Abstract
Study objective
Emergency medical services (EMS) may serve as a key source of real-time data about the evolving health of coronavirus disease 2019 (COVID-19)–affected populations, especially in low- and middle-income countries with less rapid and reliable vital statistics registration systems. Although official COVID-19 statistics in Mexico report almost exclusively inhospital mortality events, excess out-of-hospital mortality has been identified in other countries, including 1 EMS study in Italy that showed a 58% increase. Additionally, EMS and hospital reports from several countries have suggested that silent hypoxemia—low Spo2 in the absence of dyspnea—is associated with COVID-19. It is unclear, however, how these phenomena can be generalized to low- and middle-income countries. We assess how EMS data can be used in a sentinel capacity in Tijuana, a city on the Mexico–United States border with earlier exposure to COVID-19 than many low- and middle-income country settings.
Methods
In this observational study, we calculated numbers of weekly out-of-hospital deaths and respiratory cases handled by EMS in Tijuana, and estimated the difference between peak epidemic rates and expected trends based on data from 2014 to 2019. Results were compared with official COVID-19 statistics, stratified by neighborhood socioeconomic status, and examined for changing demographic or clinical features, including mean Spo2.
Results
An estimated 194.7 excess out-of-hospital deaths (95% confidence interval 135.5 to 253.9 deaths) occurred during the peak window (April 14 to May 11), representing an increase of 145% (95% CI 70% to 338%) compared with expected levels. During the same window, only 5 COVID-19–related out-of-hospital deaths were reported in official statistics. This corresponded with an increase in respiratory cases of 236.5% (95% CI 100.7% to 940.0%) and a decrease in mean Spo2 to 77.7% from 90.2% at baseline. The highest out-of-hospital death rates were observed in low-socioeconomic-status areas, although respiratory cases were more concentrated in high-socioeconomic-status areas.
Conclusion
EMS systems may play an important sentinel role in monitoring excess out-of-hospital mortality and other trends during the COVID-19 crisis in low- and middle-income countries. Using EMS data, we observed increases in out-of-hospital deaths in Tijuana that were nearly 3-fold greater than increases reported in EMS data in Italy. Increased testing in out-of-hospital settings may be required to determine whether excess mortality is being driven by COVID-19 infection, health system saturation, or patient avoidance of health care. We also found evidence of worsening rates of hypoxemia among respiratory patients treated by EMS, suggesting a possible increase in silent hypoxemia, which should be met with increased detection and clinical management efforts. Finally, we observed social disparities in out-of-hospital death that warrant monitoring and amelioration.
Introduction
Background
As coronavirus disease 2019 (COVID-19) spreads across most countries, real-time information is required to detect and manage the health of populations. This is a particular challenge in low- and middle-income countries, such as Mexico, because of less rapid and robust vital statistics registration systems. Although a vital statistics registration system does exist in Mexico, official statistics are available on an approximately 2-year lag, and records of mortality are not always reliable, a condition similar to that of most low- and middle-income countries.1, 2, 3, 4, 5 Although a number of reports in the popular press have suggested Mexico is significantly undercounting deaths from COVID-19,6 , 7 these claims have not been evaluated with excess mortality analyses because official total mortality statistics have not been available for Mexico beyond 2018 as of May 2020.8 Given these data restrictions, information from emergency medical services (EMS) may serve as a key source of real-time knowledge about the evolving health of COVID-19–affected populations, offering information of clinical significance.
Editor’s Capsule Summary.
What is already known on this topic
Emergency medical services (EMS) clinical data can be used for health surveillance; this is typically done in high-income countries. The coronavirus disease 2019 pandemic has shown the need for rapid and accurate health surveillance in every country, including those that cannot perform extensive population testing.
What question this study addressed
The study examined EMS data in a Mexican city as a proxy for a test-based diagnosis of coronavirus disease 2019. Increases were observed in out-of-hospital deaths and respiratory complaints. A decrease in average patient oxygen saturation was also found.
What this study adds to our knowledge
This study supports the idea that EMS data can be used for effective surveillance for a specific illness in accordance with its characteristic clinical effects.
How this is relevant to clinical practice
This study may lead to more EMS data for surveillance, especially perhaps in resource-challenged areas.
Importance
EMS data may play a particular role in measuring out-of-hospital mortality. As the epidemiologic properties of the COVID-19 pandemic have become more clear, excess mortality has become an important area of study. A small number of analyses have been published—initially largely by news organizations—describing excess total mortality.9, 10, 11 However, because of the aforementioned limitations, no official data from Mexico, or the majority of low- and middle-income countries, were available as of May 2020. Out-of-hospital deaths represent an important facet of total excess mortality, which may be particularly suited for measurement with EMS data. One recent report from the Lombardy region of Italy used EMS records to show an increase during the peak of the epidemic of 58% compared with previous-year values.12 This phenomenon has also been documented in the popular press for certain cities in the United States.13 , 14 It is unclear, however, how it would develop in low- and middle-income countries with relatively weaker health systems.15, 16, 17, 18, 19 In the context of COVID-19, an increase in out-of-hospital mortality could be expected either directly from COVID-19 or indirectly as patients delay care and health systems become overwhelmed.20, 21, 22 Nevertheless, rates of out-of-hospital mortality remain a generally understudied facet of the pandemic,10 , 11 , 23 and to our knowledge, there is little or no evidence on the topic for low- and middle-income countries.
Another key area that can be monitored with data from EMS systems during the COVID-19 pandemic is the detection of silent hypoxemia. Reports initially from China, and later Italy, the United States, and Norway, have described many COVID-19 patients who initially present with hypoxemia without signs of respiratory distress (silent hypoxemia) and later develop respiratory failure.24, 25, 26, 27 It is possible that this kind of hypoxemia, and subsequent rapid decompensation,28 results in mortality before patients are able to access EMS or hospital services, especially in areas in which health systems are saturated or patients are not able to quickly access health care services when decompensation occurs.
Mexico is a middle-income country that experienced its first confirmed case of COVID-19 on February 27 and reached 10,000 cases by April 17, according to official statistics.29 Tijuana, in Northern Mexico, is a city of greater than 1.7 million inhabitants that shares a heavily crossed border with San Diego County in California.30 As of May 2020, the international border remained open to residents of the United States, although Mexican nationals with tourist visas were generally barred from crossing beginning in late March. Tijuana therefore may have been subjected to earlier exposure to severe acute respiratory syndrome coronavirus 2 than the rest of Mexico because of the importation of cases from California.31 , 32 Reported cases of COVID-19 in Tijuana were among the first in Mexico, beginning on March 17. On May 11, Tijuana had the highest number of COVID-19 deaths of any municipality in the country (170), and the mortality rate (17.3 per 100,000 people) was almost 6 times the national rate of 3.1 per 100,000 people.29 , 30 , 33 Therefore, Tijuana may represent an important bellwether for the rest of Mexico and have general relevance to trends that will be subsequently experienced by the EMS systems of other low- and middle-income countries.
