Abstract
This study tested the theory that anxious fathers pose a quantitatively different environmental influence on childhood anxiety than anxious mothers. The analysed sample contained 502 linked adoption units from the Early Growth and Development Study (EGDS), a longitudinal multisite study that follows 561 adopted children (57.2% boys) and their adoptive and birth parents, who were recruited through US adoption agencies. A Bayesian latent growth model predicted child anxiety symptoms between 18 months and 4.5 years from inherited (birth parent anxiety) and rearing parent anxiety. This model revealed little evidence for a difference in the influence of maternal and paternal rearing parent anxiety on child anxiety symptoms. Contrary to theoretical predictions, anxiety in the rearing father is likely to have an equivalent influence to that of the mother on both child anxiety symptoms at 18 months old and their developmental trajectory over the preschool years.
Keywords: Parenting, Children, Anxiety symptoms, Adoption design
Introduction
Anxiety is the most common childhood psychological disorder (Cartwright-Hatton, McNicol, & Doubleday, 2006) affecting around 3% of children at any time (Ford, Goodman, & Meltzer, 2003) with a lifetime prevalence of 15–20% in community samples (Beesdo, Knappe, & Pine, 2009). Anxiety is associated with serious impairments in children’s academic and social functioning (Pine, 1997) and is a major risk factor for subsequent psychological problems (Kim-Cohen et al., 2003; Kovacs, Gatsonis, Paulauskas, & Richards, 1989; Kushner, Sher, & Beitman, 1990). Government initiatives in the UK and US emphasize early intervention (e.g., Department for Education, 2010; U.S. Public Health Service, 2000), the success of which will depend upon a solid understanding of both theoretical models of and risk factors for the development of anxiety symptoms in children.
Developmental models of anxiety symptoms suggest that much of the “development” is likely to occur in the preschool years. In a community sample of 541 preschool children, 19.6% met the criteria for at least one anxiety disorder (Dougherty et al., 2013). In a review of developmental models of anxiety, Field and Lester (2010a) concluded anxious symptomatology shows developmental change over the preteenage years, and that at least some aspects of this symptomatology are present in the preschool years. Furthermore, both the preschool level of anxiety-related symptoms and how they change over time were believed to be affected by both inherited influences and environmental ones such as parental rearing practices.
Despite these conclusions, most research on the trajectory and prevention of anxiety symptoms has focused on school aged children (for reviews, see Fisak, Richard, & Mann, 2011; Muris & Field, 2011). Measuring anxiety symptoms through self-report relies on self-reflection about thoughts, interpretations of events, and internal states. This reflection requires levels of cognitive and emotional development beyond the preschool years. Consequently, preschool measures of anxiety focus on parental report or observational tasks related to anxiety that do not capture the full range of anxiety symptoms. One example is behavioural inhibition, which measures infant’s reactions to strange situations, but not anxiety per se (e.g., Feng et al., 2008; Liu & Pérez-Edgar, 2019). As such, measuring preschool anxiety symptoms requires home visits or family visits to a laboratory, which is more time-consuming, expensive, and complex than collecting child self-report measures during school visits. These barriers have contributed to relatively little research on the trajectory of anxiety symptoms in the preschool years.
One consequence of the lack of knowledge about preschool anxiety symptoms is that prevention and intervention programs have had to rely on either applying downwards what works in older children (e.g., Barrett, Fisak, & Cooper, 2015) or targeting anxious parents’ cognitions and behaviours on the assumption that they are a risk factor for anxiety symptoms developing in their children (Cartwright-Hatton et al., 2018; Ginsburg, Drake, Tein, Teetsel, & Riddle, 2015). These parent-focussed programmes assume that children of anxious parents have not only an inherited risk for anxiety, but also an environmental risk from anxious rearing behaviours. Support for this assumption comes from twin studies, which consistently demonstrate shared environmental influences on child anxiety symptoms in preschool children (Eley et al., 2003, 2000) and 8–17 year olds (Ogliari et al., 2010; Spatola, Rende, & Battaglia, 2010; Zavos, Rijsdijk, & Eley, 2012). These studies also showed that the non-shared environment shapes anxiety symptoms. However, these studies cannot separate genetic from environmental transmission of anxiety because they are conducted with biological parents raising their own offspring. A “children-of-twins” design enables this separation although it does not eliminate passive gene-environment correlations. One such study of 385 monozygotic and 486 dizygotic same-sex twin parents and their offspring (aged 11–22) showed that environmental mechanisms accounted for parent-child similarity but the data were equally consistent with children’s anxiety affecting parental symptoms as the reverse (Eley et al., 2015). One interpretation is that parent anxiety is conducive to creating a rearing environment that fosters anxiety in the offspring, although the specifics of that environment were not explored.
Theoretical models of the intergenerational transmission of anxiety suggest numerous pathways through which anxious cognitions and behaviours could be transmitted (e.g., Creswell, Murray, Stacey, & Cooper, 2011; Murray, Creswell, & Cooper, 2009). For example, anxious parents may model anxious behaviours and be more likely to promote anxious cognitions in their children through their unintentional use of verbal threat information. Additionally, parents who exert too much control over their children and restrict autonomy could send a message that the world is dangerous and prevent the child from learning resilience through facing challenge. The authors of this model acknowledge that research has predominantly been conducted on mothers. There is an implicit assumption that, until such time that more concrete evidence exists for differing roles of paternal and maternal rearing behaviour, the model applies to both mothers and fathers. This position is supported by a meta-analysis showing that the weighted mean effects of maternal, r = 0.16, and paternal, r = 0.13, anxiety on child internalizing behaviours were almost identical (Connell & Goodman, 2002).
Other models, however, argue that paternal-maternal differences exist. For example, Flouri (2010) cited evidence for differences in the specificity of maternal and paternal rearing behaviours. In particular, maternal warmth positively impacted emotion regulation in adolescents whereas paternal control negatively impacted it (see Flouri, 2010 for a review). Flouri (2010) concluded that despite some progress in understanding the paternal role in child psychopathology, there is an urgent need for research testing theory-driven hypotheses around maternal and paternal influences on psychopathology. One of the few theory-driven hypotheses comes from Bügels and Perotti (2011) who argued that because of their typically different roles in child upbringing, mothers and fathers create rearing environments that differentially influence child anxiety symptoms. They argued that humans are relatively unusual in that high paternal investment in offspring is common and that the explanation for this lies in the complex social structures that humans have evolved (see also Möller, Majdandzic, de Vente, & Bügels, 2013). Survival depends upon the social competitiveness of the individual and that it is the father who primarily develops these skills, through physical play, risk taking, overcoming obstacles, and engaging in social competition. Bögels and Perotti (2011) argued that mothers are more likely than fathers to foster skills in emotional bonding, empathy, and caring for others. Furthermore, they suggested that fathers may take more risks with their children than mothers (and in doing so foster skills in overcoming challenging situations) because, compared to mothers, they can reproduce more easily and are less certain of their biological relation to the child. Bögels and Perotti (2011) suggested that because fathers are typically more involved in the modelling of taking risk and facing challenge, anxiety in fathers will inhibit them from encouraging their children to take risks, face challenges, or engage in social competition. Their children will, in turn, have underdeveloped skills to deal with threatening or novel situations, which creates anxiety within them. In short, the influence of rearing parent anxiety on child anxiety symptoms should be greater for fathers than mothers (especially during the preschool years when the family is the major environmental influence).
There are counter-arguments to Bögels and Perotti’s (2011) theory. First, married American mothers typically spend more time than corresponding fathers with their children: 49.8 h per week compared to 31.4 h for fathers (Raley, Bianchi, & Wang, 2012). Therefore, fathers have less opportunity to shape anxiety symptoms. Also, some of the arguments used to support the paternal role being more important than the maternal role in promoting anxiety symptoms could be used to argue the opposite. Take, for example, the argument that mothers foster emotional skills more than fathers. If mothers foster emotional skills then they plausibly have a greater role in helping children to regulate their emotional reactions in challenging situations, and would be more likely than fathers to model emotional responses, such as anxiety, to novel situations. A large comparison of maternal and paternal influences on preschool anxiety symptoms that considers inherited and parental anxiety influences is necessary to dissociate these opposing ideas. Unfortunately, no such study exists; nearly all of the research into parental influences on child anxiety symptoms has been conducted on mothers.
Studies that have compared maternal and paternal influences on child anxiety symptoms in older children are, at best, inconclusive with respect to Bögels and Perotti’s (2011) theory (for reviews, see Bögels & Phares, 2008; Möller et al., 2013). Against the theory are findings that fail to show differences between maternal and paternal influences; for example, autonomy granting from both mothers and fathers predicted some form of anxiety in 6–18 year old children (Lindhout et al., 2006). Social referencing experiments have also shown that reactions to potentially threatening situations in mothers and fathers did not significantly differentially affect children’s (aged 8–13) anxious responses to those situations (Möller, Majdandzic, Vriends, & Bögels, 2014). In addition, although mothers displayed significantly more intense encouraging facial reactions to their infant (aged 10–15 months) crossing a visual cliff than fathers, the infant’s behaviour was not differentially affected by whether the mother or father was present during the task (Möller, Majdandzic, & Bögels, 2014). Although Bögels and Perotti’s (2011) theory is specific to anxiety, work on other internalizing disorders is also inconsistent with respect to differential influence from mothers and fathers. For example, adoption studies on adolescent depression have shown that maternal but not paternal depression is a significant predictor of adolescent depression (Tully, Iacono, & McGue, 2008), both maternal and paternal depression significantly predict adolescent depression (Marmorstein, Iacono, & McGue, 2012), and paternal but not maternal substance use and nicotine dependence significantly predicts adolescent depression (Marmorstein et al., 2012).
