Abstract
The aim of the current review was to assess whether there was an association between obesity and higher levels of hospitalization, poor outcomes and mortality due to the disease of novel coronavirus (COVID-19). Methodology: A systematic review of articles on the novel coronavirus, containing information on obesity and its association with COVID-19 morbidity and mortality. In the bibliographic research, four databases were used, with the terms ['COVID-19′] AND ['hospitalization'] AND ['obesity'] AND ['mortality']. Studies published from 12/01/2019 until 05/01/2020 were included. The research contains inclusive criteria targeting studies of humans adults infected by Sars-Cov-2, with or without comorbidities. This research was selected from publications in Spanish and English languages. Results: 96 articles were identified, 15 being presented in two databases. Twenty articles were included, with a population total estimated from 1 to 7671 patients, with a prevalence of obesity ranging from 13.3% to 68.6%. The association of obesity and mortality has been observed in at least 4 studies, that 85.3% of the population was hospitalized. Among 19 of the 20 studies, more severe forms of the disease were observed and in 14 of them, higher rates of complications among obese people infected with the new coronavirus. Limitation differences in the definition of obesity was observed among publications, of which obesity was considered from a body mass index >25 kg/m². Conclusions: In the current review, obesity and overweight were represented an unfavorable factor for infection of novel coronavirus, where the higher the BMI the worse the outcomes. This occurred by worsening the infection itself, as well as increasing the prevalence of hospitalizations, worst outcomes and greater lethality; especially when co-occurring with other chronic conditions and in the elderly as well. Given this evidence, greater attention is suggested to the obese and overweight population in the face of the current pandemic.
Keywords: COVID-19, Hospitalization, Obesity, Mortality
Introduction
The novel coronavirus (COVID-19) is a recently discovered infectious disease. The first case of COVID-19 was reported to the World Health Organization (WHO) by Chinese authorities on December 31, 2019, as a report about a patient who suffered pneumonia in the city of Wuhan, Hubei province. After a rapid spread in China, new outbreaks occurred in northern Italy and in several European countries, followed by an accelerated spread to many countries in the world. On March 12, 2020, WHO announced the outbreak of COVID-19 as a pandemic [1]. Worldwide, 10,710,005 cases of COVID-19 were confirmed, with 517,877 deaths by July 3, 2020. In the Americas, on the same date, 2,291,016 infected patients were registered [2]. In Brazil, according to the Coronavirus Panel of the Ministry of Health, by July 06, 2020, there were 1,603,055 confirmed cases, with 64,807 deaths. The fatality rate is 5.0%, and 30.9% of mortality [3].
The infection by Sars-Cov-2 found in the lifestyle of post-industrial societies, globalized, with a high flow of people between countries, sedentary lifestyle, poor diet quality, increased life expectancy and high prevalence of chronic diseases, a scenario which contributed to the rapid spread of the pathogen, as well as a greater disease severity of morbidity and mortality [4]. North American studies reinforced this information, in which patients with chronic conditions such as: cardiovascular disease, diabetes mellitus, chronic respiratory diseases, arterial hypertension and cancer. In addition to, the elderly which represented those infected with the novel coronavirus, and most susceptible to severe forms of the disease and the worst outcomes [5].
According to the WHO, overweight and obesity are defined as abnormal or excessive accumulation of fat that poses a health risk. A body mass index (BMI) equal to or greater than 25 kg/m² is considered as overweight and equal to or greater than 30 kg/m² is considered as obese [6]. In 2016, more than 1.9 billion adults aged 18 and over were overweight and, of these, 650 million were obese [6]. In a recent evaluation, obesity was present in 42.4% of the North American population, 19.8% in the brazilian and 10.9% in the italian [[7], [8], [9]]. In the chinese population, for example, the WHO has different definitions due to the biotype, with overweight being defined as a 23 kg/m² ≤ BMI < 27.5 kg/m² and general obesity as a BMI ≥ 27.5 kg/m² [10]. Obesity in China is a major health concern according to the WHO, with overall rates of obesity between 5% and 6% for the country, but greater than 20% in some cities where fast food is popular [11].