Goals of This Investigation
Our primary objective was to use EMS data from Tijuana to describe the potential sentinel role for such data in monitoring the epidemiologic profile of the COVID-19 epidemic in a low- and middle-income-country context. We focused the analysis on trends in out-of-hospital mortality and silent hypoxemia among respiratory patients. We also sought to characterize any changes in demographics, geography, and neighborhood socioeconomic status among these patient groups. Additionally, we aimed to compare trends documented by the EMS system with official government statistics describing COVID-19 cases and deaths.
Materials and Methods
Study Design and Setting
We used data from the Mexican Red Cross in Tijuana, which responds to approximately 98% of 911 activations of EMS care in the city.34 We drew on routinely collected, deidentified, encounter-level records describing patient characteristics and the provision of EMS. We conducted a retrospective, descriptive analysis comparing the observed peak epidemic with previous trends. We excluded calls that were cancelled before the ambulance arrived at the scene. Given that rates of violence in Tijuana have been highly variable in recent years, complicating the estimation of expected trends, we also excluded patients with traumatic injuries from all analyses. Data were available for most of January 2014 through July 13, 2020, although some records, including files from 2018 and February 2020, were not available in digital form on the rapid timescale required to conduct this analysis. Publicly available data describing official confirmed cases and deaths stemming from COVID-19 were obtained from the Mexican National Office of Epidemiology.35 This study was deemed exempt from review by the University of California, Los Angeles institutional review board.
The EMS system in Tijuana, Mexico, is run as a collaboration between the local city government and the Mexican Red Cross, a nongovernmental organization. The system serves an estimated population of 1.75 million people (based on the 2010 census), with a mixed social profile spanning very-low-income and high-income areas.37 EMS care is regulated at the municipal and national level.36 A 911 dispatch center is operated by the city of Tijuana. Once a 911 call has been deemed a medical emergency, emergency medical technicians (EMTs) from the Tijuana chapter of the Mexican Red Cross classify the incident according to dispatch protocols and triage information and direct the closest first-responder unit to the scene. The Mexican Red Cross EMS personnel respond to approximately 98% of 911 activations leading to medical care in Tijuana, with the remainder being attended to by the city fire department or private ambulance companies. The Mexican Red Cross operates with 13 ambulances distributed in 6 EMS bases throughout the city. In Mexico, there are 3 levels of EMT training: basic, intermediate, and advanced. The ambulances are staffed with an EMT–basic and either a second EMT–basic or an EMT–intermediate. In addition, there is 1 rescue unit and 1 rapid response vehicle. The latter responds to emergencies and is staffed by an out-of-hospital physician, EMT–advanced, or EMT–intermediate but is not designed for patient transfer. The field staff is currently composed of 80 EMTs–basic, 13 EMTs–intermediate, 3 EMTs–advanced, and 3 out-of-hospital physicians. EMTs work 24-hour shifts, whereas out-of-hospital physicians’ shifts are 8 hours. In addition, there is a field supervisor who helps coordinate and manage care during each 24-hour shift. Medical control is provided by either the out-of-hospital medical director or physicians who staff the Mexican Red Cross Hospital’s emergency department. During the study period, the Mexican Red Cross in Tijuana responded to an average of 30,500 completed calls per year.
For the duration of the study, data collection at the Mexican Red Cross in Tijuana was performed through an out-of-hospital electronic medical record. Data were entered in a tablet during the patient encounter and were transferred at the end of each shift to a central repository. Completeness of the medical record was checked in weekly audits and monthly case-review sessions.
Methods of Measurement
Out-of-hospital mortality was defined as a case in which a patient was found dead on EMS arrival or died before reaching a hospital, as documented by EMS. We also assessed the number of cases of respiratory morbidity. This was defined as either a chief complaint of “respiratory,” “difficulty breathing,” or “respiratory infection” or a chief complaint that was metabolic or gastrointestinal, combined with an Spo 2 of less than 92%. The first group composed the majority of respiratory cases. The decision to include gastrointestinal or metabolic patients with low Spo 2 reflected recent reports of atypical COVID-19 patients presenting with chiefly gastrointestinal symptoms,38 as well as the association with diabetes mellitus.39 In all cases, if a series of Spo 2 measurements was recorded, we used the first available value, recorded before treatment began. It was protocolized that initial Spo 2 was measured before application of oxygen.
For cases of out-of-hospital mortality, we assessed patient age, sex, health insurance status (including uninsured, privately insured, or membership in one of several main public health care systems), time from ambulance dispatch to ambulance arrival, whether cardiopulmonary resuscitation (CPR) was administered, neighborhood of residence, and administrative geostatistical-area-level socioeconomic status. For respiratory cases, we assessed the aforementioned variables as well as level of consciousness and Spo 2.
The neighborhood of residence was mapped with a shape file from the Mexican National Population Council. An index of socioeconomic status and populations was provided at the level of basic geostatistical areas defined by the Mexican Institute of Statistics and Geography,40 , 41 which typically include several neighborhoods and are based on 2010 census data. We created a categoric socioeconomic status variable, defined as population-weighted quintiles of the continuous socioeconomic status variable, categorized as lowest, low, medium, high, and highest. Because neighborhoods and basic geostatistical area do not overlap perfectly, a linkage was performed between them to assign socioeconomic status values to each neighborhood. This involved finding the midpoint of each neighborhood and assigning it the socioeconomic status value of the basic statistical unit where it was located. In the small number of cases in which the midpoint of a neighborhood fell outside of a defined basic geostatistical area, the neighborhood cluster was assigned to the closest basic geostatistical area to the midpoint.
Official data describing COVID-19 cases and deaths35 in Tijuana were aggregated to weekly totals and graphed alongside EMS-documented numbers.
Primary Data Analysis
Changes in out-of-hospital mortality were assessed by comparing weekly statistics from January through July 2020 with forecasted values estimated by using baseline trends from January 1, 2014, to December 31, 2019. The process was repeated for the primary outcome measures (number of out-of-hospital deaths and number of respiratory cases), as well as 2 outcomes assessed as sensitivity analyses (proportion of cases that resulted in out-of-hospital mortality and proportion of cases that were respiratory) to control for potential differences in case volume. Using ordinary least squares regression, we modeled the seasonal time trend with a fixed-effect dummy variable on each week of the year. The secular trend was captured with a linear continuous fixed effect on year. Forecasts with 95% prediction intervals were made by extrapolating the model through July 2020. Ratios of observed to expected numbers and proportions, and their uncertainty intervals, were calculated by dividing the observed value in each week by the forecasted value and prediction interval. We compared pre-epidemic Spo 2 values with those observed during the peak epidemic period. We also described trends in the distribution of Spo 2 during the epidemic, as measured by quintiles of the distribution of Spo 2, and examined the relationship between Spo 2 and level of consciousness. For all analyses, “peak COVID” windows were defined as starting the week in which the outcome—either out-of-hospital mortality or respiratory morbidity—increased clearly above the baseline 95% prediction interval, and ending after the outcome value began to decrease sharply or become insignificantly elevated above baseline projections.
We also sought to ensure that no difference in nomenclature, classification, or life support practices occurred in response to the onset of the COVID-19 crisis that could cause an apparent increase in out-of-hospital mortality. We therefore assessed rates of CPR, ambulance transit times, and the total composition of all cases before and during the COVID-19 period.