In support of the theory, there is evidence that paternal, but not maternal, over-involvement significantly predicted infant (10–15 months) anxiety (Möller, Majdandzic, & Bögels, 2015). Also, a 6-month longitudinal study of children aged 2 and 4 showed that lower levels of paternal, but not maternal, autonomy granting were significantly associated with greater child anxiety symptoms (Majdandzic, Möller, de Vente, Bögels, & van den Boom, 2014). In the same study, fathers’ challenging parental behaviour predicted less subsequent social anxiety in their oldest child, whereas maternal challenging behaviour was associated with more subsequent social anxiety. Also, three longitudinal studies of preschool (age ranges 2–5) children showed that child anxiety symptoms were significantly predicted by specific maternal and paternal rearing behaviours (Edwards, Rapee, & Kennedy, 2010; Majdandzic et al., 2014; McShane & Hastings, 2009). However, these studies used only relatively short follow ups (6–12 months), and none of them could dissociate the parental anxiety influence from the inherited influence from parents.
In summary, existing theories suggest that the preschool years might be an important developmental period for anxiety symptoms, and that mothers and fathers might have differential roles in how those symptoms develop. A prediction from one theory is that paternal rearing influences on child anxiety symptoms are stronger than maternal influences, and this effect should be strongest during the preschool years. The scant research to test this prediction used relatively short followups and could not dissociate rearing parental anxiety from the inherited influence on child anxiety symptoms. The current study addresses these shortcomings by using data from the Early Growth and Development Study (EGDS) which uses a parent-offspring adoption design (Leve et al., 2013). The EGDS tracks the developmental trajectory of child anxiety symptoms in the preschool years (18–54 months approximately). Whereas children of twin designs directly estimate passive gene-environment correlations, the adoption design eliminates it because the adoptive parents provide the rearing environment but are genetically unrelated to the child. Therefore, estimates of the parental anxiety rearing influence are not confounded by heritable characteristics of anxiety transmitted from rearing parent to child. Furthermore, the EGDS contains data from both mothers and fathers (adoptive and biological), which makes it particularly well suited to test Bögels and Perotti’s (2011) theory. Based on this theory, after adjusting for inherited risk, there should be a quantitatively different effect of rearing maternal and paternal anxiety on child anxiety symptoms overall, and the trajectory of symptoms over time. However, the theory in question is based on evolutionary arguments that are difficult to substantiate and assumptions based on traditional parenting roles. In the absence of these underpinning theoretical assumptions it is equally plausible that mothers and fathers have comparable contributions to their children’s anxiety symptoms. This study, therefore, aims to estimate the maternal and paternal contributions to child anxiety symptoms using a genetically-sensitive design.
Method
Sample characteristics
The data come from the EGDS, a longitudinal, multisite study that follows 561 adopted children (57.2% boys) and their adoptive and birth parents, who were recruited through US adoption agencies. The EGDS is described in detail in Leve et al. (2013). The EGDS sample has the following characteristics: (1) infants were placed domestically with an unrelated adoptive family; (2) placement occurred within 3 months of birth; (3) infants had no known major medical conditions (e.g., extreme prematurity or extensive medical surgeries); and (4) adoptive and birth parents could read or understand English to at least eighth-grade standard. This section describes the EGDS sample before exclusions, and for ease of readability we refer to the first parent who participated as “adoptive mother” and the second as “adoptive father”, which captures over 90% of the parent genders accurately.
The ethnic composition within the EGDS sample is as follows (see Leve et al., 2013): 70.1% of birth mothers were Caucasian (13.3% African American, 2.5% American Indian/Alaska Native, 1.8% Asian American, 0.2% Native Hawaiian/Pacific, 6.7% Hispanic or Latino, 4.9% more than one race, and 0.5% unknown or not reported); 69.9% of birth fathers were Caucasian (11.5% African American, 0.5% American Indian/Alaska Native, 9.6% Hispanic or Latino, 4.8% more than one race, and 3.3% unknown or not reported); 91.8% of the first adoptive parent (96.6% female) were Caucasian (3.9% African American, 0.2% American Indian/Alaska Native, 0.9% Asian American, 2% Hispanic or Latino, 0.9% more than one race, and 0.4% unknown or not reported); 90.4% of the second adoptive parent (96.6% male) were Caucasian (4.9% African American, 0.5% Asian American, 0.5% Native Hawaiian/Pacific Islander, 1.6% Hispanic or Latino, 1.1% more than one race, and 0.9% unknown or not reported).
With respect to educational background, 68.7% of birth mothers and 77.7% of birth fathers had completed a high school degree or lower. In contrast, 78.4% of the primary adoptive parents and 73.3% of the secondary adoptive parents had achieved a 4-year college or university degree or graduate program qualification. When comparing eligible families who enrolled in the study to those who declined, no significant differences were reported in education level, income, or age (see Leve et al., 2013, for details). All infant placements occurred between 0 and 91 days from birth (M = 6.2 days, SD = 12.45, Mdn = 2 days).
The focus of the current study was to compare maternal and paternal influences on the child’s anxiety symptoms across wave 1 (approximately 5 months after birth for birth parents and 9 months for adoptive parents), 2 (18 months), 3 (27 months) and 4 (54 months). The comparison of mothers and fathers meant that children with same sex adoptive parents and single-parent adoptive families in the sample described above were excluded. The total remaining sample contained 502 linked adoption units, 89% of the sample.
Measures
Inherited influences on child anxiety symptoms (birth parent anxiety)
Inherited influences on child anxiety symptoms were quantified using the Beck Anxiety Inventory, BAI (Beck & Steer, 1993a), a widely used measure of adult anxiety, measured at around 5 and 18 months after birth. This scale is a list of 21 symptoms of anxiety such as “dizzy or lightheaded”. Participants indicate how much they have experienced each symptom in the past month on a scale ranging from 0 (not at all) to 3 (severely – it bothered me a lot). Responses are summed to create a total ranging from 0 to 63. BAI scores can be thought of as describing minimal (0–7), mild (8–15), moderate (16–25), and severe (26–63) anxiety. Table 1 shows that scores ranged into the severe anxiety category for both birth mothers and fathers and, on average, were higher than the population average of 6.6 (SD = 8.1) reported by Gillis, Haaga, and Ford (1995). The levels of anxiety in birth parents are perhaps not surprising given that they are more likely to have long standing problems with psychopathology because of difficult life circumstances, and childbirth and placing a child for adoption are likely to be stressful and anxiety evoking. Internal consistency in the current sample was α = 0.91 at 5–9 months and 0.92 at 18 months for birth mothers. The corresponding values for birth fathers were α = 0.88 and 0.89.
Table 1.
Summary statistics for the Beck Anxiety Inventory in birth parents and adoptive parents.
| Measure | Wave A (4–9 months) |
Wave B (18 months) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Range | Mdn | M | 95% CI | n | Range | Mdn | M | 95% CI | |
| Birth mother | 496 | 0–52 | 8.00 | 9.93 | [9.13, 10.73] | 444 | 0–41 | 6.50 | 8.96 | [8.13, 9.79] |
| Birth father | 169 | 0–38 | 6.00 | 8.19 | [6.94, 9.44] | 147 | 0–38 | 4.00 | 6.84 | [5.56, 8.13] |
| Adoptive mother | 495 | 0–21 | 3.00 | 3.81 | [3.49, 4.12] | 458 | 0–28 | 2.00 | 3.39 | [3.06, 3.72] |
| Adoptive father | 477 | 0–19 | 2.00 | 3.00 | [2.72, 3.28] | 446 | 0–23 | 1.00 | 2.32 | [2.02, 2.62] |
Given that using more indicator variables should yield more stable scores and because of the high comorbidity between anxiety and depression (Costello, Egger, Copeland, Erkanli, & Angold, 2011), a composite for inherited influence could have been based on many available measures. In keeping with related studies using the EGDS data the average BAI scores across the two time points were computed for birth mothers and birth fathers. As a sensitivity analysis, robust correlation coefficients based on a one-step M-estimate (Shevlyakov & Smirnov, 2011) were computed between the average BAI scores for each parent and composite scores that also included their scores on the Beck Depression Inventory, BDI (Beck & Steer, 1993b) at the same time points, and the number of anxiety and depressive disorders scored at 18 months after birth using the Composite International Diagnostic Interview (Andrews & Peters, 1998; Kessler & Üstün, 2004). In birth mothers, the average BAI score correlated almost perfectly with composites consisting of BAI and anxiety diagnosis, r = 0.99, BAI and BDI, r = 0.94, and BAI, BDI and diagnosis of both anxiety and depression, r = 0.93. The corresponding values for birth fathers were rs = 1.00, 0.95 and 0.93. These findings suggest that the choice of how to derive inherited influence had virtually no impact: all potential composites shared almost all of their variance.
Average BAI scores were available for 497 birth mothers and 172 birth fathers. Where an average BAI score was available for only one birth parent, that score was used as the indicator of inherited influence. Where average scores were present for both birth parents, and in keeping with Brooker et al. (2014), the largest score was used as the child’s indicator of inherited influence. There were 330 birth mothers and 5 birth fathers whose average BAI score was used because the corresponding score for the other birth parent was missing, and 108 birth mothers and 59 birth fathers whose average BAI score was used because it was greater than that of the other birth parent.
Rearing parent anxiety influences on child anxiety symptoms (adoptive parent anxiety)
To be comparable with the measure of inherited influence, the influence of rearing parent anxiety on child anxiety was quantified in the same way except using adoptive parents’ responses. Because the primary aim of the study was to dissociate the effect of maternal and paternal rearing parent anxiety, two scores were computed for each child. Maternal rearing parent anxiety was quantified as the average BAI score in the adoptive mother at 9- and 18-months, paternal rearing parent anxiety was quantified as the same average for adoptive fathers. Anxiety symptoms were relatively low in adoptive parents. Table 1 shows that scores ranged into the moderate to severe anxiety categories in both adoptive mothers and fathers but were, on average, lower than US norms (Gillis et al., 1995). Internal consistency in the current sample was α = 0.75 at 4–9 months and 0.78 at 18 months for adoptive mothers. The corresponding values for adoptive fathers were α = 0.73 and 0.80. Maternal and paternal rearing parent anxiety scores shared close to zero variance, r = 0.17.