Obesity can cause many physical disabilities and psychological problems, increasing dramatically a person's risk of developing multiple noncommunicable diseases (NCDs), including cardiovascular diseases, cancer and diabetes [12]. In addition, it is frequently associated with high levels of hospitalization and admissions in intensive care units (ICUs), with morbidity and mortality rates higher than population averages [1,4,13,14]. In consonance, Simonnet et al. (2020) reinforced this affirmation observing a high prevalence of admissions (47.6%) in ICUs, pointing to obesity as an independent risk factor [15]. Thus, it was found that higher levels of body mass index (BMI) would maintain a relationship directly proportional to worse outcomes by the coronavirus disease [15].
In view of the necessity to know more about clinical manifestations, pathophysiological and prognostic considerations and in order to save as many lives as possible, the present review sought to evaluate the impact of obesity in in the course of the disease caused by the novel coronavirus.
Methods
A systematic review of studies on the novel coronavirus was done, relating it to information on the presence of obesity.
For this review, we used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) perspective, as well as its checklist, following all steps it describes [16]. The objectives were based on the PICO (Population; Intervention; Comparisons; Outcomes) strategy, as well as the choosing of the key words [17]. The bibliographical research was done using as strategy the following databases: PubMed, Science Direct, BVS Regional Portal and Lilacs, with the key words being: ['COVID-19′] AND ['hospitalization'] AND [‘obesity’] AND [‘mortality’]. Selected publication dates ranged from December 1 st, 2019 until May 1 st, 2020 (research date) [16]. For this systematic review, we developed a data extraction spreadsheet, matching a record of eligibility of the studies, describing study types, inclusion criteria, exclusion criteria, examiners evaluation and agreement regarding inclusion or not, number of participants, clinical outcomes (occurence of hospitalizations and mortality prevalence), suggested assumptions, study quality, possible biases and its considerations. Moreover, statistical methods and additional analysis were also used.
As initial identification criteria, all studies were considered, provided that they were with the inclusion criteria. Those criteria were: studies related to human beings, referred to adult aligned populations infected by the novel coronavirus. We included articles written in English or Spanish. The exclusion criteria were animal studies, studies involving infants or adolescents, abstracts of scientific events and book chapters. We strictly followed every step we established for identification, selection, inclusion and exclusion criteria. Because of the nature of review studies, approval by the Ethics Committee in Research for this work was not required [15].
Results
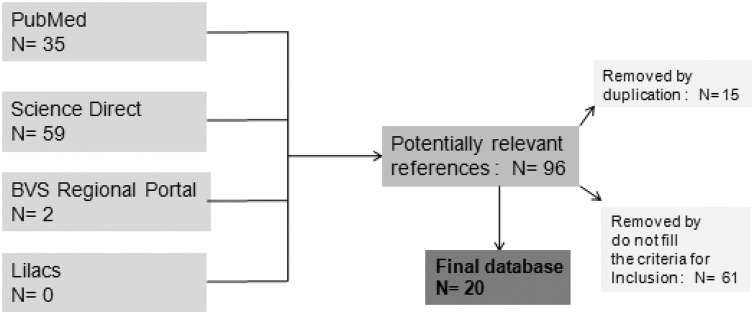
For the proposed review, 96 articles were identified, 35 of them in the PubMed database; Science Direct, 59 articles; BVS Regional Portal, 2 articles; Lilacs, no articles were found using the defined keywords. After reviewing the abstracts of the identified studies, 27 were chosen from the three databases. After the process for the present systematic review, 20 studies were included in the final selection list. Fig. 1 shows information from the selected articles.
Fig. 1.
The bibliographic search results.
Source: Produced by the authors.