All cases were included in the sections of the analysis for which they had available data. Missing values are noted as applicable in Tables 1 and 2 .
Table 1.
Characteristics of patients with out-of-hospital mortality.
| All 2019 (N=1,569) | April 14 to May 11 (N=329) | |
|---|---|---|
| Age, y | ||
| Mean (SD) | 59.2 (20.1) | 58.0 (17.4) |
| Median (min, max) | 60.0 (1.00, 104) | 59.0 (1.00, 97.0) |
| Missing (%) | 3 (0.2) | 0 |
| Categoric age (%) | ||
| 0–18: pediatric | 43 (2.7) | 5 (1.5) |
| 18–64: adult | 871 (55.5) | 211 (64.1) |
| ≥65: elderly | 652 (41.6) | 113 (34.3) |
| Missing | 3 (0.2) | 0 |
| Sex (%) | ||
| Women | 499 (31.8) | 104 (31.6) |
| Men | 1,070 (68.2) | 225 (68.4) |
| Health insurance (%) | ||
| IMSS | 469 (29.9) | 151 (45.9) |
| ISSSTE∗ | 51 (3.3) | 6 (1.8) |
| Uninsured | 686 (43.7) | 140 (42.6) |
| Seguro Popular/INSABI† | 285 (18.2) | 20 (6.1) |
| Private insurance | 78 (5.0) | 12 (3.6) |
| CPR (%) | ||
| Advanced | 21 (1.3) | 1 (0.3) |
| Basic | 47 (3.0) | 4 (1.2) |
| None | 1,501 (95.7) | 324 (98.5) |
| Call-to-arrival time, min | ||
| Mean (SD) | 16.4 (10.1) | 20.5 (12.6) |
| Median (min, max) | 15.0 (0, 190) | 19.0 (0, 135) |
| Missing (%) | 65 (4.1) | 26 (7.9) |
ISSSTE, Instituto de Seguridad y de Servicios Sociales de los Trabajadores del Estado; INSABI, Instituto Nacional de Salud para el Bienestar.
Numbers exclude trauma-related deaths. The peak observed mortality period, April 14 to May 11, is compared with all of 2019.
Health insurance for government workers.
Social safety net health insurance.
Table 2.
Characteristics of respiratory patients by week.
| March 31 (N=53) | April 7 (N=73) | April 14 (N=79) | April 21 (N=67) | April 28 (N=90) | May 5 (N=84) | All 2019 (N=1253) | |
|---|---|---|---|---|---|---|---|
| Age | |||||||
| Mean (SD), y | 55.8 (18.6) | 51.3 (17.1) | 49.6 (18.9) | 53.8 (15.6) | 55.1 (15.9) | 57.8 (14.5) | 53.5 (24.6) |
| Median (min, max) | 55.5 (1.00, 95.0) | 51.0 (19.0, 89.0) | 44.0 (1.00, 94.0) | 52.5 (2.00, 97.0) | 56.0 (4.00, 88.0) | 58.0 (28.0, 92.0) | 56.0 (1.00, 105) |
| Missing (%) | 1 (1.9) | 0 | 0 | 0 | 0 | 0 | 2 (0.2) |
| Categoric age (%) | |||||||
| 0–18: pediatric | 1 (1.9) | 0 | 1 (1.3) | 1 (1.5) | 2 (2.2) | 0 | 118 (9.4) |
| 18–64: adult | 37 (69.8) | 59 (80.8) | 57 (72.2) | 51 (75.0) | 63 (70.0) | 55 (65.5) | 666 (53.2) |
| ≥65: elderly | 14 (26.4) | 14 (19.2) | 21 (26.6) | 16 (23.5) | 25 (27.8) | 29 (34.5) | 467 (37.3) |
| Missing | 1 (1.9) | 0 | 0 | 0 | 0 | 0 | 2 (0.2) |
| Sex (%) | |||||||
| Women | 24 (45.3) | 30 (41.1) | 24 (30.4) | 28 (41.2) | 29 (32.2) | 37 (44.0) | 569 (45.4) |
| Men | 29 (54.7) | 43 (58.9) | 55 (69.6) | 40 (58.8) | 61 (67.8) | 47 (56.0) | 684 (54.6) |
| Health insurance (%) | |||||||
| IMSS | 35 (66.0) | 54 (74.0) | 56 (70.9) | 42 (61.8) | 57 (63.3) | 53 (63.1) | 487 (38.9) |
| ISSSTE∗ | 2 (3.8) | 1 (1.4) | 0 | 3 (4.4) | 2 (2.2) | 6 (7.1) | 46 (3.7) |
| Uninsured | 11 (20.8) | 11 (15.1) | 16 (20.3) | 18 (26.5) | 23 (25.6) | 18 (21.4) | 310 (24.7) |
| Seguro Popular/INSABI† | 2 (3.8) | 4 (5.5) | 4 (5.1) | 5 (7.4) | 5 (5.6) | 5 (6.0) | 359 (28.7) |
| Private | 3 (5.7) | 3 (4.1) | 3 (3.8) | 0 | 3 (3.3) | 2 (2.4) | 51 (4.1) |
| CPR (%) | |||||||
| Advanced | 0 | 0 | 0 | 0 | 0 | 0 | 3 (0.2) |
| Basic | 0 | 1 (1.4) | 1 (1.3) | 1 (1.5) | 0 | 0 | 7 (0.6) |
| None | 53 (100) | 72 (98.6) | 78 (98.7) | 67 (98.5) | 90 (100) | 84 (100) | 1,243 (99.2) |
| Call-to-arrival time | |||||||
| Mean (SD) | 18.1 (10.4) | 28.7 (63.3) | 19.8 (9.62) | 21.3 (9.05) | 19.8 (14.7) | 22.4 (13.4) | 16.4 (26.1) |
| Median (min, max) | 17.0 (0, 61.0) | 17.0 (0, 517) | 18.5 (0, 42.0) | 20.0 (8.00, 43.0) | 18.0 (0, 88.0) | 21.5 (0, 67.0) | 14.0 (0, 620) |
| Missing (%) | 0 | 8 (11.0) | 11 (13.9) | 10 (14.7) | 13 (14.4) | 4 (4.8) | 57 (4.5) |
| Level of consciousness (%) | |||||||
| Alert | 46 (86.8) | 60 (82.2) | 67 (84.8) | 48 (70.6) | 72 (80.0) | 64 (76.2) | 930 (74.2) |
| Verbal stimulus | 2 (3.8) | 3 (4.1) | 2 (2.5) | 4 (5.9) | 8 (8.9) | 2 (2.4) | 65 (5.2) |
| Painful stimulus | 2 (3.8) | 4 (5.5) | 3 (3.8) | 5 (7.4) | 3 (3.3) | 9 (10.7) | 107 (8.5) |
| Unresponsive | 0 | 1 (1.4) | 3 (3.8) | 3 (4.4) | 2 (2.2) | 0 | 78 (6.2) |
| Missing | 3 (5.7) | 5 (6.8) | 4 (5.1) | 8 (11.8) | 5 (5.6) | 9 (10.7) | 73 (5.8) |
| Spo2 | |||||||
| Mean (SD) | 89.0 (10.4) | 83.1 (15.4) | 83.1 (14.6) | 81.8 (16.2) | 77.1 (19.8) | 77.7 (18.5) | 90.0 (10.6) |
| Median (min, max) | 90.0 (50.0, 99.0) | 88.0 (40.0, 98.0) | 86.5 (30.0, 100) | 88.0 (43.0, 100) | 82.0 (0, 98.0) | 83.0 (31.0, 98.0) | 92.0 (0, 100) |
| Missing (%) | 3 (5.7) | 4 (5.5) | 3 (3.8) | 6 (8.8) | 5 (5.6) | 6 (7.1) | 65 (5.2) |
Numbers exclude trauma-related patients and out-of-hospital deaths. The peak observed respiratory case period, from March 31 to May 11, is compared with all of 2019.