Child anxiety symptoms
The outcome variable was anxiety symptoms in the child as measured by the pre-school version of the Child Behavior Checklist, which is a well-standardized, parent-report inventory of behavioural and emotional problem with excellent internal consistency, test-retest reliability, and validity (Achenbach & Rescorla, 2000). Items reflect behavioural and emotional descriptions of the child such as “nervous, highstrung, or tense”, to which parents respond on a three-point scale (0 = not true, 1 = sometimes true, 2 = very true or often true). The 10 items reflecting DSM-Anxiety were totalled separately for adoptive mothers and adoptive fathers to create two scores (out of 20) representing child anxiety symptoms (one based on maternal report and the other on paternal report). The DSM-anxiety scale has a test-retest reliability of 0.85 over 8 days, and 0.60 over 12 months. Anxiety symptoms were measured at approximately 18, 27, and 54 months after birth. Internal consistencies at those time points were α = 0.45, 0.46, and 0.72 for adoptive mother report and 0.55, 0.55, and 0.75 for adoptive father report.
Table 2 shows that DSM anxiety scores ranged from 0 to 15 with means ranging from 1.68 to 2.81 (SDs from 1.59 to 2.55). These values are comparable with the US norms published in Achenbach (2013). The current sample, therefore, represents a good range of anxiety with a distribution of scores that overlaps with clinically diagnosed anxious children (although not representing the extremes of a clinical sample).
Table 2.
Summary statistics for adoptive mother and father ratings of child anxiety symptoms (Child Behavior Checklist DSM-Anxiety).
| Measure | n | Range | Mdn | M | 95% CI |
|---|---|---|---|---|---|
| Adoptive mother | |||||
| 18 months | 457 | 0–9 | 1.00 | 1.74 | [1.59, 1.89] |
| 27 months | 442 | 0–11 | 2.00 | 2.05 | [1.88, 2.22] |
| 54 months | 371 | 0–15 | 2.00 | 2.81 | [2.55, 3.07] |
| Adoptive father | |||||
| 18 months | 442 | 0–14 | 1.00 | 1.68 | [1.52, 1.84] |
| 27 months | 424 | 0–10 | 2.00 | 1.96 | [1.79, 2.14] |
| 54 months | 342 | 0–12 | 2.00 | 2.67 | [2.42, 2.93] |
Data analysis plan
This manuscript was prepared and analysis conducted using R 3.6.1. (R Core Team, 2019) and the following packages: BayesFactor (Morey & Rouder, 2018), blavaan (Merkle & Rosseel, 2018), lavaan (Rosseel, 2012), MissMech (Jamshidian, Jalal, & Jansen, 2014), papaja (Aust & Barth, 2018), robcor (Smirnov, 2014), semTools (Jorgensen, Pornprasertmanit, Schoemann, & Rosseel, 2018) and tidyverse (Wickham, 2017).
The key hypothesis was tested using a latent growth model in which child anxiety symptoms (CBCL DSM Anxiety) at 18, 27, and 54 months were endogenous observed variables predicted from latent variables representing the intercept and slope for growth (of anxiety symptoms) over time. The loadings for the paths from the slope latent variable to the three anxiety outcomes were constrained to be 0, 9 and 36 so that the intercept represents anxiety at 18 months old. The indices of inherited influence and rearing parent anxiety were included as exogenous observed variables that predicted the intercept and slope of growth in anxiety symptoms.
The Bayesian correlations and 95% Highest Posterior Density (HPD) intervals between adoptive mothers’ and adoptive fathers’ ratings of child anxiety symptoms were r =0.42 [0.34, 0.49], BF01 = 4.38 × 1017, at 18 months, r = 0.51 [0.43, 0.58], BF01 = 4.22 × 1026, at 27 months, and r = 0.52 [0.44, 0.59], BF01 = 7.85 × 1021, at 54 months. Given this overwhelming evidence for a strong relationship between adoptive mother and father ratings of child anxiety, the average of the adoptive parents’ scores on the CBCL DSM Anxiety scale was used as the main outcome variable, which is consistent with similar work using the EGDS sample (e.g., Brooker et al., 2014, 2015).
The model was fitted simultaneously using maternal and paternal variables constraining two model parameters directly related to the main hypothesis that paternal rearing parent anxiety exerts greater influence on child anxiety symptoms than maternal rearing parent anxiety. The first of these parameters, bRPAi, quantified the effect of rearing parent anxiety on the intercept of the growth curve (i.e., child anxiety symptoms at 18 months). The second parameter, bRPAs, quantified the effect of rearing parent anxiety on the rate of change in child anxiety symptoms (the slope).
For the avoidance of doubt, in both models inherited influence for a given child was the largest of their birth mother’s or birth father’s average BAI scores when both birth parents had an average BAI score. Otherwise, it was the average BAI score from whichever parent provided data. However, in the maternal model rearing parent anxiety for each child was the average BAI score from their adoptive mothers, whereas in the paternal model it was the average BAI score from their adoptive father.
Missing values
For the maternal model, 340 of the 502 cases were complete, and in the paternal model, 335 (of 502). In both models, 17 cases were excluded because of missing data at all waves for the outcome measure. The procedure described by Jamshidian and Jalal (2010) was used to test whether data were missing completely at random. This procedure involves a nonparametric test of homogeneity of covariances between groups based on the pattern of missingness. If covariances are comparable (i.e. the test is not significant) across groups with different patterns of missingness then MCAR can be assumed. This test was applied to the maternal and paternal data separately (because the outcome data are the same in the two models) and, because these tests are not independent, a corrected alpha of α = 0.025 used to evaluate them. The homogeneity tests were non-significant (at α = 0.025) for both the maternal data, 0.09, and the paternal data 0.44 giving no reason to reject the assumption that data are missing completely at random. In addition, generalized linear models predicting missing (or not) values on the outcome measure demonstrated that missingness was not significantly predicted by the predictors in the growth model: adoptive mother anxiety χ2(1) = 0.55, p = .459, adoptive father anxiety, χ2(1) = 0.06, p = .808, and inherited influence χ2(1) = 0.05, p = .817. Missing data were handled by a process similar to multiple imputation in the Bayesian model (see the section on estimation).
Measurement invariance
Factorial invariance of the CBCL was assessed using the method described by Wu and Estabrook (2016). A model was fit in which imposed a common factor structure at each time point (configural invariance): a single latent variable (child anxiety symptoms) at each time point was indicated by the corresponding CBCL DSM scale items at that time point. Factor loadings were then constrained to be the same over time (weak invariance), followed by a model in which the intercepts of all manifest indicators are constrained to be equal (strong invariance). These models were fit simultaneously to CBCL responses from adoptive mothers and adoptive fathers also constraining parameters across respondent. In large samples, factorial invariance should be assessed by examining the change in fit indices rather than significance tests of model fit (Widaman, Ferrer, & Conger, 2010; Widaman & Thompson, 2003).
Using the CFI, model fit was below the accepted threshold of 0.90 (Bentler, 1990) for the configural, CFI = 0.82, weak, CFI = 0.76, and strong, CFI = 0.65 invariance models. However, the RMSEAs indicated good fit for the configural invariance, RMSEA = 0.05, and weak invariance, RMSEA = 0.06, models and adequate fit for the strong invariance model, RMSEA = 0.07 (MacCallum, Browne, & Sugawara, 1996). The SRMRs were in the good range (0.08 or below) for all models, SRMRs = 0.06, 0.08 and 0.09 for the configural, weak and strong invariance models respectively.
Estimation
The growth model was estimated using a Bayesian framework. Bayesian and Frequentist frameworks both yield parameter estimates that quantify the effect of inherited influences and rearing parent anxiety influences on the intercept and slope of child anxiety symptoms. They also yield estimates that quantify the difference between these parameters in the maternal and paternal model. Within a Frequentist framework, however, a parameter is assumed to be a fixed but unknown value that is estimated from the data. Typically, the parameter estimate is the one most consistent with the data (the Maximum Likelihood estimate). Within a Bayesian framework, parameters are represented probabilistically. In other words, probabilities are assigned to all possible values of a parameter. In this framework, the estimate is derived not only from the data, but from a probability distribution representing prior beliefs about the parameter values (known as the prior distribution). The sample data are used to update this prior distribution to create a new probability distribution (the posterior) of parameter values. The parameter estimate is the most probable value. If the prior distribution is completely uninformative then the Bayesian and Frequentist estimates converge.
Unlike a Bayesian model, a frequentist one will yield p-values for the parameter estimates that tell us the probability of obtaining values at least as large as the ones observed assuming that the null is true (that is assuming no effect or no difference between the maternal and paternal estimates). It will also yield confidence intervals that in 95% of samples tell us the limits between which the population value of these estimates lie and in 5% of samples do not. We have no way of knowing which category our samples falls into, meaning that these intervals provide no evidence of the true population values based on the data. These p-values and confidence intervals do not address the central aim of this study, which is to quantify the plausible influence of rearing maternal and paternal anxiety on child anxiety symptoms. First off, confidence intervals cannot tell us about the plausible values of parameters in the population because we have no way of knowing whether the confidence intervals from our data capture the population values, or not. This weakness of confidence intervals is widely known (Morey, Hoekstra, Rouder, Lee, & Wagenmakers, 2016), and they are not the correct tool for the job of providing probabilistic evidence for the plausible size of an effect in the population based on a single set of data, which is what we seek to establish. Second, p-values are not helpful because they rely on the assumption that the null is true. In our case, they provide a probability based on the assumption that the quantitative difference in the maternal and paternal influence of rearing parent anxiety is zero. Notwithstanding well-rehearsed arguments that this assumption of a zero effect is never true (e.g., Cohen, 1990; Field, 2017), this assumption is particularly problematic in the current models because a difference of zero is a theoretically interesting possibility. As such, we want information from the model that makes no a priori assumptions about the effect in question and, therefore, allows us to establish its plausible size from the data. Frequentist p-values and confidence intervals cannot provide evidence as to how plausible it is that an effect is zero because they assume that it is a priori. A secondary concern is that a reliance on p-values may be misleading because they are linked to sample size. In a large sample (such as we have) a significant p-value might reflect a trivial effect because the test has a lot of power. Even in a frequentist model we would be wise to place any p-value within the context of the associated parameter estimate.