Four systematic reviews were included, one narrative review and one integrative review, one guideline, one multicenter cohort study, four retrospective cohort studies, one case control study, two case series, one case report, three commentaries and one letter to the editor. Nine articles were originated in the United States of America, four in Italy, three in China, two in Spain, one in Mexico and one in France. The populations included in all the studies were COVID-19 infected patients, with ranging size from 1 to 5700 infected individuals. The total summarized number of patients was 7,671. Overall, 85.6% of this population infected with the novel coronavirus was hospitalized, with an obese population ranging from 13.3% to 68.6% (average of 44.9%). Among evaluated studies, mortality rate ranged from 3.2%–60.9% (average of 20.4%). The purpose of the studies was to determine the association of obesity with high rates of hospitalization, as well as with manifestations of the most severe forms of the coronavirus disease (19 out of 20 included articles). Fourteen out of the 20 studies reported higher prevalence complications among patients with obesity than among their non obese peers. Higher mortality among obese patients than among those without obesity infected with the novel coronavirus was observed in 4 publications. High BMI contributed to high mortality rates (Table 1 ).
Table 1.
Characteristics of the studies included in the analysis.
| Publication date | Authors | Journal | Location | Study Type | Infected population | Obesity (%) | COVID-19 severity | Complications (%) | Hospitalization (%) | Mortality (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| 04/25/2020 | Muscogiuri G; et al. | Metabolism 2020; 2020:1−12. | Naples, Italy | Systematic Review | 899 | 617 (68,6%) | Î | Î | Î | 471 (60,9%); Î |
| 04/26/2020 | Means C. | Metabolism 2020:108:154254. | Portland, USA | Systematic Review | Î | Î | ||||
| 03/31/2020 | Muniyappa R; et al. | Journal Physiol Endocrinol Metab 318(5):E736-E741. | Bethesda, Maryland, USA | Systematic Review | Î | Î | ||||
| 04−03-2020 | Severin R; et al. | Am J Med 2020;S0002-9343(20)30347-8. | Chicago, USA | Systematic Review/ Guideline | Î | Î | ||||
| 04/27/2020 | Khider L; et al. | JMV-Journal de Médecine Vasculaire 2020;1-6. | Paris, France and Toronto, Canadá | Guideline | Î | Î | ||||
| 04/18/2020 | Gomez JC; et al. | Rev Clin Esp 2020; | Zafra, Spain | Integrative Review | Î | Î | ||||
| 04/28/2020 | Delgado-Roche L; et al. | Archives of Medical Research 2020;1-4. | Ciudade de México, México | Narrative Review | Î | Î | 50,2 (15,8%); Î | |||
| 04/22/2020 | Redd WD; et al. | Gastroenterology 2020;1-14 | Boston, USA | Cohort Study | 318 | Î | Î | 318 (100%) | 32 (10.1%) | |
| 04-08-2020 | Li M; et al | Nutr, Metab and Cardiov Dis 2020; | Wuhan, China | Cohort Study | 83 | 42 (50%) | Î | 25 (30,12%) | 6 (7,2%) | |
| 04/26/2020 | Allocca M; et al. | Clin Gastroenterol Hepatol 2020; S1542-3565(20)30616-9. | Milan, Italy and Paris, France | Cohort Study | 15 | 2 (13,33%) | 5 (33,33%) | |||
| 03/27/2020 | MC Michael TM; et al | N Engl J Med 2020;21;382(21):2005-2011. | Seattle; USA | Cohort Study | 167 | 37 (22,2%) | 66 (39,5%) | 35 (21,0%) | ||
| 04/28/2020 | Chen Q; et al. | Infection 2020; 28:1-9. | Zhejiang, China | Cohort Study | 145 | 42 (28,96%) | Î | Î | 145 (100%) | |
| 04-08-2020 | Nobel YR; et al. | Gastroenterology 2020. | New York, USA | Control Case Study | 278 | 90 (33%) | Î | Î | 260 (93,5%) | 9 (3,2%) |
| 04/24/2020 | Richa Dson S; et al. | JAMA 2020;323(20):2052-2059. | New York, USA | Case Series | 5700 | 2528 (44,4%) | Î | Î | 5700 (100%) | 553 (21%); Î |
| 04/17/2020 | ZhenG KI; et al. | Metabolism 2020;1-17. | Wenzhou, China | Case Series | 66 | 45 (68,2%) | Î | 19 (28,8%) | ||