Health insurance for government workers.
Social safety net health insurance.
Results
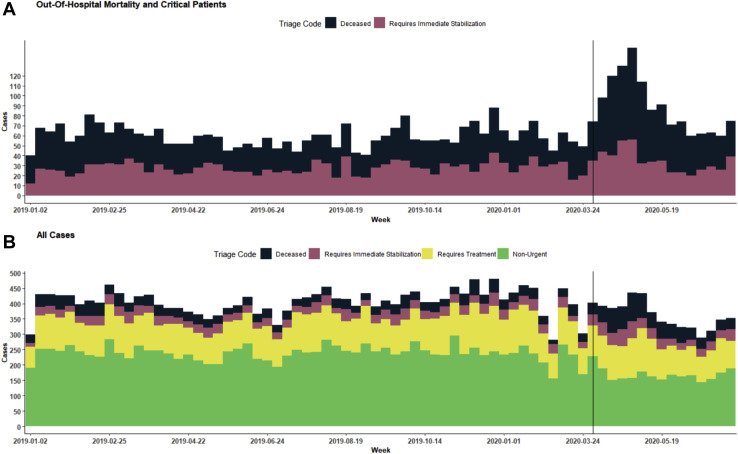
The total number of EMS cases was relatively similar before and during the peak observed COVID-19 period. There was an average of 410 weekly cases between April 14 and May 11 compared with a weekly mean of 382.9 in 2019 (Figure 1 ). There was, however, a notable shift in the composition of cases. We observed a decreasing quantity of nonurgent cases, which declined to 39.0% of all cases from April 14 to May 11, compared with a 59.1% average for 2019, likely because of social distancing and increased reluctance to use health care services for nonurgent matters. Both urgent and deceased cases increased, reaching 11.2% and 20.0%, respectively, during this period compared with 6.7% and 7.9%, respectively, in 2019.
Figure 1.
Weekly case breakdown by triage priority code, 2019 to 2020. A, Only out-of-hospital mortality cases and patients in critical condition who required urgent hospitalization. B, The full distribution of patients. Both A and B refer to nontrauma patients and include data from 2019 through June 2020. The vertical black line marks the week of March 31, when respiratory morbidity cases began to increase.
There were no substantial differences in CPR rates before or during the COVID-19 period (Table 1), likely because overall CPR administration rates were generally quite low among nontrauma patients in Tijuana (Figure E1, available online at http://www.annemergmed.com). Average ambulance travel time from dispatch to arrival on scene was slightly longer during the observed COVID-19 peak period (20.5 minutes) compared with that in 2019 (16.4 minutes). Pre-epidemic time-to-arrival intervals were higher than those typically observed in higher-income urban areas and may help explain low life-support rates among critical patients.
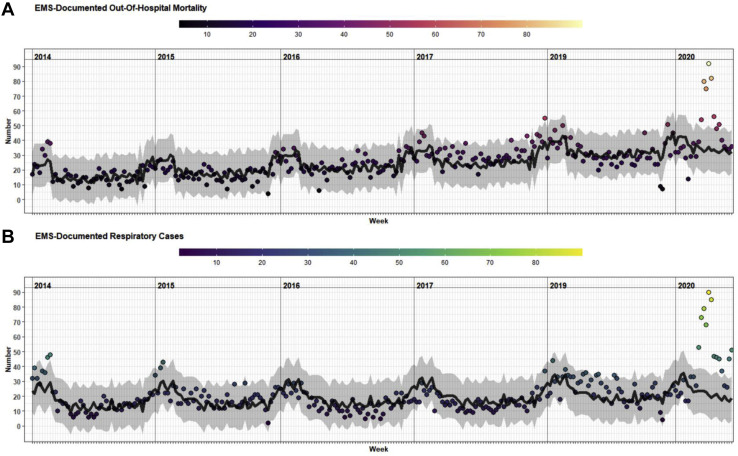
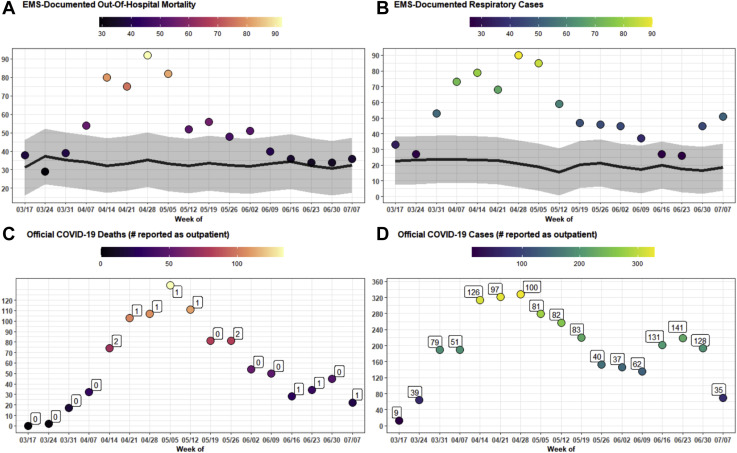
From January to March 2020, the number and proportion of out-of-hospital mortality cases were within or below the 95% prediction interval according to trends observed from 2014 to 2019 (Figure 2 ). However, the week of April 14 had 80 out-of-hospital deaths (Figure 3 A), exceeding the previously observed maximum in the time series (Figure 2). The peak epidemic window for out-of-hospital mortality lasted from April 14 to May 11. During this time, 329 deaths occurred, which were compared with the predicted number of 134.3 (95% confidence interval 75.1 to 193.5) for the same period, yielding an estimated excess of 194.7 deaths (95% CI 135.5 to 253.9). This represents an increase of 145.0% (95% CI 70.1% to 338.2%) compared with expected trends. Similar results were observed when the percentage of cases represented by deaths was modeled, and when the analysis was restricted to only dead-on-arrival out-of-hospital mortality (Figures E2 and E3, available online at http://www.annemergmed.com). The peak epidemic window of out-of-hospital mortality was observed at the same time as the highest rates of COVID-19 deaths according to official statistics (Figure 3 C). Four hundred eighteen deaths among patients with confirmed COVID-19 were reported during the same peak COVID-19 window (according to official data released on July 15, 2020). However, only 5 of these deaths were reported as occurring “in an outpatient context,” the remainder being reported as occurring among “hospitalized patients.”35
Figure 2.
