To the editor,
Globally, healthcare workers (HCWs) have met an unprecedented challenge since the outbreak of coronavirus disease 2019 (COVID-19). HCWs made up 9.0% of the confirmed cases in Italy [1] and nearly 14.0% of the confirmed cases in Spain [2] in the first month of their respective outbreaks. Reasons for the rapid surge in HCW cases may in part be the lack of effective protection measures. Personal protective equipment (PPE) has been recommended for HCWs [3] and it is important to evaluate its efficacy in protecting this vulnerable population while combating COVID-19.
We conducted a cross-sectional survey (Supplementary Table S1) on PPE usage among 3476 HCWs who completed 14-day quarantine after their healthcare service for COVID-19 patients in Hubei province (the Chinese epicentre of the epidemic); the survey was carried out via the media platform Wechat between April 21 and May 15 2020. Our online questionnaire included (a) items selected from the WHO guidance for risk assessment and management of exposure of HCWs in the context of COVID-19 [4], (b) questions addressing the results of SARS-CoV-2-related tests (virus RNA and specific neutralizing antibody) before ending quarantine, and (c) PPE-related toxicities. To better track the use of PPE by HCWs, we stratified participants by HCW type (doctor, nurse, and others) and working area (three groups, detailed in Supplementary Material: Method), and scored the frequency of use of each type of PPE. More method details are provided in Supplementary Material: Method.
Responses were obtained from a total of 960 HCWs who had provided healthcare service in over 37 Hubei hospitals (Supplementary Material Table S2). The response rate was 27.6%. Most participants were female (617, 64.3%), nurses (625, 65.1%), and HCWs assigned to work in Wuhan city (at least 856, 89.2%); the median age of the respondents was 33 (IQR 23–43) years. All participants were exposed to SARS-CoV-2 with a median period of 40 (IQR 16–64) days, and 926 (96.5%) of them cared directly for a confirmed COVID-19 patient.
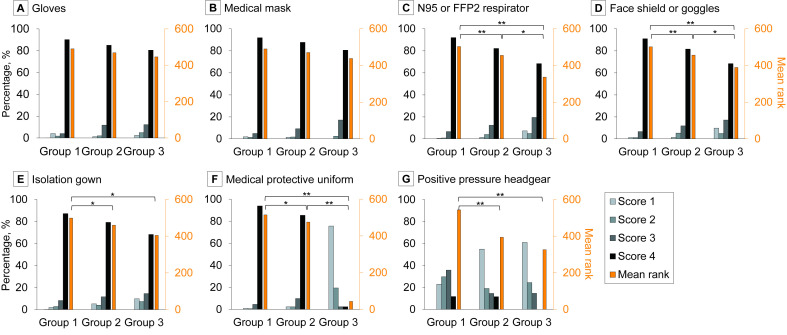
Before ending quarantine, all participants had three consecutive RT-PCR tests (7 days apart), and 672 (70.0%) were also tested for anti-SARS-CoV-2 IgG and IgM; 30.0% of the participants were not required to take this test, thus their results are unknown. All results were negative. Fig. 1 summarizes the frequency of use of each type of PPE in each HCW group, stratified by working area, and showed that there were no significant differences in the use of gloves or medical masks among the three groups; however, all other types of PPE were used most in group 1, and HCWs in group 2 (compared with those in group 3) used more N95/FFP2 respirators, face shields or goggles, and medical protective uniforms.
Fig. 1.
The usage frequency of each piece of personal protective equipment (PPE) among healthcare workers (HCWs) stratified by working area. HCWs were stratified into ‘group 1’ (n = 573, mainly working in the intensive care unit, laboratory, testing room, and operating room), ‘group 2’ (n = 346, mainly working in the fever outpatient department, general patient room, Fangcang shelter hospital, emergency department, cleaning area, imaging examination area, and transfer vehicle), and ‘group 3’ (n = 41, mainly working in the general outpatient department, community, pharmacy, and administrative area). The frequency of PPE usage was scored: score 4 = always (>95% of the time), score 3 = most of the time (≥50% but not 100%), score 2 = occasionally (20% to <50%), and score 1 = rarely (<20%). Mean rank was calculated via Kruskal–Wallis test to compare the usage frequency of each PPE among groups. ∗∗Adjust p < 0.001, ∗ adjust p < 0.05.
PPE-related adverse events occurred in 838 participants (87.3%). The most common types were skin injury (598, 62.3%), dyspnoea (593, 61.8%), dizziness (555, 57.8%), and headache (516, 53.8%) (Table 1 ). Evidence from the comparison of HCWs with any adverse events versus those without any adverse events showed that older age (33 versus 31 median years, p 0.016) and more consecutive days using PPE (40 versus 35 median days, p 0.001) were associated with a greater risk of adverse events (Supplementary Table S3). HCWs had an increased risk of adverse events from group 3 (2.6%) to group 2 (34.7%) to group 1 (62.6%), with p < 0.05 between any two groups. Both doctors (30.2%) and nurses (66.5%) had greater risks of adverse events compared with other types of HCWs (3.3%, both p < 0.05).
Table 1.
