated with sickness absence.
Introduction
Sickness absence (SA) is supposed to allow people the time and rest to recover from illness without loss of financial security. However, SA can also have negative consequences, both for individual patients and for society (1–5). Therefore, predicting and preventing avoidable SA has become a priority for institutions who bear the costs of SA (6). As it is also becoming evident that being unable to work for a long time is detrimental for the health and life expectancy of individual patients, the prediction and prevention of SA are also relevant for health care professionals (7,8). In studies in different settings, like occupational health, social security institutions or large companies, many factors which positively influence SA have been identified (9–14) such as higher age, female gender, low self-rated health, mental health problems (including depression), previous SA, emotional job demands, negative perceived work ability, heavy work and low socioeconomic position.
In most European countries, GPs have a prominent role in regulating SA (15). In those countries, patients who think they are not able to do their work are required to visit a GP (15). The GP has to certify SA and give advice about when work can be resumed and whether circumstances at work need to be modified to allow patients to successfully resume their work. Dutch GPs have no formal role in the certification of sick leave. However, it is among their primary tasks to explore the reason for encounter and the contributing factors (16). Many workers who visit a GP perceive their health problem as being work-related (17–20). Moreover, for most of those who do not think their health problem is work-related, work can still be an important contextual factor. Dutch patients appreciate an active role of GPs concerning their work (21,22). However, the extent to which Dutch GPs fulfil this role still appears to be limited, and they often do not acknowledge the work-relatedness of health problems (23,24). For instance, in a large-scale study it was found that during consultations of workers on sick leave, their GP discussed the relation between symptoms and sick leave in only 35% of the cases (24). GPs need to be aware of factors that influence SA. Therefore, we need data from patients visiting their general practitioner.
In this study, we aim (1) to address whether the perceived work-relatedness of health problems is associated with SA among patients who visit their GP. In studying this, we will take the influence of other potentially relevant determinants of SA—age, gender, experienced health, presence of chronic illness, number of visits to the GP and perceived work ability—into account and (2) to study the influence of all important factors including work-relatedness on SA.
Methods
This study is a secondary analysis of data from a randomized controlled trial about the effectiveness of education of GPs to improve patients’ coping when confronted with work-related problems (22). We consider the study a prospective cohort study and we will report it according to the STROBE guidelines (25).
Participants
This study took place in 26 GP practices in the southeast of the Netherlands. Thirty-two GPs participated in this study and collected data of 640 patients. Enrollment started in February 2012 and lasted to January 2013. To be eligible, patients had to visit one of the participating GPs, be 18–63 years old, work at least 12 hours per week and have sufficient command of the Dutch language to complete the questionnaires.
Measurements
Data were collected with self-report questionnaires, which were completed by the patients at baseline (shortly after a visit to the GP), at least 6 months after baseline and again, at least 6 months after the second questionnaire. The questionnaires comprised items about the work-relatedness of their health problem, SA, perceived work ability, experienced health, presence of chronic illness and number of visits to GP. The questionnaires have been described in more detail in the study protocol (26).
Variables
Work-relatedness was measured with the question: ‘Do you think the health problem for which you visited your GP may be related to your work?’ with answering categories ‘yes’ or ‘no’. At baseline, SA was measured over the previous year using an ordinal scale (‘none’; ‘1–5 days’; ‘6–10 days’; ‘11–20 days’; ‘more than 20 days’). Moreover, at all three measurement points, we determined SA over the last 6 months using a numerical scale (‘how many days were you absent from your work over the last 6 months?’). To quantify SA from baseline to end of follow-up (12 months), we added the estimated number of SA days from the second and third questionnaires. As there is no international consensus on a definition, we defined high SA as more than 20 days in 12 months (27).