Long-term EMS-documented out-of-hospital mortality and respiratory cases, 2014 to 2020. Expected values (black line) and 95% prediction intervals (gray band) based on model fit on data from 2014 to 2019, with forecasts through June 2020. Both series exclude trauma patients. A, EMS-documented out-of-hospital mortality. B, EMS-documented respiratory cases.
Figure 3.
EMS-documented out-of-hospital mortality and respiratory cases compared with official COVID-19 case and mortality numbers, March 17 to June 29. A, EMS-documented out-of-hospital mortality, with the observed and expected number shown in text. B, EMS-documented respiratory cases, with the observed and expected number shown in text. C, Deaths among patients with confirmed COVID-19, according to official national government statistics, with the number reported as managed in the outpatient setting and the total reported in text. D, Number of patients with confirmed COVID-19, according to official national government statistics, with the number reported as managed in the outpatient setting and the total reported in text. A to D, Weekly totals. A and B, Expected values (black line) and 95% prediction intervals (gray band) based on forecasted trends from 2014 to 2019; trauma patients are excluded.
Out-of-hospital deaths during the peak epidemic period occurred mostly in men (68.4%) aged 18 to 64 years (64.1%) who were beneficiaries of the Mexican National Institute for Social Security (IMSS) health care system (45.9%) (Table 1). IMSS is a social security scheme providing health care to individuals employed in the private formal sector (eg, salaried positions for which income is reported to the government). Although the age and sex patterns were largely similar to those observed throughout 2019, individuals were more likely to be IMSS beneficiaries (45.9% versus 29.9%; difference=16.3% [95% confidence interval 10.0% to 22.0%]).
In addition to out-of-hospital mortality, we also noted an increase in respiratory cases, which had a peak epidemic window that started earlier than that of out-of-hospital mortality. Respiratory cases increased above the prediction interval of expected values during the week of March 31 (Figure 3 B). Nevertheless, the peak observed-to-expected ratio occurred in the same week as that of out-of-hospital mortality, reaching 90 cases during the week of April 28. During March 31 to May 11, 448 respiratory cases were observed, representing 314.9 (95% CI 224.8 to 404.9) more than expected, an increase of 236.5% (95% CI 100.7% to 940.0%). Similar results were observed when we modeled the percentage of respiratory cases (Figure E3, available online at http://www.annemergmed.com). Similar to the trends observed for out-of-hospital mortality, respiratory patients during March 31 to May 11 were mainly men (61.5%), of working age (72.0%), and IMSS beneficiaries (66.4%) (Table 2). Compared with respiratory patients in 2019, those in the peak observed epidemic period were more likely to be IMSS beneficiaries (66.4% versus 38.9%; difference=27.6% [95% CI 22.3% to 32.9%]) and have an Spo 2 lower than 90% (54.8% versus 32.4%; difference=22.4% [95% CI 17.0% to 27.9%]).
The overall trend of EMS-documented respiratory cases was similar to that observed in confirmed COVID-19 cases reported in official statistics (Figure 3 D). However, the magnitude was substantially lower; the week of April 14, for example, had 314 COVID-19 cases, and 188 of these patients were hospitalized, which greatly exceeded the 79 total EMS-documented respiratory cases.
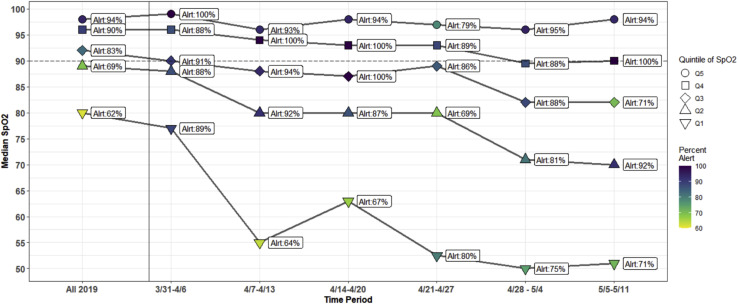
The mean Spo 2 value among respiratory patients declined steadily from 90.0% during the pre-epidemic period of 2019, reaching a low of 77.7% during the week of April 28 (Table 2). Figure 4 shows the weekly evolution of the distribution of Spo 2 values among respiratory patients. The highest quintile of the distribution of Spo 2 values remained fairly stable throughout the study period, with a median value greater than 95%. Nevertheless, Spo 2 values in the remaining quintiles of the distribution generally decreased, and a widening of the distribution of Spo 2 was observed as a result. In the week of April 7, the lowest quintile of the distribution of Spo 2 values decreased sharply, reaching a median Spo 2 of 55%. Despite the lower average Spo 2, the proportion of patients presenting as alert and oriented did not experience a commensurate decrease relative to baseline (Table 2 and Table E1 [available online at http://www.annemergmed.com]), even among the lowest quintile of Spo 2 values (Figure 4).
Figure 4.
Trends in Spo2 and percentage of patients presenting alert among EMS-documented respiratory cases. The distribution of Spo2 values over time is visualized weekly from March 31 to May 11, 2020, and compared with all data from 2019. Respiratory cases were divided into 5 quintiles of Spo2 values, and the median of each quartile is plotted. The color reflects the percentage of individuals in each quartile who presented as alert, which is also plotted as text next to each point.
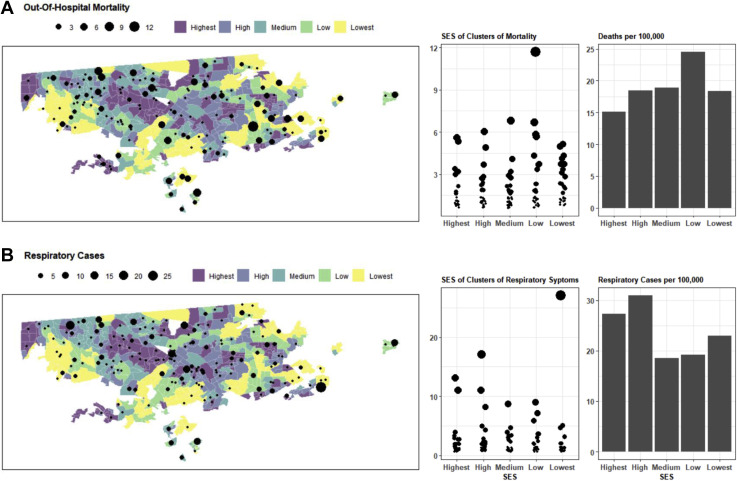
EMS data can also provide insights into the location of outbreaks and to social disparities in the distribution of the COVID-19 mortality and morbidity. Figure 5 highlights the socioeconomic status and geospatial distribution of out-of-hospital mortality and respiratory cases in Tijuana. The largest clusters of out-of-hospital mortality did not occur in the same locations as the largest clusters of respiratory cases. Clusters of respiratory cases during the peak epidemic period were most concentrated in highest- and high-socioeconomic-status quintiles of Tijuana. The largest clusters of out-of-hospital mortality cases were observed in the low-socioeconomic-status quintile. Rates per 100,000 people the low-socioeconomic-status quintile of the population had the highest rate of out-of-hospital mortality, at 24.5, whereas the high-socioeconomic-status quintile had the highest rate of respiratory cases, at 30.9.