Characteristics and responses of 960 participants
| Characteristic | No. (%) |
|---|---|
| Age, median (IQR), year | 33 (23.0–43.0) |
| Sex, female | 617 (64.3) |
| Type of healthcare worker: | |
| aDoctor | 280 (29.2) |
| bNurse | 625 (65.1) |
| cOthers | 55 (5.7) |
| Main working area: | |
| Fever outpatient department | 15 (1.6) |
| General outpatient department or community | 12 (1.3) |
| General patient room (non-intensive care unit) | 100 (10.4) |
| Intensive care unit | 556 (57.9) |
| Fangcang shelter hospital | 188 (19.6) |
| Emergency department | 30 (3.1) |
| Testing room | 9 (0.9) |
| Cleaning area | 5 (0.5) |
| Laboratory | 4 (0.4) |
| Operating room | 4 (0.4) |
| Imaging examination area | 4 (0.4) |
| Others (pharmacy, administrative area, transfer vehicle, and others) | 33 (3.4) |
| Providing direct care to a confirmed patient | 926 (96.5) |
| dPerforming any aerosol-generating procedures on the patient | 577 (60.1) |
| Accidental contact with body fluid/respiratory secretions of a confirmed patient | |
| Any | 72 (7.5) |
| In the mucous membrane of eyes | 26 (2.7) |
| In the mucous membrane of mouth/nose | 27 (2.8) |
| On non-intact skin | 40 (4.2) |
| Puncture/sharp accident with any material contaminated with biological fluid/respiratory secretions | 24 (2.5) |
| Duration with PPE per day, median (IQR), hour | 6 (5.0–7.0) |
| Consecutive days with PPE, median (IQR), day | 40 (16.0–64.0) |
| Always or most of time adhere to PPE protocols as trained | 946 (98.6) |
| Adverse event: | |
| Any | 838 (87.3) |
| Skin squeeze | 598 (62.3) |
| Dyspnoea | 593 (61.8) |
| Dizziness | 555 (57.8) |
| Headache | 516 (53.8) |
| Rash | 222 (23.1) |
| Dry skin | 199 (20.7) |
| Allergy | 162 (16.9) |
| Dermatitis | 146 (15.2) |
| Maceration | 142 (14.8) |
| Conjunctivitis | 61 (6.4) |
| Stumble | 59 (6.1) |
| Real-time RT-PCR test (three times): | |
| Negative | 960 (100.0) |
| Positive | 0 |
| Anti-SARS-CoV-2 IgM test: | |
| Negative | 672 (70.0) |
| Positive | 0 |
| Anti-SARS-CoV-2 IgG test: | |
| Negative | 672 (70.0) |
| Positive | 0 |
IQR, interquartile range; PPE, personal protective equipment; RT-PCR, reverse transcriptase–polymerase chain reaction.
Mainly including medical doctor, physician assistant, radiology technician, ophthalmologist, physical therapist, respiratory therapist, midwife, psychotherapist, nutritionist, and physiotherapist.
Mainly including registered nurse, assistant nurse, and nurse technician.
Mainly including laboratory personnel, pharmacist, pharmacy technician or dispenser, administrator, admission/reception clerk, patient transporter, and cleaner.
Mainly including nebulizer treatment, open airway suctioning, collection of sputum, tracheotomy bronchoscopy, and cardiopulmonary resuscitation.
The present study focuses on the efficacy and safety of PPE for HCWs in the Chinese epicentre of COVID-19, which we believe is critical to establishing appropriate responses to this and future epidemics.
First, the negative results of RT-PCR tests in all participants with a median 40-day exposure duration—along with negative results of antibody tests in 70.0% of participants showing that they were never infected—indicated that PPE is an efficacious measure to durably contain the nosocomial transmission of SARS-CoV-2.
Second, the efficacy of different PPE among HCWs in different working areas supports the need for guidance on rationalizing, prioritizing, and grading the use of PPE according to HCWs' infection risk. This information can also address the critical shortages of PPE, allowing appropriate allocation of PPE.
Third, basic emergency guidance or directive of PPE for protecting HCWs should be issued at the earliest stage of an epidemic, not months later. Furthermore, the need for emergency stocks of PPE has been highlighted to avoid the dire consequences of PPE shortages.
Fourth, PPE was commonly associated with adverse events in our participants, although 98.6% of them showed high levels of adherence to PPE protocols. These effects are mild in most cases but can affect HCWs both physically and psychologically. The need for improvements in PPE design is highlighted, especially with HCWs' participation and contributions.
Author contributions
YZ, WL, YL, YC, PL and RZ all contributed equally to this article as joint first authors. JH and AC supervised the overall study. JH, AC and YZ contributed to the study concept and design. WL and YC collected the data. YZ, YL and RZ analysed and interpreted the data. PL produced the figure and tables. YZ, YL and AC wrote the manuscript, and all authors approved its final version.
Transparency declaration
The authors declare no competing interests. This study was supported by the National Natural Science Foundation of China (grant number 81903421).
Ethics committee approval
The institutional review board at The First Affiliated Hospital of Guangzhou Medical University approved this study, and informed consent was obtained from all participants.
Editor: L. Leibovici
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cmi.2020.07.029.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.International Council of Nurses . 2020. High proportion of healthcare workers with COVID-19 in Italy is a Stark warning to the world: protecting nurses and their colleagues must be the number one priority.https://www.icn.ch/news/high-proportion-healthcare-workers-covid-19-italy-stark-warning-world-protecting-nurses-and Available from: [Google Scholar]
- 2.Minder R., Peltier E. The New York Times; 2020. Virus knocks thousands of health workers out of action in Europe.https://www.nytimes.com/2020/03/24/world/europe/coronavirus-europe-covid-19.html Available from: [Google Scholar]
- 3.World Health Organization . 2020. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim Guidance.https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf Available from: [Google Scholar]
- 4.World Health Organization . 2020. Risk assessment and management of exposure of health care workers in the context of COVID-19: interim Guidance.https://apps.who.int/iris/bitstream/handle/10665/331496/WHO-2019-nCov-HCW_risk_assessment-2020.2-eng.pdf Available from: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.