| 04/17/2020 | UllaH W; et al. | J Am Coll Cardiol Case Rep 2020:1-4. | Pennsylvania, USA | Case Report | Î | Î | ||||
| 04/16/2020 | Rebelos E; et al. | Metabolism 2020;108:154247. | Milan and Pisa, Italy | Letter to the Editor | Î | |||||
| 04/26/2020 | Stefan N; et al. | Nat Rev Endocrinol 2020; 1–2. | Munich, Germany and Boston, USA | Comments | Î | Î | ||||
| 04-05-2020 | Luzi L; Radaelli MG. | Acta Diabetol 2020; 1–6. | Milan, Italy | Comments | Î | Î | ||||
| 04-11-2020 | Puig-Domingo M; et al. | Endocrine 2020;1–4. | Badalona, Spain and Milan, Italy | Comments | Î | Î | Î |
Muscogiuri, et al. (2020) demonstrated that patients which were overweight or obese had a 72.1% prevalence. The patients with BMI above 40 kg/m² had high risk for novel coronavirus infection. In addition, in hospitalized patients with BMI higher than 35 kg/m², invasive mechanical ventilation had to be used in 85.7%, and those with BMI above 30 kg/m² and that were forwarded for mechanical ventilation, presented a mortality rate of 60.9% [1]. The recommendation and necessity of mechanical ventilation increased with increasing BMI [1].
Severin, et al. (2020) have considered as a possible aggravating factor for worse outcomes the consumption of oxygen up to 5 times higher in obese patients when compared to non obese patients in the mechanical ventilatory effort [13]. It was also demonstrated that obese patients with hepatic steatosis evolved to serious COVID-19 forms in 37.5% of the cases in contrast to 9.5%, compared to non obese individuals belonging to the same background [18]. Muniyappa, et al. (2020) and Means, et al. (2020) also searched for possible origins of more severe forms of coronavirus disease, and noticed that obese groups showed higher susceptibility to morbidity and mortality than non obese [4,19]. The increase in cytokine levels and immune hyperactivation acted as main factors that caused those outcomes in these obese groups [4,19].
In studies with COVID-19 positive population, Nobel, et al. (2020) observed that in a population of 278 patients classified according to BMI, at least 33% were obese [20]. During follow-up time (5–18 days), 260 patients needed hospitalization, including 16% in ICU, with a 3.2% death ratio [20]. These results were corroborated by Alloca, et al. (2020) cohort, in which patients with inflammatory bowel diseases and test positive for COVID-19 were evaluated and, between those, about 33% needed hospitalization, with an obesity rate among the hospitalized ones of 40% [21]. Redd, et al. (2020) observed that between 318 hospitalized patients, the majority presented BMI above 30 kg/m², associated to other risk factors such as cardiovascular disease or other comorbidities [22]. Chen, et al. (2020) observed that the most severely ill patients were elderly and presented comorbidities, most of them obesity and diabetes mellitus [23]. Li, et al. (2020) highlighted in their cohort that about half of the patients had cardiovascular diseases (CVDs), were overweight and clearly showed worst prognosis when compared to patients that didn’t have CVDs [24]. McMichael et al. (2020) observed high hospitalization rates (39.5%) and death rates (21%) in their cohort, in which patients were elderly (60%), and obese (22,2%) [25]. This evidence was reinforced by studies that showed that obesity would predispose to a worse clinical outcome by alterations in respiratory dynamics, manifestation of pulmonar hipertension and severe pneumonia [26,27]. Among patients diagnosed with COVID-19, the association to comorbidities such as obesity and chronic diseases, who could cause a worse disease outcome, was demonstrated by a high need for medical care in the population infected by novel coronavirus and presenting these characteristics. [24,27].
