Abstract
Case series
Patients: Male, 25-year-old • Male, 29-year-old • Female, 39-year-old • Male, 32-year-old
Final Diagnosis: Folliculitis
Symptoms: Rash
Medication: —
Clinical Procedure: Sleeve gastrectomy
Specialty: Dermatology • Surgery
Objective:
Unusual clinical course
Background:
Obesity is one of the leading causes of preventable death worldwide. Due to its increasing incidence and the difficulty in reducing its morbidity and mortality using nonsurgical methods, the demand for bariatric surgery has risen in recent times. Sleeve gastrectomy is one of the most common types of bariatric surgery, and like any other surgery, it carries a series of risks.
Case Reports:
Although complications such as gastrointestinal leaks are widely reported, there is limited literature available on cutaneous complications. Here, we report 4 cases of patients showing a peculiar skin rash 2–4 weeks following sleeve gastrectomy. We also discuss some of the mechanisms that may underlie this correlation.
Conclusions:
There is a need for further epidemiological studies to determine the prevalence of this rash. Further studies are also needed to determine the exact etiology of this rash.
MeSH Keywords: Bariatric Surgery; Gastrectomy; Obesity, Morbid
Background
Obesity is one of the biggest health problems in the modern age. It has a massive impact on both morbidity and mortality. Not only does it increase the risk of diabetes and cardiovascular disease, it is now one of the leading causes of death worldwide [1]. Many approaches have been used to reduce obesity and its catastrophic effects on today’s society, including education, dieting, exercise, and drugs. However, with its increasing incidence and severity, these nonsurgical methods do not suffice for some patients, so the demand for bariatric surgery has risen [2].
There are 3 main types of bariatric surgery:
Restrictive procedures: including laparoscopic adjustable gastric banding, laparoscopic sleeve gastrectomy, and vertical banded gastroplasty. These procedures effectively reduce the gastric lumen to induce early satiety [1,2].
Malabsorptive procedures: including jejunoileal bypass, which aims to decrease the amount of nutrients absorbed by reducing the surface area of the intestine exposed to food [1,2].
Combined restrictive-malabsorptive procedures: including Roux-en-Y gastric bypass [1,2].
Despite their ability to aid weight loss and improve mortality and morbidity rates in previously morbidly obese individuals, bariatric surgery can result in a range of complications. Although complications such as gastrointestinal leaks and intraabdominal abscesses are widely reported, [3,4] there is limited literature available on cutaneous complications. Here, we report 4 cases of patients with no other significant medical history showing a peculiar skin rash 2–4 weeks following sleeve gastrectomy, the most common subtype of bariatric surgery. The 4 patients were of Saudi Arabian descent, seen at the Suwaidi Hospital of the Habib Medical Group, Riyadh.
Because the clinical state of the presenting skin rash is rapidly self-limiting, the significance of this topic is more deeply rooted in academic interest. Nonetheless, by defining the rash and determining its association with sleeve gastrectomy, it may be possible to target it for treatment and to implement prophylactic measures before any visible dermatological manifestations occur. More broadly, defining this condition provides a basis for recognition by doctors in order to alert bariatric patients of this possible adverse effect of surgery, thereby improving doctor-patient trust by transparency.
Case Reports
Case 1
A 25-year-old man presented with a history of extensive multiple maculopapular erythematous skin rash, which started 3 weeks after sleeve gastrectomy. Before the surgery, a vitamin B12 injection was given to the patient prophylactically. There were no trace elements or vitamin deficiencies present at this time (including vitamin A and zinc). After the surgery, the rash presented all over the body, starting on the chest, spreading to the face, buttocks, trunk, and upper limbs. The rash had 2 distinguishable morphologies – the lesion on the face was clinically typical of a folliculitis rash (Figure 1B), but the remaining lesions, including the abdomen and the back (where the biopsies were taken), revealed spongiotic dermatitis (Figure 1A, 1C). The histopathology analysis showed parakeratosis with underlying interface lymphocytic infiltrate associated with vacuolar degeneration of basal cells, necrotic keratinocytes, extravasated red blood cells, perivascular lymphocytes, and scattered eosinophils. Therefore, a diagnosis of dermatitis of the trunk was made. A biopsy of the facial lesions was not taken. Apart from slightly low vitamin D levels, blood tests were unremarkable. And, apart from a previously high BMI (42 Kg/m2), the patient was otherwise well, with no signs of insulin resistance, hyper-tension, or hypercholesterolemia. The patient had no known allergies. Betamethasone and fusidic acid were given for the body rash and Clindamycin solution was given for the face rash. This produced a dramatic improvement by the second visit.