To measure perceived work ability, we used the 11-item Return to Work Self-Efficacy scale (RTW-SE) (28). Each item in this scale can be given a score from 1–6 and the final score is the mean of the items, with higher numbers indicating more positive expectations. To measure experienced health, we used a question from the SF-36: ‘how would you rate your present health?’ with a 5-point Likert scale (29). We assessed the presence of a chronic disease using the question: ‘Do you suffer from a chronic disease?’ with answering categories ‘yes’ or ‘no’. If a chronic disease was present, we asked the participants to specify it by choosing from a list of 13 chronic diseases or by using free text. We then categorized the chronic diseases as follows: mental health; musculoskeletal; other. We assessed the number of visits to the GP using the question: ‘How many times did you visit your GP over the last 6 months?’ We dichotomized the independent variables age, experienced health, chronic illness, prior SA, number of visits to the GP and perceived work ability. For age, we used the categories over 50 and 50 or younger; for experienced health, the categories fair or poor and good, very good or excellent; for chronic illness, present and not present; for prior SA, more than 5 days and 5 days or less; for visits to the GP, three or more visits and two visits or less; for perceived work ability, an RTW-SE score of 5 or less and an RTW-SE score over 5.
Analysis
We described the characteristics of the participants at baseline and compared the characteristics of the participants with a complete response with those of the participants with an incomplete response. If data were missing, we gave the number of participants for whom information about the characteristic was known. We made no use of imputation. We used the data from participants with a complete response (n = 209) for our analysis. In this sample, we assessed the characteristics of the patients who experienced work-relatedness and the patients who did not at baseline. We compared the number of SA days at follow-up of patients who experienced work-relatedness with patients who did not. Because of the skewed distribution of the number of SA days, we used a logarithmic transformation and then performed a linear regression analysis. The mean log number of SA days was exponentiated to calculate the geometric mean for both groups. We also compared the proportion of patients with high SA (>20 days in 12 months) in both groups and of those who reported no SA.
Next, we estimated the effect of experienced work-relatedness on the number of days of SA and on high SA with linear regression analysis (number of SA days as dependent variable) and logistic regression analysis (proportion of patients with high sickness >20 days in 12 months as dependent variable). Finally, we entered all independent variables (age, gender, experienced health, presence of chronic illness, prior SA, perceived work ability, number of visits to the GP) simultaneously as potential confounders in both models to estimate adjusted effects of experienced work-relatedness. After stepwise backward elimination of the least significant independent variables, we obtained a model with variables which were significantly associated with the outcomes. Finally, we checked whether adding the factor ‘allocation’ (intervention group or control group) to the models interacted with the effect of the other factors. A P-value of <0.05 was considered to be statistically significant, based on two-sided testing. All analyses were conducted using IBM SPSS Statistics version 25.
Results
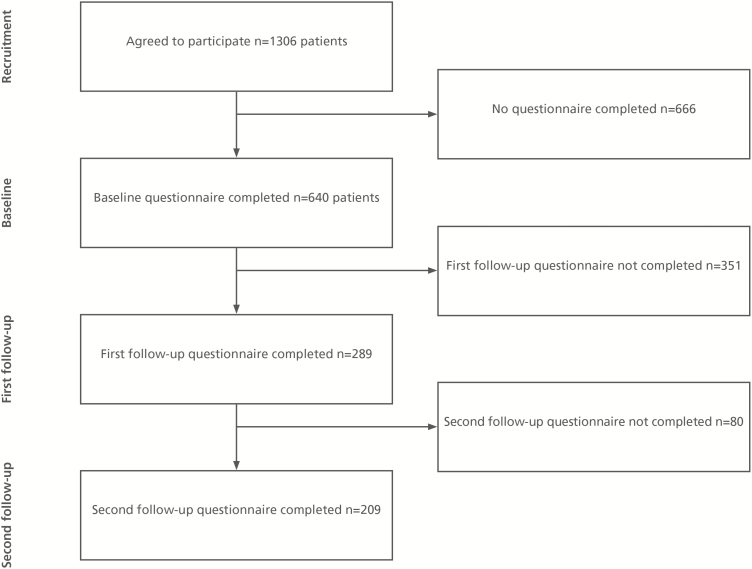
Of the 1306 patients who agreed to participate in our study, 640 returned the baseline questionnaire. The non-responders (n = 766) were younger (41.8 versus 44.5 years; P < 0.001), more often male (50.6 versus 42.0; P = 0.002) and worked more hours per week compared with the responders (33.7 versus 31.6; P < 0.001). From the responders, we had complete data of 209 patients at follow-up and incomplete data of 431 patients (Figure 1). In Table 1, we show the characteristics of the patients at baseline and compare the characteristics of the patients with complete and incomplete follow-up. Participants with complete and incomplete data were different concerning age (46.6 versus 43.5 years); chronic illness, more specifically: the presence of a mental health problem (0% versus 16%); and work-ability expectations score (4.9 versus 4.6).