Figure 5.
Out-of-hospital mortality and respiratory cases by neighborhood and neighborhood socioeconomic status. The categoric socioeconomic status of each basic statistical unit (basic geostatistical area) is mapped for Tijuana. Overlaid is the out-of-hospital mortality occurring during April 14 to May 11 (A) and respiratory cases occurring during March 31 to May 11 (B). The number of cases in each neighborhood is shown as a point, with the size reflecting the magnitude. In the middle column, the points are organized by neighborhood socioeconomic status. On the right, the number of cases is shown as a rate per 100,000 people for each quintile of neighborhood socioeconomic status. SES, Socioeconomic status.
Limitations
We were unable to differentiate whether observed excess out-of-hospital mortality was solely attributable to COVID-19 infections or whether it also reflected increased death rates from other causes. For example, increased cardiac arrest frequency could have arisen if patients stayed home during ischemic chest pain episodes, because the system was saturated, or because they were afraid to seek care. Although we did examine the diagnostic codes associated with each death, the EMTs completing the records were unable to reliably ascertain the cause of death in the majority of cases, and information about previous COVID-19 tests was typically not available. Similarly, our measure of respiratory cases reflects only Spo 2 values below 92%, or other respiratory symptoms, and cannot directly indicate patient COVID-19 status. Like any analysis using EMS data, the out-of-hospital mortality statistics presented here cannot capture events occurring in the absence of 911 activations. Although there was a large increase in out-of-hospital mortality, our results may not represent the full increase in absolute numbers. However, if the proportion of deaths resulting in 911 activations were to be correlated with the onset of the COVID-19 pandemic, that could bias our results in an unpredictable direction.
We used neighborhood-level socioeconomic status, which is an imperfect measure of person-level socioeconomic status. Furthermore, we used population and socioeconomic status values from the most recent census, 2010, because newer data were not available. This may have missed trends in some rapidly changing parts of Tijuana. This analysis should be updated when 2020 census data become available. Additionally, the model we used to extrapolate past trends into 2020 was straightforward in design, and we did not perform out-of-sample predictive validity testing or compare alternative predictive model forms. Nevertheless, given the magnitude of the disparities observed, and the presence of some missing data in past years of observed trends, we opted for a simple and easy-to-interpret model. Furthermore, many studies of this nature simply use the previous year’s values as a comparison group,12 and therefore a simple approach may be preferable. Finally, because our results and conclusions were drawn from an observational study from a single context, additional confirmation studies from other settings would be helpful in strengthening the evidence base for these potentially critical aspects of COVID-19 epidemiology.
Discussion
We used data from Tijuana, Mexico, to illustrate how EMS systems may be a useful source of real-time information for tracking the COVID-19 epidemic, perhaps especially in low- and middle-income-country contexts in which other sources of information are not rapidly available. We showed that out-of-hospital mortality documented by the EMS system increased significantly during the peak observed COVID-19 epidemic period observed in April and May 2020. The relative excess mortality—145% above baseline—represents between a 2- and 3-fold increase compared with the 58% figure reported in a recent similar study from the Lombardy region of Italy.12 This may be related to Tijuana’s being in a middle-income country, with a relatively more fragile health care system and lower-income population. These results suggest that other regions of Mexico, and low- and middle-income countries in general, may need to plan for and ameliorate sharply increasing rates of out-of-hospital mortality to prevent a large burden of potentially unmeasured death stemming from the COVID-19 pandemic. These findings echo an increasing number of calls for health system strengthening in low- and middle-income countries in the face of the COVID-19 pandemic.15, 16, 17, 18, 19
During April 14 to May 11, in which we estimate 194.7 excess deaths occurred, only 5 official COVID-19 deaths were reported as “outpatient” deaths, the remainder being categorized as deaths of “hospitalized” patients. This suggests that the increase in out-of-hospital mortality that we observed cannot be explained by official COVID-19 statistics. We were not able to ascertain the cause of the excess mortality we observed. It is therefore possible that most of the excess deaths resulted from non–COVID-19 causes stemming from delay of care or health system saturation. It is also possible that many of the deaths we observed represented COVID-19 patients who never received such a diagnosis or were never formally tracked as having it. Finally, delays in reporting or data presentation may simply have led to lower weekly totals for out-of-hospital mortality among known COVID-19 patients who were not hospitalized.42 In any case, EMS data represent an important source of near-real-time information that can be used to rapidly track the evolving health of COVID-19–affected populations. We propose that EMS systems may play an especially important sentinel role in low- and middle-income countries, and can be used to monitor excess out-of-hospital mortality during the COVID-19 crisis. This function may be of particular importance in low- and middle-income countries, given the lack of access to rapid vital statistics registration records. Nevertheless, similar trends have been noted in a number of higher-income locations,13 , 14 and therefore these findings may have relevance to a wide range of contexts.
More research is required to explore what role access to COVID-19 tests, lags in official COVID-19 statistics, or access to hospital beds may be playing in driving differences between EMS-documented and official statistics. Increased testing in out-of-hospital settings may be required to determine whether excess mortality is being driven by COVID-19 infection, health system saturation, or patient avoidance of health care.
Although EMS staff were not able to generate substantial clinical information about patients who died before reaching a hospital, because most were found dead on EMS arrival, important clues about the cause of out-of-hospital mortality may be gleaned by assessing clinical and demographic characteristics among living patients treated for respiratory symptoms during the same period. During the window of observed peak excess mortality, we also observed a concurrent elevation in the rate of patients presenting with respiratory symptoms. These patients had demographic characteristics similar to those of the patients with out-of-hospital mortality. Although the number of respiratory patients reached the highest rate observed during the 2014 to 2020 period studied, it was still lower than the number of official COVID-19 patients who were hospitalized. This suggests that most officially documented COVID-19 patients are reaching health care facilities independently of the EMS system in Tijuana.
The detection of silent hypoxemia is difficult by definition. Patients typically present to EMS services only after they experience dyspnea. Nevertheless, it is possible that some indirect evidence about silent hypoxemia can be observed in the declining Spo 2 values seen among respiratory patients during the observed peak COVID-19 window. There was a sharp decline in mean Spo 2 values, although no concomitant decrease was observed among the percentage of patients who were alert on presentation. Hypoxemia is a known predictor of mortality among COVID-19 patients,43 and these data suggest that silent hypoxemia and subsequent rapid decompensation is a relevant factor to understanding out-of-hospital mortality rates.
Given the novel nature of the COVID-19 pathophysiology, more education about silent hypoxemia is needed for physicians to better manage it clinically and for patients to better understand the risks.28 , 43 As COVID-19 quickly overwhelms frail health care systems, clinicians on the front lines may easily overlook a well-appearing patient despite a low Spo 2 to make room for patients who are overtly sick. It is important for patients to understand that in silent hypoxemia, dyspnea is a late-stage symptom, and their condition may be deteriorating without perceived decreases in subjective respiratory ability.25 Detection of hypoxemia in the general population should be undertaken, and priority areas can be identified with clusters from EMS data, such as those shown in Figure 5.