Figure 1.
Case 1: Widespread rash 3 weeks after surgery. Erythematous maculopapular rash on the chest and abdomen (A), forehead (B), and back (C).
Case 2
A 29-year-old man presented with a history of sudden eruption of maculopapular erythematous lesions, mainly on the face, neck, and upper chest, 3 weeks after sleeve gastrectomy (Figure 2). Clinically, a preliminary diagnosis of folliculitis was made. The surgery was performed in Jordan 3 weeks prior to consultation. His medical records showed a previous BMI of 40 kg/m2, without any co-morbidities. Blood tests were unre-markable, including normal vitamin and trace element levels. The were no known allergies. To confirm the post-surgical rash, a punch biopsy performed, which showed moderate inflammatory infiltrate of neutrophils and lymphocytes in the follicular ostium, confirming the diagnosis. The patient was started on Vibramycin 100 mg once a day for a month with betamethasone and fusidic acid cream twice a day for the upper chest and Clindamycin for the face. The patient came for a checkup 3 weeks later, showing complete healing (Figure 3), and was therefore discharged.
Figure 2.
Case 2: Presentation before treatment. Erythematous papules on the back (A), forehead (B) and left side of the neck (C).
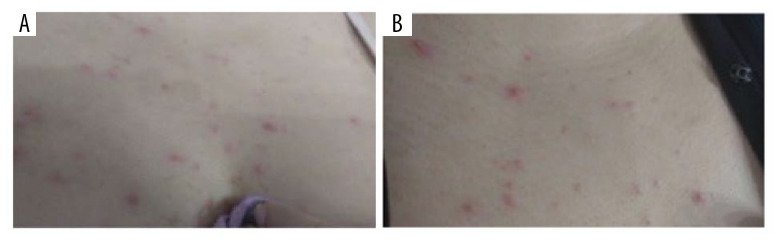
Figure 3.

Case 2: Presentation after treatment. Improvement of the skin rash with resolution of the papules, as shown in both the back (A) and the left side of the neck (B).
Case 3
A 39-year-old woman presented with a sudden eruptive rash on the upper chest and both sides of the neck just 2 weeks after a sleeve gastrectomy (previous BMI 40 Kg/m2). The rash displayed an erythematous follicular pattern, indicating folliculitis (Figure 4). We requested a biopsy to confirm the diagnosis, but this was unfortunately refused by the patient. Before surgery, vitamin and trace element levels were normal, and prophylactic supplements of vitamin B12 were given. After the surgery, blood tests were unremarkable. The patient had no known allergies. Vibramycin 100 mg once a day was given for 2 weeks, with betamethasone and fusidic acid cream twice daily. The patient returned 2 weeks later with complete healing of lesions but with post-inflammatory hyperpigmentation. Whitening cream was given, which was very effective.
Figure 4.
Case 3: Presentation before treatment. Papular rash on the chest (A, B).
Case 4
A 32-year-old man presented with a severe eruptive rash on his trunk, chest, and face, which developed 4 weeks after sleeve gastrectomy (previous BMI 40 kg/m2). The lesions in this patient were also follicular (Figure 5), which was later confirmed by histology. Like the previous patients, there were no known co-morbidities or allergies, and blood tests were unremarkable before and after surgery. Doxycycline 100 mg once a day was given for 1 month with Clindamycin solution. The patient returned in 3 weeks with complete healing.
Figure 5.
Case 4: Presentation before treatment. Maculopapular rash on the back (A), chest (B) and left side of the neck (C).
Discussion
It is reported that obese patients have a worse dermatological outcome to cosmetic surgery compared to non-obese patients [1] due to impaired wound healing in obese patients [6]. This is possibly due to poorer cutaneous health in obese individuals, who have a higher incidence of acne and hirsutism as well as certain dermatoses such as lichen sclerosis, scleroderma, and livedo reticularis [5]. Here, we report 4 patients developing a skin rash within 2–4 weeks after receiving a sleeve gastrectomy. It is of academic interest to understand the mechanism possibly underlying this relationship, which would not only help define the link, but may also aid in preventing the manifestation of a condition that has significant psychosocial impact on the patient and their quality of life.
Although the reported association may just be that (an association), several studies have reported this phenomenon of acute cutaneous skin reactions after bariatric surgery [6–9]. However, the mechanism underlying these cutaneous changes is unknown, and a range of theories have been put forward.