Figure 1.
Flow chart of the study, showing the recruitment and data collection among workers who visited a GP participating in our study, February 2012–June 2014.
Table 1.
Baseline characteristics of the 640 workers who returned the first questionnaire and comparison of characteristics of workers with complete and incomplete follow up data (N (%) or mean ± SD) (2012–2014)
| All patients (N=640) | Complete follow-up (N=209) | Incomplete follow-up (N=431) | P value | |
|---|---|---|---|---|
| Age | 44.5 ± 10.8 | 46.6 ± 9.8 | 43.5 ± 11.1 | <0.01a |
| Working hours/week | 31.6 ± 10.7 | 31.2 ± 11.2 | 31.8 ± 10.5 | 0.51a |
| Gender | ||||
| Female | 371 (58.0) | 123 (58.9) | 248 (57.5) | 0.75b |
| Experienced health (N = 631) | ||||
| Excellent | 25 (4.0) | 9 (4.3) | 16 (3.8) | 0.91b |
| Very good | 102 (16.2) | 35 (16.8) | 67 (15.8) | |
| Good | 385(61.0) | 127 (61.1) | 258 (61.0) | |
| Fair | 113 (17.9) | 36 (17.3) | 77 (18.2) | |
| Poor | 6 (1.0) | 1 (0.5) | 5 (1.2) | |
| Chronic illness (N = 640) | ||||
| None reported | 388 (60.6) | 130 (62.2) | 258 (59.9) | <0.05b |
| Musculoskeletal | 96 (15.0) | 31 (14.8) | 65 (15.1) | |
| Mental health | 16 (2.5) | 0 (0) | 16 (3.7) | |
| Other | 140 (21.9) | 48 (23.0) | 92 (21.3) | |
| Work ability expectations (RTW-SE score) | 4.7 ± 1.3 | 4.9 ± 1.2 | 4.6 ± 1.4 | <0.01a |
| Experienced work-relatedness (N = 635) | ||||
| Yes | 210 (33.1) | 65 (31.3) | 145 (34.0) | 0.5b |
| Visits to GP/6 months (N = 593) | ||||
| No visits | 54 (9.1) | 14 (6.8) | 40 (10.3) | 0.37b |
| One visit | 148 (25.0) | 52 (25.4) | 96 (24.7) | |
| Two visits | 166 (28.0) | 58 (28.3) | 108 (27.8) | |
| Three or more visits | 225 (37.9) | 81 (39.5) | 144 (37.1) | |
| SA in year before baseline (N = 621) | ||||
| No absence | 211 (34.0) | 66 (31.7) | 145 (35.1) | 0.9b |
| 1 - 5 days | 220 (35.4) | 79 (38.0) | 141 (34.1) | |
| 6 - 10 days | 61 (9.8) | 20 (9.6) | 41 (9.9) | |
| 11 - 20 days | 44 (7.1) | 15 (7.2) | 29 (7.0) | |
| More than 20 days | 85 (13.7) | 28 (13.5) | 57 (13.8) |
Complete follow-up, workers who answered all three questionnaires; Incomplete follow up, workers who completed the first questionnaire and none or only one of the two follow-up questionnaires.
a P-value calculated using t-test;
b P-value calculated using a chi-square test.
Comparing the characteristics of the patients who experienced work-relatedness and the patients who did not, we found a statistically significant difference for experienced health, perceived work ability and prior SA. Patients who did not report work-relatedness experienced better health, had more positive work ability expectations and reported fewer days of SA in the preceding year (Table 2).