A Bayesian framework avoids all of these concerns. A Bayesian model will not yield p-values, so there will be no temptation to overinterpret significant but trivial effects. It also will not yield confidence intervals, but instead produces HPD intervals which, unlike confidence intervals, can be interpreted as direct probabilistic evidence for the likely population value of a model parameter. These intervals will tell us with a certain probability (95%), the population value of a parameter. Unlike p-values and confidence intervals HPD intervals provide evidence as to the whether the difference between parameters in the maternal and paternal models can plausibly be zero and the uncertainty around that estimate. In other words, they allow us to achieve the primary goal of this study: to quantify the difference between parameters in the maternal and paternal models and establish whether 0 is a plausible value. Therefore, Bayesian estimation was used with informative priors set on the two parameters of interest (see below). Using Bayesian estimates of the model parameters and their 95% HPD intervals enabled us to determine the plausible size of the difference in the effect of maternal and paternal rearing parent anxiety on child anxiety symptoms. To sum up, a Bayesian model frees us from the shackles of the “all or nothing” thinking that p-values engender. More important, the HPD intervals enable us to make probabilistic statements about the plausible parameter values in the population.
Estimation was based on the full sample including missing values. In a Bayesian growth model, parameters are estimated using an iterative process (Markov chain Monte Carlo, MCMC) and missing values are likewise estimated as unknown parameters (Gelman et al., 2013). The process has two stages: an “imputation” step draws missing values at iteration t + 1 from the probability distribution for the missing part of the data given the observed part and the posterior at iteration t, next, the “posterior” step draws posterior values at iteration t + 1 from the probability distribution for posterior values given the observed data and the just-estimated values for the missing part at the same iteration (Merkle, 2011). This data augmentation approach has parallels to multiple imputation with the “imputation model” being the growth model and imputations are being drawn at every iteration of the MCMC procedure; however, it benefits from using the same model for sampling missing values as is used to analyse the data (Merkle, 2011).
It is worth noting that, for two reasons, the parameter estimates themselves will differ very little from those from a frequentist model using multiple imputation. First, we used weakly informative priors meaning that the posterior distributions will have been driven by the data more than the priors. Second, although many frequentist estimation methods (e.g., Maximum likelihood) rely on large sample assumptions such as asymptotic normality whereas MCMC does not (Palomo, Dunson, & Bollen, 2007), in large samples the asymptotic normality assumption will be met and the methods should converge.
The model was estimated using the blavaan package in R (Merkle & Rosseel, 2018), which is a Bayesian extension of the widely-used lavaan package (Rosseel, 2012). Models are specified in exactly the same way as lavaan but blavaan allows users to specify priors and estimates the model using MCMC. For a detailed description of the package, with examples, see Merkle and Rosseel (2018).
Prior distributions
Informative prior distributions (priors) were used in the reported model but a sensitivity analysis using the default uninformative priors from blavaan revealed that the chosen priors did not change the substantive conclusions from the models. The priors were derived in the following way. Spatola et al. (2010) estimate the proportion of variance in CBCL anxiety accounted for by additive inherited influences (A) as 0.57 with 95% CI limits of 0 and 0.74 from their ordinal ML model. For shared environmental influence (C), the mean was 0 with Cl limits of 0 and 0.18. These equate to small to large effects, which would equate to a shift on CBCL DSM in the region of 0.2–0.8 standard deviations. Population data suggest the CBCL DSM anxiety scale has an SD = 1.9 (Kristensen, Henriksen, & Bilenberg, 2010). Therefore, a standard deviation shift in the BAI (the measure that quantifies both inherited influence and rearing parent anxiety influence) equates to a change in the CBCL DSM anxiety scale in the region of 0.2 × 1.9 = 0.38 and 0.8 × 1.9 = 1.52. The BAI has M = 6.6 (SD = 8.1) in a community sample (n = 242), according to Gillis et al. (1995). Therefore, the values above are the change expected from an 8.1 unit shift in the predictor. Therefore, the raw unit change in CBCL DSM anxiety expected from a unit change in the BAI should be somewhere between 0.38/8.1 = 0.05 and 1.52/8.1 = 0.19.
Fig. 1 shows a normal prior distribution with M = 0.10, SD = 0.07. This places the bulk of the prior belief as being that a unit change in the BAI equates to an increase on the CBCL DSM anxiety scale of 0 to 0.2 points. Larger changes are entertained as is the possibility that increases in the BAI equate to decreases in the CBCL DSM anxiety score, but with low probability. To set priors in blavaan the precision is used rather than the standard deviation, which is 1/0.072 = 204.08. Therefore, the prior distribution for the substantive model parameters was set with the function dnorm(0.1, 200), which corresponds to a normal distribution with a mean of 0.1 and standard deviation of 0.07 (2 d.p.).
Fig. 1.
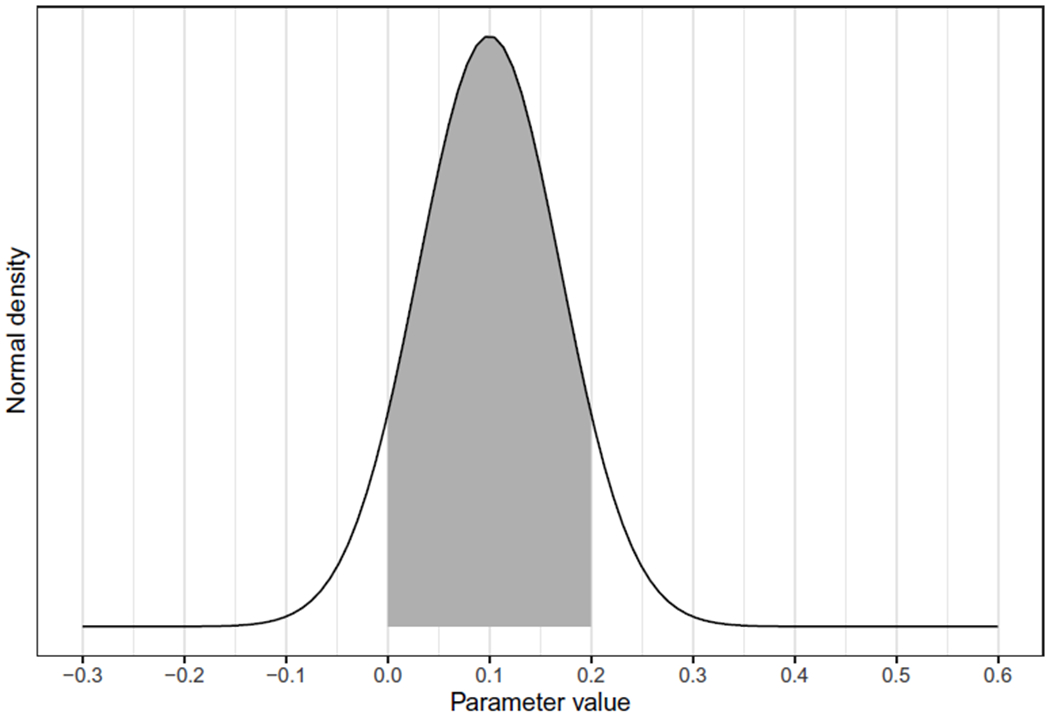
Prior distribution for the key model parameters.
Results
Relationships between variables
The composite variables representing inherited and rearing parent anxiety influences were trivially related when based on maternal data, r = −0.03 [−0.12, 0.07], BF01 = 0.13, and paternal data, r = 0.08 [−0.09, 0.24], BF01 = 0.30. In both cases the Bayes factors and posterior ps strongly favour the null (i.e., no relationship) and the HPD intervals suggest that assuming a relationship exists it is likely to be small. The fact that these relationships were, at best, small suggests that evocative gene-environment mechanisms can be largely ruled out of the main model.
Rearing parent anxiety scores for adoptive mothers and fathers were not strongly correlated, r = 0.10 [0.01, 0.19], BF01 = 1.48. The Bayes factor suggests equal evidence for the null and alternative, and estimates of the correlation suggest that if it is non-zero, it is small. For inherited influence, the correlation between birth mothers’ and fathers’ scores was also modest, r = 0.22 [0.05, 0.38], BF01 = 6.02. The Bayes factor slightly favoured the alternative hypothesis but the evidence is weak.
Bayesian latent growth model
Table 3 shows the raw correlations between variables in the growth models. Table 4 shows the unconditional growth model. The outcome data are the same in the maternal and paternal models, therefore the unconditional model is identical for mothers and fathers (i.e., it is only the predictors of the intercept and slope of child anxiety symptoms that differ). The parameter estimates show that the variances of the intercepts and slopes were greater than zero, although small for the slope (relative to its mean). More important, the 95% HPDs show that there is a 95% probability that the population variances for the intercept and slope were not zero; put another way, there is variance to be explained albeit a small amount for the slope.
Table 3.
Correlation matrix for variables in the latent growth model of child anxiety symptoms.
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| Birth parent anxiety (BAI) | 10.31 | 8.38 | |||||
| Adoptive mother anxiety (BAI) | 3.61 | 3.23 | 0.01 | ||||
| Adoptive father anxiety (BAI) | 2.67 | 2.86 | 0.00 | 0.10* | |||
| Child anxiety wave B (CBCL) | 1.72 | 1.40 | 0.00 | 0.10* | 0.15** | ||
| Child anxiety wave C (CBCL) | 1.98 | 1.58 | 0.02 | 0.13** | 0.15** | 0.58** | |
| Child anxiety wave D (CBCL) | 2.77 | 2.20 | −0.06 | 0.13** | 0.11* | 0.34** | 0.37** |
Note. RPA = Rearing parent anxiety.
p < .001,
p < .05.
Table 4.