Given that the flare up of the rash starts at random sites on the body, including the face and neck, and is normally widespread, it is unlikely that the inflammation secondary to trauma from surgery is causing the outbreak. Therefore, the mechanism underlying this association is likely to be systemic. This is supported by the fact that doxycycline has been used successfully to reverse the cutaneous manifestation in previous cases [7].
Although testosterone levels were not directly investigated in this retrospective study, we propose that a rise in testosterone levels secondary to a change in the gut flora may be driving the outburst of the rash in our patients. Given that the patients did not report shaving or any other form of aggravation at the site of the rash, we believe testosterone levels are likely to play a role here, especially given that most of the cases we reported were males, who normally have a higher baseline level of testosterone compared to females. The reasoning behind this is based on the fact that obese individuals tend to have lower testosterone levels [10] and given the established link between androgen levels and folliculitis [11], it is possible that a surge in testosterone levels 2–4 weeks after bariatric surgery causes a folliculitis outbreak. It is plausible that abdominal surgery on the stomach upsets the gut flora, which consequently affects testosterone levels in the body.
On the other hand, a recent study in mice showed that 2–4 weeks is sufficient time for gut flora to change the levels of testosterone significantly enough to increase the size of the testes. To test specific effects of probiotics, Poutahidis et al. show that outbred Swiss mice on normal (control) diet given Lactobacillus reuteri at 2 months of age had statistically significant rise in testosterone levels and testes size within 1 month [12]. The role of gut flora in changing androgen levels is supported by Ridlon et al., who found that Clostridium scin-dens, which form part of the human gut flora, contains the necessary genes to encode the enzyme required for androgen production from cortisol [13].
It is likely that sleeve gastrectomy is able to drive the growth of androgen-producing bacteria, which are consequently able to produce enough androgens to drive folliculitis. In a recent study comparing 30 obese men with a BMI of 30–45 kg/m2 undergoing laparoscopic sleeve gastrectomy, Gao et al. found that after an average decrease of approximately 10 kg/m2 in BMI, testosterone levels almost doubled (statistically significant) [10]. However, these changes were measured 6 months after surgery, and it is unlikely that levels of testosterone are doubled within 1 month. Nonetheless, given that the skin is in a constant state of inflammation and susceptible to pathological change, it is plausible that the small increases in androgen levels that are likely to exist in the short time frame are able to tip the balance enough for cutaneous manifestation, but not enough for effects such as gynecomastia to be seen. Ideally, studies measuring testosterone levels in patients like those studied by Gao et al. should be done in the first few weeks after bariatric surgery to explore the link further.
Limitations
The sample size here is very small, only including 4 reported cases. Therefore, although 75% of patients presented with folliculitis in this report, the population from which the patients were sampled may show a stronger weighting towards dermatitis. Secondly, we need to acknowledge that patients were assessed under the umbrella term of folliculitis, when subtype stratification may also be important. This is important because the known etiology of these conditions is not the same; therefore, the mechanisms underlying the possible association between bariatric surgery and folliculitis may be different. Nonetheless, despite these differences, the common denominator is skin manifestations in a large proportion of patients after bariatric surgery, manifesting within 4 weeks. Hence, this may be a unifying mechanism, as discussed.
Thirdly, all patients reported were of the same Saudi Arabian ethnicity, but it is known that the distribution of skin conditions varies with ethnicity, with a role for both genetics and the environment. We also did not control for confounding by lifestyle factors. This is significant, especially given that it is understood that various factors such as stress, smoking, and diet can have a range of effects on the skin. Furthermore, patients in need of bariatric surgery were randomly sampled, and pre-surgical factors of weight, body mass index (BMI), and secondary conditions were not taken into account. For example, one of the cases had his surgery abroad in Jordan, where the criteria for bariatric surgery appear to differ. Finally, the follow-up only extended as far as hospital visits for therapy. More specifically, it was assumed in the patient with post-surgical dermatitis that there was complete elimination of the skin rash, but without follow-up, there is no confirmation.
Finally, we must take care in extrapolating our findings to all patients developing a skin rash following bariatric surgery, especially given that some evidence shows variation in cutaneous manifestation between the subtypes of bariatric surgeries. For example, Shope et al. found that there is an increased incidence of infection in circular-stapled anastomoses compared to linear-stapled anastomoses in laparoscopic Rouxen-Y gastric bypass [14].
