Abstract
Acute respiratory infections (ARI) are a major public health problem and one of the commonest reasons for visiting primary health care centers (PHC). In developing countries, seventy-five percent of the cases are treated with antibiotics, although the majority are caused by viral infection. Our aim was to observe the pattern of physician practices with respect to ARI, in comparison to WHO protocols and to provide recommendations for health promotion enhancement. The study was conducted in Makkah PHC centers, for 2 months. A total 14 PHC centers were randomly selected. And 908 prescriptions were obtained randomly from general practitioners (GP) and analyzed. We found that males were 522 and females were and 386. Weights were not recorded in 224 (24.7%) cases. In 87 cases (9.6%) no diagnosis was recorded. In 515 (62.34%) of cases, antibiotics were prescribed; most of these cases were of simple common cold, with antibiotics not recommended. To conclude, many physicians in Makkah are not following the WHO guidelines for Acute Respiratory Infection. Educational health programs should be conducted to sensitize the physicians regarding the appropriate method of diagnosis and rational use of antibiotics.
1. INTRODUCTION
Acute respiratory infections (ARI) are considered one of the foremost public health problems [1] and are the leading cause for morbidity and mortality in several developing countries [2]. They have been estimated to cause 18–33% of all deaths of children below five years. Half of deaths in developing countries is among children under five years of age [3]; this is 10–50 times more than developed countries with the same ARI cause [4]. Acute respiratory infections (ARI) in children constitute approximately 30–60% of PHC visits around the world; they cause 20–30% of hospital admissions [5]. At least one respiratory virus is found in 15% of hospitalized children [6]. Pneumonia is responsible for more deaths of children than other illnesses – more than HIV, malaria and measles combined [7]. In addition, it is one of the commonest reasons for visits to the primary care physician [8]. The prevalence of acute respiratory infection in children is 24% in Saudi Arabia [9]. The causes for ARIs vary from self-limiting conditions such as the common cold to the more serious bacterial pneumonia. Even though the majority of cases are viral [10–12], three-quarters of antibiotics consumed are for ARIs, which has contributed to the emergence of drug-resistant bacterial pathogens, serious side effects, and a significant waste of health care resources [8]. An important concern is the inappropriate use of antibiotics for non-bacterial infections and for self-limiting clinical conditions [13]. The prescription of antibiotic in primary health care centers (PHC) is high [14]. Some of the studies reported antibiotic prescription as high as, 66%, 58.8% and 56% [15–18]. Despite the very fact that the majority infections treated at this level of care are of self-limiting in nature [19–21], there’s an overuse of antimicrobial treatments [22–24]. Therefore, assessing healthcare providers prescribing patterns is essential, as there is limited data regarding this issue [25].
Another matter of concern is of prescribed antibiotic [26–29]. This has serious consequences: exposing the patients to adverse effects, increase of number of visits for mild issues [14,26,30], and development of resistant bacterium strains [14,31]. Infections caused by resistant bacterium are related to bigger morbidity and mortality rates, and health care resources wasting. [30,32].
The World Health Organization (WHO) has developed a protocol for the management of ARI, particularly for developing countries such as Saudi Arabia, the protocol includes the revised recommendations: A) Children with fast breathing pneumonia with no chest in drawing or general danger sign should be treated with oral amoxicillin. B) Children age 2–59 months with chest in drawing pneumonia should be treated with oral amoxicillin C) Children aged 2–59 months with severe pneumonia should be treated with parenteral ampicillin (or penicillin) and gentamicin as a first-line treatment. D) Ampicillin (or penicillin when ampicillin is not available) plus gentamicin or ceftriaxone are recommended as a first-line antibiotic regimen for HIV-infected and -exposed infants and for children under 5 years of age with chest in drawing pneumonia or severe pneumonia. E) Empiric cotrimoxazole treatment for suspected Pneumocystis jirovecii (previously Pneumocystiscarinii) pneumonia (PCP) is recommended as an additional treatment for HIV-infected and -exposed infants aged from 2 months up to 1 year with chest in drawing or severe pneumonia. F) Empirical cotrimoxazole treatment for Pneumocystis jirovecii pneumonia (PCP) is not recommended for HIV-infected and -exposed children over 1 year of age with chest in drawing or severe pneumonia. [33]. This study was conducted to observe the pattern of physicians’ prescriptions, to determine their practices related to ARI management and compliance with WHO protocols, and to provide recommendations to enhance their practices in primary health care centers.