Table 2.
Comparison of baseline characteristics of patients who perceive their health problem as work-related and patients who do not; (%) N = 208* unless otherwise stated (2012–2013)
| Work-related (N = 65) | Not work-related (N = 143) | P value | |
|---|---|---|---|
| Age (mean ± SD) | 47.7 ± 8.7 | 46.1 ± 10.3 | 0.28 |
| Working hours/week (mean ± SD) | 32.7 ± 13.1 | 30.4 ± 10.1 | 0.16 |
| Gender | |||
| Female | 39 (60.0) | 84 (58.7) | 0.86 |
| Experienced health (N = 207) | |||
| Excellent | 1 (1.5) | 8 (5.6) | 0.04 |
| Very good | 7 (10.8) | 27 (19.0) | |
| Good | 39 (60.0) | 88 (62.0) | |
| Fair | 18 (27.7) | 18 (12.7) | |
| Poor | 0 (0.0) | 1 (0.7) | |
| Presence of chronic illness (N = 207) | |||
| Yes | 26 (40.0) | 53 (37.3) | 0.71 |
| Work ability expectations (RTW-SE score (mean ± sd)) | 4.5 ± 1.2 | 5.1 ± 1.1 | <0.01 |
| Visits to GP/6 months (N=204) | |||
| No visits | 2 (3.1) | 12 (8.6) | 0.12 |
| One visit | 14 (21.5) | 38 (27.3) | |
| Two visits | 16 (24.6) | 41 (29.5) | |
| Three or more visits | 33 (50.8) | 48 (34.5) | |
| SA in year before baseline (N=207) | |||
| No absence | 18 (27.7) | 48 (33.8) | <0.01 |
| 1–5 days | 19 (29.2) | 59 (41.5) | |
| 6–10 days | 4 (6.2) | 16 (11.3) | |
| 11–20 days | 11 (16.9) | 4 (2.8) | |
| More than 20 days | 13 (20.0) | 15 (10.6) |
Sd, standard deviation; RTW-SE, return-to-work self-efficacy (work ability expectations).
aOne of the patients with complete SA data had not answered the question about perceived work-relatedness. .
There was no significant difference between the geometric means of the number of SA days among the patients who experienced work-relatedness and the patients who did not: 1.6 (95% CI: 0.9–3.0) and 1.2 (95% CI: 0.8–1.8) respectively (P = 0.42). After adjustment for the other determinants the geometric means remained not significantly different: 1.8 (95% CI: 1.0–3.4) for the patients who experienced work-relatedness and 2.4 (95% CI: 1.4–4.0) for the patients who did not (P = 0.50). The percentage of patients with high SA (more than 20 days in 12 months) also did not differ significantly between the group who perceived work-relatedness (21.5%) and the group who did not (13.3%): (odds ratio 1.79; 95% CI: 0.84–3.84) (P = 0.13). After adjustment for the other determinants, the odds ratio for high SA did not significantly differ: 1.33 (95% CI: 0.56–3.15) (P = 0.52) (Table 4). The percentage of patients without SA during follow-up was similar in both groups: 46.2% and 43.4%, respectively (P = 0.71).
Table 4.