The social pattern of out-of-hospital mortality and respiratory cases also deserves consideration and monitoring in the COVID-19 crisis context. We observed a differential trend by neighborhood socioeconomic status between out-of-hospital mortality and respiratory cases. Although respiratory cases were strikingly concentrated in the high- and highest-socioeconomic-status quintiles, the highest out-of-hospital mortality rates were observed in low-socioeconomic-status areas. There was a notable difference between respiratory cases and deaths, which may suggest that the profile of individuals who have the economic or social capital to seek care early for respiratory symptoms in Tijuana differs from that of those who do not interact with the medical system until they are gravely ill. This finding adds to an increasing body of literature and social commentary suggesting that social inequalities may be translating into inequalities in the risk of infection or death from COVID-19 in numerous contexts.44, 45, 46, 47, 48, 49, 50
EMS data provide a valuable tool to rapidly track the health of populations at risk of COVID-19 in low- and middle-income countries, where other forms of real-time data may not be available. EMS information can be used to track excess out-of-hospital mortality and respiratory disease burden, as well as changing clinical or demographic features. Detected clusters of out-of-hospital mortality or cases can be subsequently targeted for screenings for hypoxemia and COVID-19 status. Social disparities in COVID-19 and out-of-hospital mortality should be monitored, and additional resources may need to be directed to low-socioeconomic-status areas.
Among respiratory patients, the decrease of Spo 2 observed during the peak epidemic period suggests that hypoxemia precedes clinical manifestations such as dyspnea (silent hypoxemia). The lack of overt clinical manifestations early in the disease and the resulting difficulty in detecting silent hypoxemia may be drivers of out-of-hospital mortality in low- and middle-income countries, where the health system is easily overwhelmed and accessing EMS services is more difficult.
Acknowledgments
The authors acknowledge Alberto Luna, BE, for his efforts related to data preparation and management; and, for facilitating data collection and access, acknowledge the Mexican Red Cross, Andres Smith, MD, Juan Carlos Mendez, MEd, and the numerous emergency medical technicians and paramedics working tirelessly on the front lines.
Footnotes
Please see page 414 for the Editor’s Capsule Summary of this article.
Supervising editor: Jonathan L. Burstein, MD. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Author contributions: JF, AC-V, and ETH conceived and designed the study and oversaw data acquisition. JF and AC-V analyzed the data. All authors contributed to data interpretation, as well as drafting and critical revision of the article. ETH takes responsibility for the paper as a whole.
All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. This study was primarily self-funded by the Mexican Red Cross in Tijuana. Mr. Friedman received support from the UCLA Medical Scientist Training program (National Institutes of Health National Institute of General Medical Science training grant GM008042).
Readers: click on the link to go directly to a survey in which you can provide feedback to Annals on this particular article.
A podcast for this article is available at www.annemergmed.com.
Supplementary Data
Number of CPR Administrations by Triage Priority Code, 2019-2020
Figure E2. EMS-Documented Dead-On-Arrival Mortality and Respiratory Cases Compared to Official COVID-19 Case and Mortality Numbers, March 17th – June 29th
Figure E3. Long-Run EMS-Documented Out-Of-Hospital Mortality and Respiratory Percent of Cases, 2014-2020
Table E1. Characteristics of Respiratory Patients by Categorical SpO2
References
- 1.Danel I. An assessment of LAC’s vital statistics system: the foundation of maternal and infant mortality monitoring. http://documents.worldbank.org/curated/en/206651468177844686/pdf/448620WP0Box3210paper01LACVitalStat.pdf Available at:
- 2.Civil Registration and Vital Statistics Knowledge Center Estimating census and death registration completeness (census completeness, death registration coverage) https://unstats.un.org/unsd/vitalstatkb/KnowledgebaseArticle50331.aspx Available at:
- 3.Mikkelsen L., Phillips D.E., AbouZahr C. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet. 2015;386:1395–1406. doi: 10.1016/S0140-6736(15)60171-4. [DOI] [PubMed] [Google Scholar]
- 4.Híjar M., Chandran A., Pérez-Núñez R. Quantifying the underestimated burden of road traffic mortality in Mexico: a comparison of three approaches. Traffic Inj Prev. 2012;13(suppl 1):5–10. doi: 10.1080/15389588.2011.631065. [DOI] [PubMed] [Google Scholar]
- 5.Lozano-Esparza S., Stern D., Hernandez-Avila J.E. Evaluation of Mexico’s low cancer mortality using two national death registries. Salud Publica Mex. 2020;62:181–185. doi: 10.21149/10635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDonnell P.J., Linthicum K., Fry W. How many people are dying of coronavirus in Mexico? it’s hard to say. https://www.latimes.com/world-nation/story/2020-05-16/how-many-people-are-dying-of-covid-19-in-mexico-no-one-knows-for-sure Available at: Published May 16, 2020. Accessed July 14, 2020.
- 7.Romero Zavala M., Despeghel L. ¿Qué nos dicen las actas de defunción de la CDMX? Actualización al 31 de mayo de 2020. https://datos.nexos.com.mx/?p=1443 Available at:
- 8.Geografía (Instituto Nacional de Estadística y Geografía). Mortalidad. Registros administrativos. Vitales. Natalidad. Matrimonios. https://www.inegi.org.mx/temas/mortalidad/ Available at: Published January 1, 1994. Accessed May 15, 2020.
- 9.Ritchie H., Roser M., Ortiz-Espinosa E. Excess mortality from the coronavirus pandemic (COVID-19) https://ourworldindata.org/excess-mortality-covid Available at:
- 10.Modi C., Boehm V., Ferraro S. How deadly is COVID-19? A rigorous analysis of excess mortality and age-dependent fatality rates in Italy. medRxiv. 2020 doi: 10.1101/2020.04.15.20067074. [DOI] [Google Scholar]
- 11.Centers for Disease Control and Prevention Excess deaths associated with COVID-19. http://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm Available at: Published May 1, 2020. Accessed May 1, 2020.
- 12.Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;38:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tamman M. At-home COVID-19 deaths may be significantly undercounted in New York City. https://www.reuters.com/article/us-health-coronavirus-fdny-idUSKBN21P3KF Available at: Published April 8, 2020. Accessed July 13, 2020.