2. METHODS
2.1. Study Setting
The study was conducted in Primary Health Care Centres (PHC) of Makkah Al Mukarramah, Saudi Arabia.
2.2. Study Design
A cross-sectional study, conducted from 1/2/2016 to 31/3/2016.
2.3. Sample Size
The sample size was calculated using the online software of Epi Info, developed by the Centers for Disease Control and Prevention (CDC), using a confidence level of 95%. As our technique was cluster sampling we chose a design effect of 2.0. The estimated sample size was 769. An additional 20% (154) was added to account for dropouts, because of possibility of refusal of any PHC physician to participate in the study with a final total of 923. (For details please, see Appendix A below).
2.4. Sampling Procedure
The sampling technique used was Multistage cluster sampling, to select PHC centers during the first phase of the study, then to select registered physicians in the second phase of the study and then later to select their prescriptions. After obtaining the list of all PHC centers of Makkah from the Ministry of Health, we randomly selected 20% of the PHC centers with the help of Statistical Package for the Social Sciences software (SPSS) version 21. As there are 70 PHC centers in Makkah, a total 14 PHC centers were selected. From each selected PHC center we randomly selected general practitioners and from each physician we randomly selected their prescriptions for ARI. After obtaining their consent, a total of 908 prescriptions were collected by going to clinic daily and collecting the prescriptions. We compared the prescriptions with WHO guidelines recommendations for acute respiratory infections [33]. The main variables assessed, beside basic demographic characteristics, included: chief complaints, temperature, pulse rate, respiratory rate, provisional diagnosis and the type of antibiotic prescribed. All variables were entered into the computer and analyzed by SPSS version 21.
The protocol was submitted to IRB of College of Medicine and ethical approval was obtained as HAPO-02-K-012-2016-02-142.
3. RESULTS
A total of 923 prescriptions were planned, whereas 908 prescriptions were collected, as one of the physician refused to participate in the study. The majority of children, 558/908 (61.5%), were seen in public PHC centers and 350/908 (38.5%) of them were in private PHC centers. By gender, more than half of the cases were males i.e. 522/908 (57.5%) and females accounted for 386/908 (42.5%). (Table 1).
Table 1.
Profile of children presenting to PHCs with acute resiratory infection, Makkah, KSA, 2016.
| Variables | Number of cases | Percentage (%) |
|---|---|---|
| Age (Years) | ||
| Less than 1 | 69 | (7.6%) |
| 1–5 | 289 | (31.8%) |
| 6–10 | 258 | (28.4%) |
| 11–15 | 161 | (17.7%) |
| 16–18 | 131 | (14.4%) |
| More than 18 | 0 | (0%) |
| Gender | ||
| Male | 522 | (57.5%) |
| Female | 386 | (42.5%) |
| Type of center | ||
| Public | 558 | (61.5%) |
| Private | 350 | (38.5) |
| Chief complaint | ||
| Fever | 120 | 120 (13.2%) |
| Cough | 75 | 75 (8.3%) |
| Runny nose | 24 | 24 (2.6%) |
| Sore throat | 13 | 13 (1.4%) |
| More than one respiratory symptom | 569 | 569 (62.7%) |
| Others | 68 | (7.5%) |
| Not written | 39 | (4.3%) |
| Physical examination | ||
| Congested throat | 121 | (13.3%) |
| Ear problems | 51 | (5.6%) |
| Pharyngeal tonsillar erythema | 99 | (10.9%) |
| Tonsillar exudate | 35 | (3.9%) |
| More than one respiratory finding | 188 | (20.7%) |
| Others | 55 | (6.1%) |
| Not written | 359 | (39.5%) |
| Clinical diagnosis | ||
| Pneumonia with tachypnea, with no costal retractions or general danger signs | 15 | (1.7%) |
| Pneumonia with costal retractions | 5 | (0.6%) |
| Severe pneumonia | 1 | (0.1%) |
| Common cold | 227 | (25.0%) |
| Upper respiratory tract infection | 103 | (11.3%) |
| Allergic asthma | 11 | (1.2%) |
| Tonsillitis and pharyngitis | 35 | (3.9%) |
| Bronchial asthma | 11 | (1.2%) |
| Pharyngitis | 123 | (13.5%) |
| Lower respiratory tract infection | 9 | (1.0%) |
| Tonsillitis | 104 | (11.5%) |
| Otitis media | 56 | (6.2%) |
| Otitis externa | 10 | (1.1%) |
| Bronchitis | 51 | (5.6%) |
| Bronchiolitis | 12 | (1.3%) |
| Influenza | 17 | (1.9%) |
| Others | 48 | (5.3%) |
| Not written | 70 | (7.7%) |
| Total | 908 | (100%) |
The predominant categories of age were from 1 to 5 years (289/908, 31.8%) and 6–10 years (258/908, 28.4%) (Table 1).