Results of logistic regression analysis to estimate the effect of the characteristics on the odds of high SA during follow up, N = 209 (2012–2014)
| Characteristic | Univariable analysis | Multivariable analysis | After backward elimination | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | β | OR (95%CI) | P value | β | OR (95%CI) | P value | β | |
| Work-relatedness | 1.79 (0.83–3.84) | 0.13 | 0.58 | 1.33 (0.56–3.15) | 0.52 | 0.28 | – | – | – |
| Age > 50 | 2.83 (1.32–6.07) | <0.01 | 1.04 | 2.37 (1.01–5.59) | <0.05 | 0.86 | 2.43 (1.08–5.46) | 0.03 | 0.89 |
| Male gender | 1.23 (0.58–2.60) | 0.58 | 0.21 | 0.86 (0.36–2.05) | 0.74 | −0.15 | – | – | – |
| Health fair or poor | 3.43 (1.50–7.83) | <0.01 | 1.23 | 1.22 (0.46–3.24) | 0.69 | 0.20 | – | – | – |
| Presence of chronic illness | 3.53 (1.62–7.67) | <0.01 | 1.26 | 2.72 (1.14–6.47) | 0.02 | 1.00 | 3.20 (1.42–7.23) | <0.01 | 1.16 |
| SA > 5 days | 4.04 (1.87–8.73) | <0.01 | 1.40 | 2.08 (0.84–5.12) | 0.11 | 0.73 | – | – | – |
| Visits to GP ≥ 3 | 2.24 (1.05–4.82) | 0.04 | 0.81 | 1.14 (0.47–2.76) | 0.76 | 0.14 | – | – | – |
| Low work ability expectations (RTW SE score ≤ 5) | 3.43 (1.51–7.80) | <0.01 | 1.23 | 2.52 (0.97–6.56) | 0.06 | 0.92 | 3.63 (1.54–8.54) | <0.01 | 1.29 |
OR, odds ratio; 95% CI, 95% confidence interval; β, regression coefficient.
The multivariable regression models showed that presence of a chronic illness, SA of 5 days or more during the year before baseline and low perceived work ability were statistically significantly positively associated with the number of SA days at follow-up (Table 3). Age over 50, presence of chronic illness and low perceived work ability were statistically significantly positively associated with high SA (Table 4). We found no interaction effect of allocation with any factors in the regression models.
Table 3.
Results of linear regression analysis to estimate the effect of the characteristics on SA days during follow-up, N = 209 (2012–2014)
| Characteristic | Univariable analysis | Multivariable analysis | After backward elimination | |||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | |
| Work-relatedness | 1.36 (0.64–2.89) | 0.42 | 0.78 (0.38–1.62) | 0.50 | – | – |
| Age > 50 | 2.10 (1.04–4.22) | 0.04 | 1.49 (0.75–2.94) | 0.25 | – | – |
| Male gender | 1.39 (0.69–2.80) | 0.36 | 1.09 (0.55–2.16) | 0.79 | – | – |
| Health fair or poor | 4.66 (1.93–11.25) | <0.01 | 1.49 (0.58–3.86) | 0.41 | – | – |
| Presence of chronic illness | 3.67 (1.84–7.32) | <0.01 | 2.53 (1.25–5.16) | 0.01 | 2.97 (1.52–5.75) | <0.01 |
| SA > 5 days | 5.37 (2.61–10.91) | <0.01 | 2.59 (1.16–5.81) | 0.02 | 3.03 (1.43–6.42) | <0.01 |
| Visits to GP ≥ 3 | 2.59 (1.28–5.21) | <0.01 | 1.32 (0.64–2.72) | 0.45 | – | – |
| Low work ability expectations (RTW-SE score ≤ 5) | 3.82 (1.95–7.39) | <0.01 | 2.51 (1.21–5.21) | 0.01 | 2.64 (1.35–5.21) | <0.01 |
Coefficient, linear regression coefficient; 95% CI, 95% confidence interval.
Discussion
Summary
We did not find statistically significant differences in the mean number of SA days or the cumulative incidence of high SA between the group of patients who experienced work-relatedness and the group who did not. The presence of chronic illness, prior SA of more than 5 days and low perceived work ability were positively associated with the number of days of SA at follow-up. The presence of chronic illness, age over 50 and low perceived work ability was positively associated with high SA at follow-up. One third of the patients in our sample experienced work-related problems. The percentage of patients without SA during follow-up was almost the same in the groups with and without perceived work-relatedness.
Strengths and limitations
To the best of our knowledge, this is the first prospective cohort study of the relation between work-relatedness as experienced by patients and ensuing SA in a population visiting the GP. A strength of our study is that patients were not selected based on the presence of work-related problems or SA. This allowed us to study the phenomenon of SA in a relatively healthy population, and sheds light on the many cases where SA does not become ‘problematic’ or does not occur at all. For instance, many patients continue their work, in spite of experiencing their health problem as work-related. On the other hand, even in this relatively small and healthy population, we could identify four variables which may be used by GPs to identify patients at an increased risk of SA.