Conclusions
As a result of the increase in incidence in bariatric surgery, rarer and less frequent complications of these procedures are more likely to become apparent. Here, we describe a possible complication of a peculiar rash developing several weeks after surgery. Currently, we only have a collection of case studies with a few plausible explanations for this presentation. However, the clinical significance (if any) of this relationship needs to be assessed by further epidemiological studies and randomized clinical trials. After defining this association and its pathogenesis, we might be able to treat it effectively and ultimately prevent it.
Footnotes
Department and Institution where work was done
This work was done in the Suwaidi Hospital of the Habib Medical Group, Riyadh, Kingdom of Saudi Arabia.
Conflicts of interest
None.
References:
- 1.Halawi A, Abiad F, Abbas O. Bariatric surgery and its effects on the skin and skin diseases. Obes Surg. 2013;23(3):408–13. doi: 10.1007/s11695-012-0859-x. [DOI] [PubMed] [Google Scholar]
- 2.Paula A, Manzoni S, Weber M. Skin changes after bariatric surgery. An Bras Dermatol. 2015;90(2):157–66. doi: 10.1590/abd1806-4841.20153139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Papavramidis T. Complications after vertical gastroplasty artificial pseudo-pylorus in the treatment morbid obesity: A 7-year experience. Obes Surg. 1999;9(6):535–38. doi: 10.1381/096089299765552620. [DOI] [PubMed] [Google Scholar]
- 4.Mason E, Renquist E. Perioperative risks and safety of surgery for severe obesity. Am J Clin Nutr. 1992;55(2):573S–76S. doi: 10.1093/ajcn/55.2.573s. [DOI] [PubMed] [Google Scholar]
- 5.Shipman A, Millington GWM, Millington G. Obesity and the skin. Br J Dermatol. 2011;165(4):743–50. doi: 10.1111/j.1365-2133.2011.10393.x. [DOI] [PubMed] [Google Scholar]
- 6.Michaels J, Coon D, Rubin J. Complications in postbariatric body contouring: Postoperative management and treatment. plastic and reconstructive surgery. 2011;127(4):1693–700. doi: 10.1097/PRS.0b013e31820a649f. [DOI] [PubMed] [Google Scholar]
- 7.Monshi B, Vigl K, Weihsengruber F. Phrynoderma and acquired acrodermatitis enteropathica in breastfeeding women after bariatric surgery. J Dtsch Dermatol Ges. 2015;13(11):1147–54. doi: 10.1111/ddg.12795. [DOI] [PubMed] [Google Scholar]
- 8.Farias MM, Gajardo C, Alvarez V, et al. Short-term skin reactions associated to sleeve gastrectomy in eight patients. Obes Surg. 2014;24(10):1826–29. doi: 10.1007/s11695-014-1381-0. [DOI] [PubMed] [Google Scholar]
- 9.Stephan F, Haber R, Maalouf D, Tomb R. A case of dermatitis herpetiformis after a mini-gastric bypass surgery. J Am Acad Dermatol. 2014;71(1):e18–20. doi: 10.1016/j.jaad.2014.01.854. [DOI] [PubMed] [Google Scholar]
- 10.Gao J, Zhang M, Zhu C, et al. The change in the percent of android and gynoid fat mass correlated with increased testosterone after laparoscopic sleeve gastrectomy in Chinese obese men: A 6-month follow-up. Obes Surg. 2018;28(7):1960–65. doi: 10.1007/s11695-018-3116-0. [DOI] [PubMed] [Google Scholar]
- 11.Arora MK, Yadav A, Saini V. Role of hormones in acne vulgaris. Clin Biochem. 2011;44(13):1035–40. doi: 10.1016/j.clinbiochem.2011.06.984. [DOI] [PubMed] [Google Scholar]
- 12.Poutahidis T, Springer A, Levkovich T, et al. Probiotic microbes sustain youthful serum testosterone levels and testicular size in aging mice. PLoS One. 2014;9(1):e84877. doi: 10.1371/journal.pone.0084877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ridlon JM, Ikegawa S, Alves J, et al. Clostridium scindens: A human gut microbe with a high potential to convert glucocorticoids into androgens. J Lipid Res. 2013;54(9):2437–49. doi: 10.1194/jlr.M038869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shope TR, Cooney RN, Mcleod J, et al. Early results after laparoscopic gastric bypass: EEA vs. GIA stapled gastrojejunal anastomosis. Obes Surg. 2003;13(3):355–59. doi: 10.1381/096089203765887651. [DOI] [PubMed] [Google Scholar]