Chief complaints were recorded in 869/908 (95.7%) cases. Most common single chief complaint was fever in 120/869 (13.8%), cough in 75/869 (8.6%), rhinorrhea in 24/869 (2.7%), and sore throat in 13/869 (1.4%) cases. More than one respiratory symptom was recorded in 569/869 (65.4%), and other complaints formed 68/869 (7.8%) of all cases. (Table 1) Unfortunately, only 550/908 (60.5%) of the paediatric patients were physically examined. Physical examination findings demonstrated: congested throat in 121/550 (22%), ear problems were found in 51/550 (9.3%), pharyngeal tonsillar erythema in 99/550 (18%) tonsillar exudate in 35/550 (6.4%), more than one respiratory finding in 188/550 (34.2%), other findings were found in 55/550 (10%) cases (Table 1).
Diagnosis was recorded in 838/908 (92.3%) of cases, with the most common diagnosis being common cold at 227/838 (27.6%), followed by 123/838 cases of pharyngitis (15%), 104/838 Tonsillitis (12.6%) and pneumonia in only 21/838 cases (2.4%). Other diagnoses were noted in 346/838 (42.1%) of cases (Table 1).
Pneumonia with tachypnea, without costal retractions or general danger signs, were noted in 15/21 cases (71.4%), pneumonia with costal retractions in 5/21 cases (23.8%) and only 1/21 child suffered from severe pneumonia (4%) (Table 1).
684/908 (75.3%) of patients had their weights recorded during their visit. Of the three main vital signs, heart rate was recorded in 602/908 (66.3%), temperature in 764/908 (84.1%) and respiratory rate in 582/908 (64.1%) (Table 2).
Table 2.
Distribution of the recording of various variables required to support a diagnosis.
| Features recorded | Yes | No |
|---|---|---|
| Weight | 684 (75.3%) | 224 (24.7%) |
| Temperature | 764 (84.1%) | 144 (15.9%) |
| Heart rate | 602 (66.3%) | 306 (33.7%) |
| Respiratory rate | 582 (64.1%) | 326 (35.9%) |
| Chief complaints | 869 (95.7%) | 39 (4.3%) |
| Physical examination | 550 (60.6%) | 358 (39.4%) |
| Provisional diagnosis | 838 (92.3%) | 70 (7.7%) |
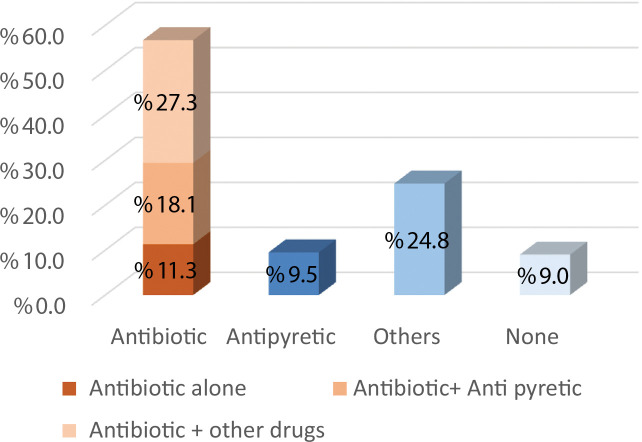
Overall, antibiotics were prescribed in 515/908 cases (56.7%), distributed as either a single therapy in 103/515 (20%), a combination of antibiotic and antipyretics in 164/515 (31.8%), or as antibiotics with other drugs in 248/515 (48.1%) (Fig. 1).