Key model parameters for the unconditional latent growth model of child anxiety symptoms (parameters excluded are the variances for the observed child anxiety symptoms at 18, 27, and 54 months).
| Effect | b | 95% HPD | Posterior SD | Prior distribution |
|---|---|---|---|---|
| αintercept | 1.707 | [1.587, 1.831] | 0.063 | norm(1.6, 0.277) |
| ψintercept | 1.434 | [1.149, 1.743] | 0.152 | wish(iden, 3) |
| αslope | 0.029 | [0.021, 0.037] | 0.004 | norm(1.6, 0.277) |
| ψslope | 0.006 | [0.005, 0.007] | 0.000 | wish(iden, 3) |
| Cov(i, s) | −0.019 | [ − 0.030, −0.008] | 0.006 | wish(iden, 3) |
Note. αintercept and ψintercept are the mean and variance of the intercept respectively. The corresponding terms for the slope are αslope and ψslope. Cov(i, s) is the covariance between the intercept and slope. HPD = Highest Posterior Density interval. Prior distributions are represented by the functions used to create them. For example norm(x, y) represents a normal distribution with M = x, and a precision of y. The precision is used rather than the standard deviation to be consistent with the convention in JAGS (the engine behind the Bayesian estimation process). To convert the value to the standard deviation use .
Table 5 shows the key parameter estimates and their 95% HPD intervals for the maternal and paternal models. First, consider the extent to which the slope of child anxiety symptoms is influenced by rearing parent anxiety. Table 4 shows strong evidence that the rate of change of anxiety symptoms is trivially affected by both maternal and paternal rearing parent anxiety when adjusting for inherited influences: the parameter estimates (RPAs in the table) are very close to zero and have HPD intervals that suggest population parameter values indicative of a trivial influence. For example, in both models the parameter value is 0.001. To put this value into perspective, a unit shift in the BAI equates to a shift of 0.001 on the CBCL DSM anxiety scale adjusting for the other variables in the model. Considering the BAI ranges from 0 to 63, a unit shift on the scale is very small, but consider that a 10-point shift would equate to an increase of 0.01 on the 20-point CBCL DSM anxiety scale. The effect is negligible.
Table 5.
Key model parameters for latent growth models of child anxiety symptoms (parameters excluded are the variances for the intercept, slope, and observed child anxiety symptoms at 18, 27, and 54 months
| Effect | b | 95% HPD | Posterior SD | Prior distribution |
|---|---|---|---|---|
| Maternal model (n = 500) | ||||
| αintercept | 1.503 | [1.262, 1.751] | 0.125 | norm(1.6, 0.277) |
| ψintercept | 1.599 | [1.279, 1.931] | 0.167 | gamma(1, 0.5) |
| αslope | 0.027 | [0.011, 0.043] | 0.008 | norm(1.6, 0.277) |
| ψslope | 0.006 | [0.005, 0.007] | 0.000 | gamma(1, 0.5) |
| Cov(i, s) | −0.038 | [ − 0.053, −0.022] | 0.008 | beta(1, 1) |
| Inheritedinfluencei | 0.003 | [ − 0.012, 0.018] | 0.008 | norm(0.1, 200) |
| Inheritedinfluences | 0.000 | [ − 0.001, 0.001] | 0.001 | norm(0.1, 200) |
| RPAi | 0.049 | [0.011, 0.087] | 0.019 | norm(0.1, 200) |
| RPAS | 0.001 | [ − 0.001, 0.004] | 0.001 | norm(0.1, 200) |
| Paternal model (n = 489) | ||||
| αintercept | 1.482 | [1.254, 1.727] | 0.120 | norm(1.6, 0.277) |
| ψintercept | 1.614 | [1.303, 1.952] | 0.167 | gamma(1, 0.5) |
| αslope | 0.030 | [0.015, 0.045] | 0.008 | norm(1.6, 0.277) |
| ψslope | 0.006 | [0.005, 0.007] | 0.000 | gamma(1, 0.5) |
| Cov(i, s) | −0.038 | [ − 0.053, −0.023] | 0.008 | beta(1, 1) |
| Inheritedinfluencei | 0.002 | [ − 0.013, 0.018] | 0.008 | norm(0.1, 200) |
| Inheritedinfluenees | 0.000 | [ − 0.001, 0.001] | 0.001 | norm(0.1, 200) |
| RPAi | 0.076 | [0.030, 0.117] | 0.022 | norm(0.1, 200) |
| RPAs | 0.000 | [ − 0.002, 0.003] | 0.001 | norm(0.1, 200) |
| Maternal-paternal difference | ||||
| RPAi difference | −0.027 | [ − 0.084, 0.031] | 0.029 | |
| RPAs difference | 0.001 | [ − 0.003, 0.005] | 0.002 | |
Note. αintercept and ψintercept are the mean and variance of the intercept respectively. The corresponding terms for the slope are αslope and ψslope. Cov(i, s) is the covariance between the intercept and slope. Baseline (intercept) child anxiety symptoms are predicted from inherited influence (Inherited influencei) and rearing parent anxiety (RPAi). The rate of change of child anxiety symptoms is predicted from inherited influence (Inherited influences) and rearing parent anxiety (RPAs). HPD = Highest Posterior Density interval. Prior distributions are represented by the functions used to create them. For example norm(x, y) represents a normal distribution with M = x, and a precision of y. The precision is used rather than the standard deviation to be consistent with the convention in JAGS (the engine behind the Bayesian estimation process). To convert the value to the standard deviation use .
The influence of rearing parent anxiety on overall anxiety at 18 months (RPAi in the table) was somewhat larger than its influence on the rate of change of anxiety. For example, in the maternal model a unit shift in the BAI equated to a shift of 0.049 on the CBCL DSM anxiety scale adjusting for the other variables in the model. A 10-point shift in BAI would, therefore, equate to a change of half a unit on the 20-point scale of the CBCL DSM anxiety scale. Similar to its effect on the rate of change of child anxiety symptoms, this effect is very small.
The main aim of the study was to evaluate the degree to which the influence of maternal or paternal rearing parent anxiety on child anxiety symptoms differs. The parameters labelled RPAi difference, and RPAs difference quantify these differences for the effect on baseline child anxiety symptoms and the rate of change of those symptoms respectively. In both cases the estimate itself and the corresponding 95% HPD intervals show that the difference between maternal and paternal influence is very close to zero and the plausible population values are exceedingly close to zero. For example, the difference in the paternal and maternal rearing parent anxiety influence on child anxiety symptoms at 18-months old (baseline) is −0.027 and there is a 95% probability that the population value falls between −0.084 and 0.031. In short, the difference is highly probably very close to zero. Using the extremes of the HPD interval, the maximum plausible difference in the parameter in favour of a stronger effect in fathers would be −0.084, in other words child anxiety symptoms would be 0.084 units higher for rearing paternal anxiety than for rearing maternal anxiety. At the other extreme, child anxiety symptoms could be 0.031 units higher for rearing maternal anxiety than rearing paternal anxiety. At either extreme, these differences are negligible within the context of the 20-point CBCL DSM anxiety scale.
Although the study focus was primarily on rearing parent anxiety, Table 5 also shows that inherited influence had almost no effect on child anxiety symptoms at 18 months, 0.003 95% HPD [−0.012, 0.018], or the rate of change over the preschool years, 0.000 95% HPD [−0.001, 0.001]. (Estimates are quoted from the maternal model, but are approximately the same in the paternal model because the inherited influence indicator was the same in both models.)
Discussion
This is the first genetically sensitive study to compare rearing paternal and maternal anxiety influences on the developmental trajectory of child anxiety symptoms during the preschool years. The key finding was that paternal and maternal anxiety influences on child anxiety symptoms at 18 months old, and their rate of change over the preschool years, is equivalent. A secondary finding was that the rearing parent anxiety influence on child anxiety symptoms was very small When predicting anxiety symptoms at 18 months, the effect of rearing parent anxiety was 0.049 in the maternal model and 0.076 in the paternal model. These values equate to a 10-point increase in rearing parent BAI corresponding to between a half and a three-quarter unit increase on the 20-point CBCL DSM anxiety scale. When predicting the rate of change over time, rearing parent anxiety had virtually no effect. There is a 95% probability that the true effect of rearing parent anxiety on anxiety symptoms at 18 months after birth falls between 0.011 and 0.087.
Implications of no difference between maternal and paternal rearing parent anxiety influences
The key theoretical question that this research aimed to address was to quantify the extent to which anxiety-driven maternal and paternal rearing influences on child anxiety symptoms differ. A secondary aim was to quantify the contribution of inherited and rearing parent anxiety influences on anxiety symptoms in the preschool years in a genetically sensitive design. On the first aim, the current study found little evidence for the Bögels and Perotti (2011) theory that anxiety in the rearing father has a stronger influence on child anxiety symptoms than anxiety in the rearing mother (after considering inherited influence). The plausible parameter estimates for maternal and paternal rearing parent anxiety were negligibly different. This finding leaves little scope for maternal and paternal influences being quantitatively different (especially when considering the range of plausible values encapsulated by the HPD intervals and how they would translate to unit changes on the CBCL DSM anxiety).
As discussed earlier, contrary to Bögels and Perotti’s (2011) model, there may be good reasons to assume that maternal anxiety rearing influences will be greater than paternal, but the current results lead to equally ambivalent beliefs in this idea: in the age range tested within this non-clinical sample there is very little evidence that the paternal influence of rearing parent anxiety on child anxiety symptoms differed from the maternal influence. Even if maternal and paternal effects fell at the opposite extremes of their plausible values, based on the HPD intervals, this would equate to a negligible difference on the CBCL DSM anxiety. It is also plausible that the difference is 0. One explanation is, of course, that theories proposing differences in parental anxiety influences on child anxiety are wrong.
A second explanation for the current results is that it is not general anxiety in the parent that matters but specific rearing practices conducive to fostering child anxiety symptoms. Put another way, our measure of parental anxiety influence may have been too blunt to capture differences between mothers and fathers. The idea that the specifics of childrearing matter has credibility. Flouri (2010) discusses the importance of specificity when looking at parenting models of child mental health. There are, for example, studies in which rearing characteristics other than parental anxiety in both fathers and mothers predict child anxiety symptoms, for example: overprotection (Edwards et al., 2010), parental control (van der Bruggen, Bögels, & van Zeilst, 2010) and negative control (Karreman, de Haas, van Tuijl, van Aken, & Dekovic, 2010). Also, studies that support Bögels and Perotti’s (2011) model have tended to look at specific aspects of rearing practices (e.g., overprotection) whereas the current study measured anxiety overall. However, across the reviewed literature there is little consistency in which aspects of maternal and paternal rearing behaviour differentially influence anxiety symptoms in the child. For example, parental over control as a predictor of child anxiety symptoms has been shown to be more important in mothers than fathers (Hudson, Comer, & Kendall, 2008), more important in fathers than mothers (van der Bruggen, Stams, Bügels, & Paulussen-Hoogeboom, 2010), and equally as important in mothers and fathers (Karreman et al., 2010). One obvious next step is to repeat the current study looking at specific, theoretically-driven aspects of parenting.