Puig-Domingo, et al. (2020) observed that young patients positive for COVID-19 with severe obesity would evolve more frequently to severe outcomes [27]. Gomez, et al. (2020) added information to these unfavorable prognosis, in which a worst humoral immune response would be related to more severe pulmonary lesions in the obese population, possibly being worsened by the inflammation and hypercoagulability state promoted by the novel coronavirus disease [28]. This affirmation was corroborated by a recent publication of the French Society of Vascular Medicine that highlighted the importance of doing prevention, diagnosis and treatment for venous thromboembolic disease in non hospitalized COVID-19 patients with higher BMI, since obesity is a risk factor for occurence of these episodes among these individuals [29].
Luzi, et al. (2020) reported a comparison between flu-like illnesses and COVID-19, which could predict the consequences of SARS-CoV-2 infection in obese population [30]. Stefan, et al. (2020) and Rebelos, et al. (2020) reinforced this theory, endorsing the relationship between high BMI and a critical course of COVID-19, in which the determinant link between obesity and diseases that predict the gravity of novel coronavirus infection, mainly arterial hypertension and diabetes mellitus, would justify this association [26,31]. Ullah, et al. (2020) pointed higher risk of thrombosis and pulmonary embolism in obese individuals, a risk that adds up to the hypercoagulability state induced by COVID-19 [32]. A case series study evaluated 4170 COVID-19 positive hospitalized patients in New York, United States of America, and showed that 41.7% had BMI ≥ 30 kg/m² and 19% presented BMI ≥ 35 kg/m² [33]. Stefan, et al. (2020), showed that a BMI ≥ 40 kg/m² was the second most important hospitalization predictor [26].
Discussion
This review demonstrated a correlation of increasing BMI, especially above 30 kg/m², with worse outcomes in patients infected with the novel coronavirus. The consulted papers also pointed out a greater severity of clinical manifestations of the novel coronavirus, higher prevalence of hospitalizations (mainly in ICUs), longer hospital stay and greater associated morbidity and mortality among those with obesity and other comorbidities.
We also reported that obesity increased the needs for medical care, in particular requiring complex procedures such as those provided in ICUs. The pandemic caused by the novel coronavirus had brought to light how a highly pathogenic virus could overwhelm health systems in the world, including developed countries. The demand for physical resources (especially ICUs and supplies) and human resources (professionals experienced in intensive care) for long periods (average length of stay) can lead to the exhaustion of the world's health systems [13,34]. A recent study showed that the historical rates of ICU occupancy in the USA varied between 66% and 82%, depending on the evaluated location [13,34]. Thus, in developing countries, where health systems are unable to provide universal assistance to their population, in a pandemic scenario with a sudden increase in demand, the fragility becomes evident [34]. In view of the current pandemic, humanity is facing a global challenge, with a growing and sudden need for greater resources in the health system, adequacy of infrastructure, qualified human resources, greater needs for beds and hospital supplies capable of as many lives as possible [13,34].
The consulted literature suggested that the novel coronavirus disease can be added to the list of high risk conditions affecting the obese population. Historically, obesity has been reported as an influencing factor for high mortality and duration in flu-like illnesses, even in those individuals who did not had other chronic conditions that could increase the risk of complications [30]. Even though there are not many studies consolidating the implications of COVID-19 in the obese population, a parallel can be drawn between influenza-like illnesses and the novel coronavírus, which could predict the consequences of SARS-CoV-2 infection in obese individuals. [30].
Obesity as a chronic and multifactorial disease is associated with a chronic inflammatory state, capable of developing a series of previously known and well-documented complications [36,37]. When this condition is added to the new scenario of the novel coronavirus, there is an increase in these complications and unfavorable results [1,13,[20], [21], [22], [23], [24], [25], [26], [27],30].
Obesity is a metabolic disease characterized by a hormonal, anti inflammatory and proinflammatory adiponectins imbalance due to the excess of dysfunctional adipose tissue. This imbalance interferes with the activation of the immune system, which can generate a bad immune response and, consequently, a worse prognosis for the obese [28,30]. Studies reinforced these information, demonstrating that high levels of proinflammatory cytokines that are produced in the adipose tissue (mainly in men) and the “cytokine storm”, a immune hyperactivation, could be possible causes of respiratory insufficiency in the most severe forms of COVID-19 [19,28,30,35]. Such outcome could be worsened by chronic conditions that commonly coexist with obesity, as type II diabetes mellitus and arterial hypertension, known risk factors for severe forms of COVID-19 [19,31].