Figure 1.
Distribution of choice of children’s treatment.
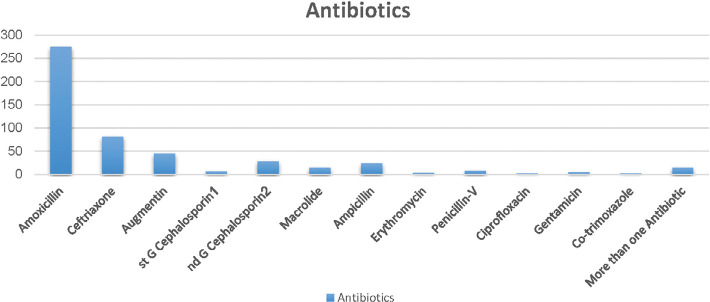
First choice of antibiotic prescribed was Amoxicillin in 275/515 (53.3%) of cases, second choice was Ceftriaxone in 81/515 (15.7%), followed by Augmentin in 45/515 (8.7%), various other antibiotics in 90/515 (17.5%), and lastly more than one antibiotic was prescribed in 14/515 cases (2.7%) (Fig. 2).
Figure 2.
Distribution of the types of antibiotics used.
4. DISCUSSION
In the PHC of Makkah, the incidence of ARI in children under 5 years old was 358 (39.4%). Several studies had a similar incidence of approximately 30–40% in children below 5 years - Al-Khalidi, Ramani, and Peasah [8,34,35]. In contrast, Siddiqui found an ARI incidence of 83.2% [7].
In the majority of studies, including ours, ARI cases consisted of upper respiratory tract infections (URTI). Lower respiratory tract infections (LRTI), such as pneumonia, bronchitis and bronchiolitis, were 10% in our study as well as in Al-Khalidi, and Saeed [8,34]. Sarfraz [25] reported a higher respiratory tract infections rate of 68%.
This study, as well as most other studies, found patients, predominantly, of male gender: Siddiqui, Al-Khalidi, Krishnan, and Dharmage [7,8,34,36,37], in contrast to Acharya [4] where both genders were equivalent. Chandwani [38] reported a male-dominated society as a possible reason.
569 (65.4%) patients presented with more than one respiratory symptom. The single most common complaint was fever, seen in 120 cases (13.8%), with a similar rate reported by Siddiqui [7] and Chandwani [21]. A much higher rate of 98.8% was found in Ramani [34]. Al-Khaldi [8] reported 70% of cases complained of cough.
Vital signs were recorded in this study and in Siddiqui [7] as follows: Temperature 144 (15.9%), 106(52%); Heart rate 306 (33.7%), 177(88%); Respiratory rate 326 (35.9%), 135(67%); and Weight 224 (24.7%), 132(65%), respectively. Al-Khaldi [8] and Ramani [34] did not mention these variables.
Congested throat was the most frequent finding in this study and Al-Khaldi [8]. Interestingly, the rank order of the most common diagnoses was similar between this study and that of Al-Khaldi [8]: Common cold was first (27.6%, 42%), followed by pharyngitis (15%, 25%), and tonsillitis (12.6%, 17%), respectively. This may be due to physician habits within the same nation.
Diagnosis was written in the great majority of PHC cases, in 92.3%, similar to Al-Khaldi [8] at 97.5%. In contrast, in Siddiqui [7] the diagnosis was written in less than half of the cases (44.6%).
The drug of choice was Amoxicillin in 275 (53.3%) of cases, followed by Ceftriaxone in 81 (15.7%), and Augmentin in 45 (8.7%) cases. One of the reason of prescribing, antibiotic other than amoxicillin, as observed by us, was non-availability of amoxicillin, in some of the centers. Siddiqui [7] reported the most common antibiotic prescribed as Amoxicillin in 21.4%, followed by a first generation cephalosporin (19.9%) and co-trimoxazole (14.3%). A recent study in Morocco by Jroundi [39] found the most commonly prescribed antibiotic was a cephalosporin (213/286; 74.5%), followed by macrolides (21%), then Gentamicin (13.6%). Al-Khaldi [8] did not report antibiotic classes. According to revised WHO guidelines, Amoxicillin should be given as first line of treatment and Ceftriaxone as second line of treatment [33].