A third explanation is that quantitatively different parental anxiety influences take effect at later ages (a point considered in due course) and our sample missed the time window during which differential parental effects occur. This idea fits with developmental “moderation” models, which propose that qualia of anxiety symptomatology exist very early in life but are moderated as a function of later cognitive development, the socio-emotional landscape of the child and inherited influence (Field & Lester, 2010a). For example, selective attention to threat has been shown in infants as young as 5 months old (for a review, see LoBue & Rakison, 2013) and attentional control during toddlerhood has been shown to be a protective factor in genetically susceptible children who are raised in low-risk environments (Brooker et al., 2014). Some moderation theories, such as Kindt’s inhibition model (Kindt & van den Hout, 2001) suggest that the moderation (or inhibition) of selective attention to threat may occur as late as 10 years old. If true, it raises the possibility that a 3-year longitudinal study during preschool is too short to capture the critical points of change of the growth curve (and, therefore, the differences in maternal and paternal rearing parent anxiety influences upon it). This explanation would also account for the differences to Eley et al. (2015), whose sample of offspring were considerably older (11–22) than ours. What is clear from the current study is that maternal and paternal rearing parent anxiety influences on the rate of change of anxiety symptoms during the preschool years in a non-clinical sample is ostensibly the same. Future work would need to look for whether a difference manifests later in the child’s development or in samples with greater clinical severity.
Have the influence of rearing parent anxiety and inherited influences been overestimated?
The current study also showed that both inherited influences and rearing parent anxiety had very small effects on anxiety symptoms at 18 months and negligible effects on the rate of change in those symptoms over the preschool years. The fact that inherited influence had a trivial effect on the developmental trajectory of a child anxiety symptoms and a tiny effect on overall symptom levels at 18 months is consistent with recent children of twins work showing that an environment pathway, but not a genetic one, significantly predicted child anxiety symptoms (Eley et al., 2015). Eley et al. (2015) concluded that although the lack of evidence for a genetic pathway is surprising in light of the twin studies showing sizeable heritability estimates, it is consistent with studies of childhood depression (e.g., Silberg, Maes, & Eaves, 2010). Other work using the EGDS data in similar age groups has found that inherited influence does not significantly predict inhibition and social anxiety in 18–27 month olds (Natsuaki et al., 2013) and also bidirectional effects of negative affect in 9–27 month old children on adoptive parent anxiety that seemed to be environmental and not due to birth parent negative affect (Brooker et al., 2015). The current study further supports this position.
As Eley et al. (2015) suggest, evidence pointing to the limited inherited influence on familial transmission of anxiety supports developmental theories that assume that parents transmit anxiety through pathways such as modelling and verbal information (Creswell et al., 2011; Field & Lester, 2010b; Field & Purkis, 2011). However, the current study suggested that, as with inherited influence, rearing parent anxiety had virtually no influence on the developmental trajectory (i.e., the change over time) of anxiety symptoms, and a very weak effect on overall levels at 18 months. At face value, this conclusion contradicts Eley et al.’s data as well as the aforementioned theories that parents transmit anxiety environmentally and the empirical work to support it (for a review, see Creswell et al., 2011). However, the current study was based on a preschool sample whereas Eley et al.’s (2015) sample was aged 11–22. One obvious explanation is that anxiety transmission through pathways such as modelling and verbal information becomes important after the preschool years as the child develops the linguistic and cognitive skills to understand the implicational meaning of threat information. This explanation ties in with the aforementioned discussion of differences in paternal and maternal influences manifesting after the preschool years.
However, twin studies have shown close to zero effects of the shared genetic environment with the non-shared environment having a much greater contribution to anxiety (Spatola et al., 2010). Adoption studies, such as the current one, measure shared environment, so the measures of rearing parental anxiety in the current study would align to the shared environment estimates in a twin study. In this sense, the current results are not surprising: it may not be rearing parent anxiety that matters so much as the broader environment or specific parenting behaviours (i.e, the proximal family environment), neither of which were included in the current analysis.
One reason why the current models yielded very small estimates for the inherited influence and rearing parent anxiety in child anxiety symptoms has been discussed already, that the developmental trajectory may not change in the time period captured by the current study. Edwards et al. (2010) found that anxiety symptoms were stable over 12 months in a preschool sample. There are other explanations though. First, perhaps the developmental trajectory of the child is already relatively fixed by 18 months (the first time point at which child anxiety symptoms were measured in this study). This explanation fits with the earlier discussion of research showing that some symptoms of anxiety (e.g., attention to threat) are present very early in life (for a review, see LoBue & Rakison, 2013). It is also supported by the fact that although there was variability in the trajectory of children’s anxiety symptoms over time, this variability was small.
Applications
Nearly all of the research on how parenting affects child anxiety symptoms has been based on samples of mothers. Theoretical models of parenting and the intergenerational transmission of anxiety (e.g., Creswell et al., 2011; Murray et al., 2009) and the interventions based upon them (e.g., Cartwright-Hatton et al., 2018; Ginsburg et al., 2015) have been operating under the assumption that what we have learnt from research on mothers translates to fathers. The good news for these models and interventions is that the findings of the current study imply that this assumption is reasonable: the influence of rearing parent anxiety appears to be very similar for mothers and fathers. The bleaker implication is that rearing parent anxiety has only a tiny effect on child anxiety symptoms meaning that there is little to gain from targeting parents’ anxious behaviours in treatment or prevention programmes. However, given that the current analysis utilised a community, not clinical, sample we should be careful not to throw out the baby with the bathwater. There may be parenting behaviours not related to anxiety that promote anxious symptoms in their children, for example, a parent’s tendency to change their behaviour to help their child to reduce their anxiety, known as accommodation (Lebowitz et al., 2013). A recent clinical trial suggests that treatments targeting these behaviours may be efficacious (Lebowitz, Marin, Martino, Shimshoni, & Silverman, 2019).
Limitations
Other explanations of the tiny effects of inherited influence and rearing parent anxiety on child anxiety symptoms, and the negligible paternal and maternal differences, relate to some of the study limitations. First, the current sample was a community, not clinical, sample, so perhaps there was insufficient variability in anxiety over time to enable us to detect moderators of that change. Second, reliability statistics were quite low for the child anxiety symptoms measure at the first two waves. The issue of low reliability could mean that there was more measurement error in early waves than later waves, which mitigated the sensitivity of the models to detect moderators of the change in anxiety over time. Also, child anxiety symptoms scores did not meet the upper extremes of the scale even at older ages when one might expect some children to have developed extremes of anxiety. A related issue is whether the CBCL truly captures child anxiety symptoms. As noted earlier, there has been relatively little research on the trajectory of anxiety symptoms in the preschool years because it is difficult to measure. Although the pre-school CBCL is a widely used and established measure of child anxiety symptoms, it is, nevertheless, a parental report of the child’s behaviour and may be an insensitive gauge of the child’s internal state.
Third, because the current sample was a community sample, there may have been insufficient variability in birth parent anxiety which would mitigate the size of inherited influence on child anxiety symptoms. This explanation seems implausible because birth parents reported levels of anxiety and depression that ranged to clinical levels (see Table 1). Related to the previous point, because they have undergone intense screening, adoptive parents may have better mental health than the general population which would again mitigate the size of effect of rearing parent anxiety on child anxiety symptoms (McGue et al., 2007). This explanation has credibility because the BAI scores of adoptive parents had low variance and range compared to the general population (see Table 1) which may have attenuated the parameter estimates (i.e., effect size estimates and their credible intervals) for the effect of rearing parent anxiety. However, in general, adoption samples have been shown not to show range restriction in measures of mental health. Nevertheless, the results may not be generalizable beyond adoption samples.
Summary
The take-home message is that in the preschool years, when controlling for inherited influences, child anxiety symptoms are relatively unaffected by rearing parent anxiety and there is little evidence that the size of this effect differs from mothers and fathers. These findings could suggest that by 18 months, anxiety symptoms are already in place and unchangeable (except perhaps by non-family environment) after 4.5 years. This could mean that parental influence on anxiety takes place before 18 months or up to 4.5 years, or that it has simply been overestimated in past theories and research.