Obese patients often have physiological respiratory dysfunction and, in addition, obesity increases the risk for hypoventilation associated pneumonia, pulmonary hypertension and cardiac stress, factors that could lead to a worse prognosis for COVID-19 [26]. Severe obesity is associated with sleep apnea syndrome, surfactant dysfunction and inadequate glycemic control (which is associated with impaired ventilatory function), and are also factors that could contribute to a worse prognosis [27]. Considering a mechanical ventilation scenario, another aggravating factor is that obese patients would be subject to longer periods of intubation, greater difficulty in weaning from mechanical ventilation and in the handling by professionals in non-specialized health centers, factors that could contribute to delay in treatment [13,26].
Obesity can represent an important thrombogenic risk factor. As a relevant example, there is the already reported greater susceptibility of obese people to the occurrence of pulmonary embolism, which may represent a strong unfavorable factor in the course of the disease of the novel coronavirus [32]. In addition to this worse humoral and cellular immune response already reported in previous studies, there were studies by Khider et al. (2020) that observed greater susceptibility and longer recovery time from infection, with the appearance of severe lung injuries. Thus, associated with the inflammatory factor, obesity could predispose the patient to a state of hypercoagulability, which could be aggravated by COVID-19 [28,29]. This fact would justify the recent guidelines on prevention, diagnosis and treatment of venous thromboembolism in non-hospitalized patients infected with COVID-19, who considered high BMI as one of the risk factors for the occurrence of thromboembolic episodes in these patients [29].
Consolidating these predictions about the prognosis of COVID-19 in obese patients, studies have reinforced obesity as a factor of greater morbidity during hospitalization, in addition to increasing the length of hospital stay [34]. Thus, the preservation of metabolic health becomes a fundamental objective for the reduction of damage to the obese population, in the times of COVID-19 [24].
As limitation of this review, it was observed that some studies considered obesity as having a BMI higher than 25 kg/m², in contrast to the WHO definition of obesity as being higher than 30 kg/m². Regarding the association of obesity with longer hospitalizations and longer periods of time, some articles did not discriminate the prevalence in relation to these conditions.
As strengths of this review, the relevance of the topic was highlighted, bringing to the discussion the effects of obesity, which has direct consequences in relation to morbidity and mortality and the financial impact generated by the current pandemic. Allied, the degree of agreement in the eligibility of the evaluated studies (greater than 0.7) and the quality of the review presented were points to be valued.
In the present review, obesity was a factor of poor prognosis for infection with the novel coronavirus, both because it worsened the infection (more severe forms of the disease in the obese population) and because it increased the prevalence of hospitalizations, with worse outcomes and greater lethality, mainly when co-occurring with other chronic conditions and in the elderly. In view of the current pandemic, greater attention is suggested to the obese and overweight population.
Financing
This work is part of the educational activities of the Extension Project entitled "Encouraging self-care learning for people with multimorbidities III", from the Medical School of the Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil; Profa. Dra. Arise Garcia de Siqueira Galil had no financial support, the content is the sole responsibility of the authors.
Competing interests
All authors declare that they have no financial relationships with any organization that may have an interest in the work submitted in the previous three years and no other relationship or activity that may appear to have influenced the work submitted.
Contributions
Siqueira JVV and Almeida LG, developed the details of the introduction, presentation of results and discussion, in addition to the detailed selection of articles, data collection and analysis. Zica BO and Brum IB were responsible for reading all the selected articles and judging those that were included, with a sequential review by Siqueira JVV, Almeida LG and Galil AGS, together with the writing of the discussion. Barceló A was responsible for being the third examiner of the work, with the final choice of the works included, with revision and refining of the manuscript. Galil AGS developed the idea of the study, collaborated in the selection, collection, data analysis and writing of the initial draft of the manuscript, in contribution with the other authors, as well as assuming the role of second examiner, collaborating in the final writing of the work. The authors state that the manuscript is an honest, accurate and transparent account of the study had being reported; that no important aspect of the study was omitted; and that any study discrepancies as planned have been explained. All rights reserved.