Our study limitation is the duration of sample collection; it was conducted at the end of the local winter season because of late approval from ethical committee.
5. CONCLUSION
Many physicians in Makkah Al Mukarramah are not following the WHO guidelines for Acute Respiratory Infection. Educational health programs should be conducted to sensitize the physicians as well as patients regarding the appropriate method of diagnosis and rational use of antibiotics [40].
ACKNOWLEDGEMENTS
The authors are grateful to Bashar Omar Babkour, Haneen Salah Al-Masoudi, Noura Awad Almalki and Marya Abdurrahman Alqithami for their role in data collection.
APPENDIX A.
SAMPLE SIZE FOR FREQUENCY IN A POPULATION
Population size (for finite population correction factor or fpc) (N): 1600000
Hypothesized % frequency of outcome factor in the population (p): 50% ±5
Confidence limits as % of 100(absolute ±%)(d): 5%
Design Effect (for cluster surveys-DEFF): 2
Sample Size(n) for Various Confidence Levels.
| Confidence level (%) | Sample size |
|---|---|
| 95% | 769 |
| 80% | 329 |
| 90% | 542 |
| 97% | 942 |
| 99% | 1327 |
| 99.9% | 2165 |
| 99.99% | 3026 |
Results from OpenEpi, Version 3, open source calculator—SSPropor
Print from the browser with ctrl-P
or select text to copy and paste to other programs.
ETHICAL CONSENT
The consent of practitioners were sought before obtaining the prescriptions.
CONFLICTS OF INTEREST
The authors declare no potential conflicts of interest with respect to research, authorship and/or publication of this manuscript.
REFERENCES
- [1].Francis NA, Butler CC, Hood K, Simpson S, Wood F, Nuttall J. Effect of using an interactive booklet about childhood respiratory tract infections in primary care consultations on reconsulting and antibiotic prescribing: a cluster randomised controlled trial. BMJ. 2009;339:b2885. doi: 10.1136/bmj.b2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].UNICEF The State of World Children. 2013 [ http://www.unicef.org/sowc2013/].
- [3].Reddaiah V, Kapoor SK. Acute respiratory infections in rural underfives. Indian J Pediatr. 1988;55:424–6. doi: 10.1007/bf02810367. [DOI] [PubMed] [Google Scholar]
- [4].Acharya D, Prasanna K, Nair S, Rao R. Acute respiratory infections in children: a community based longitudinal study in South India. Indian J Public Health. 2002;47:7–13. [PubMed] [Google Scholar]
- [5].Mitra NK. A longitudinal study on ARI among rural under fives. Indian J Community Med. 2001;26:8–11. [Google Scholar]
- [6].Wang H, Zheng Y, Deng J, Wang W, Liu P, Yang F, et al. Prevalence of respiratory viruses among children hospitalized from respiratory infections in Shenzhen, China. Virol J. 2016;13:1. doi: 10.1186/s12985-016-0493-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Siddiqui MI, Baloch AA, Ahmed SI, Jafri SIA. Audit of prescribing patterns of doctors for the management of acute respiratory infections in children. Elective Med J. 2014;2:6–9. doi: 10.18035/emj.v2i1.61. [DOI] [Google Scholar]
- [8].Al-Khaldi YM, Diab MM, Al-Gelban KS, Al-Asmari AS, Al-Amin S, Al-Shahrani MS. Prescribing patterns for acute respiratory infections in primary health care, aseer region, Saudi Arabia. J Family Community Med. 2005;12:121–6. doi: 10.4103/2347-2618.171957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Saeed AA, Bani IA. Prevalence and correlates of acute respiratory infections in children less than two years of age. Saudi Med J. 2000;21:1152–6. https://www.ncbi.nlm.nih.gov/pubmed/11360089. [PubMed] [Google Scholar]