There are some limitations as well. First, in our study, we have used self-reported SA. Compared with record-based methods, self-reporting SA leads to underreporting (30). However, self-reported SA data are sufficiently valid to be used to investigate the relative effect of different variables on SA, as we did in our study (30). Second, in our questionnaires, we have used self-reported SA days over the last 6 months to monitor SA. Our data did not allow us to differentiate between one or more spells of absence. Hence, we have chosen to use ‘high sickness absence’ rather than the more commonly used ‘long term sickness absence’. The cut off at 20 days is the same as the cut-off for long-term SA which is used in the UK NICE guidance (27). Moreover, it is congruent with the highest category of the baseline characteristic ‘Number of days of sickness absence during the last year’. Third, the results of this study are based on a secondary analysis of data which were not collected for the purpose of a prospective cohort study which limits the generalisability. Fourth, with respect to the participants the study suffered from two sources of bias: selection bias and attrition bias. Concerning selection bias, we have found that non-responders were younger, more often male and worked more hours per week. This suggests that they may be healthier and, possibly, having less experience with SA and visits to the GP, may also have been less convinced of the relevance of our study. Concerning attrition bias, participants with complete follow up were slightly older, had no chronic mental illness and slightly better-perceived work ability. The loss to follow up of all patients who reported mental health problems has probably resulted in an underestimation of SA because mental health problems are associated with high SA (31). We assume that the other differences in patient characteristics were not clinically relevant enough to have influenced the results of our analysis. Fifth, the relatively short period during which patients were followed is another limitation as it is known that work-related problems can be lingering on for years before they result in manifest health problems or SA (32).
Comparison with the literature
Authors of a recent review about person-related factors associated with SA found that experienced work-relatedness was associated with SA in some studies whereas an association was absent in other studies (13). We found no association between experienced work-relatedness and SA, but our data corroborate the importance of chronic illness, prior SA, perceived work ability and age as determinants of SA (2–4,9–14,28). The proportion of patients who experienced work-relatedness is congruent with the findings of other studies; a recent French study found that 24% of working-age patients who visited their GP, had work-related common mental health problems (17–20). In our study, low perceived work ability was associated with SA days and high SA. This indicates that it is important that GPs explore patients’ work ability. Possibly, the Return-to-Work Self-Efficacy scale might play a role here (12,28,33). We found no statistically significant relationship between gender and perceived work-relatedness. This contrasts with the results of a large study in 17 European countries over a period 1998–2008 which found that women were on average 30% more absent than men (34). The authors attributed this difference to the low quality of jobs women tend to be employed in. Many of the participants in our study were permanently employed and relatively highly educated which may explain that we did not find an effect of gender.
Implications for practice and future research
Although we did not find a statistically significant association between experienced work-relatedness and SA, the high percentage of the patients who perceived work-relatedness underlines the importance of an exploration of this field by the GP during the consultation. In addition, our results show that GPs have excellent opportunities for early recognition of a higher risk of SA, as they can easily assess the presence of the predictive factors higher age, chronic illness, prior SA and perceived work ability. At the moment many GPs still seem reluctant to discuss work with their patients and tend to underestimate the work-relatedness of health problems (24,35). Therefore, it might be necessary to teach GPs more about this subject and develop programs to help them discuss work-relatedness, SA and work ability with their patients. Experiences in the UK with GPs specializing in this field show promising results (19,35).
Further research is needed about how to systematically collect data about work-related problems, about the precise role of predictive factors concerning SA and how to optimally use this information in reducing or preventing SA, and about how to teach GPs in exploring and managing work-related factors.
Conclusion
We did not find an association between experienced work-relatedness and SA but found associations between SA and age over 50, presence of chronic illness, prior SA and perceived work ability. GPs have excellent opportunities to assess these factors, in order to contribute to the prevention or reduction of SA.
Acknowledgement
The authors wish to thank all participating patients, GPs, practice receptionists and research assistants for making this study possible.