Ethical approval
It was not necessary.
Data sharing statement
All data used to prepare this article are available from the sources cited.
References
- 1.Muscogiuri G., Pugliese G., Barrea L., et al. Obesity: the “Achilles heel” for COVID-19? Metabolism. 2020;2020:1–12. doi: 10.1016/j.metabol.2020.154251. Doi.org/10.1016/ j.metabol.2020.154251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Folha informativa da OPAS em 03 de julho de 2020, disponível em: https://www.paho.org/bra/index.php?option=com_content&view=article&id=6101:covid19&Itemid=875.
- 3.Painel Coronavírus. Capturado em 06 de julho de 2020, Disponivel em: https://covid.saude.gov.br/.
- 4.Muniyappa R; Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Journal Physiol Endocrinol Metab 318(5):E736-E741. Doi: 10.1152/ajpendo.00124.2020. [DOI] [PMC free article] [PubMed]
- 5.CDC COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.OBESITY and overweight . 2020. World health organization (WHO) Disponible in: <https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight>. Captured in: july 5, 2020. [Google Scholar]
- 7.Adult Obesity Facts . 2020. Centers for disease control and prevention (CDC) Disponible in: <https://www.cdc.gov/obesity/data/adult.html> Captured in: jun 29, 2020. [Google Scholar]
- 8.Vigitel Brasil 2018: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2018 / Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Análise em Saúde e Vigilância de Doenças não Transmissíveis. – Brasília: Ministério da Saúde, 2019. Disponible in: https://portalarquivos2.saude.gov.br/images/pdf/2019/julho/25/vigitel-brasil-2018.pdf.
- 9.I.Stat, la banca dati completa per gli espertiI. Istituto Nazionale di Statistica (Statistiche Istat), 2020. Disponible in: <http://dati.istat.it/Index.aspx>. Captured in: jun 29, 2020.
- 10.Chen Y., Peng Q., Yang Y., et al. The prevalence and increasing trends of overweight, general obesity, and abdominal obesity among Chinese adults: a repeated cross-sectional study. BMC Public Health. 2019;19 doi: 10.1186/s12889-019-7633-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Obesity in China. Disponible in: <https://en.wikipedia.org/wiki/Obesity_in_China#:∼:text=Obesity%20in%20China%20is%20a,where%20fast%20food%20is%20popular>. Captured in: july 6,2020.
- 12.Obesity . 2020. World health organization regional office for europe (WHO/Europe) Disponible in: <https://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/obesity>. Captured in: july 5, 2020. [Google Scholar]
- 13.Severin R., Arena R., Lavie C.L., et al. Respiratory muscle performance screening for infectious disease management following COVID-19: a highly pressurized situation. Am J Med. 2020;S0002-9343(20):30347–30348. doi: 10.1016/j.amjmed.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boletim epidemiológico- secretaria de vigilância em saúde- ministério da saúde. Boletim Epidemiológico. 2020;51(16):1–35. Capturado em 29 de maio de 2020. Disponível em: https://www.saude.gov.br/images/pdf/2020/April/16/Boletim-epidemiologico-SVS-16.pdf. [Google Scholar]
- 15.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A., et al. Obesity (Silver Spring); 2020. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. 10.1002/oby.22831. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.PRISMA. Transparent Reporting of Systematic Reviews and Meta-análise. Capturado em 20/05/2020. Disponível em: http://www.prisma-statement.org/.