Acknowledgements
This project was supported by the following grants: (1) R01 HD042608 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and the National Institute on Drug Abuse, NIH, U.S. PHS (PI Years 1–5: David Reiss, MD; PI Years 6–10: Leslie Leve, PhD); (2) R01 MH092118 from the National Institute of Mental Health, NIH, U.S. PHS (PIs: Jenae Neiderhiser, Ph.D. and Leslie Leve, Ph.D.); (3) R01 DA020585 from the National Institute on Drug Abuse, the National Institute of Mental Health and OBSSR, NIH, U.S. PHS (PI: Jenae Neiderhiser, Ph.D.); (4) R56 HD042608 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development, NIH, U.S. PHS (PI: Leslie Leve, PhD); (5) ES/5004467/1 from UKRI-ESRC (PI: Gordon Harold, PhD) (6) UG3/UH3 OD023389 from the Office of the Director, NIH, U.S. (PI: Leslie Leve, PhD). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health & Human Development or the National Institutes of Health. Thanks to Edgar Merkle for responding quickly and helpfully to questions about the blavaan package. A pre-print of the manuscript and analysis scripts are posted at https://osf.io/zgcg2/
References
- Achenbach TM (2013). DSM guide for the ASEBA. Burlington, VT: University of Vermont, Research Center for Children, Youth & Families. [Google Scholar]
- Achenbach TM, & Rescorla LA (2000). Manual for ASEBA preschool forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Andrews G, & Peters L (1998). The psychometric properties of the composite international diagnostic interview. Social Psychiatry and Psychiatric Epidemiology, 33, 80–88. 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- Aust F, & Barth M (2018). papaja: Create APA manuscripts with R Markdown. Retrieved from https://github.com/crsh/papaja. [Google Scholar]
- Barrett P, Fisak B, & Cooper M (2015). The treatment of anxiety in young children: Results of an open trial of the fun FRIENDS program. Behaviour Change, 32, 231–242. 10.1017/bec. [DOI] [Google Scholar]
- Beck AT, & Steer RA (1993a). Beck anxiety inventory manual. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck AT, & Steer RA (1993b). Beck depression inventory manual. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beesdo K, Knappe S, & Pine DS (2009). Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America, 32, 483–524. 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. [DOI] [PubMed] [Google Scholar]
- Bögels SM, & Perotti EC (2011). Does father know best? A formal model of the paternal influence on childhood social anxiety. Journal of Child and Family Studies, 20, 171–181. 10.1007/s10826-010-9441-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bögels SM, & Phares V (2008). Fathers’ role in the etiology, prevention and treatment of child anxiety: A review and new model. Clinical Psychology Review, 28, 539–558. 10.1016/j.cpr.2007.07.011. [DOI] [PubMed] [Google Scholar]
- Brooker RJ, Neiderhiser JM, Ganiban JM, Leve LD, Shaw DS, & Reiss D (2014). Birth and adoptive parent anxiety symptoms moderate the link between infant attention control and internalizing problems in toddlerhood. Development and Psychopathology, 26, 347–359. 10.1017/s095457941300103x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooker RJ, Neiderhiser JM, Leve LD, Shaw DS, Scaramella LV, & Reiss D (2015). Associations between infant negative affect and parent anxiety symptoms are bidirectional: Evidence from mothers and fathers. Frontiers in Psychology, 6 10.3389/fpsyg.2015.01875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Bruggen CO, Bögels SM, & van Zeilst N (2010). What influences parental controlling behaviour? The role of parent and child trait anxiety. Cognition & Emotion, 24, 141–149. 10.1080/02699930802618843. [DOI] [Google Scholar]
- van der Bruggen CO, Stams GJJM, Bögels SM, & Paulussen-Hoogeboom MC (2010). Parenting behaviour as a mediator between young children’s negative emotionality and their anxiety/depression. Infant and Child Development, 19, 354–365. 10.1002/icd.665. [DOI] [Google Scholar]
- Cartwright-Hatton S, Ewing D, Dash S, Hughes Z, Thompson EJ, Hazell CM, … Startup H (2018). Preventing family transmission of anxiety: Feasibility RCT of a brief intervention for parents. British Journal of Clinical Psychology, 57, 351–366. 10.1111/bjc.12177. [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S, McNicol K, & Doubleday E (2006). Anxiety in a neglected population: Prevalence of anxiety disorders in pre-adolescent children. Clinical Psychology Review, 26, 817–833. 10.1016/j.cpr.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Cohen J (1990). Things I have learned (so far). American Psychologist, 45, 1304–1312. 10.1037/0003-066X.45.12.1304. [DOI] [Google Scholar]
- Connell AM, & Goodman SH (2002). The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin, 128, 746–773. 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Core Team, R. (2019). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from https://www.Rproject.org/. [Google Scholar]
- Costello EJ, Egger HL, Copeland W, Erkanli A, & Angold A (2011). The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity In Silverman WK, & Field AP (Eds.). Anxiety disorders in children and adolescents: Research, assessment and intervention (pp. 56–75). (2nd ed.). Cambridge:Cambridge University Press. [Google Scholar]
- Creswell C, Murray L, Stacey J, & Cooper P (2011). Parenting and child anxiety In Silverman WK, & Field AP (Eds.). Anxiety disorders in children and adolescents: Research, assessment and intervention (pp. 299–322). (2nd ed.). Cambridge: Cambridge University Press. [Google Scholar]
- Department for Education (2010). Promoting the emotional health of children and young people: Guidance for Children’s Trust partnerships, including how to deliver NI 50. Department for Children, Schools and Families. [Google Scholar]
- Dougherty LR, Tolep MR, Bufferd SJ, Olino TM, Dyson M, Traditi J, ... Klein DN (2013). Preschool anxiety disorders: Comprehensive assessment of clinical, demographic, temperamental, familial, and life stress correlates. Journal of Clinical Child & Adolescent Psychology, 42, 577–589. 10.1080/15374416.2012.759225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards SL, Rapee RM, & Kennedy S (2010). Prediction of anxiety symptoms in preschool-aged children: Examination of maternal and paternal perspectives. Journal of Child Psychology and Psychiatry, 51, 313–321. 10.1111/j.1469-7610.2009.02160.x. [DOI] [PubMed] [Google Scholar]
- Eley TC, Bolton D, O’Connor T, Perrin S, Smith P, & Plomin R (2000). The structure of anxiety in 4-year-olds: A genetic analysis. Behavior Genetics, 30, 397–423. 10.1023/A:1017371222025. [DOI] [Google Scholar]
- Eley TC, Bolton D, O’Connor TG, Perrin S, Smith P, & Plomin R (2003). A twin study of anxiety-related behaviours in pre-school children. Journal of Child Psychology and Psychiatry, 44, 945–960. 10.1111/1469-7610.00179. [DOI] [PubMed] [Google Scholar]
- Eley TC, McAdams TA, Rijsdijk FV, Lichtenstein P, Narusyte J, Reiss D, … Neiderhiser JM (2015). The intergenerational transmission of anxiety: A childrenof-twins study. American Journal of Psychiatry, 172, 630–637. 10.1176/appi.ajp.2015.14070818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Kovacs M, Lane T, O’Rourke FE, & Alarcon JH (2008). Emotion regulation in preschoolers: The roles of behavioral inhibition, maternal affective behavior, and maternal depression. Journal of Child Psychology and Psychiatry, 49, 132–141. 10.1111/j.1469-7610. [DOI] [PubMed] [Google Scholar]
- Field AP (2017). Discovering statistics using IBM SPSS statistics (5th ed.). London: Sage. [Google Scholar]
- Field AP, & Lester KJ (2010a). Is there room for “development” in developmental models of information processing biases to threat in children and adolescents? Clinical Child and Family Psychology Review, 13, 315–332. 10.1007/s10567-010-0078-8. [DOI] [PubMed] [Google Scholar]
- Field AP, & Lester KJ (2010b). Learning of information processing biases in anxious children and adolescents In Hadwin JA, & Field AP (Eds.). Information processing biases and anxiety: A developmental perspective (pp. 253–278). Chichester: Wiley-Blackwell. [Google Scholar]
- Field AP, & Purkis HM (2011). The role of learning in the aetiology of child and adolescent fear and anxiety In Silverman WK, & Field AP (Eds.). Anxiety disorders in children and adolescents: Research, assessment and intervention (pp. 227–256). (2nd ed.). Cambridge: Cambridge University Press. [Google Scholar]
- Fisak B, Richard D, & Mann A (2011). The prevention of child and adolescent anxiety: A meta-analytic review. Prevention Science, 12, 255–268. 10.1007/s11121-011-0210-0. [DOI] [PubMed] [Google Scholar]
- Flouri E (2010). Fathers’ behaviors and children’s psychopathology. Clinical Psychology Review, 30, 363–369. 10.1016/j.cpr.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Ford T, Goodman R, & Meltzer H (2003). The British child and adolescent mental health survey 1999: The prevalence of DSM-IV disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1203–1211. 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- Gelman A, Carlin JA, Stern HS, Dunson DB, Vehtari A, & Rubin DB (2013). Bayesian data analysis (3rd ed.). Boca Raton, FL: Chapman & Hall. [Google Scholar]
- Gillis MM, Haaga DAF, & Ford GT (1995). Normative values for the Beck Anxiety Inventory, Fear Questionnaire, Penn State Worry Questionnaire, and Social Phobia and Anxiety Inventory. Psychological Assessment, 7, 450–455. 10.1037/1040-3590.7.4.450. [DOI] [Google Scholar]
- Ginsburg GS, Drake KL, Tein J-Y, Teetsel R, & Riddle MA (2015). Preventing onset of anxiety disorders in offspring of anxious parents: A randomized controlled trial of a family-based intervention. American Journal of Psychiatry, 172, 1207–1214. 10.1176/appi.ajp.2015.14091178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JL, Comer JS, & Kendall PC (2008). Parental responses to positive and negative emotions in anxious and nonanxious children. Journal of Clinical Child and Adolescent Psychology, 37, 303–313. 10.1080/15374410801955839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamshidian M, & Jalal S (2010). Tests of homoscedasticity, normality, and missing completely at random for incomplete multivariate data. Psychometrika, 75, 649–674. 10.1007/s11336-010-9175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamshidian M, Jalal S, & Jansen C (2014). MissMech: An R package for testing homoscedasticity, multivariate normality, and missing completely at random (MCAR). Journal of Statistical Software, 56, 1–31. 10.18637/jss.v056.i06. [DOI] [Google Scholar]
- Jorgensen D, Pornprasertmanit S, Schoemann MA, & Rosseel Y (2018). semTools: Useful tools for structural equation modeling. Retrieved from https://CRAN.Rproject.org/package=semTools. [Google Scholar]