- [10].van Gageldonk-Lafeber AB, Heijnen M-LA, Bartelds AI, Peters MF, van der Plas SM, Wilbrink B. A case-control study of acute respiratory tract infection in general practice patients in The Netherlands. Clin Inf Dis. 2005;41:490–7. doi: 10.1086/431982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Dyar OJ, Beović B, Vlahović-Palčevski V, Verheij T, Pulcini C. How can we improve antibiotic prescribing in primary care? Expert Rev Anti-infective Therapy. 2016;14:403–13. doi: 10.1586/14787210.2016.1151353. [DOI] [PubMed] [Google Scholar]
- [12].Urrusuno RF, Dorado MF, Arenas AV, Martino CS, Baena SC, Balosa MCM. Improving the appropriateness of antimicrobial use in primary care after implementation of a local antimicrobial guide in both levels of care. Eur J Clin Pharmacol. 2014;70:1011–20. doi: 10.1007/s00228-014-1704-z. [DOI] [PubMed] [Google Scholar]
- [13].Nash DR, Harman J, Wald ER, Kelleher KJ. Antibiotic prescribing by primary care physicians for children with upper respiratory tract infections. Arch Pediatr Adolesc Med. 2002;156:1114–9. doi: 10.1001/archpedi.156.11.1114. [DOI] [PubMed] [Google Scholar]
- [14].Goossens H, Ferech M, Vander Stichele R, Elseviers M, Group EP Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. The Lancet. 2005;365:579–87. doi: 10.1016/s0140-6736(05)70799-6. [DOI] [PubMed] [Google Scholar]
- [15].Petersen I, Hayward AC. Antibacterial prescribing in primary care. J Antimicrobial Chemother. 2007;60:i43–i7. doi: 10.1093/jac/dkm156. [DOI] [PubMed] [Google Scholar]
- [16].Serna M, Ribes E, Real J, Galván L, Gascó E, Godoy P. High exposure to antibiotics in the population and differences by sex and age. Aten Primaria. 2011;43:236–44. doi: 10.1016/j.aprim.2010.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lallana-Alvarez MJ, Feja-Solana C, Armesto-Gomez J, Bjerrum L, Rabanaque-Hernandez MJ. Outpatient antibiotic prescription in Aragón and the differences by gender and age. Enferm Infecc Microbiol Clin. 2012;30:591–6. doi: 10.1016/j.eimc.2012.03.004. [DOI] [PubMed] [Google Scholar]
- [18].Holloway KA, Ivanovska V, Wagner AK, Vialle-Valentin C, Ross-Degnan D. Prescribing for acute childhood infections in developing and transitional countries, 1990–2009. Paediatr Int Child Health. 2015;35:5–13. doi: 10.1179/2046905514y.0000000115. [DOI] [PubMed] [Google Scholar]
- [19].Arroll B. Antibiotics for upper respiratory tract infections: an overview of Cochrane reviews. Respir Med. 2005;99:255–61. doi: 10.1016/j.rmed.2004.11.004. [DOI] [PubMed] [Google Scholar]
- [20].Smith SM, Fahey T, Smucny J, Becker LA. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2004;4 doi: 10.1002/14651858.cd000245.pub2. [DOI] [Google Scholar]
- [21].Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive pulmonary disease: when are antibiotics indicated? A systematic review. Respir Res. 2007;8:30. doi: 10.1186/1465-9921-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ong DS, Kuyvenhoven MM, Van Dijk L, Verheij TJ. Antibiotics for respiratory, ear and urinary tract disorders and consistency among GPs. J Antimicrob Chemother. 2008;62:587–92. doi: 10.1093/jac/dkn230. [DOI] [PubMed] [Google Scholar]
- [23].Llor C, Cots J, Gaspar M, Alay M, Rams N. Antibiotic prescribing over the last 16 years: fewer antibiotics but the spectrum is broadening. Eur J Clin Microbiol Infect Dis. 2009;28:893–7. doi: 10.1007/s10096-009-0719-3. [DOI] [PubMed] [Google Scholar]
- [24].Adriaenssens N, Coenen S, Versporten A, Muller A, Minalu G, Faes C, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient antibiotic use in Europe (1997–2009) J Antimicrob Chemother. 2011;66 Suppl 6:vi3–vi12. doi: 10.1093/jac/dkr453. [DOI] [PubMed] [Google Scholar]
- [25].Sarfraz T. Acute respiratory infections in children. Pak Armed Forces Med J. 1996;46:28–32. [Google Scholar]
- [26].Ojeniran M, Shouval R, Miskin IN, Moses AE, Shmueli A. Costs of appropriate and inappropriate use of antibiotics in the emergency department. IMAJ-Israel Med Assoc J. 2010;12:742. [PubMed] [Google Scholar]