- 17.Santos C.M.C., Pimenta C.A.M., Nobre M.R.C. A estratégia PICO para a construção da pergunta de pesquisa e busca de evidências. Rev Latino-Am Enfermagem. 2007;15(3):1–4. [Google Scholar]
- 18.Zheng K.I., Gao F., Wang X.B., Sun Q.F., Pan K.H., Wang T.Y., et al. Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism. 2020:1–17. doi: 10.1016/j.metabol.2020.154244. Doi.org/10.1016/j.metabol.2020.154244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Means C. Mechanisms of increased morbidity and mortality of SARS- CoV-2 infection in individuals with diabetes: what this means for an effective management strategy. Metabolism. 2020;108 doi: 10.1016/j.metabol.2020.154254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nobel Y.R., Phipps M., Zucker J., et al. Gastrointestinal symptoms and COVID-19: case-control study from the United States. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.04.017. doi.org/10.1053/j.gastro.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Allocca M., Fiorino G., Zallot C., et al. Incidence and patterns of COVID-19 among inflammatory bowel disease patients from the Nancy and Milan cohorts. Clin Gastroenterol Hepatol. 2020;S1542-3565(20):30616–30619. doi: 10.1016/j.cgh.2020.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Redd W.D., Zhou J.C., Hathorn K.E., et al. Prevalence and characteristics of gastrointestinal symptoms in patients with SARS-CoV-2 infection in the United States: a multicenter cohort study. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Q., Zheng Z., Zhang C., et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID‐19) in Taizhou, Zhejiang, China. Infection. 2020;28:1–9. doi: 10.1007/s15010-020-01432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li M., Dong Y., Wang H., et al. Cardiovascular disease potentially contributes to the progression and poor prognosis of COVID-19. Nutr Metab Cardiovasc Dis. 2020 doi: 10.1016/j.numecd.2020.04.013. doi.org/10.1016/j.numecd.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mc Michael T.M., Currie D.W., et al. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stefan N., Birkenfeld A.L., Schulze M.B., et al. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol. 2020:1–2. doi: 10.1038/s41574-020-0364-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Puig-Domin/Go M., Giustina M.A. COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine. 2020:1–4. doi: 10.1007/s12020-020-02294-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gomez J.C., Lorido J.C., Sanchez F.J.C. La Obesidad y el coronavirus 2019-nCoV. Una relacion de riesgo. Rev Clin Esp. 2020 doi: 10.1016/j.rce.2020.04.008. [DOI] [Google Scholar]
- 29.Khider L., Soudet S., Laneelle D., et al. Proposal of the French Society of Vascular Medicine for the prevention, diagnosis and treatment of venous thromboembolic disease in out-patients with COVID 19. Jmv-journal Mã©decine Vasc. 2020 doi: 10.1016/j.jdmv.2020.04.008. doi.org/10.1016/j.jdmv.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luzi L., Radaelli M.G. Infuenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020:1–6. doi: 10.1007/s00592-020-01522-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rebelos E., Moriconi D., Virdis A., et al. Importance of metabolic health in the era of COVID-19. Metabolism. 2020;108 doi: 10.1016/j.metabol.2020.154247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ullah W., Saeed R., Sarwar U., et al. COVID-19 complicated by acute pulmonary embolism and right-sided heart failure. J Am Coll Cardiol Case Rep. 2020:1–4. doi: 10.1016/j.jaccas.2020.04.008. http://creativecommons.org/licenses/by- nc-nd/4.0/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 — united States, February 12–march 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Delgado-Roche L., Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch Med Res. 2020:1–4. doi: 10.1016/j.arcmed.2020.04.019. Doi.org/10.1016/j.arcmed.2020.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murphy N.F., Macintyre K., Stewart S., et al. Long-term cardiovascular consequences of obesity: 20-year follow-up of more than 15 000 middle-aged men and women (the Renfrew–paisley study) European Heart Journa. 2006;27(1):96–106. doi: 10.1093/eurheartj/ehi506. doi.org/10.1093/eurheartj/ehi506. [DOI] [PubMed] [Google Scholar]
- 37.Djalalinia S., Qorbani M., Peykari N., et al. Health impacts of obesity. Pak J Med Sci. 2015;31(1):239–242. doi: 10.12669/pjms.311.7033. [DOI] [PMC free article] [PubMed] [Google Scholar]