- 14.Hixenbaugh M., Ornstein C. As coronavirus surges, Houston confronts its hidden toll: people dying at home. https://www.nbcnews.com/news/us-news/coronavirus-surges-houston-confronts-its-hidden-toll-people-dying-home-n1233151 Available at:
- 15.Ayebare R.R., Flick R., Okware S. Adoption of COVID-19 triage strategies for low-income settings. Lancet Respir Med. 2020;8:e22. doi: 10.1016/S2213-2600(20)30114-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low- and middle-income countries. JAMA. 2020;323:1549–1550. doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- 17.Siow W.T., Liew M.F., Shrestha B.R. Managing COVID-19 in resource-limited settings: critical care considerations. Crit Care. 2020;24:1–5. doi: 10.1186/s13054-020-02890-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahmed F., Ahmed N., Pissarides C. Why inequality could spread COVID-19. Lancet Public Health. 2020;5:e240. doi: 10.1016/S2468-2667(20)30085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paternina-Caicedo A.J., Choisy M., Garcia-Calavaro C. Social interventions can lower COVID-19 deaths in middle-income countries. medRxiv. 2020 https://doi.org/10.1101/2020.04.16.20063727 [Google Scholar]
- 20.Murray C.J.L. Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. medRxiv. 2020 https://doi.org/10.1101/2020.03.27.20043752 [Google Scholar]
- 21.Brown P., Jha P., Center for Global Health Research COVID Mortality Consortium Mortality from COVID-19 in 12 countries and 6 states of the United States. medRxiv. https://doi.org/10.1101/2020.04.17.20069161
- 22.Walker P., Whitaker C., Watson O.J. Report 12: the global impact of COVID-19 and strategies for mitigation and suppression. http://www.imperial.ac.uk/medicine/departments/school-public-health/infectious-disease-epidemiology/mrc-global-infectious-disease-analysis/covid-19/report-12-global-impact-covid-19/ Available at:
- 23.Brown E., Tran A.B., Reinhard B. US deaths soared in early weeks of pandemic, far exceeding number attributed to covid-19. https://www.washingtonpost.com/investigations/2020/04/27/covid-19-death-toll-undercounted/ Available at: Published April 27, 2020. Accessed May 1, 2020.
- 24.Xie J., Tong Z., Guan X. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020;46:837–840. doi: 10.1007/s00134-020-05979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gattinoni L., Chiumello D., Caironi P. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46:1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whittle J.S., Pavlov I., Sacchetti A.D. Respiratory support for adult patients with COVID-19. J Am Coll Emerg Physicians Open. 2020;1:95–101. doi: 10.1002/emp2.12071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ottestad W., Seim M., Mæhlen J.O. COVID-19 with silent hypoxemia. Tidsskrift Nor Laegeforen. 2020;140 doi: 10.4045/tidsskr.20.0299. [DOI] [PubMed] [Google Scholar]
- 28.Kashani K.B. Hypoxia in COVID-19: sign of severity or cause for poor outcomes. Mayo Clin Proc. Mayo Clin Proc. 2020;95:1094–1096. doi: 10.1016/j.mayocp.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dirección General de Epidemiología Información referente a casos COVID-19 en México. https://datos.gob.mx/busca/dataset/informacion-referente-a-casos-covid-19-en-mexico Available at: Published May 2, 2020. Accessed May 3, 2020.
- 30.Gobierno de México Proyecciones de la Población de México y de las Entidades Federativas, 2016-2050: datos.gob.mx/busca. https://datos.gob.mx/busca/dataset/proyecciones-de-la-poblacion-de-mexico-y-de-las-entidades-federativas-2016-2050 Available at:
- 31.Bowler M., Rivlin-Nadler M. Tijuana runs low on ventilators as COVID-19 cases continue to rise. https://www.kpbs.org/news/2020/apr/24/tijuana-runs-low-ventilators-covid-19-cases-contin/ Available at:
- 32.Fry W. Ensenada blocks access to city to protect citizens from coronavirus. https://www.sandiegouniontribune.com/news/border-baja-california/story/2020-04-20/ensenada-closes-entry-to-city-to-protect-citizens-from-coronavirus Available at: Published April 21, 2020. Accessed May 1, 2020.
- 33.Universidad Nacional Autónoma de México (UNAM) COVID-19 monitoreo de la situación por municipios. https://www.arcgis.com/apps/opsdashboard/index.html#/f0f10e692a814fd8aa8afc7f8575f5d2 May 2020. Available at: Published 2020. Accessed May 3, 2020.
- 34.Mexican Red Cross. http://www.cruzrojatijuana.org.mx/socorros/ Available at:
- 35.Secretaría de Salud Datos Abiertos: Dirección General de Epidemiología. http://www.gob.mx/salud/documentos/datos-abiertos-152127 Available at:
- 36.Mexican National Government NORMA Oficial Mexicana NOM-034-SSA3-2013, Regulación de Los Servicios de Salud. Atención Médica Prehospitalaria. http://www.dof.gob.mx/nota_detalle.php?codigo=5361072&fecha=23/09/2014 Available at:
- 37.INEGI Censos y conteos de población. http://www.inegi.org.mx/sistemas/consulta_resultados/iter2010.aspx Available at:
- 38.Han C., Duan C., Zhang S. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020;115:916–923. doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hussain A., Bhowmik B., do Vale Moreira N.C. COVID-19 and diabetes: knowledge in progress. https://www-ncbi-nlm-nih-gov.offcampus.lib.washington.edu/pmc/articles/PMC7144611/ Available at: [DOI] [PMC free article] [PubMed]
- 40.Consejo Nacional de Población CONAPO Índice de marginación urbana 2010. http://www.conapo.gob.mx/es/CONAPO/Indice_de_marginacion_urbana_2010 Available at:
- 41.INEGI Geoestadística. http://www.inegi.org.mx/geo/contenidos/geoestadistica/ Available at:
- 42.Gonzalez H. Estimando el subregistro de defunciones por COVID-19 en México. https://datos.nexos.com.mx/?p=1406 Available at:
- 43.Xie J., Covassin N., Fan Z. Association between hypoxemia and mortality in patients with COVID-19. Mayo Clin Proc. 2020;95:1138–1147. doi: 10.1016/j.mayocp.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whittle R.S., Diaz-Artiles A. An ecological study of socioeconomic predictors in detection of COVID-19 cases across neighborhoods in New York City. medRxiv. 2020;18:271. doi: 10.1186/s12916-020-01731-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wadhera R.K., Wadhera P., Gaba P. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323:2191–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chung R.Y.-N., Dong D., Li M.M. Socioeconomic gradient in health and the covid-19 outbreak. BMJ. 2020;369:m1329. doi: 10.1136/bmj.m1329. [DOI] [PubMed] [Google Scholar]
- 47.Dobin D., Dobin A. Racial/ethnic and socioeconomic disparities of Covid-19 attacks rates in Suffolk County communities. http://arxiv.org/abs/2004.12175 Available at: Published April 25, 2020. Accessed May 1, 2020.
- 48.Villarosa L., Harris L.K. “A terrible price”: the deadly racial disparities of Covid-19 in America. https://www.nytimes.com/2020/04/29/magazine/racial-disparities-covid-19.html Available at: Published April 29, 2020. Accessed May 1, 2020.
- 49.Guha A., Bonsu J., Dey A. Community and socioeconomic factors associated with COVID-19 in the United States: zip code level cross sectional analysis. medRxiv. medRxiv. 2020 https://doi.org/10.1101/2020.04.19.20071944 [Google Scholar]
- 50.Raifman M., Raifman J. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59:137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Number of CPR Administrations by Triage Priority Code, 2019-2020
Figure E2. EMS-Documented Dead-On-Arrival Mortality and Respiratory Cases Compared to Official COVID-19 Case and Mortality Numbers, March 17th – June 29th
Figure E3. Long-Run EMS-Documented Out-Of-Hospital Mortality and Respiratory Percent of Cases, 2014-2020
Table E1. Characteristics of Respiratory Patients by Categorical SpO2