- [27].Murphy M, Bradley CP, Byrne S. Antibiotic prescribing in primary care, adherence to guidelines and unnecessary prescribing-an Irish perspective. BMC Family Pract. 2012;13:43. doi: 10.1186/1471-2296-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Martínez MA, Inglada L, Ochoa C, Villagrasa JR. Treatments SSGoA. Assessment of antibiotic prescription in acute urinary tract infections in adults. J Infect. 2007;54:235–44. doi: 10.1016/j.jinf.2006.05.015. [DOI] [PubMed] [Google Scholar]
- [29].Tobia CC, Aspinall SL, Good CB, Fine MJ, Hanlon JT. Appropriateness of antibiotic prescribing in veterans with community-acquired pneumonia, sinusitis, or acute exacerbations of chronic bronchitis: a cross-sectional study. Clin Ther. 2008;30:1135–44. doi: 10.1016/j.clinthera.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Lee C-C, Lee C-H, Chuang M-C, Hong M-Y, Hsu H-C, Ko W-C. Impact of inappropriate empirical antibiotic therapy on outcome of bacteremic adults visiting the ED. Am J Emerg Med. 2012;30:1447–56. doi: 10.1016/j.ajem.2011.11.010. [DOI] [PubMed] [Google Scholar]
- [31].Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096. doi: 10.1136/bmj.c2096. [DOI] [PubMed] [Google Scholar]
- [32].Butler CC, Hillier S, Roberts Z, Dunstan F, Howard A, Palmer S. Antibiotic-resistant infections in primary care are symptomatic for longer and increase workload: outcomes for patients with E. coli UTIs. Br J Gen Pract. 2006;56:686–92. https://www.ncbi.nlm.nih.gov/pubmed/16954001. [PMC free article] [PubMed] [Google Scholar]
- [33].Revised WHO classification and treatment of pneumonia in children at health facilities: evidence summaries. 2014. [PubMed]
- [34].Ramani VK, Pattankar J, Puttahonnappa SK. Acute Respiratory Infections among Under-Five Age Group Children at Urban Slums of Gulbarga City: A Longitudinal Study. J Clin Diagn Res. 2016;10:LC08. doi: 10.7860/jcdr/2016/15509.7779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Peasah SK, Purakayastha DR, Koul PA, Dawood FS, Saha S, Amarchand R, et al. The cost of acute respiratory infections in Northern India: a multi-site study. BMC Public Health. 2015;15:1. doi: 10.1186/s12889-015-1685-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Krishnan A, Amarchand R, Gupta V, Lafond KE, Suliankatchi RA, Saha S, et al. Epidemiology of acute respiratory infections in children-preliminary results of a cohort in a rural north Indian community. BMC Infect Dis. 2015;15:1. doi: 10.1186/s12879-015-1188-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Dharmage SC, Rajapaksa LC, Fernando DN. Risk factors of acute lower respiratory tract infections in children under five years of age. Southeast Asian J Trop Med Public Health. 1996;27:107–10. https://www.ncbi.nlm.nih.gov/pubmed/9031411. [PubMed] [Google Scholar]
- [38].Chandwani H, Pandor J. Healthcare-Seeking Behaviors of Mothers regarding their Children in a Tribal Community of Gujarat, India. Electron Physician. 2015;7:990. doi: 10.14661/2015.990-997. https://www.ncbi.nlm.nih.gov/pubmed/26052410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Jroundi I, Benmessaoud R, Mahraoui C, Moraleda C, Tligui H, Seffar M, et al. Antibiotic usage prior and during hospitalization for clinical severe pneumonia in children under five years of age in Rabat. Morocco Antibiotics. 2013;2:450–64. doi: 10.3390/antibiotics2040450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Md Rezal RS, Hassali MA, Alrasheedy AA, Saleem F, Md Yusof FA, Godman B. Physicians’ knowledge, perceptions and behaviour towards antibiotic prescribing: a systematic review of the literature. Exp Rev Anti-infective Ther. 2015;13:665–80. doi: 10.1586/14787210.2015.1025057. [DOI] [PubMed] [Google Scholar]