Declaration
Funding: This work was supported by Foundation Institute Gak, which funded the randomized controlled trial from which the data of this study originated [grant number 2008–762].
Ethical approval: The institutional medical research ethics committee (MREC) concluded that the ‘Medical Research Involving Human Subjects Act’ did not apply to our study (letter MREC 6 April 2011).
Conflict of interest: none.
References
- 1. Sieurin L, Josephson M, Vingård E. Positive and negative consequences of sick leave for the individual, with special focus on part-time sick leave. Scand J Public Health 2009; 37: 50–6. [DOI] [PubMed] [Google Scholar]
- 2. Helgesson M, Johansson B, Wernroth L, Vingård E. Exposure to different lengths of sick leave and subsequent work absence among young adults. BMC Public Health 2016; 16: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sumanen H, Pietiläinen O, Lahelma E, Rahkonen O. Short sickness absence and subsequent sickness absence due to mental disorders - a follow-up study among municipal employees. BMC Public Health 2017; 17: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Helgesson M, Johansson B, Nordqvist T, Lundberg I, Vingård E. Sickness absence at a young age and later sickness absence, disability pension, death, unemployment and income in native Swedes and immigrants. Eur J Public Health 2015; 25: 688–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lännerström L, Wallman T, Holmström IK. Losing independence–the lived experience of being long-term sick-listed. BMC Public Health 2013; 13: 745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Edwards A, Greasley K.. Absence from work. Dublin: European Foundation for the Improvement of Living and Working Conditions, 2010. [Google Scholar]
- 7. Waddell G, Burton AK.. Is work good for your health and well-being? London: The Stationery Office, 2006. [Google Scholar]
- 8. Van Hedel K, Van Lenthe FJ, Avendano M et al. Marital status, labour force activity and mortality: a study in the USA and six European countries. Scand J Public Health 2015; 43: 469–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Roelen C, Thorsen S, Heymans M, Twisk J, Bültmann U, Bjørner J. Development and validation of a prediction model for long-term sickness absence based on occupational health survey variables. Disabil Rehabil 2018; 40: 168–75. [DOI] [PubMed] [Google Scholar]
- 10. Boot C, Van Drongelen A, Wolbers I, Hlobil H, Van der Beek A, Smid T. Prediction of long-term and frequent sickness absence using company data. Occup Med (Lond) 2017; 67(3): 176–81. [DOI] [PubMed] [Google Scholar]
- 11. Airaksinen J, Jokela M, Virtanen M et al. Prediction of long-term absence due to sickness in employees: development and validation of a multifactorial risk score in two cohort studies. Scand J Work Environ Health 2018; 44: 274–82. [DOI] [PubMed] [Google Scholar]
- 12. Nieuwenhuijsen K, Noordik E, van Dijk FJ, van der Klink JJ. Return to work perceptions and actual return to work in workers with common mental disorders. J Occup Rehabil 2013; 23: 290–9. [DOI] [PubMed] [Google Scholar]
- 13. de Wit M, Wind H, Hulshof CTJ, Frings-Dresen MHW. Person-related factors associated with work participation in employees with health problems: a systematic review. Int Arch Occup Environ Health 2018; 91: 497–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Etuknwa A, Daniels K, Eib C. Sustainable return to work: a systematic review focusing on personal and social factors. J Occup Rehabil 2019:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. OECD. Sickness, Disability and Work: Breaking the Barriers; A Synthesis of Findings Across OECD Countries. Paris: OECD Publishing, 2010. [Google Scholar]
- 16. Dutch College of General Practitioners: Position paper on core values of general practice. Generalist, person centered and continuous [Nederlands Huisartsen Genootschap. NHG-Standpunt Kernwaarden huisartsgeneeskunde. Generalistisch, persoonsgericht en continu.]. Utrecht: NHG, 2011. [Google Scholar]