- Karreman A, de Haas S, van Tuijl C, van Aken MAG, & Dekovic M (2010). Relations among temperament, parenting and problem behavior in young children. Infant Behavior & Development, 33, 39–49. 10.1016/j.infbeh.2009.10.008. [DOI] [PubMed] [Google Scholar]
- Kessler RC, & Üstün TB (2004). The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). International Journal of Methods in Psychiatric Research, 13, 93–121. 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, & Poulton R (2003). Prior juvenile diagnoses in adults with mental disorder – Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry, 60, 709–717. 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Kindt M, & van den Hout M (2001). Selective attention and anxiety: A perspective on developmental issues and the causal status. Journal of Psychopathology and Behavioral Assessment, 23, 193–202. 10.1023/A:1010921405496. [DOI] [Google Scholar]
- Kovacs M, Gatsonis C, Paulauskas SL, & Richards C (1989). Depressive-disorders in childhood IV. A longitudinal-study of co-morbidity with and risk for anxiety disorders. Archives of General Psychiatry, 46, 776–782. 10.1001/archpsyc.1989.01810090018003. [DOI] [PubMed] [Google Scholar]
- Kristensen S, Henriksen TB, & Bilenberg N (2010). The Child Behavior Checklist for ages 1.5-5 (CBCL/11/2-5): Assessment and analysis of parent- and caregiver-reported problems in a population-based sample of Danish preschool children. Nordic Journal of Psychiatry, 64, 203–209. 10.3109/08039480903456595. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, & Beitman BD (1990). The relation between alcohol-problems and the anxiety disorders. American Journal of Psychiatry, 147, 685–695. 10.1176/ajp.147.6.685. [DOI] [PubMed] [Google Scholar]
- Lebowitz ER, Marin C, Martino A, Shimshoni Y, & Silverman WK (2019). Parentbased treatment as efficacious as cognitive-behavioral therapy for childhood anxiety: A randomized noninferiority study of supportive parenting for anxious childhood emotions. Journal of the American Academy of Child & Adolescent Psychiatry. 10.1016/j.jaac.2019.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz ER, Woolston J, Bar-Haim Y, Calvocoressi L, Dauser C, Warnick E, … Leckman JF (2013). Family accommodation in pediatric anxiety disorders. Depression and Anxiety, 30, 47–54. 10.1002/da.21998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Neiderhiser JM, Shaw DS, Ganiban J, Natsuaki MN, & Reiss D (2013). The Early Growth and Development Study: A prospective adoption study from birth through middle childhood. Twin Research and Human Genetics, 16, 412–423. 10.1017/thg.2012.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindhout I, Markus M, Hoogendijk T, Borst S, Maingay R, Spinhoven P, … Boer F (2006). Childrearing style of anxiety-disordered parents. Child Psychiatry & Human Development, 37, 89–102. 10.1007/s10578-006-0022-9. [DOI] [PubMed] [Google Scholar]
- Liu P, & Pérez-Edgar KE (2019). Developmental pathways from early behavioral inhibition to later anxiety: An integrative review of developmental psychopathology research and translational implications. Adolescent Research Review, 4, 45–58. 10.1007/s40894-018-0092-5. [DOI] [Google Scholar]
- LoBue V, & Rakison DH (2013). What we fear most: A developmental advantage for threat-relevant stimuli. Developmental Review, 33, 285–303. 10.1016/j.dr.2013.07.005. [DOI] [Google Scholar]
- MacCallum RC, Browne MW, & Sugawara HM (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1, 130–149. 10.1037/1082-989X.1.2.130. [DOI] [Google Scholar]
- Majdandzic M, Möller EL, de Vente W, Bögels SM, & van den Boom DC (2014). Fathers’ challenging parenting behavior prevents social anxiety development in their 4-year-old children: A longitudinal observational study. Journal of Abnormal Child Psychology, 42, 301–310. 10.1007/s10802-013-9774-4. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG, & McGue M (2012). Associations between substance use disorders and major depression in parents and late adolescent-emerging adult offspring: An adoption study. Addiction, 107, 1965–1973. 10.1111/j.1360-0443.2012.03934.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGue M, Keyes M, Sharma A, Elkins I, Legrand L, Johnson W, & Iacono WG (2007). The environments of adopted and non-adopted youth: Evidence on range restriction from the Sibling Interaction and Behavior Study (SIBS). Behavior Genetics, 37, 449–462. 10.1007/s10519-007-9142-7. [DOI] [PubMed] [Google Scholar]
- McShane KE, & Hastings PD (2009). The new friends vignettes: Measuring parental psychological control that confers risk for anxious adjustment in preschoolers. International Journal of Behavioral Development, 33, 481–495. 10.1177/0165025409103874. [DOI] [Google Scholar]
- Merkle EC (2011). A comparison of imputation methods for Bayesian factor analysis models. Journal of Educational and Behavioral Statistics, 36, 257–276. 10.3102/1076998610375833. [DOI] [Google Scholar]
- Merkle EC, & Rosseel Y (2018). blavaan: Bayesian structural equation models via parameter expansion. Journal of Statistical Software, 85, 1–30. 10.18637/jss.v085.i04.30505247 [DOI] [Google Scholar]
- Möller EL, Majdandzic M, & Bögels SM (2014). Fathers’ versus mothers’ social referencing signals in relation to infant anxiety and avoidance: A visual cliff experiment. Developmental Science, 17, 1012–1028. 10.1111/desc.12194. [DOI] [PubMed] [Google Scholar]
- Möller EL, Majdandzic M, & Bögels SM (2015). Parental anxiety, parenting behavior , and infant anxiety: Differential associations for fathers and mothers. Journal of Child and Family Studies, 24, 2626–2637. 10.1007/s10826-014-0065-7. [DOI] [Google Scholar]
- Möller EL, Majdandzic M, de Vente W, & Bögels SM (2013). The evolutionary basis of sex differences in parenting and its relationship with child anxiety in Western societies. Journal of Experimental Psychopathology, 4, 88–117. 10.5127/jep.026912. [DOI] [Google Scholar]
- Möller EL, Majdandzic M, Vriends N, & Bögels SM (2014). Social referencing and child anxiety: The evolutionary based role of fathers’ versus mothers’ signals. Journal of Child and Family Studies, 23, 1268–1277. 10.1007/s10826-013-9787-1. [DOI] [Google Scholar]
- Morey RD, Hoekstra R, Rouder JN, Lee MD, & Wagenmakers EJ (2016). The fallacy of placing confidence in confidence intervals. Psychonomic Bulletin & Review, 23, 103–123. 10.3758/s13423-015-0947-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey RD, & Rouder JN (2018). BayesFactor: Computation of bayes factors for common designs. Retrieved from https://CRAN.R-project.org/package=BayesFactor. [Google Scholar]
- Muris P, & Field AP (2011). The normal development of fear in children and adolescents In Silverman WK, & Field AP (Eds.). Anxiety disorders in children and adolescents: Research, assessment and intervention (pp. 76–89). (2nd ed.). Cambridge: Cambridge University Press. [Google Scholar]
- Murray L, Creswell C, & Cooper PJ (2009). The development of anxiety disorders in childhood: An integrative review. Psychological Medicine, 39, 1413–1423. 10.1017/s0033291709005157. [DOI] [PubMed] [Google Scholar]
- Natsuaki MN, Leve LD, Neiderhiser JM, Shaw DS, Scaramella LV, Ge X, & Reiss D (2013). Intergenerational transmission of risk for social inhibition: The interplay between parental responsiveness and genetic influences. Development and Psychopathology, 25, 261–274. 10.1017/s0954579412001010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogliari A, Spatola CAM, Pesenti-Gritti P, Medda E, Penna L, Stazi MA, …Fagnani C (2010). The role of genes and environment in shaping co-occurrence of DSM-IV defined anxiety dimensions among Italian twins aged 8-17. Journal of Anxiety Disorders, 24, 433–439. 10.1016/j.janxdis.2010.02.008. [DOI] [PubMed] [Google Scholar]
- Palomo J, Dunson DB, & Bollen K (2007). Bayesian structural equation modeling In Lee S-Y (Ed.). Handbook of latent variable and related models (pp. 163–188). Amsterdam: North-Holland; 10.1016/B978-044452044-9/50011-2. [DOI] [Google Scholar]
- Pine DS (1997). Childhood anxiety disorders. Current Opinion in Pediatrics, 9, 329–339. [DOI] [PubMed] [Google Scholar]
- Raley S, Bianchi SM, & Wang W (2012). When do fathers care? Mothers’ economic contribution and fathers’ involvement in child care. American Journal of Sociology 117, 1422–1459. 10.1086/663354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48, 1–36. Retrieved from http://www.jstatsoft.org/v48/i02/. [Google Scholar]
- Shevlyakov G, & Smirnov P (2011). Robust estimation of the correlation coefficient: An attempt of survey. Austrian Journal of Statistics, 40, 147–156. . [DOI] [Google Scholar]
- Silberg JL, Maes H, & Eaves LJ (2010). Genetic and environmental influences on the transmission of parental depression to children’s depression and conduct disturbance: An extended Children of Twins study. Journal of Child Psychology and Psychiatry, 51, 734–744. 10.1111/j.1469-7610.2010.02205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smirnov P (2014). Robcor: Robust correlations. Retrieved from https://CRAN.R-project.org/package=robcor.
- Spatola CAM, Rende R, & Battaglia M (2010). Genetic and environmental influences upon the CBCL/6-18 DSM-oriented scales: Similarities and differences across three different computational approaches and two age ranges. European Child & Adolescent Psychiatry, 19, 647–658. 10.1007/s00787-010-0102-z. [DOI] [PubMed] [Google Scholar]
- Tully EC, Iacono WG, & McGue M (2008). An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. American Journal of Psychiatry, 165, 1148–1154. 10.1176/appi.ajp.2008.07091438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Public Health Service (2000). Report of the surgeon general’s conference on children’s mental health: A national action agenda. Washington, DC: U.S. Department of Health and Human Services. [PubMed] [Google Scholar]
- Wickham H (2017). Tidyverse: Easily install and load the ‘tidyverse’. Retrieved from https://CRAN.R-project.org/package=tidyverse.
- Widaman KF, Ferrer E, & Conger RD (2010). Factorial invariance within longitudinal structural equation models: Measuring the same construct across time. Child Development Perspectives, 4, 10–18. 10.1111/j.1750-8606.2009.00110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widaman KF, & Thompson JS (2003). On specifying the null model for incremental fit indices in structural equation modeling. Psychological Methods, 8, 16–37. 10.1037/1082-989X.8.1.16. [DOI] [PubMed] [Google Scholar]
- Wu H, & Estabrook R (2016). Identification of confirmatory factor analysis models of different levels of invariance for ordered categorical outcomes. Psychometrika, 81, 1014–1045. 10.1007/s11336-016-9506-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zavos HMS, Rijsdijk FV, & Eley TC (2012). A longitudinal, genetically informative, study of associations between anxiety sensitivity, anxiety and depression. Behavior Genetics, 42, 592–602. 10.1007/s10519-012-9535-0. [DOI] [PubMed] [Google Scholar]