- 17. Harber P, Mullin M, Merz B, Tarazi M. Frequency of occupational health concerns in general clinics. J Occup Environ Med 2001; 43: 939–45. [DOI] [PubMed] [Google Scholar]
- 18. Weevers HJ, van der Beek AJ, Anema JR, van der Wal G, van Mechelen W. Work-related disease in general practice: a systematic review. Fam Pract 2005; 22: 197–204. [DOI] [PubMed] [Google Scholar]
- 19. Hussey L, Turner S, Thorley K, McNamee R, Agius R. Work-related ill health in general practice, as reported to a UK-wide surveillance scheme. Br J Gen Pract 2008; 58: 637–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rivière M, Plancke L, Leroyer A et al. Prevalence of work-related common psychiatric disorders in primary care: the French Héraclès study. Psychiatry Res 2018; 259: 579–86. [DOI] [PubMed] [Google Scholar]
- 21. Buijs P, Gunnyeon B, van Weel C. Primary health care: what role for occupational health? Br J Gen Pract 2012; 62: 623–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. de Kock CA, Lucassen PLBJ, Bor H et al. Training GPs to improve their management of work-related problems: results of a cluster randomized controlled trial. Eur J Gen Pract 2018; 24: 258–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. de Kock CA, Lucassen PL, Spinnewijn L et al. How do dutch GPs address work-related problems? A focus group study. Eur J Gen Pract 2016; 22: 169–75. [DOI] [PubMed] [Google Scholar]
- 24. Hooftman W, Mars G, Janssen B, De Vroome E, Pleijers A, Michiels J.. Nationale Enquête Arbeidsomstandigheden (NEA) 2016. Methodologie en Globale Resultaten [The Netherlands Working Conditions Survey 2016: methodology and Overall Results]. Hoofddorp: TNO; 2016. [Google Scholar]
- 25. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014; 12: 1495–9.25046131 [Google Scholar]
- 26. de Kock KA, Steenbeek R, Buijs PC, Lucassen PL, Knottnerus JA, Lagro-Janssen AL. An education programme to increase general practitioners’ awareness of their patients’ employment: design of a cluster randomised controlled trial. BMC Fam Pract 2014; 15: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. National Institute for Health and Clinical Excellence. Public health guidance 19. Management of long-term sickness absence and incapacity for work. London: National Institute for Health and Clinical Excellence; 2009. http://guidance.nice.org.uk/PH19 (accessed 5 February 2019) [Google Scholar]
- 28. Lagerveld SE, Blonk RW, Brenninkmeijer V, Schaufeli WB. Return to work among employees with mental health problems: development and validation of a self-efficacy questionnaire. Work Stress 2010; 24(4): 359–75. [Google Scholar]
- 29. Ware JE Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol 1998; 51: 903–12. [DOI] [PubMed] [Google Scholar]
- 30. Johns G, Miraglia M. The reliability, validity, and accuracy of self-reported absenteeism from work: a meta-analysis. J Occup Health Psychol 2015; 20: 1–14. [DOI] [PubMed] [Google Scholar]
- 31. de Vries H, Fishta A, Weikert B, Rodriguez Sanchez A, Wegewitz U. Determinants of sickness absence and return to work among employees with common mental disorders: a scoping review. J Occup Rehabil 2018; 28: 393–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Whittaker W, Sutton M, Maxwell M et al. Predicting which people with psychosocial distress are at risk of becoming dependent on state benefits: analysis of routinely available data. BMJ 2010; 341: c3838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lagerveld SE, Brenninkmeijer V, Blonk RW, Twisk J, Schaufeli WB. Predictive value of work-related self-efficacy change on RTW for employees with common mental disorders. Occup Environ Med 2017; 74: 381–3. [DOI] [PubMed] [Google Scholar]
- 34. Melsom AM, Mastekaasa A. Gender, occupational gender segregation and sickness absence: longitudinal evidence. Acta Sociol 2018; 61(3): 227–45. [Google Scholar]
- 35. Hussey L, Turner S, Thorley K, McNamee R, Agius R. Work-related sickness absence as reported by UK general practitioners. Occup Med (Lond) 2012; 62: 105–11. [DOI] [PubMed] [Google Scholar]